Abstract
As an integral part of the overall life cycle, it is crucial to ensure equity and accessibility to palliative care services at the end of life. The knowledge of healthcare providers has a significant beneficial impact on the quality of palliative care services. This study aimed to compare the nationwide geographic distribution of healthcare providers’ knowledge of palliative care at the provincial level in China and identify the possible factors associated with its geographic disparities. A descriptive cross-sectional study was conducted in all provinces (n = 29) that implemented palliative care pilot programs in China. Data were collected online using a structured questionnaire. The possible factors associated with healthcare providers’ knowledge including economy, demographics, and health, were explored by using exploratory regression and ordinary least squares. In addition, spatial autocorrelation was also examined with Moran’s I, LISA, and Geographically Weighted Regression. A total of 18,272 participants from 903 health institutions in 87 palliative care pilot cities were included across 29 out of 31 provinces in China. The average knowledge score (mean ± standard deviation [SD]) was 8.61 ± 2.85. A positive spatial correlation was observed in healthcare providers’ palliative care knowledge level in China. The high level of knowledge was significantly associated with fewer hospitals per 10,000 population (β = −0.384, 95% CI: −0.601 to −0.168, p = 0.001), more primary healthcare institutions per 10,000 population (β = 0.220, 95% CI: 0.032–0.407, p = 0.024), and more community health center visits (β = 0.259, 95% CI: 0.054–0.465, p = 0.016), with higher coefficients being observed in the northwest and northeast regions. This study suggested that the knowledge level of palliative care among healthcare providers nationwide was relatively low, indicating the existence of a disparity between the supply and demand of palliative care services. There may be regional disparities in palliative care services based on the substantial geographical variation in healthcare provider knowledge, emphasizing the necessity of tailored interventions targeting areas with the greatest need.
Similar content being viewed by others
Introduction
China, as the country with the largest share of the older population in the world (Fang et al., 2015), is confronted with the formidable challenge of population aging. Simultaneously, the increasing prevalence of chronic illnesses has resulted in a growing demand for palliative care. Palliative care is in high demand as a crucial element of the “last mile” of integrated health services throughout the life cycle. The life cycle approach incorporates all aspects of health promotion from fetal development to the end of life. Given that the palliative care service is an essential component of the total life cycle, it is imperative to ensure equity and accessibility to them at the end of life, which is becoming a widespread global public health concern. However, there exists a significant disparity between the supply and demand of palliative care services (Zhu et al., 2021). To address this issue, the National Health Commission launched palliative care pilot programs in five cities in 2017 (China, 2017a, 2017b), subsequently expanding to 71 cities in 2019, including Shanghai (China, 2019). With increased attention from the government and the promotion of palliative care, both the supply and demand for palliative care in China have been steadily rising, and this upward trajectory is expected to continue in the future. However, as the pilot programs continue to expand, there is an increasing focus on the effectiveness and quality of palliative care services. Healthcare providers play a vital role in the development of palliative care (Teng et al., 2022), as they are responsible for delivering optimal care to patients. Consequently, the knowledge level of healthcare providers in palliative care is paramount, as it forms the foundation for delivering high-quality palliative care services.
Despite the importance of healthcare provider knowledge, previous studies on palliative care in China have primarily focused on specific local areas, specific units, or specific populations. For instance, Wu et al. investigated the knowledge of 167 oncology medical staff in Harbin and found insufficient understanding of palliative care among them (Wu et al., 2020). Similarly, a study conducted in Guangxi province in China reported that nurses displayed moderate mean knowledge scores (Chen et al., 2022). However, previous studies focused only on localized areas. There is a lack of comprehensive studies that assess the overall knowledge level and spatial distribution of palliative care knowledge at a broader scale. Furthermore, most existing studies have examined the factors associated with healthcare provider knowledge based on demographic characteristics, while objective social factors have received limited attention. Yet, differences in regional development inevitably led to disparities in healthcare provision. Healthcare providers, as active participants in the healthcare system, are influenced by various social objective factors that shape their knowledge levels. Moreover, the equitable allocation of healthcare resources is reflected in the quality of care, which can be partially captured through knowledge levels. Consequently, two critical research questions are expected to be addressed in the current paper: What is the spatial distribution of healthcare provider knowledge levels in China within the field of palliative care? What objective factors are associated with this distribution?
