Abstract
In this review, we cover the current understanding of BRAF mutations and associated clinical characteristics in patients with metastatic NSCLC, approved and emerging treatment options, BRAF sequencing approaches, and unmet needs. The BRAFV600E mutation confers constitutive activity of the MAPK pathway, leading to enhanced growth, proliferation, and survival of tumor cells. Testing for BRAF mutations enables patients to be treated with therapies that directly target BRAFV600E and the MAPK pathway, but BRAF testing lags behind other oncogene testing in metastatic NSCLC. Additional therapies targeting BRAFV600E mutations provide options for patients with metastatic NSCLC. Emerging therapies and combinations under investigation could potentially overcome issues of resistance and target non-V600E mutations. Therefore, because targeted therapies with enhanced efficacy are on the horizon, being able to identify BRAF mutations in metastatic NSCLC may become even more important.
Similar content being viewed by others
Introduction
Mutations in the v-Raf murine sarcoma viral oncogene homolog B (BRAF) gene have been found in ~4–8% of all cancers, with the greatest number found in colorectal cancer (CRC), melanoma, and non-small cell lung cancer (NSCLC)1,2,3. The most common BRAF mutation is a point mutation (T1799A) resulting in an amino acid substitution at codon 600 (V600E), which confers constitutive BRAF kinase activity2,4,5. BRAFV600E accounts for ~1–2% of NSCLCs, making it an actionable therapeutic target given the success of other therapies that target actionable mutations with similar frequencies in NSCLC (e.g., ALK, EGFR)6,7,8,9. Targeted therapeutic approaches with BRAF inhibitor monotherapy (vemurafenib and dabrafenib) demonstrated efficacy in phase 2 trials with generally acceptable toxicity in patients with BRAFV600-mutant advanced NSCLC10,11.
While BRAFV600E inhibitor monotherapy is initially effective, acquired resistance and paradoxical activation are associated with reactivation of the mitogen-activated protein kinase (MAPK) pathway and subsequent disease progression12,13,14. To delay onset of resistance, BRAF inhibitors were combined with a downstream inhibitor of the MAPK pathway, MAPK kinase (MEK)14. Trametinib, a MEK inhibitor, in combination with dabrafenib showed durable anti-tumor activity and acceptable safety in patients with BRAFV600E-mutant metastatic NSCLC in phase 2 trials15,16,17. The combination of BRAF inhibitor encorafenib plus MEK inhibitor binimetinib is being investigated in ongoing phase 2 trials in patients with BRAFV600E-mutant metastatic NSCLC5,18,19. Initial results of the PHAROS trial revealed the combination had substantial and durable anti-tumor activity and a manageable safety profile18. Based on the results from this study, in October 2023, the US Food and Drug Administration (FDA) approved encorafenib plus binimetinib for patients with BRAFV600E-mutant metastatic NSCLC20. Current guidelines recommend dabrafenib plus trametinib or encorafenib plus binimetinib as preferred first-line treatment options or as subsequent treatment for BRAFV600E-mutant metastatic NSCLC21. BRAF monotherapy could be considered in certain circumstances, such as lack of tolerability.
While there has been notable progress in effective treatments for BRAF-mutant NSCLC17,18, several uncertainties remain. Current guidelines for BRAFV600-mutant NSCLC recommend BRAF-targeted therapy in the first-line setting, but the optimal course for patients who do not tolerate or progress while on first-line BRAF and MEK inhibitor combinations remains ambiguous21,22. Second-line recommendations include immunotherapy, chemotherapy, or a combination; however, immunotherapy data are limited and conflicting for patients with BRAFV600-mutant NSCLC22,23,24. Current targeted therapeutic approaches have limited efficacy in patients with non-V600 BRAF mutations, and most clinical trials have focused primarily on the V600E mutation since its discovery11,17,18,25. There remains a need to better understand the incidence, impact, and management of brain metastases; mechanisms of resistance; optimal sequencing; and other patient- (e.g., smoking history) or disease-related factors (e.g., PD-L1 expression) that influence treatment outcomes of BRAF-mutant metastatic NSCLC. This manuscript provides a review of BRAF-mutant metastatic NSCLC and the therapeutic landscape with particular emphasis on targeted therapies for the V600E mutation.
BRAF-mutant metastatic NSCLC disease overview
Clinical characteristics
While BRAF mutations are predominantly found in adenocarcinomas (>85%), there is no clear association of BRAF mutation status with other patient characteristics, such as age, ethnicity, and sex6,8,9,26. Epidemiological patterns are difficult to identify since BRAF mutations occur in a small number of patients with advanced NSCLC5. One study reported that BRAFV600E mutations were significantly more common in females (P < 0.001), but that finding was not consistent with other studies6,10,26. While data are limited, studies have also shown that the incidence of BRAF mutations is lower in Asian patients than white patients6,26,27. Smoking history can be associated with BRAF mutations, as well as KRAS, MET, and other mutations9,28,29. However, a few studies have also suggested that BRAFV600E is less associated with smoking history than other BRAF mutations26,30,31. Therefore, all patients with advanced NSCLC regardless of smoking history should undergo broad-based mutation testing, including BRAF5,21,22. Programmed death ligand 1 (PD-L1) expression and tumor mutation burden (TMB) are potentially important indicators of immunotherapy response and are frequently elevated in BRAF-mutant NSCLC24. The prognostic implication of BRAF mutation status is inconclusive due to small patient numbers and conflicting studies8,26,28. However, a few studies reported worse outcomes with chemotherapy in patients with V600E mutations versus wild type (WT) BRAF and conflicting results for V600E versus non-V600E mutations6,31,32,33. In addition to the small patient number, discrepancies in patient characteristics and prognosis could be attributed to the heterogeneity of BRAF mutations in NSCLC33,34.
Classification of BRAF mutations
BRAF mutations are heterogenous with distinct mutation classes that each yield a functionally diverse BRAF protein, resulting in different clinical features and treatment ramifications33,35. BRAF-mutant proteins interact with and activate the MAPK pathway in various ways and to different degrees (Fig. 1)25,35,36. In the MAPK pathway, the signaling cascade begins with growth factor binding to receptor tyrosine kinase (RTK) which facilitates RAS binding GTP14,25,36. Activated RAS promotes a cascade of activation starting with RAF family kinases (ARAF, BRAF, CRAF), which form activated RAF homo- or heterodimers. RAF kinases activate MEK, which subsequently activates extracellular signal-regulated kinase (ERK). ERK has multiple downstream targets, including transcription factors that promote cell growth, proliferation, and survival. Negative feedback loops from ERK also regulate the pathway25.
Class I and II mutations are RAS-independent, constitutively active monomers (class I) or dimers (class II). Class III mutations are RAS-dependent dimers with compromised kinase activity. Current BRAF inhibitors are effective for class I-mutant monomers. Next-generation RAF inhibitors can inhibit dimers and may inhibit class II and III mutations. P, phosphorylation.
There are over 200 identified BRAF mutations categorized into three classes based on dimerization status, RAS-dependence, and kinase activity level5,37. Class I BRAF mutations occur on codon 600 (BRAFV600), substituting the valine to a glutamic acid, lysine, aspartic acid, arginine, or methionine (V600E, V600K, V600D, V600R, and V600M mutations, respectively) and can biochemically transform BRAF into a RAS-independent constitutively active monomer25,36. BRAFV600E is the most prevalent class I mutation and accounts for ~30–50% of all BRAF mutations in NSCLC6,7,33. Class I mutant proteins have a high level of kinase activity, and BRAFV600E is ~500-fold times more active than WT BRAF, leading to increased cellular proliferation4,36. Class I mutations all occur at codon 600 aberrantly activating monomers, but class II and III mutations occur at various other non-600 codons and form dimers5,25,36. Class II BRAF mutations span from G464 to K601, which includes the activation segment and P-loop domains of BRAF. These mutations, along with fusions and in-frame deletion mutations, are shown or predicted to be able to biochemically transform BRAF into a RAS-independent constitutively active dimer with ranges of intermediate to high kinase activity. Class III mutations, which tend to have impaired kinase activity, occur in the P-loop, catalytic loop, or DFG motif to form RAS-dependent heterodimers with CRAFWT. These mutations require upstream activation of RAS to amplify downstream signaling, similar to its normal physiological role and function.
