Abstract
We conducted a meta-analysis of articles published in PubMed, MEDLINE, EMBASE, and Cochrane library to investigate the effectiveness of local consolidative therapy (LCT) against oligometastases. Data from randomized controlled trials (RCTs), balanced studies, and all studies combined were analyzed in a hierarchical manner. Pooled analyses of 31 studies (including seven randomized trials) investigating the effectiveness of LCT on overall survival revealed odds ratios of 3.04, 2.56, and 1.41 for all studies, balanced studies, and RCTs, respectively (all p < 0.05). The benefit of LCT was more prominent in patients with non-small cell lung and colorectal cancers than in those with prostate and small cell lung cancers. Moreover, the benefit of LCT was smaller in patients with high metastatic burdens (p = 0.054). In four of 12 studies with available information, additional grade ≥3 toxicities due to LCTs were reported. Overall, LCT is beneficial for patients with oligometastases, although such benefits are less evident in RCTs than in observational studies. Appropriate LCTs should be carefully selected considering their feasibility, disease type, and metastatic burden.
Similar content being viewed by others
Introduction
To date, cancer treatments have been selected depending on the pathologic stage of progression. The highest solid cancer stage indicates a systemic disease that has spread beyond the primary tumor and lymphatics and has little-to-no chance of being cured. Systemic administration of chemotherapy is regarded as the only valid option, while local modalities such as surgery or radiotherapy are deemed ineffective in terms of survival.
However, long-term survival is not uncommon among patients with metastases who have successfully undergone local salvage treatment. In the late twentieth century, a pivotal case series revealed that patients who underwent resection of the liver for metastases from colorectal cancer had a 5-year survival rate of 28–37%1,2,3; this rate reached 58% as reported in a more recent series4. The International Registry of Lung Metastases study revealed 5- and 10-year survival rates of 36% and 26%, respectively, after curative resection for lung metastases5. Survival outcomes were affected by smaller metastatic burdens or lower levels of tumor markers, which indicated the gradually progressing nature of the metastatic cascade and the presence of an intermediate state, that is, oligometastasis.
Nevertheless, more than two-thirds of such patients ultimately experience polymetastases, and open surgery might be burdensome for some patients whose chance of cure is uncertain and who are debilitated by their disease. The practical and clinical considerations of oligometastases have increased with technological advances in radiotherapy. Given the development of conformal technologies based on computed tomography planning, such as stereotactic body radiotherapy (SBRT), noninvasive, and ablative irradiation methods for metastatic lesions have become feasible6.
Extensive literature has recently emerged regarding the application of local consolidative treatment (LCT) for oligometastases7,8; however, the vast majority of publications are single-arm observational studies. This is partly because it can be difficult to design randomized controlled trials (RCTs) involving patients with metastases given ethical considerations (e.g., the possibility of missing a beneficial treatment because of assignment to a control arm) and patients’ widely varying clinical characteristics. The biological understanding of oligometastatic disease has evolved but remains unclear. Therefore, whether patients can benefit from local treatment for their metastases and whether oligometastasis exists as a status remains controversial9,10.
This meta-analysis aimed to assess the effectiveness of LCT for patients with oligometastases due to any type of solid cancer, thereby validating the benefit of LCT and aiding in clinical decision-making.
Results
Study selection and characteristics
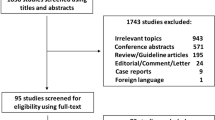
The meta-analysis included 31 controlled studies (23 retrospective and eight prospective studies)9,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40 identified from 436 initially searched records in three databases; the studies included 4762 patients, of whom 2186 and 2576 were divided into the LCT and control arms, respectively. The study inclusion process is depicted in Fig. 1. Eight studies reported conflicts of interest with industrial sponsorship; the remainder had nothing to disclose. Seven studies were RCTs, eight used propensity score matching, 12 reported statistical comparisons of major clinical indicators between arms, and four had no comparative statistical data. Twelve studies included patients with non-small cell lung cancer (NSCLC), two included patients with small cell lung cancer (SCLC), six included patients with prostate cancer, three included patients with colorectal cancer, two included patients with esophageal cancer, two included patients with hepatocellular carcinoma (HCC), and one each included patients with the bile duct, head and neck, sarcoma, and multiple cancers. Most studies (25, 81%) included patients with synchronous and/or metachronous oligometastases and six (19%) targeted patients with metachronous oligometastases. Eleven studies (35%) defined oligometastases as the presence of ≤5 metastases; eight studies (26%) defined it as the presence of ≤3 metastases, and the remainder used varying definitions (Table 1; a detailed version is also provided in Supplementary Table 1).