Therefore, this study aims to address these gaps by conducting a novel large-scale empirical investigation to comprehensively measure healthcare provider knowledge in palliative care, utilizing a localized scale developed by our research team (Shu et al., 2021). Additionally, based on the unique investigation and the representativeness dataset, we will innovatively analyze the spatial distribution characteristics of healthcare provider knowledge using spatial statistics theory, which will break through the limitations of focusing only on localized areas in previous studies. Furthermore, we will examine the social objective factors associated with healthcare provider knowledge in palliative care, which will overcome the constraints of being limited to demographic characteristics in previous studies. By undertaking this study, we aim to enhance the understanding of healthcare provider knowledge in palliative care and pave the way for targeted interventions and improved service delivery in various areas with the greatest need.
Methods
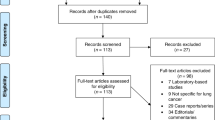
Study design and sampling
We conducted a robust cross-sectional study using a localized scale developed by our research team, which has demonstrated good reliability and validity (Shu et al., 2021). The knowledge assessment scale comprised 15 multiple-choice questions, each offering three to five options, with only one correct answer. Participants were assigned a score of one for selecting the correct option and zero for selecting any other option. The total scores ranged from 0 to 15, with higher scores indicating a higher level of knowledge. To analyze the associated factors, data were obtained from the 2021 China Health Statistics Yearbook. Based on a thorough literature review and data availability, economic factors (GDP per capita and disposable income per capita), demographic factors (population density, proportion of population aged 65 and above, and average life expectancy), and health factors (number of hospitals per 10,000 population, number of primary health care institutions per 10,000 population, number of health personnel per 10,000 population, number of health technicians per 1000 population and number of health technicians per 1000 population) were included in the analysis. Each factor was operationalized as a Z-score.
Figure 1 depicts the distribution of palliative care pilot cities in China. To obtain a systematic and comprehensive understanding of healthcare provider knowledge, we employed a multi-stage stratified sampling approach. In April 2021, an anonymous online questionnaire was administered to a total of 9 selected medical and health institutions in each of the 87 pilot cities (districts) across 29 provinces in China. These institutions encompassed various healthcare settings such as hospitals, community health service centers, township health centers, and nursing homes. Within each institution, we selected 20 certified physicians, nurses, health technicians, and administrators to participate in the questionnaire survey, ensuring a diverse representation of healthcare providers.
Statistical methods
Theoretical basis
Knowledge–Attitude–Practice (KAP), one of the most commonly used behavioral intervention theories, is used in this study to explain how knowledge affects behavior (Paço and Lavrador, 2017; Wang and Zhang, 2021). KAP theory suggests that change in human practice is a gradual process involving the acquisition of knowledge, the subsequent generation of positive attitudes, and finally, the adoption of practice (Singh et al., 2021). In this theory, behavioral change is divided into three successive periods, namely, the stage of acquiring knowledge, changing attitudes, and gradual formation of behaviors, in which knowledge actually refers to the cognitive situation of the relevant knowledge. Therefore, based on KAP theory, this study was conducted to examine the level of palliative care knowledge among healthcare providers.
Procedures
Provincial administrative districts were used as research units in this study. The average of the palliative care knowledge scores of all healthcare providers in a province was used to represent the average level of the province. Firstly, descriptive analysis was performed. Secondly, based on spatial statistics theory, the spatial autocorrelation of healthcare provider knowledge in palliative care was assessed. Then, Exploratory Regression was applied to assess all possible combinations of candidate explanatory variables, aiming to identify the ordinary least squares (OLS) model that best explained the knowledge level. Finally, based on the most appropriate OLS model, the factors that reached statistical significance were incorporated into the geographically weighted regression (GWR) model. Table 1 presents the candidate explanatory variables used in the exploratory regression analysis.
