Abstract
Over eight decades of mass antimicrobial exposures have changed microbial populations and genes at a global level. This thought piece argues that adequately responding to the anthropogenic transformation of the microbial commons requires reframing antimicrobial resistance (AMR) as the pheno- and genotypic signal of a new geological era – an Antibiocene. Thinking through the multiple spatiotemporal, biological, and social scales of this Antibiocene opens important perspectives on the long-term goals of (anti)microbial stewardship, the injustices connected with unequal antimicrobial exposures, and the scale of necessary changes to health, food production, and waste disposal systems. Conceptualising AMR within an Antibiocene also necessitates shifting the political gaze from the clinic and sites of food production to the hitherto neglected environmental domain of One Health, whose terrestrial and aquatic milieus act as crucial reservoirs for antimicrobial substances, antimicrobial resistance genes, and resistant organisms. Finally, disentangling the human and non-human dimensions of the Antibiocene requires working across the humanities, social-, environmental, and biomedical sciences. The thought piece ends by proposing comparative research on particularly contaminated sites as a promising way of reconstructing the microbial, biochemical, and societal fallouts of chronic antimicrobial exposures as well as already existing societal adaptations. Resulting findings will provide orientation for emerging debates on the preservation of our microbial commons and the development of new forms of ‘eubiotic governance’.
Similar content being viewed by others
Introduction
Our biosphere is rapidly changing. In the case of microbial environments, the rise of antimicrobial resistance (AMR) across a wide number of bacterial species is a significant genetic and phenotypic marker of humanity’s growing planetary footprint. Although phylogenetic studies indicate that many genetic traits conferring AMR predate the antimicrobial era (Roumagnac et al. 2006; Holt et al. 2008; Tran-Dien et al. 2017; Baker et al. 2018), the rapid rise in the release of antimicrobial substances such as pharmaceuticals, heavy metals, and biocides from the 19th century onwards has played a significant role in accelerating this “Anthropocene in the cell” (D’Abramo and Landecker 2019). Researchers, policymakers, and journalists have responded to the ongoing acceleration of AMR burdens with increasingly vocal calls for antimicrobial stewardship and drug innovation to avert a pending “antibiotic apocalypse” (McKie 2017) when essential drugs no longer work (Davies 2013a; Davies 2013b).
But what if the alleged apocalypse is already upon us – just not as a Hollywood-style catastrophic systems collapse – but as an increasingly apparent degradation of the microbial commons humanity relies on? If a return to an era of microbial sensitivity is not possible both because of the inbuilt antimicrobial dependency of our food and medical infrastructures as well as the genetic legacy antimicrobial exposures have already created in our biosphere (Chandler, Hutchinson, and Hutchison 2016), it is time to focus on what life amongst the detritus of the antimicrobial era – the AntibioceneFootnote 1 – looks like. Abandoning the apocalyptic genre that has grown up around AMR debates is neither defeatist nor does it remove the need for urgent action to prevent deaths from priority pathogens or ongoing stewardship efforts. Instead, it is to contextualise and orientate ad hoc mitigation efforts within a more long-term analytical eco-social framework of constantly evolving human-microbial interactions.
In this thought piece, I first review existing attempts to make sense of the unintended fallouts of our antimicrobial era and the inherent limitations of traditional portrayals of antimicrobial resistance (AMR) as a short-termist challenge of treatment failure and individual responsibility. In part two of the article (Introducing the Antibiocene), I then move on to argue that engaging with AMR as a major signal of an unfolding planetary Antibiocene opens the door for integrating rich strands of already ongoing social sciences, environmental humanities, and biomedical research on the various scales and fallouts of antimicrobial exposures and microbiota shifts. Thinking about AMR not as a standalone medical or productivity challenge but as a potent signal with which to assess wider shifts of human-microbial relations and biochemical environments challenges the long-standing prioritisation of human and animal over environmental health (Destoumieux-Garzón et al. 2018). It also enables new ways of thinking about microbial time in relation to geological shifts and anthropogenic agency by laying bear the “pluribiotic” constantly evolving multispecies entanglements (Brives 2021, Barad 2007) around us. And finally, it reveals the stark inequalities with which the burdens of antimicrobial exposures have been distributed between and within societies. In part three (Unearthing the Antibiocene), I end by discussing how comparative investigations of sites of chronic antimicrobial hyperexposure can untangle the biosocial dynamics of the Antibiocene and inform emerging debates on fostering balanced eubiotic (Berg et al. 2020) microbiota.