LCT was performed principally to treat distant metastatic lesions as reported in 24 studies (77%) and to treat primary tumors in nine studies. Surgical resection was the LCT modality of choice in 19 studies (61%) and was performed exclusively in five studies and combined with other modalities in 14 studies (mostly radiotherapy in 12 studies). Radiotherapy was performed in 22 studies (71%), exclusively in nine studies and in combination with other modalities in 13 (mostly surgery, in 12 studies). Radiofrequency or microwave ablation was used in a few studies involving patients with liver neoplasms or metastases. Although only three studies reported significant differences in the number of metastases between the study arms, 12 of the 22 studies (55%) reported a higher frequency of single or low number metastases, without statistical significance, in the LCT arm. Clinical data from the studies are shown in Table 2 (with a more detailed version in Supplementary Table 2).
Pooled analyses of primary endpoints
In the pooled analyses of overall survival (OS), the odds ratios (ORs) were 3.04 (95% confidence interval [CI]: 2.28–4.06, p < 0.001), 2.56 (95% CI: 1.79–3.66, p < 0.001), and 1.41 (95% CI: 1.02–1.95, p = 0.041) for all studies, balanced studies, and RCTs, respectively. In the pooled analyses of progression-free survival (PFS), the pooled ORs were 2.82 (95% CI: 1.96–4.06, p < 0.001), 2.32 (95% CI: 1.60–3.38, p < 0.001), and 1.39 (95% CI: 1.09–1.80, p = 0.009) for all studies, balanced studies, and RCTs, respectively. The pooled ORs for OS in studies principally targeting metastatic and primary tumors were 3.34 (95% CI: 2.40–4.66, p < 0.001) and 2.22 (95% CI: 1.21–4.08, p = 0.010), respectively, with no significant difference in subgroup comparisons (p = 0.248); the corresponding ORs for PFS were 3.34 (95% CI: 2.18–5.13) and 1.60 (95% CI: 0.99–2.59), respectively, with a significant difference between subgroups (p = 0.025). The pooled ORs for OS according to high versus low metastatic burden studies were 2.23 (95% CI: 1.56–3.20, p < 0.001) and 4.32 (95% CI: 2.45–7.59, p < 0.001), respectively, although the difference between these subgroups had a nonsignificant trend (p = 0.054). Regarding PFS, the ORs were 2.27 (95% CI: 1.67–3.09, p < 0.001) and 3.43 (95% CI: 1.70–6.96, p = 0.001), respectively, with no significant difference between the subgroups (p = 0.293). Heterogeneity was significant in most pooled analyses, but was low and insignificant in the pooled analyses of RCTs alone and in the pooled PFS analysis of the high metastatic burden subgroup. Possible publication biases were noted in the pooled analyses of OS in all studies and those investigating metastases, as well as in the pooled analyses of PFS in all studies, balanced studies, studies investigating metastases, and high metastatic burden studies. The main results are presented as Forest plots in Fig. 2, and the detailed results of pooled analysis are shown in Table 3.
In the pooled analyses of OS according to cancer types, the benefit of LCT was more prominent in patients with NSCLC (OR: 3.14, p < 0.001; pooled 2-year OS: 65.2 vs. 37.0%) and colorectal cancer (OR: 4.11, p = 0.066; 2-year OS: 66.2 vs. 33.2%) than in those with prostate cancer (OR: 1.87, p = 0.006; 3-year OS: 95.6 vs. 92.6%) and SCLC (OR: 1.04, p = 0.942; 60.7 vs. 42.8%). Heterogeneity was not significant in the pooled analyses of OS for patients with NSCLC, SCLC, and prostate cancer but was significant in the pooled analyses of OS for those with colorectal cancer. Similar results were obtained for the pooled analyses of PFS; the benefit of LCT was higher for patients with NSCLC (OR: 3.28, p < 0.001; pooled 2-year PFS: 28.9 vs. 8.6%) and colorectal cancer (OR: 4.69, p = 0.055; 2-year PFS: 35.7 vs. 10.5%) and was lower for those with prostate cancer (OR: 2.36, p = 0.019, 2-year PFS: 82.7 vs. 61.7%) and SCLC (OR: 1.65, p = 0.376; 1-year PFS: 30.9 vs. 16.6%). Heterogeneity was not significant in the pooled analyses of PFS for patients with SCLC but was significant for those with NSCLC and those with prostate and colorectal cancers. Detailed results according to the disease type are shown in Tables 3 and 4.