The methods and procedures used in this study are less commonly used in existing research. The main application in the medical field is in the epidemiological study of diseases. Specifically, the methods and procedures can be used to study the spatial distribution of diseases and their associated determinants to provide a basis for decision-making in public health interventions. This procedure was used by Kauhl et al. to study the spatial distribution of Hepatitis C Virus infections and associated determinants in the southern area of the Netherlands (Kauhl et al., 2015). However, the procedure of this study has not yet been applied in the field of health utility management. This may result from the barriers between disciplines. The application of the procedure in this area may open new avenues for future research related to the management of healthcare providers in palliative care and the allocation of human resources for health.
Description
Continuous variables were summarized as means and standard deviations (SD), while categorical variables were presented as numbers and percentages. To visualize the nationwide distribution of healthcare provider knowledge, a knowledge distribution map was created to provide a geographical representation of the findings.
Spatial autocorrelation
Spatial autocorrelation analysis was conducted, which enables the examination of statistical relationships between attribute values considering the spatial arrangement of geographic features. To assess the spatial autocorrelation of healthcare provider knowledge in palliative care, both Global Moran’s I (Moran and Patrick, 1950) and Local Moran’s I (also known as local indication of spatial autocorrelation, LISA) (Anselin, 1995) were employed. The Global Moran’s I index ranges from −1 to 1, where a value close to 1 indicates a significant positive spatial autocorrelation, while a value near −1 suggests a strong negative spatial autocorrelation. The formulas for calculating Global Moran’s I and Local Moran’s I are as follows (Xiao et al., 2015):
In this formula: n is the number of areas in this study; \({w}_{ij}\) is the spatial weight matrix; \({x}_{i}\) and \({x}_{j}\) are the healthcare provider knowledge of palliative care in area i and area j; and \(\overline{x}\) is the average value of healthcare provider knowledge of palliative care.
Exploratory regression
Exploratory regression evaluates all possible variable combinations that form a properly specified OLS regression model (Kauhl et al., 2015). When there are multiple exposure variables in a study and all of these variables are reported to significantly influence the dependent variable, it can be difficult to find an OLS model that meets all the conditions. Exploratory regression is able to traverse all combinations of exposure variables to find optimal combinations of driving factors without multicollinearity and data redundancy (Feng and Tong, 2017).
Geographically weighted regression
As an extension of the ordinary linear regression model, Geographically Weighted Regression (GWR) (Brunsdon et al., 1998) incorporates the spatial location of data into the regression equation, taking the local effects of spatial objects into account. GWR specifies that the regression coefficients vary over observations as (Fotheringham et al., 2003):
In this formula: \({{y}}_{{i}}\) is healthcare provider knowledge of palliative care in area i; \(({u}_{i},{v}_{i})\) is the spatial coordinate of area i; \({{x}}_{{ki}}\) is the observation of the independent variable xk in area i; \({\beta }_{0}({u}_{i},{v}_{i})\) and \({\beta }_{{j}}({u}_{i},{v}_{i})\) are the constants and coefficient in area I, respectively; and \({\varepsilon }_{{i}}\) is the random error.
Results
Spatial pattern of healthcare provider knowledge of palliative care
Among the 87 palliative care pilot cities spread across 29 provinces in China, a total of 18,272 participants were recruited from 903 institutions, of which 18,151 responses were valid without missing values. The average knowledge score (mean ± SD) was 8.61 ± 2.85 with a correct rate of 57.40%, indicating a relatively low level. The spatial pattern of healthcare provider knowledge in palliative care is illustrated in Fig. 2, with darker areas indicating a higher level of palliative care knowledge among healthcare providers. Jiangsu, Guangxi, and Shanghai emerged as the top three provinces with the highest knowledge levels. The Global Moran’s I index was 0.196 (P < 0.05), suggesting a spatial positive correlation in palliative care knowledge levels across the provinces in China. Figure 3 presents the local spatial autocorrelation clustering phenomenon for healthcare provider knowledge in palliative care. The LISA chart depicted significant high-high aggregation in Jiangsu, Zhejiang, and Shanghai, located in the east of China, while Jilin and Inner Mongolia, located in the east of China, exhibited low-low aggregation, indicating that physically close provinces tend to have similar knowledge levels.