Although constitutive activity of class I and II mutations can suppress RAS through ERK-negative feedback loop, class III mutations only mildly activate ERK, resulting in minimal negative feedback of RAS25,38. To overcome that feedback inhibition, class III BRAF mutations are often observed with concurrent RAS activating mutations25,33,38. While these coexisting mutations often occur in melanoma cancers, CRC and NSCLC cancers have fewer cases25,38: one study in NSCLC tumors reported coexisting RAS mutations in 22% of class III mutations (n = 54), including 42% of kinase-dead mutations (n = 19)33. This may be explained by basal RTK activation and subsequent RAS activity that is sufficient to support these class III mutants25.
Currently approved BRAF inhibitors effectively inhibit only class I mutant proteins and show substantially less efficacy against BRAF-mutant dimers (Fig. 1)25. BRAF monomer inhibitors binding to dimers can cause paradoxical transactivation of the unbound RAFWT protomer, enabling MEK/ERK signaling and subsequent disease progression12,13,25. Upstream inhibition may be an effective therapeutic strategy for treatment of class III mutations25,33,38. A better understanding of BRAF mutations, especially class II and III mutations, may enable the rational design of new targeted therapies and the development of next-generation drug combination strategies to treat BRAF-mutant cancers, including NSCLC25,33.
BRAF testing
Guidelines recommend that all patients with advanced non-squamous NSCLC undergo broad-based molecular testing to identify molecular drivers—including but not limited to BRAFV600 mutations21,22. Recommended and approved molecular testing assays include polymerase chain reaction (PCR) and next-generation sequencing (NGS)39,40,41. PCR offers rapid turn-around, reproducibility, specificity, sensitivity, and lower costs, but it is a single-gene assay typically limited to detection of V600E mutation39. Panel-based NGS has gained popularity for the ability to simultaneously test multiple genes, including BRAF, for both V600E and non-V600E mutations, which is more cost-effective than sequential single-gene assays and uses relatively little tumor tissue39,40. Availability of sufficient tumor tissue is a major constraint when testing for the numerous actionable mutations in NSCLC, so approaches that conserve tissue while providing a full molecular profile are being evaluated42. Liquid biopsy, a noninvasive and more rapid alternative to tissue biopsies that collects blood-based biomarkers—including circulating tumor DNA (ctDNA), can be used to detect genomic alterations5,43. Immunohistochemistry (IHC) is a highly sensitive and specific diagnostic test that uses the monoclonal antibody VE1 to detect BRAFV600E-mutant proteins39,44. While there are no current standard recommendations for IHC in BRAFV600E mutation detection, guideline recommendations for other oncogenes suggest that IHC be confirmed with a molecular test22,39. BRAF testing rates lag behind other driver oncogene testing rates, likely due to limited tissue availability and the fact that other actionable biomarkers (e.g., EGFR, ALK, PD-L1) are prioritized for testing when a sequential selective approach is used45. Given the demonstrated efficacy of BRAFV600E inhibitors in NSCLC, there is a need to improve the rate of BRAF testing so the results can be applied to clinical decision-making.
Treatment landscape
BRAF and MEK inhibitors in solid tumors
The identification of BRAF mutations, especially V600E, and their role in cancer led to the development of highly-selective BRAF inhibitors such as vemurafenib, dabrafenib, and encorafenib (Figs. 1 and 2) 46,47,48. These small-molecule inhibitors preferentially bind to the active conformation of BRAF kinase; through competitive occupation of the ATP binding pocket, the drugs stabilize the active conformation, resulting in potent inhibition of BRAFV600 47,48,49. Both vemurafenib and dabrafenib have confirmed activity against V600E, V600K, V600R, and V600D BRAF mutations 50,51,52. Encorafenib has confirmed activity against BRAFV600E and BRAFV600K mutants and BRAFWT 48,49.
Positive data readouts for BRAF-mutant NSCLC (blue) and approved treatments for BRAFV600E-mutant NSCLC (green) are shown. aBRAF inhibitors. bMEK inhibitors. cIn 2022, dabrafenib plus trametinib was approved for patients with unresectable metastatic BRAFV600E-mutant solid tumors who progressed on previous treatments and have no acceptable alternative option. dImmunotherapy that targets PD-1. eImmunotherapy that targets PD-L1.
BRAF inhibitor monotherapy has had varying degrees of efficacy in solid tumors53,54,55. In patients with BRAFV600E-mutant metastatic melanoma, single-agent vemurafenib was associated with a relative reduction of 63% in the risk of death and 74% in the risk of tumor progression compared with dacarbazine; median progression-free survival (PFS) was 5.3 months with vemurafenib (n = 275) and 1.6 months with dacarbazine (n = 274)53. With single-agent dabrafenib, patients with BRAFV600E-mutant metastatic melanoma (n = 76) had an objective response rate (ORR) of 59%, median PFS of 6.3 months, and median overall survival (OS) of 13.1 months56. In the dose expansion phase of a single-agent encorafenib study in patients with BRAFV600-mutant melanoma, ORR was 60.0%, median PFS was 12.4 months (95% CI, 7.4–not estimable [NE]), and median OS was NE for BRAF inhibitor-naive patients (n = 15); corresponding data for BRAF inhibitor-pretreated patients (n = 18) were 22.2%, 1.9 months (95% CI, 0.9–3.7), and 9.07 months (95% CI, 3.68–10.84)57.
A basket study evaluated vemurafenib monotherapy in patients with nonmelanoma BRAFV600-mutant cancers55. NSCLC and CRC cohorts had ORRs of 42% (95% CI, 20–67%) and 0%, respectively (Table 1). The poor clinical activity of BRAF inhibitor monotherapy in patients with CRC was consistent in additional vemurafenib (5% partial response [PR]; n = 21), dabrafenib (11% PR; n = 9), and encorafenib studies (0% PR; n = 18)54,58,59. In patients with BRAFV600-mutant CRC, addition of cetuximab, an anti-EGFR-antibody, improved ORR with vemurafenib (4%; n = 27) and encorafenib (19.5%; n = 220)55,60.
While BRAF inhibitor monotherapy is initially effective, acquired resistance enables reactivation of the MAPK pathway, limiting the clinical utility of monotherapy14,61. In addition, BRAF monomer inhibitors can cause paradoxical activation of the MAPK pathway in BRAFWT cells, which has been associated with hyperproliferative cutaneous events, including squamous cell carcinoma (SCC) and keratoacanthoma12,13,14,57. BRAF monomer inhibitors were combined with downstream MEK inhibitors to overcome resistance and paradoxical activation of the MAPK pathway, which increased efficacy and tolerability, resulting in several combination therapies being approved for unresectable metastatic BRAFV600-mutant melanoma (e.g., dabrafenib plus trametinib, vemurafenib plus cobimetinib, encorafenib plus binimetinib)14,62,63,64. The FDA granted accelerated approval of dabrafenib plus trametinib treatment for previously treated unresectable or metastatic solid tumors with the BRAFV600E protein in patients with no alternative treatment options65. This approval was supported by the ROAR study, which enrolled 206 patients into eight cohorts, each a different BRAFV600E-mutant rare cancer. ORR ranged from 0% for gastrointestinal stromal tumor (n = 1) to 89% for hairy cell leukemia (n = 55); ORR was ≥33% for the remaining cohorts.
The safety profile of BRAF inhibitor monotherapy was similar across solid tumors; common adverse events (AEs) included arthralgia, fatigue, rash, cutaneous events (e.g., SCC, keratoacanthoma), and gastrointestinal issues (e.g., diarrhea, nausea)10,48,53,54,57,62,64,66. Drug-specific AEs include photosensitivity with vemurafenib, pyrexia with dabrafenib, and reduced incidences of SCC and keratoacanthoma with encorafenib. Adding a MEK inhibitor resulted in a few key differences in the safety profiles62,64: pyrexia was more frequent with dabrafenib plus trametinib versus dabrafenib monotherapy15,62 and hyperproliferative cutaneous events were less common with dabrafenib plus trametinib and encorafenib plus binimetinib15,62,64.
