Abstract
Adoption of a health information system is always a challenge for hospitals. It is because most of the medical staff do not have enough skills to use the new technology and due to the sensitivity of medical data. These factors pose a challenge for the successful adoption of health information system in hospitals. The aim of this research is to find out the factors which influence the adoption of information systems in hospitals. The study investigated the impact of the Financial status of the Hospital; Perceived Usefulness and Perceived Ease of Use on the adoption of health information systems through a questionnaire survey. Data was collected from 602 healthcare workers from 20 hospitals through close-ended questionnaire in Pakistan, where the adoption of health information systems is very slow. PLS-SEM was used for the analysis. The findings show that the Financial status of the Hospital; Perceived Usefulness and Perceived Ease of Use have positive and significant role in the adoption of Health Information Systems. The finding also shows that hospital size moderates the relationship of Perceived ease of use and the adoption of health information systems and interestingly it does not moderate the relationship among perceived usefulness and financial strength toward the adoption of health information systems. The study concludes that perceived ease of use, perceived usefulness and financial strength are the main factors, necessary for the adoption of health information systems. The findings of the study have useful implications for policy makers, medical professionals to successfully adopt health information systems in hospitals. It also provides new avenues for researchers to explore other factors and test this framework in other countries.
Similar content being viewed by others
Introduction
Digitalization and the adoption of new technologies are irrevocable phenomena across the globe. Organizations are shifting toward the use of the latest technologies, either for competitive advantage or to operate efficiently (Bloomberg, 2018). From education (Ahmad et al. 2021, 2022) to the supply chain (Khan et al. 2022a), from business organizations (Broccardo et al. 2023) to healthcare sectors (Stachwitz and Debatin 2023), all are embracing this technological change. COVID-19 significantly influenced the adoption of technologies for the smooth running of organizations and the health sector is one of them (Ndayishimiye et al. 2023). It is important to understand that efficient utilization of resources is one of the main objectives of sustainable development goals. And the new technology is one of the means to contribute to sustainable development through paperless operations, according to the tasks of the organization (Xiong 2021). For every organization, data collection, record keeping, storage, and utilization are some of the main tasks, and traditionally, these tasks were not possible without paper, facilities, and dedicated human resources but now they can be done with the help of information systems (IS). In hospitals, IS digitally stores patient records, provides instant access to the right people and improves the interactions between doctors and patients (Ohio University, 2020). The IS used by healthcare organizations is known as Health Information System (HIS). Nowadays, hospitals are adopting HIS for-patient records, storage, and easy access for the medical staff. In addition to patient records, HIS also records and stores data related to hospital facilities like wards, operating rooms, etc. (Sinhasane 2022). This minimizes the utilization of resources and increases the outcomes. Due to its benefits, many countries are now regulating the health sector to adopt HIS in hospitals.
The adoption of HIS has become an essential in the rapidly evolving healthcare landscape, offering opportunities for increased effectiveness, improved outcomes for patients, and more efficient healthcare delivery. In Pakistan especially, hospitals are facing difficulties in the adoption of HIS and understanding the factors impacting the adoption becomes essential (Malik et al. 2021). Major challenges are the unavailability of adequate infrastructure, especially in remote areas where power supplies and internet connectivity are irregular (Shahzad et al. 2021). The adoption of HIS also requires initial investments and ongoing maintenance expenditures, which are hindered by financial constraints, i.e., limited budget and resource. Similarly, healthcare employees also resist the adoption of HIS and fears about job displacement and disruptions to workflow. The adoption of technology has also attracted many researchers and academicians to find out the factors that are necessary for the adoption of new technology (Davis 1989; Brown et al. 2010; Turel et al. 2011; Venkatesh et al. 2012; Abbas et al. 2017; Ibrahim et al. 2014, 2015; Sayed et al. 2020; Khan et al. 2022b; Liu et al. 2022) to name a few.
This study explores the complex interactions of perceived usefulness (PU), perceived ease of use (PEU), and financial strength as essential factors influencing the adoption of HIS in Pakistan. The study also adds a moderator, hospital size to further enhance the significance of the research by recognizing the contextual realities that hospitals of different sizes face during the HIS adoption. All these factors were taken from technology theories like Technology Acceptance Model (TAM) (Davis 1989) and Resource-Based View Theory (RBV) (Barney 1991). PU is the user’s belief that using HIS will improve their performance, PEU represents the perceived ease of system interaction, and financial strength represents the economic resilience, influencing its ability to fund and maintain the adoption of HIS (Nezamdoust et al. 2022). The objective behind investigating the complex relationships among these variables is to find out the complex dynamics that influence the adoption of HIS decision-making. Although these factors are known to be important in the adoption of technology, there still exists a gap regarding their combined effects, especially when considering different hospital sizes (Zaman et al. 2022). There is also limited work done so far on HIS adoption in the context of Pakistan. To fill the gap, this study examines the relationship between PU, PEU, financial strength and the moderating impact of hospital size in the adoption of HIS. Despite the fact that HIS provides many benefits for healthcare professionals and delivery, the adoption is too slow in Pakistan. And it is necessary to find out the factors which hinders this adoption. The study has the following objectives:
-
(1)
To find out the relationship between financial strength and HIS adoption.
-
(2)
To find out the relationship between perceived ease of use and HIS adoption.
-
(3)
To find out the relationship between perceived usefulness and HIS adoption.
-
(4)
To find out the moderating role of hospital size on the relationship between financial strength, PU and PEU toward the adoption of HIS.
The study has significance for technology developers, legislators, and healthcare professionals especially for the development, and adoption of HIS. It will facilitate the healthcare industry to develop well-informed strategies from HIS adoption according to the healthcare landscape.
Literature review
Theories
The development of the theoretical framework is based on two theories: Technology acceptance model (TAM) and the Resource-based view (RBV). According to these theories, a hospital’s financial health, perceived ease of use and perceived usefulness of a HIS have a significant impact on its adoption. These relationships may be moderated the hospital’s size, as bigger hospitals with more users and stronger financial resources may find the adoption of HIS easier and useful than smaller hospitals.
Technology acceptance model
A popular theory regarding the acceptance and utilization of technology is the TAM. It suggests that crucial elements influencing the acceptability and adoption of technology are perceived ease of use and perceived usefulness (Davis 1989). Perceived usefulness is the extent to which people think employing a certain technology would improve their productivity. In a hospital setting, employees are more inclined to adopt a health information system (HIS) if they believe it would increase their productivity, improve patient care, or facilitate operations. Therefore, people having a positive perception about the HIS usefulness are more likely to adopt it. The extent to which people believe a certain technology will be user-friendly and effortless is known as perceived ease of use. The adoption of HIS will be influenced if the employees believe that it is easy to use, and incorporate into the current workflow of the hospital. Peoples are more likely to adopt the HIS if they believe it is easy to use.
Resource-based view (RBV)
The RBV emphasize on the importance of resources and competencies in an organization. It implies that a company’s resources, such as its financial resources, can affect how well it adopts and applies new technology (Barney 1991). Hospitals will invest on a HIS adoption according to their financial status. Better-funded hospitals could have more money available to spend on the purchase, and adoption of a HIS. They can also allocate funds for investing in hardware and software, training employees, and recruiting IT specialists. Therefore, compared to hospitals with low financial resources, those with better financial standing are more likely to adopt and implement a HIS successfully. The association between financial situation, perceived usefulness, perceived ease of use, and HIS adoption is moderated by the hospital size. Larger hospitals typically have more financial resources and to put complex ISs in place and adopt new HIS. Additionally, they could have more staff and divisions that use the system, increasing its perceived usefulness. Smaller hospitals, on the other hand, may find it more difficult to adopt an HIS, despite their perceived ease of use and usefulness. These hospitals also tend to have fewer staff members and financial resources.