Analysis of driving factors of healthcare provider knowledge of palliative care
According to the results of exploratory regression, the OLS model included several independent variables with the highest explanatory power, namely the proportion of population aged 65 and above, average life expectancy, number of hospitals per 10,000 population, number of primary health care institutions per 10,000 population, number of health technicians per 1000 population, and community health center visits. Table 2 provides the results of the OLS model, with an overall R2 of 0.5. Among the six variables, the number of hospitals per 10,000 population showed a negative association with healthcare provider knowledge of palliative care, while the number of primary healthcare institutions per 10,000 population and community health center visits exhibited a positive association.
Building upon the OLS model results, we incorporated the number of hospitals per 10,000 population, the number of primary healthcare institutions per 10,000 population, and community health center visits into the GWR model to explore the spatial distribution of regression coefficients. Figure 4 presents the outcomes of the GWR model, with an overall R2 of 0.44. It is evident that the number of hospitals per 10,000 population and the number of primary healthcare institutions per 10,000 population exert a stronger impact on healthcare provider knowledge in palliative care in the northwest regions compared to the southeast regions. Additionally, community health center visits have a greater influence on healthcare provider knowledge in palliative care in the northeast regions compared to the southwest regions.
A Spatial distribution of regression coefficients of number of hospitals per 10,000 population. B Spatial distribution of regression coefficients of number of primary health care institutions per 10,000 population. C Spatial distribution of regression coefficients of community health center visits. This shows the extent to which different associated factors influence the level of palliative care knowledge of healthcare providers in various provinces.
Discussion
This study represents a pioneering effort as, to the best of our knowledge, it is the first to investigate the knowledge of palliative care among healthcare providers across all provinces in China, with a large sample size. It provides valuable insights into the spatial distribution of healthcare provider knowledge of palliative care at the provincial level and identifies the factors associated with this knowledge. The findings reveal that the correct accuracy of healthcare provider knowledge of palliative care is only 57.40%, indicating that palliative care development in China is still in its early stages. These findings can serve as a reference for future research focusing on specific local areas or populations.
Based on KAP theory, having adequate knowledge among healthcare providers is crucial for delivering high-quality palliative services to patients. Their level of knowledge not only impacts their attitudes and practices but also plays a significant role in the overall development of palliative care services in society. While various professionals contribute to the palliative care service team (Fernando and Hughes, 2019; Mandel, 1993; Wang et al., 2023), healthcare providers are the primary individuals responsible for its implementation (Wu et al., 2016). Moreover, the cultural background in China has led to a limited understanding and acceptance of palliative care among the general public, which may affect the availability of palliative care services (Tam et al., 2021; Xie et al., 2020). As healthcare providers have the most direct contact with dying patients, their advice and recommendations heavily affect patients’ medical decisions and referrals. Therefore, it is essential for healthcare providers to receive targeted education about the tasks and benefits of palliative care in their regular practice (Collins et al., 2020). They can play a pivotal role in raising public awareness and promoting the importance of palliative care. The study highlights a significant knowledge gap among healthcare providers in palliative care, which can be attributed to the lack of comprehensive palliative care education. Teng et al. showed that healthcare providers demonstrated insufficient knowledge of palliative care, especially related to psychological care, the management of pain and other symptoms, and the application of traditional Chinese medicine (Teng et al., 2022). Previous studies have shown that training programs improve the knowledge and practice of healthcare providers in palliative care (Hao et al., 2021; Kim et al., 2020; Pelayo et al., 2011). Therefore, in order to enhance healthcare provider knowledge and practice of palliative care across the nation, it is crucial to implement more interventions and training programs. These efforts will contribute to improving the overall quality of palliative care services, meeting the growing demand for such care, and reducing health disparities in China.