BRAF and MEK inhibitors in metastatic NSCLC
Clinical trials with BRAF inhibitor monotherapy in patients with BRAFV600-mutant NSCLC are summarized in Table 110,11,55,66. In several trials, vemurafenib monotherapy was an effective treatment for treatment-naive (ORR: 37.5%; median PFS: 12.9 months) and previously treated patients (ORR: 37.0–44.8%; median PFS: 5.2–6.1 months) with BRAFV600-mutant NSCLC11,66. In one study, serious AEs occurred in 63% of patients, most commonly cutaneous SCC (15%) and keratoacanthoma (15%)66. Dabrafenib monotherapy was effective for previously treated patients (ORR: 33%; median PFS: 5.5 months) with BRAFV600E-mutant metastatic NSCLC; however, data were limited for treatment-naive patients because of a decision to prioritize the combination with trametinib with the expectation of improved response rates10. Pyrexia was the most common any-grade AE (36%), including grade 3 occurrences in 2% of patients. Pyrexia led to dose interruption or reduction in 11% and 4% of patients, respectively. Serious AEs occurred in 42% of patients, including pyrexia in 6% of patients.
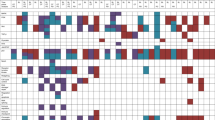
The combination of BRAF and MEK inhibitors demonstrated synergistic anti-tumor activity with a manageable safety profile (Table 1)14,15,16,18. The multicenter, non-randomized, open-label, phase 2 trial evaluated dabrafenib plus trametinib in patients with BRAFV600E-mutant metastatic NSCLC15,16,17. At the initial data analysis with a median follow-up of 15.9 months, for treatment-naive patients (n = 36), ORR by investigator was 64% (95% CI, 46–79%), median duration of response (DOR) was 10.4 months (95% CI, 8.3–17.9), median PFS was 10.9 months (95% CI, 7.0–16.6), and median OS was 24.6 months (95% CI, 12.3–NR)16. The most common AEs included pyrexia (64%), nausea (56%), and diarrhea (36%); grade 3–4 AEs occurred in 69% of patients, including pyrexia (11%) (Fig. 3a). For previously treated patients (n = 57), with a median follow-up of 11.6 months, ORR by investigator was 63.2% (95% CI, 49.3–75.6%), median DOR was 9.0 months (95% CI, 6.9–18.3), median PFS was 9.7 months (95% CI, 6.9–19.6), and median OS was immature15. The most common AEs included pyrexia (46%), nausea (40%), and vomiting (35%); grade 3–4 AEs occurred in 49% of patients, including pyrexia (2%) (Fig. 3a). At the 5-year follow-up analysis, median PFS and OS were 10.8 months (95% CI, 7.0–14.5) and 17.3 months (95% CI, 12.3–40.2) for treatment-naive patients and 10.2 months (95% CI, 6.9–16.7) and 18.2 months (95% CI, 14.3–28.6) for previously treated patients, respectively17. The most common AE remained pyrexia (56%), and grade 3–4 AEs occurred in 66% of patients with most manageable with dose modifications. Pyrexia led to dose reduction in 11 patients (12%) and permanent treatment discontinuation in two patients (2%). The addition of the MEK inhibitor was associated with lower incidence of cutaneous SCC compared with BRAF inhibitor monotherapy (4% versus 12%)10,15. Based on these data, the FDA and European Medicines Agency approved dabrafenib plus trametinib combination for treatment of patients with BRAFV600E-mutant metastatic NSCLC67,68. A later retrospective analysis supported the use of dabrafenib plus trametinib, where the risk of death for treatment-naive patients with BRAF-mutant advanced NSCLC was significantly lower with dabrafenib plus trametinib versus platinum-based chemotherapy (HR = 0.51; 95% CI, 0.29–0.92; P = 0.03), and median OS was 17.3 months (95% CI, 14.6–NR) versus 9.7 months (95% CI, 6.4–19.6), respectively68.
a Adverse events (AEs) shown for dabrafenib plus trametinib occurred in at least 10% of patients in combined data from interim analysis of treatment-naive and previously treated patients15,16. AEs led to dose reduction, dose interruption, and permanent treatment discontinuation in 37%, 67%, and 16% of patients. aChest pain includes musculoskeletal chest pain. b Treatment-related AEs (TRAEs) shown for encorafenib plus binimetinib occurred in at least 10% of patients18. TRAEs led to dose reduction, dose interruption, and permanent treatment discontinuation in 24%, 44%, and 15% of patients. Comparisons of safety profiles should be done cautiously since data are from different trials and reported as all-causality AEs for one treatment combination and as TRAEs for the other combination. ALP alkaline phosphatase, ALT alanine aminotransferase, AST aspartate aminotransferase, CNS central nervous system, CPK creatine phosphokinase.
The combination of encorafenib plus binimetinib is being investigated in ongoing phase 2 trials in patients with BRAFV600E-mutant NSCLC5,18,19. PHAROS, a single-arm, open-label, multicenter trial (NCT03915951), enrolled 98 patients with BRAFV600E-mutant metastatic NSCLC (n = 59 treatment-naive, n = 39 previously treated)18. In treatment-naive patients, with a median follow-up for PFS by independent radiology review (IRR) of 18.2 months (95% CI, 16.4–22.3), ORR assessed by IRR was 75% (95% CI, 62–85%), median DOR by IRR was NE (95% CI, 23.1–NE), and median PFS by IRR was NE (95% CI, 15.7–NE). In previously treated patients, with a median follow-up for PFS by IRR of 12.8 months (95% CI, 9.0–19.8), ORR by IRR was 46% (95% CI, 30–63%), median DOR by IRR was 16.7 months (95% CI, 7.4–NE), and median PFS by IRR was 9.3 months (95% CI, 6.2–NE). OS was NE in both groups. The most frequently reported treatment-related AEs (TRAEs) were nausea (50%), diarrhea (43%), fatigue (32%), and vomiting (29%); serious TRAEs occurred in 14% of patients with the most common being colitis (3%) (Fig. 3b). All-causality pyrexia occurred in 22% of patients, and treatment-related pyrexia led to one dose interruption and no dose reductions or permanent discontinuations. The ENCO-BRAF trial (NCT04526782) includes treatment-naive and previously treated cohorts, with an estimated enrollment of 119 patients to conclude in 202619. Encorafenib plus binimetinib combination treatment was recently approved by the FDA for patients with BRAFV600E-mutant metastatic NSCLC based on the PHAROS trial20.
Primary and acquired drug resistance to BRAF-targeted therapy
Baseline concurrent mutations prior to receipt of targeted therapy have been identified in 22–30% of patients with BRAFV600E-mutant NSCLC and may be a cause of primary resistance17,61,69. Common concurrent mutations included alterations in the TP53 and SETD2 genes and the PI3K (e.g., PIK3CA E545K, PTEN R14K) and MAPK (e.g., KRAS G12C) pathways17,18,61,69. The incidence of concurrent TP53 or RAS gene family mutations was higher with BRAF class II or III mutations than class I mutations31,33,70. In several studies, the presence of a concurrent mutation in TP53, PIK3CA, KRAS, or PTEN was associated with poorer outcomes17,61,69. In a study evaluating dabrafenib plus trametinib for BRAFV600E-mutant metastatic NSCLC, patients with a concurrent mutation in the PI3K pathway (n = 4) had a median OS of 5.4 months compared with 22.7 months in patients without an identified concurrent mutation (n = 34)17. In the PHAROS trial, which evaluated encorafenib plus binimetinib for BRAFV600E-mutant metastatic NSCLC, concurrent mutations were identified, with the most common being SETD2 and TP53 (43%, each); however, there was no association between concurrent mutations and outcome18. As most of this data comes from studies with small numbers of patients, further research is necessary to understand the impact of concurrent mutations in patients with BRAFV600E-mutant NSCLC17,18,69.
The mechanisms of acquired resistance to BRAF inhibitors, alone or combined with MEK inhibitors, are poorly understood, and there is no standardized sequential treatment strategy21,61. While data are limited, acquired resistance appears to occur through bypassing or reactivating the MAPK pathway14,61. Bypassing the MAPK pathway and activating a parallel pathway (e.g., PI3K/AKT) can lead to disease progression. A PTEN frameshift mutation that could potentially activate the PI3K pathway was identified in a patient with BRAFV600E-mutant NSCLC that progressed on dabrafenib71. In preclinical BRAFV600E-mutant lung cancer models, the presence of a cooperating mutation silencing RBMS3, a regulator of the WNT pathway, promoted resistance to dabrafenib plus trametinib72.