Adoption of information systems in healthcare
The adoption of ISs in healthcare is becoming a requirement as other industries embrace new technologies (Crisan and Mihaila 2023). Whether a healthcare organization wants it or not, it must implement and adopt information technology and software to plan its resources, store its records, easily extract data, make better decisions, and so on (Mahdi et al. 2023; Khanna et al. 2022; Dicuonzo et al. 2023). But the speed of adoption of IS is very low in the health sector as compared to other sectors (Hopper 2015). It is also important to highlight that the adoption of IS and other technologies is strongly linked to the financial strength of an organization (Wang et al. 2005). Healthcare organizations are rarely a source of income, but rather a provider of services, and if there is insufficient funding to provide other basic health services, the likelihood of investing in and adopting new IS becomes low in comparison to profit-generating organizations. Employees of healthcare organizations are frequently experts in providing health services but have little knowledge of the benefits and necessity of IS (Jarva et al. 2023). This also leads to the poor adoption of IS in the health sector (Hedayati and Schniederjans 2022). Similarly, the employees do not know the usefulness of technology, so they usually seem reluctant to adopt it in healthcare. To address these issues, it is necessary to provide guidance about the benefits and usefulness of IS to healthcare professionals (Alboliteeh et al. 2022) to increase the speed of IS adoption and make healthcare activities easy and simple.
Perceived ease of use
Perceived ease of use is one of the main factors in technology adoption (Almaiah et al. 2022). It is “the degree to which a person believes that using a particular system would be free of effort” (Davis 1989). Almost all researchers agree on the importance and role of PEOU in the adoption of technology. People adopt technology when they believe it is effort-free and will minimize their work (Alsyouf et al. 2023). The same is true for IS in a healthcare system. Employees and health organizations will be more accepting of an IS if it is expected to reduce user effort (Yulianto et al. 2022). If the employees perceive that the IS will not reduce their efforts, then they will be reluctant to adopt it. If the technology is complex to use and difficult for the employees to understand or learn to use (Rohani and Yusof 2023). They will never possess a positive attitude regarding its adoption. They will oppose the adoption of such an IS, even if it is beneficial for other tasks (Rey-Moreno et al. 2022). As a result, healthcare organizations must choose an IS that is perceived to reduce the effort required for individual routine tasks and make their work easier (Veikkolainen et al. 2023).
Perceived usefulness
Perceived usefulness (PU) is also critical for the adoption of technology (Park and Kim 2023). It is “the degree to which a person believes that using a particular system would improve their job performance” (Davis 1989). It is one of the agreed-upon factors for technology adoption. The important indicators for PU of technology are; its influence on task performance time, effort reduction, cost reduction, and general usefulness (Alsyouf et al. 2023; Renny et al. 2013). If the employees of a healthcare facility believe that the IS will reduce the time it takes to perform a task, reduce effort, reduce cost, and be generally useful for them, their attitude toward the adoption will be positive (Addotey-Delove et al. 2023). If they do not see any of the above elements, then they will be reluctant to adopt IS. Therefore, healthcare firms must choose an IS that is perceived to be useful according to the mentioned indicators (Sturmberg and Bircher 2019).
Financial strength
The size and financial resources of an organization have a significant impact on the adoption of new technologies (Kim et al. 2011). A key deciding factor is the organization’s ability to cover the installation and any improvement expenses of technology (Kuan and Chau 2001). Financially weak organizations hesitate to invest in new technology and are overcautious in making such decisions (Mousa and Bouraoui 2023; Endriyas et al. 2023). They are unable to take risks and adopt new technology as they are aware of the consequences and believe any failure may lead to their economic failure (Cheng et al. 2023; Singerman and Lence 2023). Because new technologies necessitate long-term investment and high IT setup costs, organizations with significant financial resources encourage their adoption (LaBerge 2020; Philibert 2003). As a result, only firms with adequate financial resources are able to embrace new technology. In the context of this study, healthcare centers or hospitals that are financially stable will be more likely to adopt IS compared to weaker ones. They can provide funds for the adoption of IS and can also take the risk of failure due to their financial strength. Those healthcare facilities that are financially weak will hesitate to adopt IS because of a lack of money and the risk they cannot afford (Vassolo et al. 2021; McAdory 2021).
Size of the hospital
The size of organizations or firms influences the adoption of new technology (Salah et al. 2021). Not every organization wants or can afford to adopt new technology (Lind et al. 1989). There are multiple reasons for this, like the fact that big organizations have more resources and are generally financially stronger than smaller ones (Dewar and Dutton 1986). As a result, they can invest in technology while also taking risks (Lee and Xia 2006). Smaller firms prefer less risky technological adventures (Shahadat et al. 2023). Similarly, employees have to perform a lot of tasks and exert effort in larger organizations than in some organizations. They possess more positive attitudes toward the adoption of technology, as they believe it will reduce their efforts as compared to the employees in smaller firms (Prasad 2018). Likewise, employees in large organizations expect more positive attitudes toward the usefulness of new technology than those in smaller ones (Lind et al. 1989). In other words, the adoption of IS healthcare is influenced by the size of the hospital.
Theoretical mechanism and hypotheses
The foundation of the study is based on the Integration of the TAM and the RBV. These theories provide understanding about the complex dynamics that influence the HIS adoption. The key concepts of TAM are PU and PEOU, both regarded as critical drivers for acceptance and use of technology (Pufahl et al. 2022). When it comes to adopting HIS, healthcare professionals critically evaluate the usefulness of the system in improving workflow, decision-making in healthcare services. PU is especially important in healthcare, since HIS directly impact patient outcomes and the standard of care. Stakeholders can assess how well the HIS meets their professional requirements and improves healthcare (Akther and Nur 2022). A HIS that simplifies the management of patient data, expedites decision-making, and improves communication between healthcare practitioners could be considered useful. Furthermore, PEU is another key factor for HIS adoption. The PEU of the HIS is crucial in healthcare where time is very important for various tasks. A user-friendly design, and easy operation all help to create an appealing sense of usefulness and encourage people to adopt the technology (Nezamdoust et al. 2022).
In addition to TAM, RBV focuses on the strategic and competitive role of organizational resources (Tseng et al. 2022; Tortorella et al. 2022). When considering the implementation of HIS, financial strength becomes an essential factor. Hospitals with adequate funding have a stronger position to purchase cutting edge HIS. They can support training, maintenance, and upgrades to the system beside the initial implementation costs. In addition, RBV also underscores the importance of finance in hiring and retaining HIS experts.
The HIS adoption is not universal for all size hospitals. This theoretical structure adds a more complex layer in the form of the hospital size as a moderating variable. Hospitals of different sizes face unique challenges during the HIS adoption process. For example, large hospitals may have financial resources but their complex organizational structure may have impacted the HIS adoption decision and process. This makes the PU more critical, because it is essential that it must be able to meet a variety of professional demands and improve organizational efficiency. However, smaller hospitals have exclusive challenges because of limited funding and they may be not capable to invest in expensive HIS implementation. In situations like this, people typically prefer PEU more, as simple and affordable solutions with little training requirements. It might be also easy for smaller hospitals to adopt changes due to simple organizational structure.