The allocation of healthcare provider knowledge of palliative care exhibits a clear variation across space, suggesting the presence of regional disparities in the development of palliative care services. Moreover, the healthcare provider knowledge also demonstrates a positive spatial autocorrelation. The World Health Organization (WHO) advocates for the integration of palliative care strengthening into a country’s commitment to enhancing primary health care (PHC) and achieving universal health coverage (UHC) (WHO, 2021). UHC has become a key priority for numerous countries worldwide (Sachs, 2012), and China has explicitly prioritized health on a national level (The Lancet, 2016). Over the past few years, the Chinese government has introduced various health policies aimed at improving the overall health status of the population. One notable initiative is the approval of the Healthy China 2030 plan in 2016, which emphasizes the provision of equitable, accessible, systematic, and continuous health services with a focus on the entire population and the complete life cycle (China, 2016). This life cycle approach encompasses health promotion from fetal development to the end of life. Therefore, ensuring equity and accessibility to palliative care services at the end of life is crucial, as they are an integral part of the overall life cycle. The knowledge level of healthcare providers, who represent a vital human resource, serves as a significant reflection of the level of palliative care development (Chu et al., 2022). The sociality of healthcare providers suggests that health policies, lifestyles, cultural practices, and other variables may have an impact on the positive geographical correlation in knowledge levels of palliative care shown in this study. Due to population movements, similar environments, and common climates, neighboring provinces often influence each other. In fact, this also aligns with Tobler’s First Law of Geography—“everything is related to everything else, but near things are more related than distant things (Tobler and Waldo, 1970).” Palliative care has garnered significant attention and impact from society as a livelihood concern and public policy topic. As a result, the emergence of palliative care is a complicated phenomenon impacted by a wide range of intricate elements both inside and outside the healthcare system.
Despite China’s ongoing efforts to enhance equity and accessibility in healthcare services, the actual provision of healthcare is significantly influenced by social conditions and factors. The study findings reveal that the number of hospitals per 10,000 population, the number of primary healthcare institutions per 10,000 population, and community health center visits are associated with the level of healthcare provider knowledge in palliative care. Specifically, a higher number of primary healthcare institutions per 10,000 population and increased community health center visits positively correlate with greater palliative care knowledge among healthcare providers, while a higher number of hospitals per 10,000 population is negatively associated with palliative care knowledge. These findings align with the World Health Organization’s recommendation for the decentralization of palliative care services to the home and community (WHO, 2018). Currently, community health centers serve as the primary providers of palliative care in China (Li et al., 2022), which could explain the results observed in the OLS model. In our study, the term “hospitals” encompasses general hospitals, traditional Chinese medicine hospitals, combined Chinese and Western medicine hospitals, ethnic hospitals, specialty hospitals, and nursing homes while excluding primary healthcare institutions. Compared to hospitals, healthcare providers working in primary healthcare institutions have more opportunities to engage with palliative care services (Commission, 2022). Therefore, areas with a higher number of primary healthcare institutions and greater community health center visits tend to have healthcare providers with higher levels of palliative care knowledge (Teng et al., 2022). Conversely, in regions with a higher concentration of hospitals, healthcare providers are more focused on disease treatment, resulting in relatively lower levels of palliative care knowledge. Besides, government documents clearly state that, in addition to providing patients with basic services such as symptom control and comfort care, palliative care is also required to provide patients with condition assessment, psychological counseling, nutritional guidance, and other service items (China, 2017a, 2017b). However, in the context of China’s current widespread pilot DRG/DIP in secondary and tertiary hospitals, palliative care service projects involving psychological, spiritual, and social support have become a bottleneck restricting the sustainable development of palliative care because of the lack of a clear basis for charging fees and the failure to reflect the value of labor, which affects the motivation of healthcare institutions and healthcare providers to provide services (Duckett, 2018). Furthermore, the analysis of the GWR model also reveals a spatial distribution of regression coefficients that gradually changes across space which indicates the existence of spatial heterogeneity. The regions where the three factors included in the GWR model have a significant impact on healthcare provider knowledge levels are predominantly located in the northwest and northeast regions. This indicates that the number of different types of medical institutions exerts a greater influence on the level of palliative care knowledge among healthcare providers in these areas. This may be attributed to the sparser population and smaller number of diverse medical institutions in these regions, causing variations in their numbers to have a more pronounced marginal effect on healthcare providers’ palliative care knowledge levels.
