Abstract
Advanced aging is expected to become a major social problem in China during the second half of the 21st century. Current projections of temperature-related mortality in the context of advanced aging are inadequate, and may underestimate the risks posed by global warming on people aged 90+ years. The present study addresses this issue in Nantong City, which was the city in China with the highest aging and advanced aging rates in the 2000, 2010, and 2020 population censuses. Based on 27 global climate models from the Coupled Model Intercomparison Project Phase 6 and statistical downscaling methods, the impacts of climate change and advanced aging on future temperature-related elderly mortality were explored. Our results indicate that global warming will continue to increase the proportion of people who die from non-optimal temperatures even without considering the impact of advanced aging. Moreover, a higher warming range led to a more significant increase in net-temperature-related mortality and advanced aging is likely to increase heat-related mortality and offset the decline in cold-related mortality. Our study demonstrates a “1 + 1 > 2” effect between advanced aging and climate change, under the four shared socioeconomic pathway climate change scenarios considered here. These findings contribute to a better understanding of the impact of climate change on elderly health and facilitate the development of more effective adaptive strategies for advanced aging societies.
Similar content being viewed by others
Introduction
Global climate change and population aging are two prominent and interlinked concerns of the 21st century1,2. The >1.2 °C global warming relative to preindustrial temperature, which has been driven by human activity3, is a recognised challenge to public health. Climate change’s direct (e.g., rising global temperatures have significant impacts on mortality, morbidity, and injury) and indirect (e.g., disturbance of social processes and ecosystem changes) effects pose immediate or deferred health risks to the human population4. Several Studies have projected future temperature-related mortality under climate change, either at the city or national and global5,6,7 levels, based mainly on the increase in heat-related deaths caused by global warming. Contrastingly, few studies have examined the effects of low temperatures, particularly the interaction between cold and advanced aging (i.e., the increase in the proportion of people over 80 years), primarily because the frequency of low temperatures is expected to decrease in the future. However, the risks imposed by cold and heat do not increase equally with age. According to Global Burden of Disease (GBD) 2019 data (https://vizhub.healthdat.org/gbd-compare/), low temperatures accounted for a higher percentage of global noncommunicable deaths due to disease than high temperatures, with older age groups at a much higher risk of cold-related deaths than heat-related deaths. Our previous study showed that people aged 70–74, 80–84, and 90–94 who died from cold-associated conditions were at higher risk (2.75-, 4.84-, and 6.54-times, respectively) than those who died from heat-associated conditions8. These results indicated that the effect of cold temperatures does not necessarily weaken with aging. Therefore, ignoring the effect of the cold temperatures on the trend of advanced aging could lead to severe public health consequences.
Global population aging is accelerating because of declining fertility rates and increased life expectancy. According to the United Nations World Population Outlook 2022, the proportion of elderly individuals will increase globally by 60% from 2022 to 2050. China, for instance, became a moderately aging society in 2021 (aging rate ≥14%) and is estimated to become a severely aging society (aging rate ≥21%) by 2035, encompassing more than 400 million elderly people. Demographers predict that the aging rate and size of China’s elderly population will continue to rise until 2055 and then stabilise. However, China’s population over 80 years of age will continue to grow after 2055, remaining above 120 million from 2055 to 2100, i.e., 3−4 times higher than the 35.8 million registered in 2020, which accounted for 18.8% of the aging population. Under the medium-pace life expectancy growth scenario, this proportion is expected to be 24.2%, 35.6%, 40.0%, and 51.3% in 2040, 2060, 2080, and 2100, respectively. Advanced aging will thus become a substantial demographic issue in China in the second half of the 21st century. Aging plays a critical role in increasing temperature-related deaths9. Yang et al. (2021) estimated 128,000 and 229,000 heat-related deaths in China in the 2090s under the RCP4.5 and RCP8.5 emission scenarios, respectively, with no changes in population demographics. However, these numbers increased to 361,000 and 654,000, respectively, under the average of the six population scenarios10. Another study found that aging in Beijing would result in a 49−326% increase in temperature-related deaths due to cardiovascular disease in the future, which is the most prominent disadvantage in tackling climate change11. Although population aging has been included in some studies focusing on the effects climate change may exert on mortality rates, none has considered changes in the 80+ and 90+ years population groups, which are the most affected by non-optimal temperatures. Failure to include the oldest-old as an independent group in health risk projections related to climate change may therefore lead to a significant underestimation of health risks.
The present study aimed to provide a comprehensive understanding of the dependent and interactive effects of climate change and advanced aging on heat, cold, and net-temperature-related deaths among the elderly in China’s most heavily aging cities. Specifically, the present study projected these effects under 27 global climate models included in the Coupled Model Intercomparison Project Phase 6 (CMIP6) and four emission scenarios.