Complications
Twelve of 31 studies (38.7%) involving 2176 patients contained the data of complications related to treatment modalities. Palma et al.40 reported three grade 5 cases (4.5%) possibly related to SBRT, whereas Gore et al.35 reported a significantly higher rate of grade 3 toxicity (24.8 vs. 9.5%) in the LCT arm (with one patient developing grade 5 toxicity). Ruo et al.36 reported a serious postoperative morbidity rate of 20.5%, with two patients developing grade 5 complications within 30 days of elective colorectal surgery. Ni et al.41 reported that 9.3% of patients needed chest tube insertion, while no serious toxicities were reported in the control arm. Otherwise, no significant additional toxicities due to LCTs were reported in eight studies in which LCT consisted mainly of radiotherapy (Table 5).
Discussion
The concept of oligometastases has attracted significant interest as a potentially curative opportunity for patients whose diseases were deemed intractable. Molecular studies that aim to identify disease-specific biomarkers or gene profiles to identify oligometastases have shown promising results42,43; however, external or internal validation was lacking or unsuccessful10. Clinical data reported to date are heterogeneous, making it difficult for physicians to decide whether or not to administer LCTs. Currently, decisions regarding the application of LCTs are made depending on single-arm studies that demonstrated favorable survival outcomes in select patients. However, complications arising from LCTs, the possibility of missed occult metastases, and the distribution of medical resources are issues for consideration6,9.
In the present meta-analysis, LCT was beneficial in terms of OS; the pooled results from all studies (OR: 3.04, p < 0.001) and balanced studies (i.e., those without significant differences in major clinical indicators; OR: 2.56, p < 0.001) were significant, with a high degree of heterogeneity. Possible publication biases were noted, and the trimmed value after sensitivity analysis was lower than the original value (OR: 2.32). The OR was also significant in the pooled analysis of RCTs (OR: 1.41, p = 0.041), with a low degree of heterogeneity, but it was lower in magnitude than the ORs of total and balanced studies. The pooled results of PFS also showed trends similar to those of OS. The significant results obtained from the pooled analyses of RCTs with respect to both OS and PFS support the application of LCT in oligometastatic settings. However, the extent of this benefit might be smaller than that derived from observational study findings, which mostly showed favorable survival outcomes in select patients10. The significant heterogeneity and possible publication biases additionally indicate that selection biases might be present in the literature, despite making efforts to balance both arms using statistical tests. For example, patients in the LCT arm of 12 of 22 studies (55%) with available information tended to have fewer numbers of metastases, although the differences were not significant.
Most of the clinical literature on oligometastases is disease specific, and only a few studies have compared outcomes among different cancer types. According to subgroup analyses based on cancer types, the benefits of LCT and survival outcomes vary among disease entities. The survival benefits of LCTs were the most prominent for patients with NSCLC and colorectal cancer. Of note, the benefit of LCTs in terms of OS and PFS in patients with colorectal cancer showed borderline significance in the pooled analyses (p = 0.066 and 0.055, respectively). However, considering that all three colorectal cancer studies individually showed a significant benefit in terms of OS or PFS29,33,36 and given that the long-term results of Ruers et al.’s study29 (in which the 5-year OS rates were 43.1% and 30.3% and the 5-year PFS rates were 24.4% and 5.9% in the LCT and non-LCT arms, respectively) were not reflected in the analyses, the pooled results should not be interpreted as nonsignificant. Although the benefit of LCT was significant for patients with prostate cancer, its magnitude was relatively small. Survival outcomes of patients with oligometastatic prostate cancer were favorable regardless of the application of LCTs, suggesting that prostate cancer has a less aggressive tumor biology than other cancer types44. The benefit of LCT was not significant for patients with SCLC in terms of either OS or PFS (p = 0.942 and 0.376, respectively). This finding was consistent with the conventional notion that SCLC behaves more like a systemic disease and metastasizes early45.