HIS adoption cannot be understood in the absence of the interaction between PU, PEU and financial strength of hospitals, and the size of the hospital. PEU could be particularly important in smaller hospitals with limited resources. The HIS’s PEU remain a crucial factor in overcoming resource limitations and promoting its adoption among medical practitioners. Larger hospitals due to huge financial resources may customize the HIS according to their need to enhance its PU and optimize its impact. They can also invest in training to equip healthcare professionals for the potential use of HIS, and continuously improve and adapt HIS.
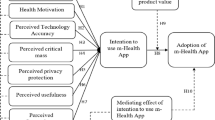
To sum up, the combination of TAM and RBV offers a thorough theoretical base for comprehending the complex aspects of HIS adoption, with particular focus on PU, PEU and financial strength of a hospital. The hospital size as a moderator, emphasize on the necessity for customized solutions according to the challenges and requirements of the hospital. The aforementioned theoretical structure presents practical insights for hospitals trying to cope with the complex environment of HIS adoption. The framework as shown in Fig. 1 shows that there are six hypotheses, three of which are moderating ones. The first hypothesis as represented by H1 shows the relationship of financial capability/strength with the adoption of HIS. Similarly, the second hypothesis as represented by H2 shows the relationship of PEU with the adoption of HIS. Moreover, the third hypothesis as represented by H3 shows the relationship of PU with the adoption of HIS. In addition, there are three moderating hypotheses in the proposed theoretical framework. H4 represents the moderating role of the size of hospitals on the relationship between the financial capability/strength and the adoption of HIS. Similarly, H5 represents the moderating role of the size of hospitals on the relationship between the PEU and the adoption of HIS. Moreover, H6 represents the moderating role of the size of hospitals on the relationship between the PU and the adoption of HIS.
H1: FC has a positive relationship with HIS adoption.
H2: PEU has a positive relationship with HIS adoption.
H3: PU has a positive relationship with HIS adoption.
H4: The size of a hospital moderates the relationship between FC and HIS adoption.
H5: The size of a hospital moderates the relationship between PEU and HIS adoption.
H6: The size of a hospital moderates the relationship between PU and HIS adoption.
Methodology
Philosophy
The philosophical foundation of this study is rooted in the post-positivist paradigm. The post-positivism paradigm is a scientific paradigm that uses an objective inquiry approach to reality, considering the possible effect of the researcher’s biases. A deductive reasoning approach and a quantitative method were used to address the issue of the assumed reality.
Study population and scale
Despite the fact that HIS can benefit the healthcare sector, it’s adoption in Pakistan is very slow. The hospitals are facing difficulties in the adoption of HIS and understanding the factors impacting the adoption becomes essential for addressing the issue. This study was taken with the aims to find out the factors responsible for the slow adoption of HIS in Pakistan. A purposive sampling technique was employed to collect the primary data from the doctors and nurses in Pakistan’s healthcare sector. Data from 602 respondents was gathered via a closed-ended questionnaire using a five-point Likert scale. The respondents were selected from both the private and public sector hospitals across Pakistan. All the hospitals were general hospitals belonging to different geographical contexts of Pakistan. Data was gathered via a closed-ended questionnaire, which was floated through Google forms by the researcher’s different contacts. The questionnaire was composed of the scales adopted from the prior studies, considering their reliability and validity. Before collecting the data, a pilot survey was also conducted to confirm the validity of the questionnaire with a sample size of 120. After the pilot survey, all the validity and reliability measures were found to be sound, so this further survey was enhanced to cover the overall sample size. partial least squares technique with the help of SmartPLS was used to carry out the data analysis. All the constructs, except for the size of the hospital, were adapted from the prior studies, keeping in mind their reliability and validity to gauge the phenomenon more accurately. While the single-item construct for the size of the hospital was a self-made item by the researcher, it was used to evaluate the size of the respondent’s hospital on a five-point scale showing a very small hospital, a small hospital, a medium-sized hospital, a large hospital, and a very large hospital based on the number of beds. A hospital with less than ten beds was considered a very small hospital; a hospital with 10 to 20 beds was considered a small hospital; a hospital with more than 20 to 35 beds was considered a medium-sized hospital; a hospital with more than 35 to 50 beds was considered a large hospital; and a hospital with more than 50 beds was considered to be a very large hospital. Based on this size criteria, they were ordered from 1 to 5 on a Likert scale. The details of the items are given in Table 1.
General sample characteristics
Table 2 shows the demographic characteristics of the research respondents. The table shows that there were 602 total respondents for the said research. The first section of the table shows their gender distribution, indicating that 317 were males and 285 were females. The second section of the table indicates their age-wise distribution, which indicates that 130 were in the age group of 20–30 years, 268 were in the age group of 31–40 years, 168 were in the age group of 41–50 years, and the rest, 36, were above the age of 50 years. The third section of the table represents the resident country of the respondents. This section indicates that 602 were from Pakistan. The table’s fourth and last section shows the respondents’ designation. This section indicates that among the 602 respondents, 315 were medical doctors and 287 were nurses.
Results and findings
Measurement model
The measurement model includes the relationship of the overall construct with its respective items. Four common measures used for the measurement model when using a structural equation model are item reliability, construct reliability, convergent validity, and discriminant validity.
Reliability and convergent validity
Reliability means the degree to which the result of a measurement or calculation is accurate. Two common types of reliability used in the measurement model are item reliability and construct reliability. The outer loading values are used to assess item reliability, and Cronbach’s alpha and composite reliability are used to assess construct reliability. The threshold value for both reliability measures is 0.7, and a value of 0.6 is also acceptable if the basic criteria of convergent validity are established. Table 3 shows that all the reliability values are within the threshold value limit, indicating that the items’ and constructs’ reliability is established. The next measure for the measurement model is convergent validity, which means how closely a test relates to other tests that measure the same (or similar) constructs. The measure used for convergent validity is AVE. The threshold value for the AVE is 0.5 or above. Table 3 shows that all the constructs have an AVE value greater than the threshold value, indicating that all the constructs are convergently valid.
Discriminant validity
Discriminant validity specifically measures whether constructs are related or not. The Fornell–Larcker criteria, HTMT ratios, and cross-loading are all common measures for discriminant validity. But most social scientists recommend the Fornell–Larcker criteria and HTMT as the most robust measures for discriminant validity. Table 4 shows the Fornell–Larcker criteria for the model. The threshold value for the Fornell–Larcker criteria is that the diagonal square AVE values must be greater than the values of their respective columns and rows. Table 4 of the Fornell–Larcker criteria shows that all the diagonal values are greater than the values of their respective columns and rows, indicating that the constructs’ discriminant validity is established based on these criteria.
The second measure used for discriminant validity is HTMT ratios. The threshold value for the HTMT ratio is that all the HTMT values must be less than 0.85. Table 5 of the HTMT ratios shows the HTMT values of the constructs. Table 5 shows that all the values are smaller than the threshold range of HTMT, which indicates that the constructs have achieved their discriminant validity based on the HTMT scale.