Explosive Exposure
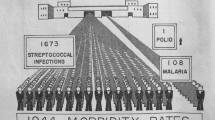
For microbes, the modern era has been one of explosive exposure to a growing number of selective pressures. Over the past two centuries, warming temperatures, acidifying oceans, and the anthropogenic release of amonia, nitrogen, and atmospheric carbon dioxide and methane into our biosphere have impacted microbial abundance and diversity (Gillings and Paulsen, 2014). In addition, microbial populations have also been exposed to a rapidly expanding number of highly selective antimicrobial substances such as pharmaceuticals, heavy metals, and biocides (Lorimer 2020). While it is impossible to quantify the exact amount of antimicrobial material released by humans since the early industrial era or the launch of the first mass-marketed sulphonamides around 1935, accretive exposure to millions of tons of antimicrobial substances has transformed the microbiota in and around us (Changing Markets and Ecostorm 2016).Footnote 2
Ironically, many of the most potent modern antimicrobials or their chemical forbears are produced by microbes themselves. For millennia, certain microbes have used antimicrobials to signal and compete with others (Marinelli and Genilloud 2013; Yim et al. 2007; Abrudan et al. 2015). Humans’ discovery and subsequent mass-production of these substances via chemical synthesis or by culturing vast monocultures of microbial anti-microbial producers has dramatically amplified this aspect of interbacterial relations. The result of this selective amplification of interbacterial signalling has been uncompromising evolutionary pressure: antimicrobial exposures have forced microbes to evolve numerous ways to resist antimicrobial substances and pass on these old and new AMR traits. Although humans have reacted to microbial resistance by trying to increase antibiotic innovation and preserve the efficacy of existing antimicrobials, they have simultaneously allowed their health- and food-systems to become more and more antibiotic dependent (Podolsky 2015; Gradmann 2018; Podolsky 2018; Kirchhelle 2018a, 2020).
As a result, virtually no microbiota have escaped the thin soup of antimicrobial substances with which humans have covered most of the planet. Routine antimicrobial exposure has occurred in a wide range of terrestrial (You and Silbergeld 2014) and aquatic (Kümmerer 2009; Kraemer, Ramachandran, and Perron 2019) environments. Whereas some environments contain only miniscule amounts of antimicrobial substances, far higher selective concentrations have been reported in areas linked to human and livestock habitation. A 2014 survey found high selective concentrations of antimicrobials in the tap water of major Chinese cities (Huang et al. 2015). Eight years later, a survey of 258 rivers, representing the environmental influence of 471.4 million people, found levels of various antimicrobials in excess of industry-set safety levels on all continents (Wilkinson et al. 2022). Worryingly, recent research indicates that even very low concentrations of antimicrobials, which were previously deemed nonselective can impact microbiota and select for AMR (Grenni 2022), with new data indicating potential associations between particulate air pollution and local AMR levels (Zhou et al. 2023).
Microbial genomes have changed accordingly. Spreading by air, land, and sea (Silbergeld 2016), antimicrobial resistance genes (ARGs) have been recovered from frozen Antarctic environments (Jara et al. 2020) to the microbiomes of uncontacted tribes from remote South American jungles (Clemente et al. 2015) and clouds above French mountains (Rossi et al. 2023). Similar to the ongoing global increase of antimicrobial exposures, the spread of ARGs appears to be cumulative. In 2010, an analysis of archived Dutch soils found a significant increase of alleles of genes conferring AMR between 1940 and 2008 with the abundance of some alleles associated with tetracycline resistance increasing >15 fold between 1970 and 2008 (Knapp et al. 2010; Zhu and Penuelas, 2020). If antibiotic drugs were once heralded as a symbol of modernity’s promise to alleviate disease and hunger with technological progress (Bud 2007), rising AMR is a major signal of the enormous environmental and genomic externalities of a new geological era – an Antibiocene – characterised by the explosive planetary increase and persistence of multiple anthropogenic antimicrobial exposures.