Regarding complications, additional grade ≥3 toxicities with LCTs were reported in four of 12 studies with available information, including seven cases of grade 5 toxicities. Among five studies of patients with lung cancer, two reported grade 5 toxicities30,35 and two had higher rates of serious complications after LCT41. In the colorectal cancer study conducted by Ruo et al.36 bowel surgery resulted in additional complications, including two cases of 30-day mortality and serious perioperative morbidity (20.5%). In comparison, additional serious toxicities due to LCTs were rarely reported in prostate cancer studies22,31,32,34. Therefore, the application of LCTs for lung cancer, particularly in terms of technical planning and patient selection, should be performed with caution to minimize serious toxicities such as pneumonitis or esophagitis. Bowel surgery should be performed for patients whose clinical conditions allow it and in whom resection is feasible. Administering LCTs for oligometastatic prostate cancer was a relatively safe option. Because the adverse effects and oncologic benefits resulting from LCTs are different for each type of cancer, a tailored strategy for each patient is necessary considering the risk–benefit balance of LCT for oligometastatic diseases.
As observed in the included studies, the definition of oligometastasis varies. Some studies allowed for ≤3 metastases, some studies allowed for ≤5, and a few studies selected patients based on the ability of LCT to cover the metastases. Given clinical heterogeneities, it is difficult to set a clear cut-off number for metastases for determining the benefit of LCTs, even though clinical and biological differences are apparently present between oligometastatic and polymetastatic statuses46,47. Parker et al.32 reported that LCT was beneficial only for patients with low metastatic burdens (≤3 metastases) and not for those with higher metastatic burdens. In the same vein, our study revealed lower ORs in the high metastatic burden subgroup than in the low metastatic burden subgroup with a borderline significant difference (p = 0.054). Little is known about whether LCT that targets the primary disease is as beneficial as that which targets all the oligometastatic foci; other than for nephrectomy and metastatic renal cell carcinomas, data regarding LCT benefit are mostly preclinical or exploratory48. Although the OS benefit was not significantly different in subgroup comparisons, the PFS benefit differed among studies investigating primary diseases vs. those examining metastases. Our hypothesis regarding this PFS benefit is that LCTs covering metastatic lesions might have additional oncologic benefits over systemic treatment and that the studies that principally investigated primary tumors might have involved more patients with uncontrolled primary disease than did the other studies. The meta-analysis methodology is limited in its ability to evaluate the causes of the aforementioned differences. However, our results will aid in clinical decision-making in clinical practice and will lead to hypotheses for future oligometastasis research to identify differences among cancer types and define LCT targets.
We included studies with multiple cancer types, which is not an uncommon approach in investigations of LCTs for oligometastases40. This might cause heterogeneity to some extent among studies that affect the pooled analyses. However, this might also be a method to test the hypothesis that many cancers share an intermediate metastatic cascade called oligometastasis. In addition, this method overcomes the limitation of the small number of studies available for each specific cancer type. To improve the quality of our analyses and results, we rigorously evaluated and interpreted heterogeneity based on statistical methods and performed various subgroup analyses and stepwise analyses according to the studies’ quality. Other limitations include the small number of available studies involving patients with diseases other than NSCLC, prostate cancer, and colorectal cancer, as well as the methodological limitations of meta-analyses in that only outcomes, but not causes, can be determined.
In conclusion, our study demonstrated the oncologic benefits of LCTs in oligometastatic settings in terms of both OS and PFS. Although benefits were also observed when analyzing RCTs, their extent was smaller than that expected from literature data that included observational studies. LCT benefits were more prominent for oligometastases from NSCLC and colorectal cancer. Additional grade ≥3 complications due to LCT were found in approximately one-third of studies with available information. Patients with low metastatic burdens can derive greater benefits from LCTs. Therefore, appropriate LCTs should be selected carefully considering patients’ clinical conditions and disease types. Future research is warranted to identify the oligometastatic conditions in which LCTs are most likely to provide benefit and to investigate the underlying biology of oligometastases with respect to the benefits of LCT.