Common method bias
The term “common method bias” refers to a spurious variance that attributes the measurement method rather than the construct that the measures are supposed to represent. It is a significant issue for researchers working with primary data. VIF values reflect the multicollinearity issue of the model and address the common method bias problem. If a model has VIF values less than 3.0, it indicates that the model is free from the issue of common method bias. Table 3 of the reliability, multicollinearity, and convergent validity shows that all the individual construct items have a VIF value less than the threshold value, indicating that the model is free from the issue of common method bias.
Structural model
Below Fig. 2 represents the study’s structural model, which indicates the relationship among all the variable of the study.
Hypothesis testing and regression analysis
Regression analysis is a very old statistical technique used to estimate the significance level of a cause-and-effect relationship between the two variables. Regression was first coined by the social scientist Francis Galton in the nineteenth century. Different techniques are used in the regression analysis: ordinary least square, Partial least square, most likelihood error estimation, etc. The ordinary least square is used for the secondary data, while the PLS and MLE are used for the primary data. Partial least square is used for the hypothesis testing on a model based on predetermined solid theories, while MLE is used for the model being tested for the first time; as this study is based on pre-developed theories, a partial least square technique was adopted to estimate the hypothesis. Table 6 shows the list of the hypotheses based on the model of this study and their significance level. The table shows six hypotheses, of which three are based on direct relationships, and the rest are based on moderate relationships. The measures used for a relationship’s statistical significance are the T and p values. The threshold value for the t value is 1.96 and above, while the threshold value for the p value is 0.05 or less. From Table 6, it was identified that, among the six hypotheses, four are statistically significant. At the same time, the other two are statistically insignificant, not meeting the basic requirements of the threshold values. While the beta value for each relationship shows the strength of that relationship. Interpretation of the hypothesis’s analysis, as shown in Table 6 are given below.
H1: FC has a positive relationship with HIS adoption.
The values of regression analysis show that there is positive and significant relationship between FC and the adoption of HIS with a β value of 0.16, a p value of 0.02, a t-statistic of 1.995. These values provide evidence that the assumption about the significant role of financial capability or strength in the adoption of HIS is positive and significant. In other words, FC positively influence the adoption of HIS.
H2: PEU has a positive relationship with HIS adoption.
The values of regression analysis show that there is positive and significant relationship between PEU and the adoption of HIS with a β value of 0.076, a p value of 0.044 and a t-statistic of 1.998. These values provide evidence that the assumption about the significant role of PEU in the adoption of HIS is positive and significant. In other words, PEU positively influence the adoption of HIS.
H3: PU has a positive relationship with HIS adoption.
The values of regression analysis show that there is positive and significant relationship between PU and the adoption of HIS with a β value of 0.254, a p value of 0.000 and a t-statistic of 4.16. These values provide evidence that the assumption about the significant role of PU in the adoption of HIS is positive and significant. In other words, PU positively influence the adoption of HIS.
H4: The size of a hospital moderates the relationship between FC and HIS adoption.
The values of regression analysis show that there is no positive and significant moderating role of hospital size exist on the relationship between FC and the adoption of HIS with a β value of −0.075, a p value of 0.213 and a t-statistic of 1.426. These values provide evidence that the assumption about the significant moderating role of hospital size on FC and HIS adoption is not significant. In other words, hospital size does not moderate this relationship.
H5: The size of a hospital moderates the relationship between PEU and HIS adoption.
The values of regression analysis show that there exist a positive and significant moderating role of hospital size on the relationship between PEU and the adoption of HIS with a β value of 0.101, a p value of 0.009 and a t-statistic of 2.618. These values provide evidence that the assumption about the significant moderating role of hospital size on PEU and HIS adoption is not significant. In other words, hospital size does not moderate this relationship.
H6: The size of a hospital moderates the relationship between PU and HIS adoption.
The values of regression analysis show that there is no positive and significant moderating role of hospital size exist on the relationship between PU and the adoption of HIS with a β value of 0.08, a p value of 0.283 and a t-statistic of 1.07. These values provide evidence that the assumption about the significant moderating role of hospital size on PU and HIS adoption is not significant. In other words, hospital size does not moderate this relationship.
Model fitness
In statistical modeling, model fit is essential because it directly affects the validity of inferences obtained from the data and the reliability of findings. For the model fitness, several measures are available in the SmartPLS, like the SRMR, Chi-square, NFI, etc., but most of the researchers recommend the SRMR for the model fitness in the PLS-SEM. When applying a structural equation model based on PLS, a value less than 0.08 is generally considered a good fit. Table 7 shows that the SRMR value is 0.068, which is less than the threshold value, which indicates that the model fitness has been achieved.
R square
R square is a measure used for the computation of the coefficient of determination, which explains how the combined effect of the independent variables causes variations in the dependent variable. R square is the collective effect of the variables, which also denotes the explanation power of the model. The greater the R square value, the better the model explanation power. A value of R square for the primary data greater than 10% is considered a reasonable explanation power. However, a value greater than 40% is considered good for the secondary data. Table 8 shows that the R square value for the said model is 0.126, indicating that the 12.6% variation on the dependent variable is due to the independent variables in this research model.
Predictive relevance of the model
Predictive relevance is an advanced tool used in the SmartPLS to detect the prediction power of a model. According to social scientists, a model with more than zero prediction power based on primary data is considered good. The measure used for the prediction power is Q square. Table 8 shows that the model has a Q square value of 0.052, which indicates a moderate level of prediction power.
IPMA analysis
IPMA stands for importance and performance analysis, an advanced technique used in the SmartPLS. This technique explains the importance and performance of each variable for the variable of interest, known as the dependent variable. According to Table 9, perceived usefulness is the most important and performed variable for the aforementioned model to adapt the IS. The importance value for the PU is 36.5%, and the performance value is 68.29%. The IPMA analysis provides guidelines to the policymakers about the importance of variables and needs to be considered. For example, performance values indicate how well the system works in each category. PEU and Financial Capability have 58.02 and 62.5 values respectively, while PU received a highest score of 67.29, which indicates strong performance. These statistics helps to prioritize areas that require improvement. It emphasizes on importance of PU as the highest priority during the adoption of HIS.
MGA analysis
A multigroup analysis is an advanced technique used in the structural equation model to compare the difference between the two groups about the statistical significance of a relationship. Table 10 compares the statistical differences of the respondents in each relationship based on gender. The table indicates no significant impact of gender. It is a significant sign that there is no difference between the data based on the groups, which shows that the data is homogenous. There is no heterogeneity in the data because heterogeneity is one of the basic assumptions of a proper and efficient regression analysis considered free from the bias of the data.
Table 11 compares the respondents’ differences in each model’s relationship. The table shows no difference due to the designation of any relationship except perceived usefulness to adapting the IS. According to the table, doctors show much behavior about the perceived usefulness of the adaptation of ISs.