Human awareness of the potential costs of large-scale antimicrobial interference with our biosphere dates back to the mid-20th century. The emergence of microbial ‘drug fastness’ was first observed and investigated around 1910 (Gradmann 2011). By the late 1930s, doctors were reporting that pathogens could rapidly develop resistance to sulphonamides (Landecker 2019; Lesch 2007). Two decades later, prominent microbiologists such as René Dubos, discoverer of the first clinically tested and produced biological antibiotic gramicidin, began to warn about destabilising wider microbial ecosystems with mass antimicrobial usage (Dubos 1942, [1959] 1985 [1965]; 1987). Dubos’ warnings were amplified between 1958 and 1965 by the Japanese in vitro discovery of mobile resistance factors (R-factors) and the British in vivo observation that R-factors were exchanged between different bacteria species in clinical and farm environments (Kirchhelle 2018b). Since this time, predictions of a pending end of antibiotic efficacy as a result of AMR have been a regular feature of scientific and mass media publications. Stalling antibiotic innovation, fears of (re-)emerging diseases, and advances in genomic surveillance meant that warnings reached an international crescendo ahead of the World Health Organisation’s (WHO) 2015 Global Action Plan on AMR (Overton et al. 2021; WHO 2015).
Despite human awareness of the potential planetary impacts of accelerating antimicrobial exposures, resulting policy interventions have been remarkably selective in their focus. Since the 1950s, the overwhelming majority of relevant policy publications have focused on the immediate threat to health and productivity posed by antibiotic failure in human and food production (Overton et al. 2021). This short-termist framing of AMR as a threat of therapy failure or productivity loss is understandable given the significant mortality and morbidity resistant infections have already caused throughout the world (Murray et al. 2022). Warning about an imminent end of antibiotic efficacy – narrowly defined as the end of therapeutic effectiveness but not as ongoing antimicrobial selectivity – is also impactful when it comes to generating short-term societal attention. Over the decades, reports about ‘superbugs’ (US Senate 2010; McKenna 2010; Häusler 2006), a time ‘when the drugs don’t work’ (Davies 2013a), or a return to the ‘preantibiotic Middle Ages’ (Anon 1966; Cohen 1992) have spawned countless awareness campaigns, attempts to quantify AMR’s economic impacts (O’Neill Review 2016), and increasingly integrated governance frameworks for antimicrobial stewardship and innovation (Overton et al. 2021). At first glance, the goal of these stewardship and innovation initiatives is clear: to prevent deaths from resistant infections and to ward off an imminent return to the pre- or -post-antibiotic dark ages. What is, however, often less clear is what form the predicted apocalypse will take: will it be a total loss of antibiotic functionality? What is the timescale at which it will take place? Whose health and access to antibiotics should be prioritised when it comes to making the most of remaining therapeutically effective antimicrobials? Should the ultimate goal of stewardship be to phase out the need for antibiotics altogether or to stabilise usage at a yet to be defined sustainable level? Or is the goal to restore previous levels of microbial sensitivity? (Kirchhelle et al. 2020).
This lack of long-term orientation and focus on short-term clinical and productivity outcomes has fragmented global AMR responses. It has also led to a very narrow focus on exposures caused by antimicrobial pharmaceuticals rather than co-selective non-pharmaceutical substances and a relative policy neglect of wider antimicrobial impacts on microbial ecologies. A recent review of 248 international policy reports on AMR since 1950 found that only two had exclusively and explicitly focused on the third – environmental – domain of One Health (Overton et al. 2021). Similarly, a 2017 analysis of the 2015 WHO Global Action Plan found that only a minority of policy proposals focused on the environment (Ogyu et al. 2020). Although a gradual turn towards environmental AMR hazards is occurring with the UN Environmental Program emerging as an influential advocate (UNEP, 2023; WHO One Health Global Leaders Group, 2022; UNEP 2022; FAO/WHO 2019; FAO/WHO/OIE/UNEP, 2022), the entrenched political neglect of AMR’s ecological dimensions should not surprise us. In addition to the traditionally lower status of environmental as opposed to clinical and veterinary sciences, (Destoumieux-Garzón et al. 2018) environmental AMR data is difficult to translate into policy. Despite growing knowledge about environmental antimicrobial exposures and AMR reservoirs, a comparative lack of systematised studies on resulting medium- and long-term threats complicates proving conclusive impacts on human and animal health or other detrimental impacts. Lack of policy attention towards AMR’s indirect environmental pathways is exacerbated by decisionmakers’ tendency to neglect more abstract scenarios of biosphere degradation with no straightforward – and more costly– solutions in favour of “quick fix” (Willis and Chandler 2019; Sariola and Butcher 2022) policies targeting quantifiable threats at the farm and clinical level (Singer et al. 2016).