While community health centers play a crucial role in providing palliative care services, it is important to recognize that certain services require the expertise and support of specialists and departments due to factors such as personnel qualifications, training, and the availability of specialized equipment and drugs (Lockman et al., 2022). Therefore, hospitals are expected to incorporate the principles and concepts of palliative care into their ward services and establish a coordinated mechanism with palliative care wards in community health service centers. This integration and collaboration between hospitals and community health centers can effectively enhance the overall quality of palliative care services and establish a well-functioning palliative care service system. In addition to the collaboration between healthcare institutions, policymakers at both national and regional levels should also consider adjusting the distribution of different types of healthcare institutions based on the specific needs and circumstances of each area. It is essential to establish a reliable referral system that ensures seamless transitions between different levels of healthcare providers. Furthermore, efforts should be made to enhance the understanding of palliative care among healthcare providers and raise public awareness about palliative care. These measures will contribute to the overall improvement of palliative care services and facilitate the establishment of a comprehensive and effective palliative care system.
Conclusion
To the best of our knowledge, this study innovatively investigates palliative care knowledge among healthcare providers across all provinces involved in pilot programs in China. An investigation with a large sample size was conducted, and the results were discussed from the disparity perspective, enhancing the generalizability and robustness of the findings. Previous studies tended to examine the factors associated with healthcare provider knowledge based on demographic characteristics, while objective social factors have received limited attention. Using GIS technology, the results shed light on the relatively low level of palliative care knowledge among healthcare providers, emphasizing the need for systematic training programs. Furthermore, the geographical variation in healthcare provider knowledge of palliative care suggests the existence of regional inequities in palliative care services. The study found that a higher knowledge level was associated with fewer hospitals and more primary healthcare institutions and community health center visits. Notably, these associations were particularly pronounced in the northwest and northeast regions, indicating the importance of tailored interventions targeting the specific needs of these local areas. However, this study may have a bias in the representation of provinces due to the uneven distribution of pilot areas, although 29 out of 31 provinces have been included in the analysis with a large representativeness. Besides, further studies with more associated factors are warranted to examine the availability of palliative care.
Data availability
The data that support the findings of this study can be provided by the corresponding author, upon reasonable request.