Discussion
The IS is an important aspect of technology that is overcoming all the manual management systems in most organizations; the health sector is one among them (Alotaibi and Subahi 2022). There are several factors, according to the literature, which is responsible for the adaptation of the IS (Chen et al. 2020). Six hypotheses were claimed based on this study’s model, among which three are based on direct relationships, and the other is based on moderating relationships. Among these six, only two hypotheses were not supported by the findings of this study, while the other four were supported. The first hypothesis claims that financial capability will lead to a better adaptation of the IS in the healthcare sector of Pakistan. However, the findings of this study support the claimed hypothesis with the β = 0.168; p = 0.023. Several studies from the past literature also have similar findings to this study that financial capability or strength is a significant factor that leads toward adapting ISs (Deepu and Ravi 2021; Shahbaz et al. 2019). The second hypothesis based on direct relationship claimed that perceived ease of use would lead toward adaptation of ISs in Pakistan’s healthcare sector. However, the findings of this study support the claimed hypothesis with β = 0.076; p = 0.044. Although several studies from the past literature have the same findings, perceived ease of use is a sufficient factor for adopting healthcare ISs in different sectors along with the healthcare sector. According to them, people adopt new technology products and services mostly based on how useful and easy to use the new one is (Nikou and Maslov 2021). The third and last direct relationship based supported hypothesis claims that perceived usefulness will lead to better adaptation of ISs in the healthcare sector; however, the findings of this study support the claim that perceived usefulness will encourage the adaptation of ISs with β = 0.254; p = 0.000. Although there are several studies from past researcher which has been conducted in different geographical regions on different IS adaptation other than the healthcare sector, they show their findings also in line with the said study (Chen and Aklikokou 2020; Lin et al. 2012).
The fourth hypothesis claimed that a change in the size of the hospital would moderate the relationship of financial capability with the adaptation of ISs in the healthcare sector. However, from the findings of this study, it was found that the hypothesis is not supported by a statistically insignificant relationship with β = 0.075; p = 0.213. Past literature also claimed that several studies have the same findings as the said study about the said hypothesis (Kuek and Hakkennes 2020). This may be because the hospital’s size does not mean the hospital is more capable of financing or having more profit margin to invest in these technological things (Shahbaz et al. 2019). The fifth hypothesis based on this study’s model claims that the hospital’s size will affect the perceived ease of use impact on the adaptation of ISs in the healthcare sector. However, the findings of this study also support the said argument that the increase in the hospital size perceived ease of use will have more effect on the adaptation of ISs in the healthcare sector with β = 0.101; p = 0.009. Several studies from the past also have the same type of findings; the reason for that how much the size of a hospital is increased it will lead a better communication between the employees and it will indirectly enhance the people’s psyche to understand the said technology to be easy to be used (Dhagarra et al. 2020). The sixth and last hypothesis argues that the size of the hospital will moderate the perceived usefulness impact on the adaptation of the IS in the healthcare sector of Pakistan. However, the study results don’t show consistency with the argument claimed with β = 0.080; p = 0.283. Several studies from the past literature also have the same types of findings, which are in line with the findings of this study (Zhao et al. 2019). The reason for that may be that size of the hospital may not be a significant factor affecting its usefulness. If a product or service is useful, people will use and adopt it regarding the size of that organization (Tsai et al. 2019).
PU and PEU are popular terms, emphasizing that people are more inclined to accept technology that they believe to be useful and easy to use. PU and PEU become significant considerations in the healthcare context because of the complicated tasks and sensitive nature of data, which need the adoption of useful and user-friendly technologies (Huarng et al. 2022). Similarly, financial capability (Endriyas et al. 2023) of a healthcare organization is also critical as the adoption of HIS requires large investments in technological facilities, training, and maintenance. Hospitals might face difficulties in the adoption and integration of HIS if they have financial difficulties. This could impede their capacity to fully utilize HIS for better services. Therefore, consideration of PEU, PU and financial capability are essential determinants for HIS adopting strategies. In addition, the research also investigated the moderating influence of hospital size (Kraus et al. 2021) on the impact of PU, PEU and financial capability on the adoption of HIS. It is clear from the findings that hospital size has a moderating role on the impact of PEU on HIS adoption. In other words, the role of PEU on HIS adoption is dependent on the hospital size. PEU may impact the adoption of HIS in large hospitals more than in smaller hospitals, as large hospitals have more organizational resources and complexities than the smaller ones. Due to the importance of this moderating effect, PEU-enhancing measures must to be adapted according to the specific needs associated with hospital sizes. It is essential to understand the relationship between hospital size and PEU in influencing the adoption of HIS in order to establish tailored strategies and measures according to the various needs and difficulties, faced by different size healthcare organizations. As shown by the findings, there exists no significant moderating role of the hospital size on the relationship between financial capability, PU and the adoption of HIS. The influence of financial capability and PU on HIS adoption is similar in hospitals of various sizes. In other words, PU and funding capacity have a considerable impact on the decision to adopt HIS, regardless of the hospital’s size. The absence of this moderating impact suggests that tactics to increase PU and provide funding for the adoption of HIS should be widely used in all hospital of all size. It emphasizes the significance of these elements as broadly applicable drivers for the HIS adoption across all hospitals. The research has the following implications.
Theoretical implications
The study investigated the role of PU, PEU, and financial strength or capability on the adoption of HIS while considering the hospital size a moderating variable. The research identifies these factors as necessary for the adoption of HIS and broadening the horizon of TAM and RBV. The study integrates TAM and RBV and develop its own theoretical model. Further, the research also makes an important contribution toward the understanding of successful adoption of HIS.
Policy implications
The study offers some important implications for the policy makers, who are involved in the decisions regarding the adoption of HIS. Policymakers need to recognize the critical role that funds play in the adoption of HIS in hospitals and provide them enough funding. It is also necessary for policy makers to provide training and awareness among the healthcare professionals regarding the PEU and PU of HIS. This will provide a clear picture and purpose of the HIS adoption to the employees. Policy makers should adapt tailored approach while selecting and adopting HIS according to the needs and uniqueness of hospitals, e.g., size and financial strength.
Practical implications
The study also provides some essential implications for hospitals. Hospital managers should asses and do careful financial planning about the viability of adopting and implementing a HIS. Hospitals should actively include healthcare workers in the HIS implementation process to improve PEU and PU, and provide training. In order to successfully adopt HIS, hospitals of all sizes should work together and with other healthcare organizations to share experiences, lessons learned, and best practices.
Conclusion
The study concludes that perceived ease of use, perceived usefulness, and financial capability of healthcare facilities have a significant impact on the adoption of a HIS. The PEU is one of the main contributing factors for the adoption of HIS. If the employees perceive that they are able to use the HIS easily and there is no difficulty in utilizing it, or no extra training is required for using the HIS, then they will be inclined toward the adoption of HIS, otherwise, if they perceive that it is difficult to use the new HIS then they will be reluctant to adopt. If the employees believe that the HIS is useful for their work and will enhance their performance, as well as the overall performance of their hospital, they will be more likely to adopt the HIS. Similarly, if the employees perceive that the adoption of the HIS is not useful for their jobs and performance, then they will be reluctant to adopt. In addition, the financial strength of hospitals has also a significant role in HIS adoption. In countries like Pakistan, there is not enough budget for healthcare and the primary objective of healthcare budget is healthcare services. The findings show that if the hospitals are more financially stable and have enough budget, they will invest in HIS. Last but not least, the size of hospitals also impacts the relationship between PEU and the adoption of HIS, and has no influence on the relationship between PU, and hospital size on the adoption of HIS, which is quite interesting and surprising.
Recommendations
-
Health organizations should allocate funds to new technology adoption (Poon et al. 2004).