Introducing the Antibiocene: appreciating the multi-scalar dynamics of AMR
Overcoming the short-termist and narrow pharmaceutical mode of AMR policy requires complementing risk framings of therapy failure with a more long-term ecological understanding of the fundamental shifts our biosphere has and will continue to experience due to accelerating antimicrobial exposures. Similar to the historicization of other anthropogenic impacts of planetary scale, a promising way of achieving this scalar reorientation lies in retelling the traditional clinic-focussed history of the antibiotic era as part of a much wider, explosive, and still unfolding Antibiocene: a new geological era characterised by a profound planetary shift of microbial genomes, cells, and ecosystems in response to multiple accelerating anthropogenic antimicrobial exposures. In the following, I argue that reconceptualising AMR as a major signal of this Antibiocene allows us to: (1) overcome what historian Dipesh Chakrabarty has described as the “outscal[ing]” (Chakrabarty, 2018) of human senses by the spatiotemporal scales of the planetary Anthropocene; (2) foreground a new form of eubiotic governance to manage the microbial commons amidst intensifying antimicrobial fallouts; (3) pay greater attention to the significant variations of geographic and social vulnerability to chronic antimicrobial exposures and dysbiotic environments.
Inscaling the anthropocene
Conceptually, reconceiving of AMR and associated microbial population shifts as signals of an Antibiocene opens new ways of engaging with the rich social sciences scholarship that has arisen around multi-species entanglements within the broader Anthropocene.
Since its popularisation around 2000 (Crutzen 2006), the concept of an Anthropocene as a distinct geological epoch shaped by human action has posed challenges for social and humanities scholars concerned about the concept’s anthropocentrism and how to analyse change at geological scales. In his 2018 article “Anthropocene Time”, historian Dipesh Chakrabarty noted:
…in most discussions of the Anthropocene, questions of geological time fall out of view and the time of human world history comes to dominate. This one-sided conversion of Earth-historical time of world history extracts an intellectual price, for if we do not take into account Earth-History processes that outscale our very human sense of time, we do not quite see the depth of the predicament that confronts humans today. (Chakrabarty 2018).
But what if the implied vastness of Chakrabarty’s “Earth-History processes” (Chakrabarty 2018) itself results from an anthropocentric preoccupation with change at spatiotemporal scales that are grander than the human? In contrast to the million-year cycles invoked by Chakrabarty, thinking through geological eras at the microbial level entails attuning our thinking to processes that can be both faster and slower than what is normally considered in debates about the Anthropocene.
On the one hand, the sheer age, vastness, and adaptiveness of microbial life seem to militate against the often criticised anthropo- and biocentricism of the Anthropocene genre. Prokaryotic (unicellular) microbes and archaea not only account for the vast majority of life and biodiversity on earth, but have also been at the heart of major geochemical processes in ocean, continent and atmospheric chemistry for billions of years (Locey and Lennon 2016; Druschel and Kappler 2015). According to social scientists Myra Hird and Kathryn Yusoff, placing this “conversation between bacteria and rocks front and centre as the most enduring relation in processes of [geological] stratification” reveals the limits of current preoccupations with humans as geological agents: “geology and life are already involved in a complex inter-evolutionary relation that precedes and exceeds human activities but nonetheless hitches an evolutionary ride on its material practices (…). Given enough time, everything becomes digestable to bacteria” (Hird and Yusoff, 2019). Indeed, recent reviews of AMR in the environment suggest that “external environments already harbour resistance factors for all antibiotics that will ever be developed” (Larsson and Flach, 2022). According to Hird and others, “indifferent” (Hird, 2010) microbes and the mechanisms with which they express and resist antimicrobials were here before us, will rapidly adapt to our “infrastructures of waste” (Hird, 2016a, b), and persist long after we have gone.