Results
Baseline exposure-response relationship between temperature and mortality
Figure 1 displays the historical exposure-response relationship between temperature and the elderly population in different age groups. Specifically, the minimum mortality temperature (MMT) for the elderly population in Nantong increased with age. For the elderly aged 65−79, 80−89, and 90+, the MMT was 24, 25, and 26 °C, respectively. In comparison to MMT, the mortality risk (relative risk, RR) at the 2.5th percentile (1 °C) for the same age groups was 1.280 (95% confidence interval (CI):1.209−1.355), 1.708 (95% CI:1.583−1.844) and 2.217 (95% CI:1.981−2.480), respectively, and that at the 97.5th percentile (31 °C) was 1.192 (95% CI:1.139–1.246), 1.340 (95% CI:1.283–1.399), and 1.492 (95% CI:1.402–1.588), respectively. The temperature–mortality associations were similar when we used 10−21 maximum lag days for temperature, 4−6 df for relative humidity, and 4−8 df for air pollutants (Supplementary Figs. 1–4).
a 65–79 years; b 80–89 years; and c 90+ years. The bars indicate temperature frequency at each 1 °C interval during 2012–2017. The error band denotes the corresponding 95% confidence intervals. The vertical solid line represents minimum mortality temperature; the vertical dashed lines represent 2.5th and 97.5th temperature percentile.
Trends in projected temperature and age-specific mortality
Figure 2 presents an overview of the changes in the annual average temperature and frequency of extremely high temperatures in Nantong under four different climate change scenarios from 1961 to 2100. The shared socioeconomic pathway (SSP) scenarios SSP1-2.6, SSP2-4.5, and SSP3-7.0 scenarios demonstrate similar temperature increases before 2050, with projected annual average temperatures during 2041−2050 being 2.28, 2.27, and 2.24 °C higher than that during 1961−2000 (15.9 °C), respectively. However, temperature increases under these scenarios after 2050 exhibit significant differences. Hence, during 2091−2100, projected annual average temperatures are 2.51, 3.67, and 4.98 °C higher than those during 1961−2000. Under the highest temperature increase scenario, i.e., SSP5-8.5, average annual temperatures during 2041−2050 and 2091−2100 are estimated to be 2.78 and 6.51 °C higher than that during 1961−2000, respectively. The annual frequency of extremely high temperatures (i.e., above 31 °C) estimated under the four scenarios showed a similar trend to the average annual temperature. Specifically, under SSP1-2.6, SSP2-4.5, SSP3-7.0, and SSP5-8.5, the annual frequency of extremely high temperatures during 2041−2050 is predicted to increase by 18.1, 17.8, 17.7, and 23.9 days, respectively, which are much higher values than the 6.6 days baseline of 1961−2000. More extended periods of extremely high temperatures are anticipated during 2091−2100, with increases of 22.2, 38.3, 56.8, and 80.2 days under the SSP1-2.6, SSP2-4.5, SSP3-7.0, and SSP5-8.5 scenarios, respectively, when compared to the baseline period.
a Annual average temperature under SSP1-2.6 and 2-4.5; b annual average temperature under SSP 3-7.0 and 5-8.5; c annual frequency of extremely high temperatures under SSP 1-2.6 and 2-4.5; and d annual frequency of extremely high temperatures under SSP 3-7.0 and 5-8.5. The solid lines denote the annual average temperature and frequency of extremely high temperatures under each scenario and the shaded areas denote the corresponding 95% confidence intervals. The grey-shaded area is where the CIs of both scenarios are superimposed.
Figure 3 presents a projection of the age-specific number of deaths under five United Nations’ life expectancy models. The number of deaths among people aged 65–79 years will decrease steadily after 2040. In contrast, the number of deaths among those aged 80–89 and 90+ years is projected to continue to increase. After 2055, the 90+ years age group is expected to become the one with the highest number of deaths. Supplementary Fig. 5 presents a detailed projection for the age-specific number of deaths under the medium-pace life expectancy growth scenario and nine United Nations’ model life tables.
a Very slow life expectancy growth scenario; b slow-pace life expectancy growth scenario; c medium-pace life expectancy growth scenario; d fast life expectancy growth scenario; and e very fast life expectancy growth scenario. Solid lines represent the average value of nine United Nations’ model life tables and shaded areas are the corresponding 95% confidence intervals.