Reactivation of the MAPK pathway can occur in BRAF-dependent or -independent manners. Resistance to targeted therapies often occurs due to secondary mutations or epigenetic changes in the target gene, and an aberrant splice variant of BRAF was identified in BRAFV600E NSCLC cells that acquired resistance73,74. However, secondary BRAF mutations may be rare, as none were discovered in several resistance studies with BRAF-mutant NSCLC and melanoma61,73,75. BRAF-independent reactivation of the MAPK pathway includes alterations either upstream or downstream of BRAF14. Mutations in RAS (NRAS, KRAS) were discovered in a few studies61,71. Strong evidence came from a study that compared ctDNA sequencing at diagnosis and disease progression for 35 patients with BRAF-mutant NSCLC who progressed on either BRAF inhibitor monotherapy or dabrafenib plus trametinib61. RAS mutations (KRAS G12V; KRAS Q61R; NRAS Q61R) were present at disease progression and not diagnosis, which suggests mutation occurred during treatment. Resistance studies of patients with BRAFV600E-mutant melanoma suggested that upregulation of RAS or overexpression of ARAF and CRAF could alleviate BRAF-dependence in tumor cells73,75. Downstream mutations in MEK1 were also identified in patients with BRAFV600E-mutant NSCLC that progressed on dabrafenib plus trametinib71. Further understanding of acquired resistance mechanisms is critical to inform optimal sequencing and providing insight for evaluation of combination approaches or next-generation target therapies.
Immunotherapy
Compared with studies with BRAF and MEK inhibitors, data concerning efficacy and safety of immunotherapy in patients with BRAFV600E-mutant NSCLC are limited; studies have not prospectively enrolled patients with BRAFV600 mutations, and immunotherapy is not specifically approved for patients with this mutation76,77,78,79. Evidence for efficacy of immunotherapy is derived from conflicting, small, retrospective studies (Table 2)23,24,77. In a multi-cohort retrospective study of immunotherapy in patients with oncogene-driven advanced lung cancer, patients (n = 10) with BRAF-mutant NSCLC in one cohort had a significantly longer median PFS (7.4 months) than patients with other common oncogene drivers (versus KRAS 2.8 months; HR 0.36, 95% CI, 0.14–0.88; P = 0.026)24. In the other cohort, PFS was longer in patients with V600E mutations (n = 30; 9.8 months) versus non-V600E mutations (n = 35; 5.4 months). However, in another retrospective study, similar PFS (2.1–3.4 months) was reported across oncogenes with immunotherapy77. In that study, two trends emerged in the BRAF cohort (n = 43). PFS was longer in patients who previously or currently smoked (4.1 months) versus had never smoked (1.9 months) and with non-V600E mutations (4.1 months) versus V600E mutations (1.8 months). According to guidelines of the European Society for Medical Oncology, patients with BRAFV600-mutant metastatic NSCLC that progresses on BRAF plus MEK inhibitor should receive immunotherapy with optional chemotherapy (in patients with smoking history) or chemotherapy with optional immunotherapy (in patients without smoking history)22.
Chemotherapy
Prior to the development of targeted therapy for BRAFV600E-mutant metastatic NSCLC, platinum-based chemotherapy was the standard of care68,78. However, retrospective studies reported that patients with BRAFV600E-mutant NSCLC had poorer outcomes with platinum-based chemotherapy than those with BRAFWT NSCLC (Table 2)6,32. While those retrospective studies also reported a shorter PFS in patients with V600E mutations (4.1–5.2 months) versus non-V600E mutations (6.4–8.9 months), another retrospective study reported that carboplatin-pemetrexed in patients with treatment-naive BRAF-mutant metastatic NSCLC resulted in longer PFS in patients with class I mutations (6.2 months) versus class II or III mutations (3.3 months and 4.9 months, respectively)33. Additionally, in a multi-institutional prospective lung cancer screening project, median PFS with platinum-containing chemotherapy was longer in patients with class I mutations (11.5 months) than in those with class III mutations (5.3 months)31. Several trials demonstrated that BRAF monotherapy or BRAF plus MEK inhibitor therapy was effective in patients who had progressed on chemotherapy10,15,18,66. Chemotherapy remains a second-line recommendation for patients with a BRAFV600 mutation21,22.
Immunochemotherapy
The combination of immunotherapy and chemotherapy is approved for first-line treatment of patients with metastatic NSCLC but not specifically for patients with BRAFV600E mutations80. In a phase 3 trial of treatment-naive patients with metastatic non-squamous NSCLC, the combination of pembrolizumab, pemetrexed, and a platinum resulted in significantly longer median PFS compared with chemotherapy alone (8.8 versus 4.9 months; HR = 0.52; P < 0.001)81. In a small retrospective study in China, immunotherapy plus chemotherapy (n = 9) in treatment-naive patients with BRAFV600E-mutant advanced NSCLC resulted in a significantly longer median PFS compared with chemotherapy or targeted therapy (n = 20; 18.5 versus 4.1 months; P = 0.0098)82. This efficacy benefit with immunochemotherapy was not observed in later lines. Another retrospective study showed similar efficacy with immunotherapy-based treatments in patients with advanced NSCLC with or without BRAF mutations; median PFS was 8.4 months in both patient populations83. In the BRAF cohort, median PFS was similar for V600E and non-600E mutations (10.0 versus 8.0 months). Median PFS was longer in the first line than in subsequent treatment lines in patients with WT (12.8 versus 5.6 months) and BRAF-mutant (11.2 versus 4.0 months) NSCLC. These studies suggest that immunotherapy-based treatments are an option for patients with BRAFV600E-mutant advanced NSCLC82,83.
Emerging treatments and approaches
Immunotherapy plus targeted therapy combinations
The combination of BRAF-targeted therapy plus immunotherapy may produce a synergistic anti-tumor effect; tolerability of the combined approach will be a key consideration14. Studies have investigated various combinations of anti-PD-1/PD-L1 with BRAF and/or MEK inhibitors and reported positive outcomes in solid tumors, including BRAFV600E/K-mutant melanoma, CRC, and BRAFV600E-mutant NSCLC84,85,86,87. In a phase 1/1b, global, multicenter, open-label study, cobimetinib and atezolizumab (anti-PD-L1) were evaluated in immunotherapy-naive patients with advanced solid tumors (n = 150); patients had received a median of 5.0 prior systemic therapies, and 15% had BRAF mutations84. In patients with metastatic CRC (n = 84), ORR was 8% (95% CI, 3–16%), median PFS was 1.9 months (95% CI, 1.8–2.3), and median OS was 9.8 months (95% CI, 6.2–14.1). In patients with melanoma (n = 22), ORR was 41% (95% CI, 21–64%), median PFS was 13.3 months (95% CI, 2.8–NE), and median OS was NE (95% CI, 18.7–NE). In patients with NSCLC (n = 28), ORR was 18% (95% CI, 6–37%), median PFS was 5.8 months (95% CI, 2.7–9.2), and median OS was 13.2 months (95% CI, 9.2–NE). In the safety analysis (n = 150), the most common TRAEs were diarrhea (67%), rash (48%), and fatigue (40%); 44% of patients reported grade 3–4 TRAEs. Another trial (NCT03991819) is evaluating the combination of binimetinib and pembrolizumab in patients with EGFR WT, ALK-rearrangement–negative advanced or metastatic NSCLC with PD-L1 tumor proportion score (TPS) ≥ 50%; initial results reported that 33% of nine evaluable patients had a partial response, including one patient with BRAFV600E-mutant metastatic NSCLC85,86.