And yet, the very speed with which microbial signalling and adaptation occurs across interconnected biogeographies simultaneously undermines this plus ça change concept of indifferent microbial time. While one human generation lasts between 20–30 years, some bacteria species such as E. coli can double as quickly every 20 minutes in laboratory settings and human guts and every 15 hours in the environment (Gibson et al. 2018). The awe-inspiring speed with which life and generational time occur at the microbial level means that one human generation can experience the rise and global proliferation of entirely new microbial organisms, genes, and environments. In the case of the over 30-year Long-Term Evolution Experiment (LTEE), US researchers witnessed a wide array of pheno- and genotypic changes whilst examining more than 73,000 microbial generations of 12 initially almost identical cultures of E. coli (Tenaillon et al. 2016; Lenski 2020). The amazing speed of genetic change within bacterial communities is amplified by the promiscuous exchange of genetic material between bacteria via plasmid- or bacteriophage-borne horizontal gene transfer (HGT) and by transduction, the adsorption of ‘free floating’ genetic material from the environment. Conservative estimates suggest that HGT is extremely common in the bacterial world with exchanged accessory genes frequently encoding for AMR and antimicrobial exposures amplifying the likelihood of HGT (Liu et al. 2022; Sheinman et al. 2021). It is against this background of ultra-fast microbial time and “extreme genetic fluidity” (Margulis and Sagan 2007) that the Anthropocene becomes amenable to world history: while most and perhaps all AMR mechanisms predate humans, the last two centuries have seen humans become a planetary force by creating an increasingly selective antimicrobial bottleneck that is reshaping the abundance of these mechanisms in microbial genomes across nearly all biogeographies.
Similar to the expansion of a specific dialect within an existing language, the resulting “anthropocene in [and around the microbial] cell” (D’Abramo and Landecker 2019) is not abstract but measurable. By combining genomic, ecological, biochemical, archaeological, and historical data, we can reconstruct how accelerating antimicrobial exposures radically amplified certain forms of microbial signalling such as AMR and not others, as well as relative shifts in microbial population abundance and diversity including extinction of host-associated population niches (Weinbauer and Rassoulzadegan, 2007; Gillings and Paulsen, 2014; Achmon et al., 2018). We can simultaneously use the dense web of traces these changes have left in the historical record via reports of antimicrobial treatment failure, changing disease ecologies, and altered fermentation processes (see below) to map how macrobial life was impacted and reacted – often by introducing further selective pressures.
Taking both the antiquity and speed of microbial signalling seriously thus allows us to answer Chakrabarty’s challenge not by ‘outscaling’ but by ‘inscaling’ the spatiotemporal frameworks with which we study the “relational ontologies” (Castree 2003) connecting micro- and macrobial life in the Antibiocene (Lorimer 2012; 2020; Greenhough 2012; Haraway 2013 [2008]; Hinchliffe 2022; Paxson 2008; Sariola and Gilbert 2020; Brives 2021). Fortunately, there are a variety of analytical frameworks we can draw on to orientate interdisciplinary debates about this new phase of human-microbial relations. If the Antibiocene is a cumulative externality of what environmental historians call the “great acceleration” (McNeill and Engelke 2016) of humanity’s impacts on planetary biogeochemical systems, we can analyse its’ inflection points and complex dynamics with tools developed for other acceleration externalities such as pollution and the wider human exposome (Gille and Lepawsky 2022; Webster and Mai 2021; Karlsson et al. 2021), the climate emergency (McNeill 2008; Chakrabarty 2009; Smith et al. 2011; McKibben 2011; Locher and Fressoz 2012; Mcneill 2015; Chakrabarty 2021), or biodiversity loss (Rose et al. 2017; Padilla 2021).
Eubiotic governance
At the conceptual level, the Antibiocene’s tracing of AMR to ‘inscale’ the broader Anthropocene provides an effective analytical framework with which to merge the evaluation of accelerating change at the level of microbial cells, genes, and communities, biochemical environments, and human societies. At the policy level, the concept’s interlayered approach to human-microbial relations also allows us to move beyond traditional short-termist concerns about antimicrobial efficacy and develop more long-term forms of eubiotic governance for our microbial commons.