Projection of cold- and heat-related mortality burdens, assuming no population changes
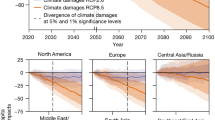
Figure 4 shows the changes in the population-attributable fraction (PAF) of heat-, cold-, and net- (heat and cold) temperature-related excess mortality under four climate change models, assuming no population changes. Under scenarios SSP2-4.5, SSP3-7.0, and SSP5-8.5, the PAF of cold exhibits a continuous decrease whereas that of heat shows a continuous increase. Interestingly, under SSP1-2.6, the PAF of cold and heat remains stable after 2050, and under SSP1-2.6 and SSP2-4.5, the PAF of heat will not surpass that of cold until 2100. However, under SSP3-7.0 and SSP5-8.5, the PAF of heat will exceed that of cold in the 2090s and the 2060s, respectively. The net PAF will continue to increase, with projections indicating that in 2080−2089 it will increase by 2.64%, 6.39%, 13.57%, and 29.46% compared to 2010−2019 values, under the SSP1-2.6, SSP2-4.5, SSP3-7.0, and SSP5-8.5 scenarios, respectively.
Figure 5 shows the age-specific changes in the heat-, cold-, and net-temperature-related PAF under the four SSPs, assuming no population changes. Interestingly, the time at which the PAF of heat exceeded that of cold occurred later in older age groups. For instance, under SSP5-8.5, the PAF of heat is expected to surpass that of cold during 2040−2049 in the 65−79 years age group, during 2060−2069 in the 80−89 years age group, and during 2070−2079 in the 90+ years age group. The net PAF will continue to increase across all age groups. For instance, the projected net PAF of 65−79, 80−89, and 90+ years age groups under SSP5-8.5 during 2080−2089 is estimated to be 11.67 (95% CI: 8.78−14.75), 19.63 (95% CI: 15.93−23.95), and 25.90 (95% CI: 20.58−31.78), respectively, which are 1.50, 1.23, and 1.23 times higher than the corresponding values observed during 2010−2019.
a age 65–79 under SSP 1-2.6 scenario; b age 80–89 under SSP 1-2.6 scenario; c age 90+ under SSP 1-2.6 scenario; d age 65–79 under SSP 2-4.5 scenario; e age 80–89 under SSP 2-4.5 scenario; f age 90+ under SSP 2-4.5 scenario; g age 65–79 under SSP 3-7.0 scenario; h age 80–89 under SSP 3-7.0 scenario; i age 90+ under SSP 3-7.0 scenario; j age 65–79 under SSP 5-8.5 scenario; k age 80–89 under SSP 5-8.5 scenario; and l age 90+ under SSP 5-8.5 scenario. The error band denotes the 95% empirical confidence interval, which is produced by Monte Carlo simulations generating 1000 samples.
Interactive effects of climate change and advanced aging
Figure 6 presents a holistic evaluation of the interactive effects of climate change and advanced aging on future temperature-related excess mortality rates. Overall, the net-temperature PAF increased under all four climate change scenarios and advanced population aging. Specifically, net-temperature-related excess mortality under SSP1-2.6, SSP2-4.5, SSP3-7.0, and SSP5-8.5 scenarios assuming no population changes is estimated at 13.86% (95% CI: 11.39−16.25%), 14.30% (95% CI: 11.46−17.03%), 15.27% (95% CI: 12.13−19.38%), and 17.35% (95% CI: 13.94−21.42%), respectively, during 2080−2089. However, when advanced aging is considered, net-temperature-related excess mortality is estimated to increase to 18.30% (95% CI: 14.80−21.62%), 18.77% (95% CI: 14.95−22.47%), 19.86% (95% CI: 15.59−24.79%), and 22.05% (95% CI: 17.62−27.00%), respectively, during the same period. In addition, advanced aging is expected to increase the risk of net-temperature-related excessive mortality. Under the SSP1-2.6, SSP2-4.5, SSP3-7.0, and SSP5-8.5 scenarios, the risk of net-temperature PAF is estimated to be 1.33-, 1.37-, 1.44-, and 1.62-times higher in 2080−2089 than in 2020−2029, respectively, whereas the risk was only 1.03, 1.07, 1.13, and 1.31 when advanced aging was not considered. Advanced aging is also expected to considerably weaken the decline of cold-related excessive mortality. In fact, under SSP1-2.6, SSP2-4.5, and SSP3-7.0 scenarios, cold-related excessive mortality might increase during 2020−2089, 2020−2069, and 2020−2059, respectively. The time at which the heat PAF exceeds cold PAF is estimated to occur later when advanced aging is considered. These findings emphasise the critical importance of identifying effective adaptation strategies to mitigate the risks of climate change-induced temperature-related excessive mortality, particularly in the elderly population.