Trials have investigated the efficacy and safety of triple combination therapies for BRAF-mutant melanomas87,88,89. A phase 2, randomized trial enrolled patients with treatment-naive advanced melanoma with a V600E or V600K mutation to receive dabrafenib plus trametinib with or without pembrolizumab (triplet, n = 60; doublet, n = 60)88. When compared with the doublet therapy, triplet therapy resulted in longer median PFS (10.7 versus 16.9 months) and higher incidence of grade ≥3 TRAEs (25.0% versus 58.3%). Grade ≥3 AEs occurred in 70% of patients in the triplet arm and 45% of patients in the doublet arm. Immune-mediated AEs occurred in 15% and 52% of patients in the doublet and triplet treatment arms, respectively; pneumonitis (17%) and hypothyroidism (8%) were the most common immune-mediated AEs reported with triplet therapy. An open-label, phase 1/2 trial combined encorafenib plus binimetinib with pembrolizumab for patients with BRAFV600-mutant advanced melanoma (n = 15); ORR was 64% (95% CI, 35–87%), and 12-month PFS was 41% (95% CI, 13–68%)87. TRAEs were reported by 87% of patients; grade ≥3 TRAEs were reported in 53% of patients, with increases in aspartate aminotransferases, gamma glutamyl transferase, and creatine phosphokinase being the most common. A meta-analysis of triplet therapies compared with doublet therapy or monotherapy for melanoma revealed that triplet therapy significantly improved PFS and OS but was associated with increased frequency of immune-related AEs, including hypothyroidism, arthralgia, myalgia, alanine aminotransferase elevations, aspartate aminotransferase elevations, asthenia, and pyrexia90. Triplet therapy did not increase the overall incidence of AEs or grade ≥3 AEs. The increased incidence of AEs should be considered when determining the optimal combination of immunotherapy and targeted therapy88,90.
Next-generation BRAF inhibitors
Next-generation BRAF inhibitors target dimerization since it is an essential component of activation for WT and many mutant BRAF kinases, plays a role in resistance mechanisms to BRAF inhibitors, and is associated with AEs91. These drugs were developed following two main strategies aimed at inhibiting mutant RAF while preventing paradoxical activation and common acquired resistance mechanisms92. Type II pan-RAF inhibitors bind the active conformation of RAF monomers and dimers92,93. Despite the name of pan-RAF, at least three of these agents (naporafenib [LXH254], tovorafenib [TAK-580], belvarafenib) demonstrated poor inhibition of ARAF and potent inhibition of WT and mutant versions of CRAF and BRAF93. Paradox breakers (e.g., PLX8394, PLX7904) are more specific BRAF inhibitors that alter the dimer interface and subsequently prevent BRAF-homodimer and BRAF:CRAF heterodimer formations92,94. Data from preclinical and clinical studies suggest that BRAF non-V600 mutations could be targeted with these new inhibitors, and several are being investigated in ongoing trials to better define their efficacy and safety (Table 3)34,95,96.
Unmet needs
Brain metastases
Brain metastases (BMs), a common (26% at diagnosis) challenge for patients with metastatic NSCLC, are associated with poor prognosis and quality of life97,98. One study reported that the incidence of baseline BMs in patients with BRAF-mutant metastatic NSCLC was significantly lower for class I mutations (9%) than for class II (29%; P = 0.011) or class III (31%; P = 0.007) mutations33. However, this subset of patients has been predominantly excluded from trials of targeted therapies15,16,18. In a trial evaluating vemurafenib in patients with BRAF-mutant advanced NSCLC, median PFS was 1.9 months (95% CI, 1.5–3.9) and 5.4 months (95% CI, 3.8–7.2) in patients with (n = 26) and without (n = 89) baseline BMs11. In patients enrolled in PHAROS with BRAFV600E-mutant metastatic NSCLC asymptomatic BMs, ORR was 100% (95% CI, 39.8–100.0%) for treatment-naive patients (n = 4) and 0% for previously treated patients (n = 4)18. Better understanding of the epidemiology, risk, impact, and treatment of BMs in patients with BRAF-mutant metastatic NSCLC remains an unmet need.
More robust efficacy analysis of patients with BMs has been conducted for BRAF-mutant metastatic melanoma treated with BRAF/MEK inhibitors. In a phase 3 study of patients with BRAFV600-mutant unresectable or metastatic melanoma with BMs (n = 275), systemic outcomes with dabrafenib plus trametinib were ORR of 41.5% and median PFS of 5.68 months (95% CI, 5.29–6.87)99. Treatment-naive patients had a significantly longer median PFS than previously treated patients (7.23 versus 4.96 months; P = 0.0061). An open-label, multi-cohort, phase 2 study evaluated the efficacy of dabrafenib plus trametinib in patients with BRAFV600-mutant melanoma with BMs (n = 125), including the largest cohort (n = 76) with asymptomatic BRAFV600E-mutant BMs and no prior brain-directed therapy100. For the largest cohort, intracranial response rate (IC ORR) was 58% (95% CI, 46–69%), median PFS was 5.6 months (95% CI, 5.3–7.4), and median OS was 10.8 months (95% CI, 8.7–19.6). The safety profile was consistent with those in previous dabrafenib plus trametinib studies. In a multicenter, retrospective case series investigation, encorafenib plus binimetinib combination treatment of 24 patients with BRAF-mutant metastatic melanoma BMs resulted in IC ORR of 33% and ORR of 21%101. The safety profile was consistent with what was reported in patients with melanoma without BMs.
Conclusion
BRAFV600E is an actionable mutation for metastatic NSCLC with safe and effective treatment options8,16,18. BRAF and MEK inhibitor combination therapies have demonstrated rapid and durable responses in the majority of patients15,16,18. The safety profiles of these combinations are well described, and appropriate therapy management principles should be employed for responding patients. Disease progression is inevitable, as only ~50% of patients with metastatic NSCLC receive a second-line treatment102,103. Therefore, it is prudent to use the most efficacious agents in the first-line setting. Further studies are necessary to determine optimal sequencing methods, understand resistance mechanisms, determine efficacy of treatments for BMs, and develop targeted therapies for non-V600E mutations.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
No datasets were generated or analyzed for this article. Data referenced in this review can be accessed by following resources numbered in the References section.
References
Nguyen-Ngoc, T., Bouchaab, H., Adjei, A. A. & Peters, S. BRAF alterations as therapeutic targets in non-small-cell lung cancer. J. Thorac. Oncol. 10, 1396–1403 (2015).
Owsley, J. et al. Prevalence of class I-III BRAF mutations among 114,662 cancer patients in a large genomic database. Exp. Biol. Med. 246, 31–39 (2021).
Davies, H. et al. Mutations of the BRAF gene in human cancer. Nature 417, 949–954 (2002).
Wan, P. T. C. et al. Mechanism of activation of the RAF-ERK signaling pathway by oncogenic mutations of B-RAF. Cell 116, 855–867 (2004).
Abdayem, P. A. & Planchard, D. Ongoing progress in BRAF-mutated non-small cell lung cancer. Clin. Adv. Hematol. Oncol. 20, 662–672 (2022).
Cardarella, S. et al. Clinical, pathologic, and biologic features associated with BRAF mutations in non-small cell lung cancer. Clin. Cancer Res. 19, 4532–4540 (2013).
Sheikine, Y. et al. BRAF in lung cancers: analysis of patient cases reveals recurrent BRAF mutations, fusions, kinase duplications, and concurrent alterations. JCO Precis. Oncol. 2, PO.17.00172 (2018).
Baik, C. S., Myall, N. J. & Wakelee, H. A. Targeting BRAF-mutant non-small cell lung cancer: from molecular profiling to rationally designed therapy. Oncologist 22, 786–796 (2017).
Barlesi, F. et al. Routine molecular profiling of cancer: results of a one-year nationwide program at the French Cooperative Thoracic Intergroup (IFCT) for advanced non-small cell lung cancer (NSCLC) patients. Lancet 387, 1415–1426 (2016).
Planchard, D. et al. Dabrafenib in patients with BRAF(V600E)-positive advanced non-small-cell lung cancer: a single-arm, multicentre, open-label, phase 2 trial. Lancet Oncol. 17, 642–650 (2016).
Mazieres, J. et al. Vemurafenib in non-small-cell lung cancer patients with BRAFV600 and BRAFnonV600 mutations. Ann. Oncol. 31, 289–294 (2020).
Poulikakos, P. I., Zhang, C., Bollag, G., Shokat, K. M. & Rosen, N. RAF inhibitors transactivate RAF dimers and ERK signalling in cells with wild-type BRAF. Nature 464, 427–430 (2010).
Hatzivassiliou, G. et al. RAF inhibitors prime wild-type RAF to activate the MAPK pathway and enhance growth. Nature 464, 431–435 (2010).