Methods
Study protocol
Our study adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines. The meta-analysis was designed to answer the following PICO question: “Does LCT confer an oncologic benefit for patients with oligometastases?” By implication, the response to this question would demonstrate whether a clinically meaningful “oligometastatic” status exists. LCT was defined as any local treatment targeted toward metastases and/or remnant primary disease in an oligometastatic setting. PubMed, MEDLINE, EMBASE, and Cochrane library were systematically searched by two independent reviewers for articles published up to March 4, 2020. The following search terms were used with no language restrictions: (oligometastasis OR oligometastases OR oligometastatic OR “limited metastatic” OR “limited metastasis” OR “limited metastases”) AND survival AND (randomized OR randomized OR versus OR comparison OR compare OR controlled). The reference lists of the extracted articles were also searched. Details of the searching strategy are shown in Supplementary Note 1. We compared the data of the LCT and control arms in the retrieved published studies; studies published before 2000 were excluded to avoid introducing potential bias from outdated treatments. Online registration of the protocol was not performed.
Selection criteria
The inclusion criteria were as follows: (1) controlled trials (including both randomized and non-randomized) involving patients with oligometastases that compared the outcomes of those who underwent LCT with the outcomes of those in the control group, (2) ≥10 patients in each arm, (3) at least one primary endpoint provided, and (4) oligometastases defined as ≤5 metastases or as metastases that could definitely be encompassed and treated with LCT. The primary endpoints were OS and PFS. Grade ≥3 complications related to LCTs were assessed subjectively. For multiple studies published from a single institution, only those with a larger number of patients and no (or negligible) overlapping patient pools were included. Duplicate studies and those with irrelevant formats (e.g., reviews, editorials, letters, or case reports) were automatically filtered. Full-text reviews were performed to identify studies that fulfilled the inclusion criteria.
Data extraction and quality assessment
Data were extracted using a pre-standardized form; PFS and OS data were estimated from descriptive graphs in the absence of numerical reports. Quality assessment was performed using the Newcastle-Ottawa Scale49 for cohort studies. Among the three scale domains (“selection” [four points], “comparability” [two points], and “outcome” [three points]), the difference in scores among the studies was mostly due to “comparability.” To avoid subjectivity, we defined the rationale for evaluating comparability based on discussion between clinical oncologists and a biostatistician on the following topics: (1) RCTs were assigned a full score (two points) unless they had serious clinical differences between the comparison arms or flaws in their study designs; (2) statistically matched cohorts (e.g., propensity score matching) or cohorts without significant differences in major clinical indicators were assigned one point; and (3) those with no statistical comparisons or no possibility of clinically significant differences between arms were allotted zero points. Major clinical indicators included the number of metastases, performance status, age, T stage, N stage, prostate-specific antigen (for prostate cancer), and primary disease control; the locations of the metastases were not considered. Studies that scored eight points or higher were considered to have high quality and balanced, while those with six or seven points were considered to have medium quality; lower scores were indicative of low quality.
Statistical analyses
Pooled analyses of primary endpoints were performed (considering the study quality) in a stepwise-hierarchical manner. Overall analysis of all the studies was first performed; next, pooled analyses of balanced studies (eight points or higher on the Newcastle-Ottawa scale) were performed, followed by pooled analyses of the RCTs alone. Considering the varying study designs, treatment modalities, and clinical characteristics, the random-effects model was used for the first two analyses. While the fixed-effects model was used for the pooled analyses of RCTs. The 2-year OS and PFS rates were evaluated in pooled analysis: the 1-year rate was considered when the survival interval was too short or the 2-year rate neared 0% (e.g., patients with SCLC and HCC); the 3- or 5-year rates were considered if the survival rates were too high at 1 or 2 years (e.g., patients with prostate cancer). Pooled analyses of studies were also performed after categorizing them according to specific malignancies, LCT target (primary tumor vs. metastatic distant lesion), and metastatic burden using a random-effects model. Studies that enrolled >80% of patients with a single metastasis or those that included patients with ≤3 metastases were categorized as low-burden studies; otherwise, they were considered as high-burden (e.g., studies that enrolled patients with ≤5 metastasis were considered as high-burden studies). Heterogeneities were assessed using Cochran Q50 and I2 statistics51. Significant heterogeneity was considered to exist at p values <0.1 and I2 values ≥50%. The degree of heterogeneity was evaluated using the I2 values: 0–25% was considered indicative of low heterogeneity; 26–50%, moderate; 51–75%, high; and ≥76%, very high. I2 values <10% with p values <0.05 together indicated very low heterogeneity. Publication bias was evaluated using funnel plots and quantitatively using Egger’s test52. If a significant possibility of bias was detected (two-tailed p < 0.1)52, Duval and Tweedie’s trim and fill method53 was used for sensitivity analysis. Pooled temporal analyses of numerical OS and PFS rates according to the cancer type were performed using the Q test based on analysis of variance. Publication bias assessment was performed only for pooled analyses that included ≥10 studies. All statistical analyses were performed using Comprehensive Meta-Analysis software, version 3 (Biostat Inc., Englewood, NJ, USA).