Table 1 presents a comparative analysis of PAF changes when considering the interactive effects of climate change and advanced aging or assuming their independent effects. The scenario assuming no climate change (independent effect of advanced aging) indicates that the temperature-related PAF will increase by approximately 30% by the end of the 21st century compared to 2010−2019. On the other hand, assuming no population changes (independent effect of climate change), the temperature-related PAF is expected to increase by 1.87% (SSP1-2.6) to 39.29% (SSP5-8.5) at the end of the 21st century compared to 2010−2019. However, the combined effect of advanced aging and climate change was greater than the sum of their independent effects, particularly under heat-related PAF under the SSP2-4.5, SSP3-7.0, and SSP5-8.5 scenarios. Similarly, cold-related PAF increased in most periods under the SSP1-2.6 and SSP2-4.5 scenarios.
Discussion
The present study estimated an increase in net-temperature-related PAF in Nantong, China, by decade and under all four climate change scenarios considered; this trend will be strengthened by advanced aging. Our findings indicate that advanced aging and climate change will increase heat-related mortality and reverse the declining trend in cold-related mortality.
In Nantong, climate change is projected to lead to a continuous increase in the proportion of mortality attributable to non-optimal temperatures, under the assumption of no changes in population demographics. This is because climate change is associated with a decrease in moderately low temperatures (low RR) and an increase in extremely high temperatures (high RR), as indicated in Supplementary Table 1. Although the incidence of heat-related excess mortality is expected to rise globally in the future12, it remains unclear whether climate change will result in positive or negative net annual mortality related to temperature. A study conducted across 23 countries revealed that climate change generally increases the mortality rate associated with non-optimal temperatures; however, the results also demonstrated significant regional disparities13. In Beijing, China, the net annual temperature-related ischaemic stroke deaths were projected to surge by nearly 100% by the 2080s compared to the 1980s, regardless of population changes, under the RCP8.5 scenario14. Similarly, research has revealed that climate change in Tianjin, China, will lead to a net increase in deaths resulting from cardiovascular diseases attributable to temperature and that the increase in heat-related mortality will be higher than the decrease in cold-related mortality15. A study conducted in New York, United States (US), revealed that climate change is expected to lead to positive annual net mortality related to temperature16. Under the higher-emission RCP8.5 scenario, eight of the ten metropolitan areas in the US are expected to experience a net increase in temperature-related deaths per million people by 2086−209517. Conversely, studies conducted in 28 cities in the US suggested that climate change will reduce the burden of temperature-related diseases and mortality18. In Brisbane and Sydney, Australia, net annual temperature-related deaths are expected to increase in the future, whereas a slight decrease will occur in Melbourne19. The present study’s findings are consistent with these previous conclusions, wherein most regions across the world had their minimum temperature-related mortality located within the 70−90% local temperature percentile, and the range of high temperatures was narrower than that of low temperatures20,21,22. However, the relationship between temperature and mortality is affected by various social factors, such as the region’s development and economic performance, urbanisation rate, population age structure, central heating, and usage of air conditioning23,24, all contributing to different temperature–mortality curves across regions and diseases. Furthermore, the magnitude of the temperature increase varies among world regions, resulting in different net-temperature-related mortality changes across them25. A study on 15 diseases in Ningbo, China, projected a decline in deaths resulting from ten of those diseases, represented by chronic lower respiratory diseases, and an increase in deaths resulting from the other five diseases, represented by ischaemic heart disease, attributed to climate change26. In addition, whether the PAF of heat exceeds that of cold remains uncertain and depends on several factors that vary among regions, age groups, and causes of death. Research in the United Kingdom (UK) has shown that the number of people dying from low temperature-associated causes is expected to be 13.0, 5.8, and 2.9 times higher than those dying from high temperature-associated causes in 2020, 2050, and 2080, respectively27. Similarly, the present study found that the PAF of cold and heat is expected to vary among the different climate and population change scenarios analysed.