Subbiah, V., Baik, C. & Kirkwood, J. M. Clinical development of BRAF plus MEK inhibitor combinations. Trends Cancer 6, 797–810 (2020).
Planchard, D. et al. Dabrafenib plus trametinib in patients with previously treated BRAFV600E-mutant metastatic non-small cell lung cancer: an open-label, multicentre phase 2 trial. Lancet Oncol. 17, 984–993 (2016).
Planchard, D. et al. Dabrafenib plus trametinib in patients with previously untreated BRAFV600E-mutant metastatic non-small-cell lung cancer: an open-label, phase 2 trial. Lancet Oncol. 18, 1307–1316 (2017).
Planchard, D. et al. Phase 2 study of dabrafenib plus trametinib in patients with BRAF V600E-mutant metastatic NSCLC: updated 5-year survival rates and genomic analysis. J. Thorac. Oncol. 17, 103–115 (2022).
Riely, G. J. et al. Phase II, open-label study of encorafenib plus binimetinib in patients with BRAFV600-mutant metastatic non-small-cell lung cancer. J. Clin. Oncol. 14, 3700–3711 (2023).
Intergroupe Francophone de Cancerlogie Thoracique. ENCOrafenib with Binimetinib in bRAF NSCLC. https://classic.clinicaltrials.gov/ct2/show/NCT04526782 (2020).
US Food and Drug Administration. FDA Approves Encorafenib with Binimetinib for Metastatic Non-small Cell Lung Cancer with a BRAF V600E Mutation. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-encorafenib-binimetinib-metastatic-non-small-cell-lung-cancer-braf-v600e-mutation (2023).
Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Non-Small Cell Lung Cancer V.5.2023. © National Comprehensive Cancer Network, Inc. 2023. All rights reserved. Accessed [November 29, 2023]. To view the most recent complete version of the guideline, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way. NCCN, National Comprehensive Cancer Network® (NCCN®).
Hendriks, L. E. et al. Oncogene-addicted metastatic non-small-cell lung cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up. Ann. Oncol. 34, 339–357 (2023).
Guisier, F. et al. Efficacy and safety of anti-PD-1 immunotherapy in patients with advanced NSCLC with BRAF, HER2, or MET mutations or RET translocation translocation: GFPC 01-2018: GFPC. J. Thorac. Oncol. 15, 628–636 (2020).
Negrao, M. V. et al. Oncogene-specific differences in tumor mutational burden, PD-L1 expression, and outcomes from immunotherapy in non-small cell lung cancer. Immunother. Cancer https://doi.org/10.1136/jitc-2021-002891 (2021).
Yaeger, R. & Corcoran, R. B. Targeting alterations in the RAF-MEK pathway. Cancer Discov. 9, 329–341 (2019).
Marchetti, A. et al. Clinical features and outcome of patients with non-small-cell lung cancer harboring BRAF mutations. J. Clin. Oncol. 29, 3574–3579 (2011).
Kinno, T. et al. Clinicopathological features of nonsmall cell lung carcinomas with BRAF mutations. Ann. Oncol. 25, 138–142 (2014).
Villaruz, L. C. et al. Clinicopathologic features and outcomes of patients with lung adenocarcinomas harboring BRAF mutations in the Lung Cancer Mutation Consortium. Cancer 121, 448–456 (2015).
Wolf, J. et al. Capmatinib in MET exon 14-mutated or MET-amplified non-small-cell lung cancer. N. Engl. J. Med. 383, 944–957 (2020).
Di Federico, A. et al. Genomic landscape, clinical features and outcomes of non-small cell lung cancer patients harboring BRAF alterations of distinct functional classes. Cancers (Basel) 14, 3472 (2022).
Sakai, T. et al. Clinicogenomic features and targetable mutations in NSCLCs harboring BRAF non-V600E mutations: a multi-institutional genomic screening study (LC-SCRUM-Asia). J. Thorac. Oncol. 18, 1538–1549 (2023).
Ding, X. et al. Clinicopathologic characteristics and outcomes of Chinese patients with non-small-cell lung cancer and BRAF mutation. Cancer Med. 6, 555–562 (2017).
Dagogo-Jack, I. et al. Impact of BRAF mutation class on disease characteristics and clinical outcomes in BRAF-mutant lung cancer. Clin. Cancer Res. 25, 158–165 (2019).
Negrao, M. V. et al. Molecular landscape of BRAF-mutant NSCLC reveals an association between clonality and driver mutations and identifies targetable non-V600 driver mutations. J. Thorac. Oncol. 15, 1611–1623 (2020).
Bracht, J. W. P. et al. BRAF mutations classes I, II, and III in NSCLC patients included in the SLLIP trial: the need for a new pre-clinical treatment rationale. Cancers (Basel) https://doi.org/10.3390/cancers11091381 (2019).
Smiech, M., Leszczynski, P., Kono, H., Wardell, C. & Taniguchi, H. Emerging BRAF mutations in cancer progression and their possible effects on transcriptional networks. Genes (Basel) https://doi.org/10.3390/genes11111342 (2020).
Roviello, G. et al. Advances in anti-BRAF therapies for lung cancer. Invest. New Drugs 39, 879–890 (2021).
Yao, Z. et al. Tumours with class 3 BRAF mutants are sensitive to the inhibition of activated RAS. Nature 548, 234–238 (2017).
Sholl, L., Cooper, W. A., Kerr, K., Tan D. S. W. & Tsao, M. S. (eds) IASLC Atlas of Molecular Testing for Targeted Therapy in Lung Cancer (International Association for the Study of Lung Cancer, 2023).
Lokhandwala, P. M. et al. Clinical mutational profiling and categorization of BRAF mutations in melanomas using next generation sequencing. BMC Cancer 19, 665 (2019).
Odogwu, L. et al. FDA Approval summary: dabrafenib and trametinib for the treatment of metastatic non‐small cell lung cancers harboring BRAF V600E mutations. Oncologist 23, 740–745 (2018).
Penault-Llorca, F. et al. Expert opinion on NSCLC small specimen biomarker testing - part 1: tissue collection and management. Virchows Arch. 481, 335–350 (2022).
Ilie, M. et al. Current challenges for detection of circulating tumor cells and cell-free circulating nucleic acids, and their characterization in non-small cell lung carcinoma patients. What is the best blood substrate for personalized medicine? Ann. Transl. Med. 2, 107 (2014).
Gow, C. H., Hsieh, M. S., Lin, Y. T., Liu, Y. N. & Shih, J. Y. Validation of immunohistochemistry for the detection of BRAF V600E-mutated lung adenocarcinomas. Cancers (Basel) https://doi.org/10.3390/cancers11060866 (2019).
Waterhouse, D. M., Tseng, W. Y., Espirito, J. L. & Robert, N. J. Understanding contemporary molecular biomarker testing rates and trends for metastatic NSCLC among community oncologists. Clin. Lung Cancer 22, e901–e910 (2021).
Luke, J. J. & Hodi, F. S. Vemurafenib and BRAF inhibition: a new class of treatment for metastatic melanoma. Clin. Cancer Res. 18, 9–14 (2012).
Rheault, T. R. et al. Discovery of dabrafenib: a selective inhibitor of Raf kinases with antitumor activity against B-Raf-driven tumors. ACS Med. Chem. Lett. 4, 358–362 (2013).
Koelblinger, P., Thuerigen, O. & Dummer, R. Development of encorafenib for BRAF-mutated advanced melanoma. Curr. Opin. Oncol. 30, 125–133 (2018).
Proietti, I. et al. BRAF inhibitors: molecular targeting and immunomodulatory actions. Cancers (Basel) https://doi.org/10.3390/cancers12071823 (2020).
Yang, H. et al. RG7204 (PLX4032), a selective BRAFV600E inhibitor, displays potent antitumor activity in preclinical melanoma models. Cancer Res. 70, 5518–5527 (2010).
King, A. J. et al. Dabrafenib; preclinical characterization, increased efficacy when combined with trametinib, while BRAF/MEK tool combination reduced skin lesions. PLoS ONE 8, e67583 (2013).
Gentilcore, G. et al. Effect of dabrafenib on melanoma cell lines harbouring the BRAF V600/R mutations. BMC Cancer 13, 17 (2013).