-
For successful implementation or adoption of an IS, the firms should select the system that is perceived to be useful and effortless (Nezamdoust et al. 2022; Zaman et al. 2022).
-
Hospitals, etc., should train their employees on the usefulness of the new system before implementation (Pedota et al. 2023).
-
Large hospitals need more careful selection of HIS as many parties will be involved in the using (Yusif et al. 2022).
Limitations and future work
-
Other theories and variables can be incorporated into the framework in future to make it more comprehensive.
-
Given that this study was taken in Pakistan, the framework could also be tested in other countries to test is generalizability.
-
Further research is needed to explore the influence of hospital size on the relationship of PU and financial strength.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to privacy issues but are available from the corresponding author on reasonable request.
References
Abbas M, Shahid Nawaz M, Ahmad J, Ashraf M (2017) The effect of innovation and consumer related factors on consumer resistance to innovation. Cogent Bus Manag 4(1):1312058. https://doi.org/10.1080/23311975.2017.1312058
Addotey-Delove M, Scott RE, Mars M (2023) Healthcare workers’ perspectives of mHealth adoption factors in the developing world: scoping review. Int J Environ Res Public Health 20(2):1244. https://doi.org/10.3390/ijerph20021244
Ahmad SF, Alam MM, Rahmat MK, Mubarik MS, Hyder SI (2022) Academic and administrative role of artificial intelligence in education. Sustainability 14(3):1101. https://doi.org/10.3390/su14031101
Ahmad SF, Rahmat MK, Mubarik MS, Alam MM, Hyder SI (2021) Artificial intelligence and its role in education. Sustainability 13(22):12902. https://doi.org/10.3390/su132212902
Akther T, Nur T (2022) A model of factors influencing COVID-19 vaccine acceptance: a synthesis of the theory of reasoned action, conspiracy theory belief, awareness, perceived usefulness, and perceived ease of use. PLoS ONE 17(1):e0261869. https://doi.org/10.1371/journal.pone.0261869
Alboliteeh M, Alrashidi MS, Alrashedi N, Gonzales A, Mostoles RJ, Pasay-an E, Dator WL (2022) Knowledge management and sustainability performance of hospital organisations: the healthcare managers’ perspective. Sustainability 15(1):203. https://doi.org/10.3390/su15010203
Almaiah MA, Alhumaid K, Aldhuhoori A, Alnazzawi N, Aburayya A, Alfaisal R, Salloum SA, Lutfi A, Al Mulhem A, Alkhdour T, Awad AB, Shehab R (2022) Factors affecting the adoption of digital information technologies in higher education: an empirical study. Electronics 11(21):3572. https://doi.org/10.3390/electronics11213572
Alotaibi Y, Subahi AF (2022) New goal-oriented requirements extraction framework for e-health services: a case study of diagnostic testing during the COVID-19 outbreak. Bus Process Manag J 28(1):273–292. https://doi.org/10.1108/BPMJ-09-2020-0414
Alsyouf A, Lutfi A, Alsubahi N, Alhazmi FN, Al-Mugheed K, Anshasi RJ, Alharbi NI, Albugami M (2023) The use of a technology acceptance model (TAM) to predict patients’ usage of a personal health record system: the role of security, privacy, and usability. Int J Environ Res Public Health 20(2):1347. https://doi.org/10.3390/ijerph20021347
Barney J (1991) Firm resources and sustained competitive advantage. J Manag 17(1):99–120. https://doi.org/10.1177/014920639101700108
Bloomberg J (2018) Digitization, digitalization, and digital transformation: confuse them at your peril. Forbes
Broccardo L, Zicari A, Jabeen F, Bhatti ZA (2023) How digitalization supports a sustainable business model: a literature review. Technol Forecast Soc Change 187:122146. https://doi.org/10.1016/j.techfore.2022.122146
Brown SA, Dennis AR, Venkatesh V (2010) Predicting collaboration technology use: integrating technology adoption and collaboration research. J Manag Inf Syst 27(2):9–54. https://doi.org/10.2753/MIS0742-1222270201
Chen L, Aklikokou AK (2020) Determinants of E-government adoption: testing the mediating effects of perceived usefulness and perceived ease of use. Int J Public Adm 43(10):850–865. https://doi.org/10.1080/01900692.2019.1660989
Chen P-T, Lin C-L, Wu W-N (2020) Big data management in healthcare: adoption challenges and implications. Int J Inf Manag 53:102078. https://doi.org/10.1016/j.ijinfomgt.2020.102078
Cheng N, Li H, Bang Y (2023) Pay-for-performance schemes and hospital HIT adoption. Decis Support Syst 164:113868. https://doi.org/10.1016/j.dss.2022.113868
Crisan EL, Mihaila A (2023) Health-care information systems adoption—a review of management practices. Vilakshan XIMB J Manag 20(1):130–139. https://doi.org/10.1108/XJM-04-2021-0121
Dewar RD, Dutton JE (1986) The adoption of radical and incremental innovations: an empirical analysis. Manag Sci 32(11):1422–1433
Davis FD (1989) Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q 13(3):319. https://doi.org/10.2307/249008
Deepu TS, Ravi V (2021) Supply chain digitalization: an integrated MCDM approach for inter-organizational information systems selection in an electronic supply chain. Int J Inf Manag Data Insights 1(2):100038. https://doi.org/10.1016/j.jjimei.2021.100038
Dhagarra D, Goswami M, Kumar G (2020) Impact of trust and privacy concerns on technology acceptance in healthcare: an Indian perspective. Int J Med Inform 141:104164. https://doi.org/10.1016/j.ijmedinf.2020.104164
Dicuonzo G, Donofrio F, Fusco A, Shini M (2023) Healthcare system: moving forward with artificial intelligence. Technovation 120:102510. https://doi.org/10.1016/j.technovation.2022.102510
Endriyas M, Alano A, Mekonnen E, Hailu S, Hailemariam T, Ayele S, Shiferaw M, Kelaye T, Misganaw T, Samuel T (2023) Factors contributing to poor healthcare data quality: qualitative study from Southern Ethiopia. Health Technol. https://doi.org/10.1007/s12553-023-00741-7
Hedayati MK, Schniederjans DG (2022) Integration of knowledge management in digital healthcare industries. In: Wang J (ed) Encyclopedia of data science and machine learning. IGI Global United States of America, p 1703–1716. https://doi.org/10.4018/978-1-7998-9220-5.ch102
Hopper AM (2015) Using data management techniques to modernize healthcare. Productivity Press
Hu K, O’Brien S (2016) Applying TAM (Technology Acceptance Model) to testing MT acceptance. [online] https://commission.europa.eu/document/. [Accessed 08 July 2023]
Huarng K-H, Yu TH-K, Lee CF (2022) Adoption model of healthcare wearable devices. Technol Forecast Soc Change 174:121286. https://doi.org/10.1016/j.techfore.2021.121286
Ibrahim M, Shahid MK, Ahmed SF (2014) The impact of telecom services characteristics on consumer for use in Pakistan. Adv Econ Bus 2(4):172–179. https://doi.org/10.13189/aeb.2014.020403
Ibrahim M, Shahid M, Akbar S, Ahmed SF (2015) Determining the effect of innovations for mobile banking adoption in Pakistan. J Inf Eng Appl 5(11):16–23