This study examined the impact of advanced aging on the risk of climate change, particularly in people aged 90+ years. Although the proportion of the oldest old is growing slowly, this growth rate will accelerate every year, becoming a serious social issue after 2050 in China and in Nantong City in particular. The 2050 − 2100 period is expected to be of intense warming under most climate-change scenarios. The present study found that advanced aging magnifies heat-related mortality, and that the interactive effect of heat and advanced aging is even higher than the sum of their independent effects. Additionally, advanced aging has an adverse effect on the declining trend of cold-related mortality, which has not been identified in previous studies. Previous research has shown that aging increases the risk of heat-related mortality owing to climate change. For instance, aging will aggravate the risk of heat-related mortality in Guangzhou, China, and every 1% increase in the proportion of the elderly population will increase heat-related years of life lost (YLLs) by 420 in the 2030s28. Taking aging into account, the mortality from cardiovascular diseases in Beijing is expected to rise by 16.6%, 73.8%, and 134.0% in 2020, 2050, and 2080, respectively, under the RCP8.5 scenario29. Aging is also expected to lead to an increase in heat-related YLLs due to cardiovascular diseases in Ningbo, China, in the 2050s and 2070s30. Research in the UK has shown that climate change has a significant impact on cold- and heat-related deaths among the elderly. Heat-related deaths are expected to increase sharply in the second half of the 21st century, whereas cold-related deaths will likely not decline significantly. A study in South Korea has found that regardless of aging, temperature-related mortality in the 2090s is expected to be 0.5–1.5 times higher than that in 1992−2010, but it will experience a 4−6 times increase when considering population demographic changes31. One review has shown that the elderly are particularly sensitive to climate change32. Hence, advanced aging should be considered as a potentially influencing factor, especially after 2055, when people aged 90+ years are estimated to stand the largest mortality. According to national population censuses in China, the number of deaths in people over 80 years old accounted for an increasing percentage (14.8% in 1990 to 38.5% in 2020) of total deaths, and people aged 80−89 years and 90+ years are expected to become the groups sustaining the highest mortality during 2030−2060 and 2060−2100, respectively. This will lead to an inevitable increase in the excessive mortality attributable to non-optimal temperatures, and not accounting for the different mortality rate of people in these age groups will underestimate the public health consequences of climate change.
The results obtained in the present study have several major environmental and public health implications. First, irrespective of advanced aging, the net-temperature-related PAF will increase with increasing global warming, and it is urgent for governments worldwide to develop policies that eliminate greenhouse gas emissions to slow the pace of global warming. Second, cold-related mortality will continue to increase, or at least not decline, owing to advanced aging, and ignoring the health risks of low temperatures will lead to serious public health consequences. Therefore, local governments should play a positive role in reducing the negative impact of cold on the aging population, especially in areas with high advanced aging rates. Third, our study revealed that advanced aging will further increase temperature-related deaths among the elderly. Fourth, the time at which the PAF of heat exceeds that of cold varies among age groups and climate change scenarios, and people above 80 years of age will suffer more from cold-related mortality. Therefore, it is crucial to formulate both cold and heat prevention policies according to the local population structure and magnitude of warming. Overall, our findings provide valuable insights for policymakers to develop effective strategies for mitigating the impacts of climate change on public health and aging populations.
Our study had some limitations. First, population adaptation was not considered. Most previous studies have employed population adaptation scenarios where adaptation increases by a certain percentage per decade; however, the extent of this adaptation is uncertain and difficult to predict accurately33,34. With economic development, increasing urbanisation, and the increased use of air conditioning, people’s adaptation to hot and cold conditions will be strengthened35. However, the lower frequency of moderate and extremely low temperatures expected in the future will weaken the people’s adaptation to occasional extremely low temperatures36. Second, new technologies such as wearable cooling equipment and new building materials may affect the temperature exposure of individuals and lead to discrepancies between the temperature measured by official outdoor temperature stations and the temperature to which people are exposed to. Third, all air pollutants could potentially affect the association between temperature and mortality. For example, the concentration of ozone in many Chinese cities has increased in recent years and is positively associated with temperature. This could potentially confound the effects of global warming on mortality and should therefore be considered in future studies. Finally, the present study was conducted in a city located in a north subtropical region and thus the results obtained cannot be generalised to geographic areas with different climates and population characteristics. MMT in Nantong city is increasing with age, but we cannot discern if it is an occasional, local phenomenon, or a general one. A nationwide study in Spain found that MMT decreased with age but varied with population, climatic characteristics, and socioeconomic conditions37. However, the underlying mechanisms require further investigation.
Methods
Study population and region
The research area chosen for this study was Nantong City (121°E, 32°N), located in the northern subtropics, and recognised as the pioneer of an aging society in China. Based on the fifth, sixth, and seventh national population censuses conducted in 2000, 2010, and 2020, respectively, the proportion of people over 65 years of age in the total population of Nantong was 12.44%, 16.50%, and 22.67%, respectively. This means the city has persistently maintained its position as the city with the highest proportion of old people among 340 cities above the prefecture level in China. In 2010 and 2020, advanced aging rates in Nantong were 3.65% and 5.15%, respectively, ranking first among 340 cities nationwide. The significant increase in advanced aging rates and the large elderly population (over 1.7 million people over 65 years old in 2020) make Nantong one of the most vulnerable areas to climate change-related health risks.
Data collection
Death, weather, and air pollution data
Daily all-causes mortality data from 1 January 2012 to 31 December 2017 were obtained from the Nantong Health Commission. The data were divided into three groups according to age: young-old (65−79 years, 105,746 records), middle-old (80−89 years, 108,623 records), and oldest-old (90+ years, 41,668 records). This study has been approved by the Ethics Committee of the Nantong University (No. 2022(05)). No participants were contacted, and data were analysed at an aggregate level. Temperature and humidity data for the same period were collected from the National Meteorological Data Sharing Service Network and air pollutants data were collected from a local air quality monitoring station.