Chapman, P. B. et al. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N. Engl. J. Med. 364, 2507–2516 (2011).
Kopetz, S. et al. Phase II pilot study of vemurafenib in patients with metastatic BRAF-mutated colorectal cancer. J. Clin. Oncol. 33, 4032–4038 (2015).
Hyman, D. M. et al. Vemurafenib in multiple nonmelanoma cancers with BRAF V600 mutations. N. Engl. J. Med. 373, 726–736 (2015).
Ascierto, P. A. et al. Phase II trial (BREAK-2) of the BRAF inhibitor dabrafenib (GSK2118436) in patients with metastatic melanoma. J. Clin. Oncol. 31, 3205–3211 (2013).
Delord, J. P. et al. Phase I dose-escalation and -expansion study of the BRAF inhibitor encorafenib (LGX818) in metastatic BRAF-mutant melanoma. Clin. Cancer Res. 23, 5339–5348 (2017).
Falchook, G. S. et al. Dabrafenib in patients with melanoma, untreated brain metastases, and other solid tumours: a phase 1 dose-escalation trial. Lancet 379, 1893–1901 (2012).
Gomez-Roca, C. A. et al. Encorafenib (Lgx818), an oral Braf inhibitor, in patients (Pts) with Braf V600E metastatic colorectal cancer (Mcrc): results of dose expansion in an open-label, phase 1 study. Ann. Oncol. https://doi.org/10.1093/annonc/mdu333.38 (2014).
Tabernero, J. et al. Encorafenib plus cetuximab as new standard of care for previously treated BRAF V600E-mutant metastatic colorectal cancer: updated survival results and subgroup analyses from the BEACON study. J. Clin. Oncol 39, 273–284 (2021).
Ortiz-Cuaran, S. et al. Circulating tumor DNA genomics reveals potential mechanisms of resistance to BRAF-targeted therapies in BRAF-mutant metastatic non-small cell lung cancer patients. Clin. Cancer Res. 26, 6242–6253 (2020).
Long, G. V. et al. Combined BRAF and MEK inhibition versus BRAF inhibition alone in melanoma. N. Engl. J. Med. 371, 1877–1888 (2014).
Ascierto, P. A. et al. 5-Year outcomes with cobimetinib plus vemurafenib in BRAFV600 mutation-positive advanced melanoma: extended follow-up of the coBRIM study. Clin. Cancer Res. 27, 5225–5235 (2021).
Dummer, R. et al. COLUMBUS 5-year update: a randomized, open-label, phase III trial of encorafenib plus binimetinib versus vemurafenib or encorafenib in patients with BRAF V600-mutant melanoma. J. Clin. Oncol. 40, 4178–4188 (2022).
Subbiah, V. et al. Dabrafenib plus trametinib in BRAFV600E-mutated rare cancers: the phase 2 ROAR trial. Nat. Med. 29, 1103–1112 (2023).
Subbiah, V. et al. Efficacy of vemurafenib in patients with non-small-cell lung cancer with BRAD V600 mutation: an open label, single-arm cohort of the histology-independent VE-BASKET study. JCO Precis. Oncol. 3, 18.00266 (2019).
Auliac, J.-B. et al. Efficacy of dabrafenib plus trametinib combination in patients with BRAF V600E-mutant NSCLC in real-world setting: GFPC 01-2019. Cancers https://doi.org/10.3390/cancers12123608 (2020).
Johnson, B. E. et al. Clinical outcomes with dabrafenib plus trametinib in a clinical trial versus real-world standard of care in patients with BRAF-mutated advanced NSCLC. JTO Clin. Res. Rep. https://doi.org/10.1016/j.jtocrr.2022.100324 (2022).
Qu, J. et al. Clinical characteristics, co-mutations, and treatment outcomes in advanced non-small-cell lung cancer patients with the BRAF-V600E mutation. Front. Oncol. 12, 911303 (2022).
Niu, J. et al. BRAF mutation classes and co-occurring mutations in NSCLC. J. Clin. Oncol. 40, 9083 (2022).
Facchinetti, F. et al. Molecular mechanisms of resistance to BRAF and MEK inhibitors in BRAFV600E non-small cell lung cancer. Eur. J. Cancer 132, 211–223 (2020).
Vaishnavi, A. et al. Transposon mutagenesis reveals RBMS3 silencing as a promoter of malignant progression of BRAFV600E-driven lung tumorigenesis. Cancer Res. 82, 4261–4273 (2022).
Villanueva, J., Vultur, A. & Herlyn, M. Resistance to BRAF inhibitors: unraveling mechanisms and future treatment options. Cancer Res 71, 7137–7140 (2011).
Lin, L. et al. Mapping the molecular determinants of BRAF oncogene dependence in human lung cancer. Proc. Natl. Acad. Sci. U.S.A. 111, E748–757 (2014).
Nazarian, R. et al. Melanomas acquire resistance to B-RAF(V600E) inhibition by RTK or N-RAS upregulation. Nature 468, 973–977 (2010).
Dudnik, E. et al. BRAF mutant lung cancer: programmed death ligand 1 expression, tumor mutational burden, microsatellite instability status, and response to immune check-point inhibitors. J. Thorac. Oncol. 13, 1128–1137 (2018).
Mazieres, J. et al. Immune checkpoint inhibitors for patients with advanced lung cancer and oncogenic driver alterations: results from the IMMUNOTARGET registry. Ann. Oncol. 30, 1321–1328 (2019).
Pai-Scherf, L. et al. FDA approval summary: pembrolizumab for treatment of metastatic non-small cell lung cancer: first-line therapy and beyond. Oncologist 22, 1392–1399 (2017).
Reck, M. et al. Pembrolizumab versus chemotherapy for PD-L1-positive non-small-cell lung cancer. N. Engl. J. Med. 375, 1823–1833 (2016).
Shields, M. D., Marin-Acevedo, J. A. & Pellini, B. Immunotherapy for advanced non-small cell lung cancer: a decade of progress. Am. Soc. Clin. Oncol. Educ. Book 41, 1–23 (2021).
Gandhi, L. et al. Pembrolizumab plus chemotherapy in metastatic non-small-cell lung cancer. N. Engl. J. Med. 378, 2078–2092 (2018).
Wang, H. et al. Efficacy of immune checkpoint inhibitors in advanced non-small cell lung cancer harboring BRAF mutations. Transl. Lung Cancer Res. 12, 219–229 (2023).
Li, H. et al. Tumor immune microenvironment and immunotherapy efficacy in BRAF mutation non-small-cell lung cancer. Cell Death Dis. 13, 1064 (2022).
Hellmann, M. D. et al. Phase Ib study of atezolizumab combined with cobimetinib in patients with solid tumors. Ann. Oncol. 30, 1134–1142 (2019).
University Health Network. Study of Binimetinib in Combination with Pembrolizumab in Advanced Non-small Cell Lung Cancer. https://www.clinicaltrials.gov/study/NCT03991819?cond=NSCLC&term=binimetinib%20pembrolizumab&rank=1 (2019).
Theriau, C. F. et al. Abstract CT206: a phase I study of binimetinib, a MEK inhibitor, in combination with pembrolizumab in patients with advanced non-small cell lung cancer (NSCLC). Cancer Res. 83, CT206–CT206 (2023).
Zimmer, L. et al. Encorafenib, binimetinib plus pembrolizumab triplet therapy in patients with advanced BRAFV600 mutant melanoma: safety and tolerability results from the phase I IMMU-TARGET trial. Eur. J. Cancer 158, 72–84 (2021).
Ferrucci, P. F. et al. KEYNOTE-022 part 3: a randomized, double-blind, phase 2 study of pembrolizumab, dabrafenib, and trametinib in BRAF-mutant melanoma. J. Immunother. Cancer 8, e001806 (2020).
Burton, E. M. et al. Safety and efficacy of TRIplet combination of nivolumab (N) with dabrafenib (D) and trametinib (T) [TRIDeNT] in patients (pts) with BRAF-mutated metastatic melanoma (MM): a single center phase II study. Ann. Oncol. 30, v534–v535 (2019).
Liu, Y., Zhang, X., Wang, G. & Cui, X. Triple combination therapy with PD-1/PD-L1, BRAF, and MEK inhibitor for stage III-IV melanoma: a systematic review and meta-analysis. Front. Oncol. 11, 693655 (2021).