Ethical consideration
Ethical approval was not required because this study retrieved and synthesized using only previously published data.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
This is a meta-analysis article that has used data retrieved directly from the text, figures, tables, and supplementary files of published articles. A list of all 31 articles used during this meta-analysis can be found in the following metadata record: https://doi.org/10.6084/m9.figshare.1329221354.
Code availability
The authors declare that no custom code was used to generate the dataset. Statistical analyses were performed using Comprehensive Meta-Analysis software, version 3 (Biostat Inc., Englewood, NJ, USA).
References
Hughes, K. S. et al. Resection of the liver for colorectal carcinoma metastases. Dis. Colon Rectum 31, 1–4 (1988).
Nordlinger, B. et al. Surgical resection of colorectal carcinoma metastases to the liver: a prognostic scoring system to improve case selection, based on 1568 patients. Cancer 77, 1254–1262 (1996).
Fong, Y., Fortner, J., Sun, R. L., Brennan, M. F. & Blumgart, L. H. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann. Surg. 230, 309 (1999).
Pawlik, T. M. et al. Effect of surgical margin status on survival and site of recurrence after hepatic resection for colorectal metastases. Ann. Surg. 241, 715 (2005).
Pastorino, U. et al. Long-term results of lung metastasectomy: prognostic analyses based on 5206 cases. J. Thorac. Cardiovasc. Surg. 113, 37–49 (1997).
Tree, A. C. et al. Stereotactic body radiotherapy for oligometastases. Lancet Oncol. 14, e28–e37 (2013).
Petrelli, F. et al. Addition of radiotherapy to the primary tumour in oligometastatic NSCLC: a systematic review and meta-analysis. Lung Cancer 126, 194–200 (2018).
Tilki, D. et al. Local treatment for metastatic prostate cancer: a systematic review. Int. J. Urol. 25, 390–403 (2018).
Guckenberger, M. et al. Characterisation and classification of oligometastatic disease: a European Society for Radiotherapy and Oncology and European Organisation for Research and Treatment of Cancer consensus recommendation. Lancet Oncol. 21, e18–e28 (2020).
Palma, D. A. et al. The oligometastatic state—separating truth from wishful thinking. Nat. Rev. Clin. Oncol. 11, 549 (2014).
Iyengar, P. et al. Consolidative radiotherapy for limited metastatic non–small-cell lung cancer: a phase 2 randomized clinical trial. JAMA Oncol. 4, e173501 (2018).
Sheu, T. et al. Propensity score–matched analysis of comprehensive local therapy for oligometastatic non-small cell lung cancer that did not progress after front-line chemotherapy. Int. J. Radiat. Oncol. Biol. Phys. 90, 850–857 (2014).
Yano, T. et al. Prognostic impact of local treatment against postoperative oligometastases in non‐small cell lung cancer. J. Surg. Oncol. 102, 852–855 (2010).
Frost, N. et al. Local ablative treatment for synchronous single organ oligometastatic lung cancer—a propensity score analysis of 180 patients. Lung Cancer 125, 164–173 (2018).
Gomez, D. R. et al. Local consolidative therapy vs. maintenance therapy or observation for patients with oligometastatic non–small-cell lung cancer: long-term results of a multi-institutional, phase II, randomized study. J. Clin. Oncol. 37, 1558–1565 (2019).