Projection of annual age structure
Regarding demography, the scale and number of deaths of the elderly population in a particular region are predicted based on three key parameters: life expectancy, model life table, and migration. The primary parameter for future projections is life expectancy, which determines the number of deaths in different age groups. A higher life expectancy will result in fewer deaths in the young-old and more deaths in the oldest-old. The secondary parameter is the model life table, which represents the mortality rate at specific ages for a given life expectancy. For the present study, the seventh population census conducted in 2020 in Nantong was selected as the base population. Information regarding the age structure of the base population is provided in Supplementary Table 2. In Nantong, the life expectancy in 2020 was 79.58 years, as provided by the National Bureau of Statistics, which was 1.65 years higher than China’s nationwide average life expectancy (77.93 years) in the same year. Migration was not included in the present study because Nantong City maintained a migration balance from 1990 to 2020, According to China’s population censuses, the annual net migration rates in Nantong City during the last three decades were 0.492% (1990–2000), 0.204% (2000–2010), –0.755% (2010–2020), which are much lower than those in most cities in China. Age- and sex-specific mortality rates between 2021 and 2100 were calculated according to future life expectancy and the model life table. Five UN life expectancy growth models (very slow, slow pace, medium pace, fast, and very fast) were used in the present study, starting from the 2020 study. The results obtained from these are presented in Supplementary Table 3. Nine commonly used model life tables were adopted to calculate the annual age-specific population and the age-specific number of deaths from 2021 to 2100. Each model life table represents a distinct age- and sex-specific mortality rate within the same life expectancy and would lead to different age structures in the future. These included four Coale-Demeny regional model life tables for developed countries (East, West, South, and North) and five UN model life tables for developing countries (Latin, Chile, South Asia, General, and Far East). Calculations were as follows (1):
where \({m}_{i}\left(j\right)\) refers to the mortality rate of the population aged j in year i, as determined by the predicted value of future life expectancy and the model life table; \({P}_{i}(j)\) is the number of people aged j in year i; and \({M}_{i}\left(j\right)\) represents the number of deaths in the population aged j in year i. Population predictions were obtained using the PADIS-INT software (version 1.70), which is a widely used and recommended population prediction software by the UN Population Division.
Projections of daily temperature
The daily temperature prediction dataset for 1961−2100 under 27 General Circulation Models (GCMs, Supplementary Table 4) and four emission scenarios (SSP1-2.6, SSP2-4.5, SSP3-7.0, SSP5-8.5) provided by CMIP6 were selected. The NWAI-WG statistical downscaling model was used to downscale the GCMs’ monthly grid data of the corresponding national meteorological station (No. 58259) in Nantong City into daily data38. The statistical downscaling model consisted of three main steps: spatial downscaling, bias correction, and temporal downscaling. Spatial downscaling involves inverse distance-weighted interpolation based on the centre of the nearest four grid points in the GCMs to avoid multiple counties within a grid sharing the same projected value. Bias correction of the GCM-projected monthly values and historically observed temperatures was performed using the equidistant quantile method. Finally, a modified version of the stochastic weather generator was used to downscale the bias-corrected monthly GCM projections to the daily time series of key climate variables such as the daily maximum and minimum temperatures, and the daily average temperature of the 27 GCMs in Nantong was calculated.
Statistical analyses
Historical temperature–mortality relationship
Considering the lag effect and nonlinear relationship between temperature and mortality, the distributed lag nonlinear model (DLNM) was used to assess the historical effect of temperature on mortality in the three age groups13 as follows (2):
Where Yt represents the number of deaths on day t; α is the intercept; the cross-basis function generated by DLNM was used for the daily average temperature with a natural cubic spline function (NS) by placing three knots at the 10th, 50th, and 90th percentiles of temperature, and an NS for the lag dimension (up to 14 days); β is the coefficient; μit indicates the covariates, including relative humidity and two major air pollutants (PM2.5 and O3), which were adjusted using NS with three df; DOWt is the day of the week. The parameters used in the DLNM model and the strategy for sensitivity analyses were similar to those used in our previous work8.