Gunderwala, A. Y., Nimbvikar, A. A., Cope, N. J., Li, Z. & Wang, Z. Development of allosteric BRAF peptide inhibitors targeting the dimer interface of BRAF. ACS Chem. Biol. 14, 1471–1480 (2019).
Cook, F. A. & Cook, S. J. Inhibition of RAF dimers: it takes two to tango. Biochem. Soc. Trans. 49, 237–251 (2021).
Tkacik, E. et al. Structure and RAF family kinase isoform selectivity of type II RAF inhibitors tovorafenib and naporafenib. J. Biol. Chem. 299, 104634 (2023).
Yao, Z. et al. RAF inhibitor PLX8394 selectively disrupts BRAF dimers and RAS-independent BRAF-mutant-driven signaling. Nat. Med. 25, 284–291 (2019).
de Braud, F. et al. Initial evidence for the efficacy of naporafenib in combination with trametinib in NRAS-mutant melanoma: results from the expansion arm of a phase Ib, open-label study. J. Clin. Oncol. 41, 2651–2660 (2023).
Rasco, D. W. et al. Phase 1 study of the pan-RAF inhibitor tovorafenib in patients with advanced solid tumors followed by dose expansion in patients with metastatic melanoma. Cancer Chemother. Pharmacol. 92, 15–28 (2023).
Ali, A., Goffin, J. R., Arnold, A. & Ellis, P. M. Survival of patients with non-small-cell lung cancer after a diagnosis of brain metastases. Curr. Oncol. 20, e300–e306 (2013).
Waqar, S. N. et al. Non-small-cell lung cancer with brain metastasis at presentation. Clin. Lung Cancer 19, e373–e379 (2018).
Dutriaux, C. et al. An open label, non-randomised, phase IIIb study of trametinib in combination with dabrafenib in patients with unresectable (stage III) or distant metastatic (stage IV) BRAF V600-mutant melanoma: A subgroup analysis of patients with brain metastases. Eur. J. Cancer 175, 254–262 (2022).
Davies, M. A. et al. Dabrafenib plus trametinib in patients with BRAFV600-mutant melanoma brain metastases (COMBI-MB): a multicentre, multicohort, open-label, phase 2 trial. Lancet Oncol. 18, 863–873 (2017).
Holbrook, K. et al. Intracranial antitumor activity with encorafenib plus binimetinib in patients with melanoma brain metastases: a case series. Cancer 126, 523–530 (2020).
Reinmuth, N. et al. Treatment and outcome of patients with metastatic NSCLC: a retrospective institution analysis of 493 patients. Respir. Res. 14, 139 (2013).
Simeone, J. C., Nordstrom, B. L., Patel, K. & Klein, A. B. Treatment patterns and overall survival in metastatic non-small-cell lung cancer in a real-world, US setting. Future Oncol. 15, 3491–3502 (2019).
Tan, I. et al. Therapeutic outcomes in non-small cell lung cancer with BRAF mutations: a single institution, retrospective cohort study. Transl. Lung Cancer Res. 8, 258–267 (2019).
Gibson, A. J. W. et al. Real-world treatment patterns and effectiveness of targeted and immune checkpoint inhibitor-based systemic therapy in BRAF mutation-positive NSCLC. JTO Clin. Res. Rep. 4, 100460 (2023).
Franovic, A. et al. The next-generation pan-RAF inhibitor, KIN-2787, is active in class II and class III BRAF mutant models. J Clin Oncol 39, 3116–3116 (2021).
Kinnate Biopharma. A Study to Evaluate KIN-2787 in Participants with BRAF and/or NRAS Mutation Positive Solid Tumors. https://www.clinicaltrials.gov/study/NCT04913285?cond=NCT04913285&rank=1 (2021).
Novartis Pharmaceuticals. A Phase Ib Study of LXH254-Centric Combinations in NSCLC or Melanoma. https://classic.clinicaltrials.gov/ct2/show/NCT02974725 (2016).
Millenium Pharmaceuticals Inc. Study of MLN2480 in Participants with Relapses Or Refractory Solid Tumors Followed by a Dose Expansion in Participants with Metastatic Melanoma. https://classic.clinicaltrials.gov/ct2/show/NCT01425008 (2011).
Day One Biopharmaceuticals Inc. Tovorafenib (DAY101) Monotherapy or in Combination with Other Therapies for Patients with Melanoma and Other Solid Tumors. https://classic.clinicaltrials.gov/ct2/show/NCT04985604?term=tovorafenib&cond=Nsclc&draw=2&rank=1 (2021).
Shanghai Henlius Biotech. A Phase II Clinical Trial to Evaluate HLX208 in Advanced Non-small Cell Lung Cancer Patients with BRAF V600 Mutation. https://clinicaltrials.gov/ct2/show/NCT05065398?term=hlx-208&cond=braf&draw=2&rank=9 (2021).
Shanghai Henlius Biotech. A Phase Ib/II Trial to Evaluate the Safety and Efficacy of HLX208+HLX10 in NSCLC with BRAF V600E Mutation. https://classic.clinicaltrials.gov/ct2/show/NCT05641493?term=braf&recrs=abdef&type=Intr&cond=Non-small+Cell+Lung+Cancer&draw=2 (2022).
Acknowledgements
Medical writing support was provided by Mark McCollum, PhD, and Caitlin Cash, PhD, of Nucleus Global and was funded by Pfizer.
Author information
Authors and Affiliations
Contributions
D.P., R.E.S., M.V.N., A.V., and E.F.S. contributed to the drafting and revisions of the manuscript, take responsibility for the integrity of the work, and have provided their approval for the final version.
Corresponding author
Ethics declarations
Competing interests
D.P. reports receiving honoraria from Prime Oncology and PeerVoice; and has had a consulting or advisory role for AstraZeneca, Boehringer Ingelheim, Bristol Myers Squibb, Novartis, Roche, Pfizer, Merck Sharp & Dohme Oncology, Celgene, MedImmune, BeiGene, Samsung, AbbVie, Janssen, Seagen, Takeda, ArriVent, Mirati, Pierre Fabre, and Daiichi Sankyo/AstraZeneca; and has received research funding (institutional financial interest, clinical trials research as principal or co-investigator) from AstraZeneca/MedImmune, Bristol Myers Squibb, Boehringer Ingelheim, Lilly, Merck, Novartis, Pfizer, Roche, Sanofi/Aventis, Taiho Pharmaceutical, Daiichi Sankyo, AbbVie, Janssen, ArriVent, Mirati, Pierre Fabre, Seagen, and Takeda. R.S. reports receiving honoraria from AstraZeneca, GameOn!, Illumina, OncLive, and Targeted Oncology; and has had a consulting or advisory role for Amgen, AstraZeneca, EMD Serono, Daiichi Sankyo, G1 Therapeutics, GE HealthCare, Gilead, GlaxoSmithKline, Janssen Oncology, Regeneron, Sanofi Aventis; and has received research funding from Bristol Myers Squibb, Merck, and AstraZeneca. M.N. reports receiving research funding to institution from Mirati, Novartis, Checkmate, Alaunos, AstraZeneca, Pfizer, Genentech, Navire; a consultant or advisory role for Mirati, Merck/MSD, Novartis, Genentech, Sanofi; and other support from Ziopharm Oncology, ApotheCom, Ashfield Healthcare. A.V. reports no conflicts of interest. E.S. reports receiving honoraria from AstraZeneca, Daiichi Sankyo/AstraZeneca, Merck KGaA, and Boehringer Ingelheim; and has had a consulting or advisory role at Lilly, AstraZeneca, Boehringer Ingelheim, Roche/Genentech, Bristol Myers Squibb, Merck KGaA, MSD Oncology, Takeda, Bayer, Novartis, Daiichi Sankyo, and Seagen; and has received research funding from Boehringer Ingelheim, Bayer, Roche/Genentech, AstraZeneca, and Bristol Myers Squibb.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Planchard, D., Sanborn, R.E., Negrao, M.V. et al. BRAFV600E-mutant metastatic NSCLC: disease overview and treatment landscape. npj Precis. Onc. 8, 90 (2024). https://doi.org/10.1038/s41698-024-00552-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41698-024-00552-7