Gray, P. J. et al. Aggressive therapy for patients with non-small cell lung carcinoma and synchronous brain-only oligometastatic disease is associated with long-term survival. Lung Cancer 85, 239–244 (2014).
Chen, Y. et al. Outcomes of concurrent chemoradiotherapy versus chemotherapy alone for esophageal squamous cell cancer patients presenting with oligometastases. J. Thorac. Dis. 11, 1536 (2019).
Song, Y.-Q. et al. Treatment patterns and survival after 18F-fluorodeoxyglucose positron emission tomography/computed tomography-guided local consolidation therapy for oligometastatic non-small cell lung cancer: a two-center propensity score-matched analysis. J. Cancer Res. Clin. Oncol. 146, 1021–1031 (2020).
Chen, J. et al. Sorafenib monotherapy versus sorafenib combined with regional therapies for hepatocellular carcinoma patients with pulmonary oligometastases: a propensity score-matched analysis. J. Cancer 9, 1745 (2018).
Xu, L.-M. et al. Thoracic radiotherapy (TRT) improved survival in both oligo-and polymetastatic extensive stage small cell lung cancer. Sci. Rep. 7, 1–8 (2017).
Lan, T., Chen, Y., Su, Q. & Ye, J. Oncological outcome of cytoreductive radical prostatectomy in prostate cancer patients with bone oligometastases. Urology 131, 166–175 (2019).
Ost, P. et al. Surveillance or metastasis-directed therapy for oligometastatic prostate cancer recurrence: a prospective, randomized, multicenter phase II trial. J. Clin. Oncol. 36, 446–453 (2018).
Steuber, T. et al. Standard of care versus metastases-directed therapy for PET-detected nodal oligorecurrent prostate cancer following multimodality treatment: a multi-institutional case-control study. Eur. Urol. Focus 5, 1007–1013 (2019).
Depypere, L. P. et al. Palliative esophagectomy in unexpected metastatic disease: sense or nonsense? Asian Cardiovasc. Thorac. Ann. 26, 552–557 (2018).
Pan, T. et al. Percutaneous CT-guided radiofrequency ablation for lymph node oligometastases from hepatocellular carcinoma: a propensity score–matching analysis. Radiology 282, 259–270 (2017).
Morino, K. et al. Proposed definition for oligometastatic recurrence in biliary tract cancer based on results of locoregional treatment: a propensity-score-stratified analysis. Ann. Surg. Oncol. 27, 1908–1917 (2020).
Schulz, D. et al. Improved overall survival in head and neck cancer patients after specific therapy of distant metastases. Eur. Arch. Otorhinolaryngol. 275, 1239–1247 (2018).
Falk, A. et al. Effect on survival of local ablative treatment of metastases from sarcomas: a study of the French sarcoma group. Clin. Oncol. 27, 48–55 (2015).
Ruers, T. et al. Local treatment of unresectable colorectal liver metastases: results of a randomized phase II trial. J. Natl Cancer Inst. 109, djx015 (2017).
Shang, S. et al. Local therapy combined with chemotherapy versus chemotherapy for postoperative oligometastatic non-small-cell lung cancer. Fut. Oncol. 15, 1593–1603 (2019).
Tsumura, H. et al. Long‐term outcomes of combining prostate brachytherapy and metastasis‐directed radiotherapy in newly diagnosed oligometastatic prostate cancer: a retrospective cohort study. Prostate 79, 506–514 (2019).
Parker, C. C. et al. Radiotherapy to the primary tumour for newly diagnosed, metastatic prostate cancer (STAMPEDE): a randomised controlled phase 3 trial. Lancet 392, 2353–2366 (2018).
Giessen, C. et al. Evaluation of prognostic factors in liver-limited metastatic colorectal cancer: a preplanned analysis of the FIRE-1 trial. Br. J. Cancer 109, 1428–1436 (2013).
Bouman-Wammes, E. W. et al. Benefits of using stereotactic body radiotherapy in patients with metachronous oligometastases of hormone-sensitive prostate cancer detected by [18F] fluoromethylcholine PET/CT. Clin. Genitourin. Cancer 15, e773–e782 (2017).