Projections of future temperature-related mortality
To estimate the temperature-related mortality burden in 2020−2099, we incorporated 27 GCMs of CMIP6 to simulate the daily mean temperature using the historical temperature–mortality relationship. We calculated the daily number of deaths from mean temperature exposure under different climate change scenarios. Daily non-optimal temperature (cold, heat, and net)-related mortality in the four different climate change scenarios was calculated using the daily number of deaths and the attributable fraction of non-optimal temperature, which was calculated as follows (3):
Where, \(\triangle M\) represents the number of cold- or heat-related deaths in a future day (defined as temperatures below or above the MMT; MMT was defined as the specific temperature associated with the lowest mortality risk); M represents the number of deaths on each age group (65−79, 80−89, 90+) on a certain day in the future; j is the age group (65−79, 80−89, 90+); RR represents the mortality relative risk of the projected daily mean temperature relative to MMT. The sum of excess deaths for all cold and hot days is the number of deaths attributed to cold and heat, respectively, and the sum of both is the net effect of cold and heat. The attributable fraction (AF) was calculated by dividing the number of deaths attributed to non-optimal temperatures (i.e., cold and heat) by the total number of deaths. Monte Carlo simulations generating 1000 samples by assuming a multivariate normal distribution for the coefficients derived from the cross-basis function were computed to produce the empirical confidence intervals.
The independent effects of advanced aging and climate change were defined by assuming no climate change or no population changes, respectively. Under the scenario of no climate change, the RR of daily cold- and heat-related mortality did not differ from that during the historical period. Under the scenario of no population changes, the number of deaths at 65−79, 80−89, and 90+ years (Mj) did not differ from that during the historical period. The interactive effect was defined under scenarios of climate change and advanced aging, in which RRj was calculated by comparing the projected daily mean temperature to the MMT, and Mj was estimated based on the projections of age structure changes obtained in the previous step.
Data availability
Data are publicly available from the websites for baseline weather data (http://data.cma.cn/), baseline air pollution data (http://www.cnemc.cn/), and projected temperatures (https://esgf-node.llnl.gov/search/cmip6/). The projected population is provided in Supplementary Information. Raw data on mortality were collected under a data sharing agreement, and the authors are not authorised to redistribute the data.
Code availability
The underlying code for this study is not publicly available but could be made available to qualified researchers upon reasonable request.
References
Costello, A. et al. Managing the health effects of climate change: lancet and University College London Institute for Global Health Commission. Lancet 373, 1693–1733 (2009).
Watts, N. et al. The Lancet Countdown: Tracking progress on health and climate change. Lancet 389, 1151–1164 (2017).
World Meteorological Organization. The State of the Global Climate. https://public.wmo.int/en/our-mandate/climate/wmo-statement-state-of-global-climate. (World Meteorological Organization, 2021).
Tong, S. et al. Current and future threats to human health in the Anthropocene. Environ. Int. 158, 106892 (2022).
Wang, Y. et al. Tens of thousands additional deaths annually in cities of China between 1.5oC and 2.0oC warming. Nat. Commun. 10, 3376 (2019).
Li, Y., Ren, T., Kinney, P. L., Joyner, A. & Zhang, W. Projecting future climate change impacts on heat-related mortality in large urban areas in China. Environ. Res. 163, 171–185 (2018).
Heaviside, C. et al. Heat-related mortality in Cyprus for current and future climate scenarios. Sci. Total Environ. 569-70, 627–633 (2016).
Huang, Y., Yang, J., Chen, J., Shi, H. & Lu, X. Association between ambient temperature and age-specific mortality from the elderly: epidemiological evidence from the Chinese prefecture with most serious aging. Environ. Res. 211, 113103 (2022).
Chen, K., Vicedo-Cabrera, A. M. & Dubrow, R. Projections of ambient temperature- and air pollution-related mortality burden under combined climate change and population aging scenarios: a review. Curr. Env. Hlth. Rep. 7, 243–255 (2020).
Yang, J. et al. Projecting heat-related excess mortality under climate change scenarios in China. Nat. Commun. 12, 1039 (2021).
Qian, X. et al. Projections of future temperature-related cardiovascular mortality under climate change, urbanization and population aging in Beijing, China. Environ. Int. 163, 107231 (2022).
Guo, Y. et al. Quantifying excess deaths related to heatwaves under climate change scenarios: A multicountry time series modelling study. PLoS Med. 15, 1–17 (2018).
Gasparrini, A. et al. Projections of temperature-related excess mortality under climate change scenarios. Lancet Planet. Health 1, e360–e367 (2017).
Li, T. et al. Long-term projections of temperature-related mortality risks for ischemic stroke, hemorrhagic stroke, and acute ischemic heart disease under changing climate in Beijing, China. Environ. Int. 112, 1–9 (2018).
Li, G., Li, Y., Tian, L., Guo, Q. & Pan, X. Future temperature-related years of life lost projections for cardiovascular disease in Tianjin, China. Sci. Total Environ. 630, 943–950 (2018).
Li, T., Horton, R. & Kinney, P. Future projections of seasonal patterns in temperature-related deaths for Manhattan. Nat. Clim. Change 3, 717–721 (2013).