Jarva E, Oikarinen A, Andersson J, Tomietto M, Kääriäinen M, Mikkonen K (2023) Healthcare professionals’ digital health competence and its core factors; development and psychometric testing of two instruments. Int J Med Inform 171:104995. https://doi.org/10.1016/j.ijmedinf.2023.104995
Khan Y, Su’ud MBM, Alam MM, Ahmad SF, Ahmad (Ayassrah) AYAB, Khan N (2022a) Application of internet of things (IoT) in sustainable supply chain management. Sustainability 15(1):694. https://doi.org/10.3390/su15010694
Khan Y, Su’ud MBM, Alam MM, Ahmad SF, Salim NA, Khan N (2022b) Architectural threats to security and privacy: a challenge for internet of things (IoT) applications. Electronics 12(1):88. https://doi.org/10.3390/electronics12010088
Khanna RR, Murray SG, Wen T, Salmeen K, Illangasekare T, Benfield N, Adler-Milstein J, Savage L (2022) Protecting reproductive health information in the post-Roe era: interoperability strategies for healthcare institutions. J Am Med Inform Assoc 30(1):161–166. https://doi.org/10.1093/jamia/ocac194
Kim D-Y, Jang S (Shawn), Morrison AM (2011) Factors affecting organizational information technology acceptance: a comparison of convention and visitor bureaus and meeting planners in the United States. J Conv Event Touri 12(1):1–24. https://doi.org/10.1080/15470148.2010.551291
Kraus S, Schiavone F, Pluzhnikova A, Invernizzi AC (2021) Digital transformation in healthcare: analyzing the current state-of-research. J Bus Res 123:557–567. https://doi.org/10.1016/j.jbusres.2020.10.030
Kuan KKY, Chau PYK (2001) A perception-based model for EDI adoption in small businesses using a technology–organization–environment framework. Inf Manag 38(8):507–521. https://doi.org/10.1016/S0378-7206(01)00073-8
Kuek A, Hakkennes S (2020) Healthcare staff digital literacy levels and their attitudes towards information systems. Health Inform J 26(1):592–612. https://doi.org/10.1177/1460458219839613
LaBerge L (2020) How COVID-19 has pushed companies over the technology tipping point—and transformed business forever. Mckinsey. https://www.mckinsey.com/capabilities/strategy-and-corporate-finance/our-insights/how-covid-19-has-pushed-companies-over-the-technology-tipping-point-and-transformed-business-forever
Lee G, Xia W (2006) Organizational size and IT innovation adoption: a meta-analysis. Inf Manag 43(8):975–985. https://doi.org/10.1016/j.im.2006.09.003
Lin C, Lin I-C, Roan J (2012) Barriers to physicians’ adoption of healthcare information technology: an empirical study on multiple hospitals. J Med Syst 36(3):1965–1977. https://doi.org/10.1007/s10916-011-9656-7
Liu X, Ahmad SF, Anser MK, Ke J, Irshad M, Ul-Haq J, Abbas S (2022) Cyber security threats: a never-ending challenge for e-commerce. Front Psychol 13. https://doi.org/10.3389/fpsyg.2022.927398
Lind MR, Zmud RW, Fischer WA (1989) Microcomputer adoption—the impact of organizational size and structure. Inf Manag 16(3):157–162
Loke V, Choi L, Libby M (2015) Increasing Youth Financial Capability: An Evaluation of the MyPath Savings Initiative. J Consum Aff 49(1):97–126. https://doi.org/10.1111/joca.12066
Mahdi SS, Battineni G, Khawaja M, Allana R, Siddiqui MK, Agha D (2023) How does artificial intelligence impact digital healthcare initiatives? A review of AI applications in dental healthcare. Int J Inf Manag Data Insights 3(1):100144. https://doi.org/10.1016/j.jjimei.2022.100144
Malik M, Kazi AF, Hussain A (2021) Adoption of health technologies for effective health information system: need of the hour for Pakistan. PLoS ONE 16(10):e0258081. https://doi.org/10.1371/journal.pone.0258081
McAdory BJ (2021) Investment in information technology can improve profitability in U.S. hospitals. https://harbert.auburn.edu/news/investment-in-information-technology-can-improve-profitability-in-us-hospitals.html
Mousa S, Bouraoui T (2023) The role of sustainability and innovation in financial services business transformation. Theor Econ Lett 13(1):84–108. https://doi.org/10.4236/tel.2023.131005
Ndayishimiye C, Lopes H, Middleton J (2023) A systematic scoping review of digital health technologies during COVID-19: a new normal in primary health care delivery. Health Technol. https://doi.org/10.1007/s12553-023-00725-7
Nezamdoust S, Abdekhoda M, Rahmani A (2022) Determinant factors in adopting mobile health application in healthcare by nurses. BMC Med Inform Decis Mak 22(1):47. https://doi.org/10.1186/s12911-022-01784-y
Nikou S, Maslov I (2021) An analysis of students’ perspectives on e-learning participation—the case of COVID-19 pandemic. Int J Inf Learn Technol 38(3):299–315. https://doi.org/10.1108/IJILT-12-2020-0220
Ohio University (2020) Health information systems: health care for the present and future. Ohio University. https://onlinemasters.ohio.edu/blog/health-information-systems/
Park DY, Kim H (2023) Determinants of intentions to use digital mental healthcare content among university students, faculty, and staff: motivation, perceived usefulness, perceived ease of use, and parasocial interaction with AI Chatbot. Sustainability 15(1):872. https://doi.org/10.3390/su15010872
Park SY (2009) An Analysis of the Technology Acceptance Model in Understanding University Students’ Behavioral Intention to Use e-Learning. Edu Technol Soc 12(3):150–162
Pedota M, Grilli L, Piscitello L (2023) Technology adoption and upskilling in the wake of Industry 4.0. Technol Forecast Soc Change 187:122085. https://doi.org/10.1016/j.techfore.2022.122085
Philibert C (2003) Technology innovation, development and diffusion. https://www.oecd.org/env/cc/2956490.pdf
Poon EG, Blumenthal D, Jaggi T, Honour MM, Bates DW, Kaushal R (2004) Overcoming barriers to adopting and implementing computerized physician order entry systems in U.S. hospitals. Health Aff 23(4):184–190. https://doi.org/10.1377/hlthaff.23.4.184
Prasad A (2018) 10 ways technology has reshaped the modern workplace. Quickfms. https://www.quickfms.com/blog/how-technology-has-reshaped-the-workplace
Pufahl L, Zerbato F, Weber B, Weber I (2022) BPMN in healthcare: challenges and best practices. Inf Syst 107:102013. https://doi.org/10.1016/j.is.2022.102013
Renny, Guritno S, Siringoringo H (2013) Perceived usefulness, ease of use, and attitude towards online shopping usefulness towards online airlines ticket purchase. Procedia Soc Behav Sci 81:212–216. https://doi.org/10.1016/j.sbspro.2013.06.415
Rey-Moreno M, Periáñez-Cristóbal R, Calvo-Mora A (2022) Reflections on sustainable urban mobility, mobility as a service (MaaS) and adoption models. Int J Environ Res Public Health 20(1):274. https://doi.org/10.3390/ijerph20010274
Rohani N, Yusof MM (2023) Unintended consequences of pharmacy information systems: a case study. Int J Med Inform 170:104958. https://doi.org/10.1016/j.ijmedinf.2022.104958
Saeed KA, Abdinnour-Helm S (2008) Examining the effects of information system characteristics and perceived usefulness on post adoption usage of information systems. Inf Manag 45(6):376–386. https://doi.org/10.1016/j.im.2008.06.002