References
Anselin L (1995) Local indicators of spatial association—LISA. Geogr Anal 27(2):93–115
Brunsdon et al. (1998) Geographically weighted regression. J R Stat Soc: Ser D (Statistician) 47(3):431–443
Chen L et al. (2022) Nurses’ knowledge, attitudes, and willingness to practice hospice care: An analysis of influencing factors. PLoS ONE 17(2):e0259647. https://doi.org/10.1371/journal.pone.0259647
China CPGO (2016) The CPC Central Committee and the State Council issued the “Health China 2030” plan, vol 2022. China CPGO
China NHCO (2017a) Notice on the pilot work of palliative care, vol 2023. China NHCO
China NHCO (2017b) Notice on Issuance of palliative care practice guidelines (Trial), vol 2017. China NHCO
China NHCO (2019) Notice on launching the second batch of palliative care pilot work, vol 2023. China NHCO
Chu T et al. (2022) Predicting the behavioral intentions of hospice and palliative care providers from real-world data using supervised learning: a cross-sectional survey study. Front Public Health 10:927874. https://doi.org/10.3389/fpubh.2022.927874
Collins A, McLachlan SA, Philip J (2020) Community knowledge of and attitudes to palliative care: a descriptive study. Palliat Med 34(2):245–252. https://doi.org/10.1177/0269216319888371
Commission SMH (2022) Reply to No. 0628 proposal of the sixth session of the 15th Municipal People’s Congress, vol 2023. Commission SMH
Duckett S (2018) Aligning policy objectives and payment design in palliative care. BMC Palliat Care 17(1):42. https://doi.org/10.1186/s12904-018-0294-4
Fang EF et al. (2015) A research agenda for aging in China in the 21st century Ageing Res Rev 24(Part B):197–205. https://doi.org/10.1016/j.arr.2015.08.003
Feng Y, Tong X (2017) Using exploratory regression to identify optimal driving factors for cellular automaton modeling of land use change. Environ Monit Assess 189(10):515. https://doi.org/10.1007/s10661-017-6224-8
Fernando G, Hughes S (2019) Team approaches in palliative care: a review of the literature. Int J Palliat Nurs 25(9):444–451. https://doi.org/10.12968/ijpn.2019.25.9.444
Fotheringham AS, Brunsdon C, Charlton M (2003) Geographically weighted regression: the analysis of spatially varying relationships. John Wiley & Sons
Hao Y et al. (2021) Nurses’ knowledge and attitudes towards palliative care and death: a learning intervention. BMC Palliat Care 20(1):50. https://doi.org/10.1186/s12904-021-00738-x
Kauhl B et al. (2015) The spatial distribution of hepatitis C virus infections and associated determinants–an application of a geographically weighted Poisson regression for evidence-based screening interventions in hotspots. PLoS ONE 10(9):e0135656. https://doi.org/10.1371/journal.pone.0135656
Kim S, Lee K, Kim S (2020) Knowledge, attitude, confidence, and educational needs of palliative care in nurses caring for non-cancer patients: a cross-sectional, descriptive study. BMC Palliat Care 19(1):105. https://doi.org/10.1186/s12904-020-00581-6
Li X, Kongsuwan W, Yodchai K (2022) Attitude toward care of the dying and practice of peaceful end-of-life care in community hospitals in China. Int Nurs Rev 70(3):345–354. https://doi.org/10.1111/inr.12812
Lockman K et al. (2022) Development of entrustable professional activities for specialist hospice and palliative care pharmacists. J Pain Symptom Manag 64(1):37–48. https://doi.org/10.1016/j.jpainsymman.2022.03.004
Mandel SE (1993) The role of the music therapist on the hospice/palliative care team. J Palliat Care 9(4):37–9
Moran, Patrick AP (1950) Notes on continuous stochastic phenomena. Biometrika 37(1/2):17–23
Paço A, Lavrador (2017) Environmental knowledge and attitudes and behaviours towards energy consumption. J Environ Manag 197:384–392. https://doi.org/10.1016/j.jenvman.2017.03.100
Pelayo M et al. (2011) Effects of online palliative care training on knowledge, attitude and satisfaction of primary care physicians. BMC Fam Pract 12:37. https://doi.org/10.1186/1471-2296-12-37
Sachs JD (2012) Achieving universal health coverage in low-income settings. Lancet 380(9845):944–7. https://doi.org/10.1016/S0140-6736(12)61149-0
Shu Z et al. (2021) Instrument development of health providers’ Knowledge, Attitude and Practice of Hospice Care Scale in China. Int J Health Plann Manag 36(2):364–380. https://doi.org/10.1002/hpm.3074