Weinberger, K. et al. Projected temperature-related deaths in ten large U.S. metropolitan areas under different climate change scenarios. Environ. Int. 107, 196–204 (2017).
Davis, R., Knappenberger, P., Michaels, P. & Novicoff, W. Seasonality of climate-human mortality relationships in US cities and impacts of climate change. Clim. Res. 26, 61–76 (2004).
Guo, Y. et al. Projecting future temperature-related mortality in three largest Australian cities. Environ. Pollut. 208, 66–73 (2016).
Gasparrini, A. et al. Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet 386, 369–375 (2015).
Wang, C. et al. Nonlinear relationship between extreme temperature and mortality in different temperature zones: a systematic study of 122 communities across the mainland of China. Sci. Total Environ. 586, 96–106 (2017).
Ma, W. et al. The temperature–mortality relationship in China: An analysis from 66 Chinese communities. Environ. Res. 137, 72–77 (2015).
Zhang, L., Zhang, Z., Wang, C., Zhou, M. & Yin, P. Different mortality effects of extreme temperature stress in three large city clusters of Northern and Southern China. Int. J. Disast. Risk. Sci. 8, 445–456 (2017).
Chen, K. et al. Impact of climate change on heat-related mortality in Jiangsu province, China. Environ. Pollut. 224, 317–325 (2017).
TONG, S., Jorn, O. & Patrick, L. Climate change and temperature-related mortality: implications for health-related climate policy. Biomed. Environ. Sci. 34, 379–386 (2021).
Gu, S. et al. Projections of temperature-related cause-specifific mortality under climate change scenarios in a coastal city of China. Environ. Int. 143, 105889 (2020).
Hajat, S., Vardoulakis, S., Heaviside, C. & Eggen, B. Climate change effects on human health: projections of temperature-related mortality for the UK during the 2020 s, 2050 s and 2080 s. J. Epidemiol. Community Health 68, 641–648 (2014).
Liu, T. et al. Modification effects of population expansion, ageing, and adaptation on heat-related mortality risks under different climate change scenarios in Guangzhou, China. Int. J. Environ. Res. Public Health 16, 376 (2019).
Li, T. et al. Aging will amplify the heat related mortality risk under a changing climate: Projection for the elderly in Beijing, China. Sci. Rep. 6, 28161 (2016).
Huang, J. et al. Projections for temperature-related years of life lost from cardiovascular diseases in the elderly in a Chinese city with typical subtropical climate. Environ. Res. 167, 614–621 (2018).
Lee, J. & Kim, H. Projection of future temperature-related mortality due to climate and demographic changes. Environ. Int. 94, 489–494 (2016).
Bunker, A. et al. Effects of air temperature on climate-sensitive mortality and morbidity outcomes in the elderly; a systematic review and meta-analysis of epidemiological evidence. EBioMedicine 6, 258–268 (2016).
Carter, J. G. et al. Climate change and the city: building capacity for urban adaptation. Prog. Plan. 95, 1–66 (2015).
Vicedo-Cabrera, A. M. et al. A multi-country analysis on potential adaptive mechanisms to cold and heat in a changing climate. Environ. Int. 111, 239–246 (2018).
Hondula, D., Balling, R. Jr, Vanos, J. & Georgescu, M. Rising temperatures, human health, and the role of adaptation. Curr. Clim. Change Rep. 1, 144–154 (2015).
Kinney, P. et al. Winter season mortality: will climate warming bring benefits? Environ. Res. Lett. 10, 064016 (2015).
Achebak, H., Devolder, D. & Ballester, J. Trends in temperature-related age-speciffc and sex-speciffc mortality from cardiovascular diseases in Spain: a national time-series analysis. Lancet Planet. Health 3, e297–e306 (2019).
Liu, D. & Zuo, H. Statistical downscaling of daily climate variables for climate change impact assessment over New South Wales, Australia. Clim. Change 115, 629–666 (2012).
Acknowledgements
This study was funded by the National Natural Science Foundation of China (Grant No. 82003552). The funder played no role in the study design, data collection, analysis, and interpretation of data, or writing of the manuscript.
Author information
Authors and Affiliations
Contributions
Y.H. and J.Y. initiated the study. Y.H., C.L., D.L.L., and J.Y. collected the data. Y.H. cleaned and analysed the data. Y.H. and J.Y. drafted the manuscript with important input from C.L. and D.L.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Huang, Y., Li, C., Liu, D.L. et al. Projection of temperature-related mortality among the elderly under advanced aging and climate change scenario. npj Clim Atmos Sci 6, 153 (2023). https://doi.org/10.1038/s41612-023-00487-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41612-023-00487-z
This article is cited by
-
Avoiding overestimates of climate risks from population ageing
npj Climate and Atmospheric Science (2024)