Salah OH, Yusof ZM, Mohamed H (2021) The determinant factors for the adoption of CRM in the Palestinian SMEs: the moderating effect of firm size. PLoS ONE 16(3):e0243355. https://doi.org/10.1371/journal.pone.0243355
Sayed AF, Shahid MK, Ahmad SF (2020) Adoption of mobile payment application and its impact on business. pp. 253–269. https://doi.org/10.4018/978-1-7998-2398-8.ch012
Shahadat MMH, Nekmahmud M, Ebrahimi P, Fekete-Farkas M (2023) Digital technology adoption in SMEs: what technological, environmental and organizational factors influence in emerging countries? Glob Bus Rev 097215092211371. https://doi.org/10.1177/09721509221137199
Shahbaz M, Gao C, Zhai L, Shahzad F, Hu Y (2019) Investigating the adoption of big data analytics in healthcare: the moderating role of resistance to change. J Big Data 6(1):6. https://doi.org/10.1186/s40537-019-0170-y
Shahzad K, Jianqiu Z, Zia MA, Shaheen A, Sardar T (2021) Essential factors for adopting hospital information system: a case study from Pakistan. Int J Comput Appl 43(1):26–37. https://doi.org/10.1080/1206212X.2018.1504460
Singerman A, Lence SH (2023) The source of uncertainty influences technology adoption. Eur Rev Agric Econ. https://doi.org/10.1093/erae/jbac036
Sinhasane S (2022) What is health information system and its significance in the healthcare sector? https://mobisoftinfotech.com/resources/blog/importance-of-health-information-system/
Stachwitz P, Debatin JF (2023) Digitalisierung im Gesundheitswesen: heute und in Zukunft. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 66(2):105–113. https://doi.org/10.1007/s00103-022-03642-8
Sturmberg JP, Bircher J (2019) Better and fulfilling healthcare at lower costs: the need to manage health systems as complex adaptive systems. F1000Research 8:789. https://doi.org/10.12688/f1000research.19414.1
Tortorella GL, Fogliatto FS, Espôsto KF, Mac Cawley Vergara A, Vassolo R, Tlapa Mendoza D, Narayanamurthy G (2022) Measuring the effect of Healthcare 4.0 implementation on hospitals’ performance. Prod Plan Control 33(4):386–401. https://doi.org/10.1080/09537287.2020.1824283
Tsai M-F, Hung S-Y, Yu W-J, Chen CC, Yen DC (2019) Understanding physicians’ adoption of electronic medical records: healthcare technology self-efficacy, service level and risk perspectives. Comput Stand Interfaces 66:103342. https://doi.org/10.1016/j.csi.2019.04.001
Tseng M-L, Ha HM, Wu K-J, Xue B (2022) Healthcare industry circular supply chain collaboration in Vietnam: vision and learning influences on connection in a circular supply chain and circularity business model. Int J Logist Res Appl 25(4–5):743–768. https://doi.org/10.1080/13675567.2021.1923671
Turel O, Serenko A, Giles P (2011) Integrating technology addiction and use: an empirical investigation of online auction users. MIS Q 35(4):1043. https://doi.org/10.2307/41409972
Vassolo RS, Mac Cawley AF, Tortorella GL, Fogliatto FS, Tlapa D, Narayanamurthy G (2021) Hospital investment decisions in healthcare 4.0 technologies: scoping review and framework for exploring challenges, trends, and research directions. J Med Internet Res 23(8):e27571. https://doi.org/10.2196/27571
Veikkolainen P, Tuovinen T, Jarva E, Tuomikoski A-M, Männistö M, Pääkkönen J, Pihlajasalo T, Reponen J (2023) eHealth competence building for future doctors and nurses—attitudes and capabilities. Int J Med Inform 169:104912. https://doi.org/10.1016/j.ijmedinf.2022.104912
Venkatesh V, Thong JYL, Xu X (2012) Consumer acceptance and use of information technology: extending the unified theory of acceptance and use of technology. MIS Q 36(1):157. https://doi.org/10.2307/41410412
Wang BB, Wan TTH, Burke DE, Bazzoli GJ, Lin BYJ (2005) Factors influencing health information system adoption in American hospitals. Health Care Manag Rev 30(1):44–51
Xiong E (2021) The sustainable impact of a paperless office. Forbes. https://www.forbes.com/sites/forbestechcouncil/2021/05/11/the-sustainable-impact-of-a-paperless-office/?sh=1fb81b421095
Yulianto A, Ahmad S, Lelly A, Nobia S (2022) Ease of use technology as a dominant factor in technology acceptance hospital information system by officers at the Jambi provincial government hospital. In: Proceedings of the 5th European international conference on industrial engineering and operations management Rome, Italy, July 26–28, 2022. IEOM Society International
Yusif S, Hafeez-Baig A, Soar J (2022) Change management and adoption of health information technology (HIT)/eHealth in public hospitals in Ghana: a qualitative study. Appl Comput Inform 18(3/4):279–289. https://doi.org/10.1016/j.aci.2019.11.007
Zaman SB, Khan RK, Evans RG, Thrift AG, Maddison R, Islam SMS (2022) Exploring barriers to and enablers of the adoption of information and communication technology for the care of older adults with chronic diseases: scoping review. JMIR Aging 5(1):e25251. https://doi.org/10.2196/25251
Zhao Y, Li K, Zhang L (2019) A meta-analysis of online health adoption and the moderating effect of economic development level. Int J Med Inform 127:68–79. https://doi.org/10.1016/j.ijmedinf.2019.04.015
Acknowledgements
The authors extend appreciation to the Deputyship for Research and Innovation, Ministry of Education in Saudi Arabia, for funding this research Project through Researchers Supporting project Number (RSPD2024R870), Kind Saud University, Riyadh, Saudi Arabia.
Author information
Authors and Affiliations
Contributions
Conceptualization: JL and SFA; methodology: AA, YO and MI; resources: RA and STU; data curation: RA, STU and GA; data collection and data analysis: RA, STU, GA and MI; writing—original draft preparation: AA and YO; writing—review and editing: JL, SFA, RA and STU; supervision: SFA; project administration: JL and YO; funding acquisition: RA, STU, GA and AA. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests. All authors have approved the manuscript and agree with its submission.
Ethical approval
The evaluation survey questionnaire and methodology were examined, approved, and endorsed by the research ethics committee University of Gwadar on 15 August, 2022 having ethical approval no. 2022/UG/ORIC/P-03. The study meets the requirements of the National Statement on Ethical Conduct in Human Research (2007). The procedures used in this study adhere to the tents of the declaration of Helsinki.
Informed consent
Informed consent was obtained from all participants before the data were collected. We informed each participant of their rights, the purpose of the study and to safeguard their personal information.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Luo, J., Ahmad, S.F., Alyaemeni, A. et al. Role of perceived ease of use, usefulness, and financial strength on the adoption of health information systems: the moderating role of hospital size. Humanit Soc Sci Commun 11, 516 (2024). https://doi.org/10.1057/s41599-024-02976-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1057/s41599-024-02976-9