Singh V et al. (2021) Impact of video modules-based training on knowledge, attitude, and practices of cleaning and disinfection among housekeeping staff at a tertiary care center during the COVID-19 pandemic. Cureus 13(10):e19125. https://doi.org/10.7759/cureus.19125
Tam KI et al. (2021) Knowledge of palliative care and preference of end of life care: a cross-sectional survey of residents in the Chinese socio-cultural background of Macao. BMC Palliat Care 20(1):87. https://doi.org/10.1186/s12904-021-00798-z
Teng X et al. (2022) Healthcare provider knowledge, attitudes, and practices in hospice care and their influencing factors: a crosssectional study in Shanghai. Int J Health Policy Manag 11(12):3090–3100. https://doi.org/10.34172/ijhpm.2022.6525
The Lancet (2016) The best science for achieving Healthy China 2030. Lancet 388(10054):1851. https://doi.org/10.1016/S0140-6736(16)31842-6
Tobler, Waldo R (1970) A computer movie simulating urban growth in the Detroit region. Econ Geogr 46(supply 1):234–240
Wang J et al. (2023) Volunteers’ spiritual care competence and its relationship with attitudes toward palliative care: a cross-sectional study. Palliat Support Care 13:1–7. https://doi.org/10.1017/S1478951523000123
Wang K, Zhang L (2021) The impact of ecological civilization theory on university students’ pro-environmental behavior: an application of knowledge–attitude–practice theoretical model. Front Psychol 12:681409. https://doi.org/10.3389/fpsyg.2021.681409
WHO (2018) Integrating palliative care and symptom relief into primary health care: a WHO guide for planners, implementers and managers. World Health Organization, Geneva
WHO (2021) Assessing the development of palliative care worldwide: a set of actionable indicators. World Health Organization, Geneva
Wu X et al. (2020) Analysis of knowledge, attitude and behavior of oncology medical staff in palliative care. Ann Palliat Med 9(3):985–992. https://doi.org/10.21037/apm-20-851
Wu Y et al. (2016) Hospice and palliative care: development and challenges in China. Clin J Oncol Nurs 20(1):E16–E19. https://doi.org/10.1188/16.CJON.E16-E19
Xiao R et al. (2015) Quantifying determinants of cash crop expansion and their relative effects using logistic regression modeling and variance partitioning. Int J Appl Earth Obs Geoinf 34:258–263. https://doi.org/10.1016/j.jag.2014.08.015
Xie Y et al. (2020) Investigation of the awareness of and demand for hospice care and attitudes towards life-sustaining treatment at the end of life among community residents in Hangzhou. BMC Palliat Care 19(1):128. https://doi.org/10.1186/s12904-020-00628-8
Zhu S et al. (2021) Care needs of dying patients and their family caregivers in hospice and palliative care in mainland China: a meta-synthesis of qualitative and quantitative studies. BMJ Open 11(11):e051717. https://doi.org/10.1136/bmjopen-2021-051717
Acknowledgements
This work was supported by Shanghai Science and Technology Commission, Natural Science Foundation (NO. 22ZR1461400), Shanghai Science and Technology Commission, Soft science Research Project of Science and Technology Innovation Action Plan (NO. 23692112700), and Ministry of Education, Humanities and Social Sciences Planning (NO. 20YJAZH045).
Author information
Authors and Affiliations
Contributions
JW, SS, and GM: Data analysis and manuscript writing. XT, YX, ZS, and XZ: Data collection. LJ and JS: Study supervision. LJ: Study design, revision, administration, and resources. JW, SS and GM have contributed equally to this work and share first authorship. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The design of the study and participants’ selection were approved by the ethical review committee of Ninth People’s Hospital Affiliated to Medical School of Shanghai Jiaotong University (NO. SH9H-2021-T11-1). The study was conducted in accordance with the Declaration of Helsinki.
Informed consent
The respondents were told in advance about the anonymous investigation and informed consent was obtained.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, J., Song, S., Mai, G. et al. The comparison of spatial patterns and factors associated with healthcare provider knowledge in palliative care in various regions of China. Humanit Soc Sci Commun 11, 510 (2024). https://doi.org/10.1057/s41599-024-02998-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1057/s41599-024-02998-3