Gore, E. M. et al. Randomized phase II study comparing prophylactic cranial irradiation alone to prophylactic cranial irradiation and consolidative extracranial irradiation for extensive-disease small cell lung cancer (ED SCLC): NRG Oncology RTOG 0937. J. Thorac. Oncol. 12, 1561–1570 (2017).
Ruo, L. et al. Elective bowel resection for incurable stage IV colorectal cancer: prognostic variables for asymptomatic patients. J. Am. Coll. Surg. 196, 722–728 (2003).
Xu, Q. et al. Consolidative local ablative therapy improves the survival of patients with synchronous oligometastatic NSCLC harboring EGFR activating mutation treated with first-line EGFR-TKIs. J. Thorac. Oncol. 13, 1383–1392 (2018).
He, J., Li, Y., An, J., Hu, L. & Zhang, J. Surgical treatment in non-small cell lung cancer with pulmonary oligometastasis. World J. Surg. Oncol. 15, 36 (2017).
Hu, F. et al. Efficacy of local consolidative therapy for oligometastatic lung adenocarcinoma patients harboring epidermal growth factor receptor mutations. Clin. Lung Cancer 20, e81–e90 (2019).
Palma, D. A. et al. Stereotactic ablative radiotherapy versus standard of care palliative treatment in patients with oligometastatic cancers (SABR-COMET): a randomised, phase 2, open-label trial. Lancet 393, 2051–2058 (2019).
Ni, Y. et al. Microwave ablation as local consolidative therapy for patients with extracranial oligometastatic EGFR-mutant non-small cell lung cancer without progression after first-line EGFR-TKIs treatment. J. Cancer Res. Clin. Oncol. 146, 197–203 (2020).
Pitroda, S. P. & Weichselbaum, R. R. Integrated molecular and clinical staging defines the spectrum of metastatic cancer. Nat. Rev. Clin. Oncol. 16, 581–588 (2019).
Lussier, Y. A. et al. Oligo-and polymetastatic progression in lung metastasis (es) patients is associated with specific microRNAs. PLoS ONE 7, e50141 (2012).
Esserman, L. J. et al. Addressing overdiagnosis and overtreatment in cancer: a prescription for change. Lancet Oncol. 15, e234–e242 (2014).
Sher, T., Dy, G. K. & Adjei, A. A. Small cell lung cancer. Mayo Clin. Proc. 83, 355–367 (2008).
Lievens, Y. et al. Defining oligometastatic disease from a radiation oncology perspective: an ESTRO-ASTRO consensus document. Radiother. Oncol. 148, 157–166 (2020).
Reyes, D. K. & Pienta, K. J. The biology and treatment of oligometastatic cancer. Oncotarget 6, 8491 (2015).
Arcangeli, S., Zilli, T., De Bari, B. & Alongi, F. “Hit the primary”: a paradigm shift in the treatment of metastatic prostate cancer? Crit. Rev. Oncol. Hematol. 97, 231–237 (2016).
Peterson, J., Welch, V., Losos, M. & Tugwell, P. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 1 Feb 2020.
Cochran, W. G. The combination of estimates from different experiments. Biometrics 10, 101–129 (1954).
Higgins, J. P. T. & Thompson, S. G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 21, 1539–1558 (2002).
Egger, M., Smith, G. D., Schneider, M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 315, 629–634 (1997).
Duval, S. & Tweedie, R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56, 455–463 (2000).
Rim, C. H., Shin, I.-S., Park, S. & Lee, H. Y. Metadata supporting the article: benefits of local consolidative treatment in oligometastases of solid cancers: a step-wise hierarchical pooled analysis and systematic review. figshare https://doi.org/10.6084/m9.figshare.13292213 (2020).
Acknowledgements
This study was supported by the National Research Fund of Korea (NRF-2018R1D1A1B07046998).
Author information
Authors and Affiliations
Contributions
C.H.R. contributed to the conceptualization, writing original draft and editing, and data curation; I.-S.S. performed the statistical analysis as a biostatistician; S.P. contributed to data curation and patient recruitment; H.Y.L. contributed to the supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rim, C.H., Shin, IS., Park, S. et al. Benefits of local consolidative treatment in oligometastases of solid cancers: a stepwise-hierarchical pooled analysis and systematic review. npj Precis. Onc. 5, 2 (2021). https://doi.org/10.1038/s41698-020-00141-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41698-020-00141-4