Achieving the described multiscalar reorientation entails seeing the resistant microbe we encounter in a given moment as the end product – a living archive – of a series of interlayered short-, medium-, and long-term processes that constitute the broader Antibiocene. Historians ranging from the French Annales School to Reinhard Koselleck have long compared the analysis of individual temporal events to a geological mode of enquiry (Braudel and Wallerstein 2009; Koselleck 2003). Similar to a mineralogical sample, each temporal event must be studied as the cumulative outcome of multiple geological processes with different timescales, varying depths, and distinct features (Koselleck 2003). Keeping these different speeds, features, or time layers in mind is key when it comes to understanding the microbial environments around us and our place within them. Clinicians and patients rightly primarily see AMR in terms of an individual instance of treatment success or failure. However, as science studies scholar Hannah Landecker points out, the genetic and phenotypic traits of the infections we encounter simultaneously reflect decades of antimicrobial exposures and other selective pressures humans have historically brought to bear on microbial populations (Landecker 2016). Some of these additional pressures may be global such as human population growth, anthropogenic climatic shifts, exposure to co-selective substances such as heavy metals and biocides, and encroachment on new ecologies, but others may well be more local such as the built environments of specific cities and hospitals or shifting local land- and water-use patterns.
Keeping this genealogy of biosocial antimicrobial exposures and microbial reactions in mind is crucial when it comes to devising more sustainable policy solutions. At the societal level, acknowledging the Antibiocene’s interlayered spatiotemporal, biochemical, genomic, ecological, and social dynamics poses an inherent challenge to the traditionally short-termist, behaviourist, and pharmaceutical-oriented policies that have characterised the AMR space since the 1940s (Gradmann and Kirchhelle 2023). In the case of current antimicrobial stewardship efforts, understanding the full biochemical range of past and present anthropogenic AMR drivers shows the futility of reducing AMR governance to a challenge of individual responsibility for ‘correct’ drug use (Tompson and Chandler 2021). Interconnected microbiota and the cumulative legacies of antimicrobial exposures across multiple environments also reveal the limits of prioritising one aspect of the One Health triad over another. Conceptualising AMR as rooted in deeper time frames with multi-scalar eco-social drivers thus shifts the focus of interventions from pharmaceutical use by individuals and specific institutions towards broader eco-societal interventions. These structural interventions need to target both the socially entrenched dimensions of current antibiotic dependent “infrastructures” (Chandler 2019) and the still selective legacies of past pharmaceutical and non-pharmaceutical exposures.
The Antibiocene’s multiscalar reorientation of popular AMR discourse also enables us to move from policies that only target antimicrobial efficacy for individual bug-drug combinations to new modes of microbial governance. Despite its planetary importance, considerations of microbial life and the protection of microbial diversity have been mostly excluded from major international legal frameworks such as the 1993 UN Convention on Biodiversity or the 2010 Nagoya Protocol on Access And Benefit Sharing. The last 20 years have nonetheless seen a growing number of biomedical and social scientists conceive of a variety of conservation and stewardship frameworks for microbiota. In line with geographer Jamie Lorimer’s description of the recent turn towards “probiotic governance” (Lorimer 2020), much of this work has concentrated on conserving host-associated or rare microbiota and rewilding microbial ecologies in light of dysbiosis – a disruptive imbalance resulting in negative changes to a microbiota’s functional composition and metabolic activities (Cockell and Jones 2009; Cockell 2011; Trevelline et al. 2019; Redford 2023). Research has also focused on exploiting microbial adaptation to remediate polluted environments (Achmon et al. 2018) and preparing for microbial disasters and microbiota degradation (Guerra et al. 2021; Valliere et al. 2020; Smith and Casadevall 2022; Reese and Dunn 2018; Berg et al. 2020; Kirchhelle et al. 2020).
Social scientists have critiqued the anthropocentrism (Clark, 2011), uncritical affirmation of capitalist geopower (Chandler 2018; Yusoff 2016), and technological hubris (Hird and Yussof 2019) engrained in many of these approaches. The concept of the Antibiocene safeguards against overly ambitious technological solutions by highlighting the degree of change that has already occurred and moving the focus away from ‘fixing’ or restoring previous systems. Instead of trying to avert an ‘antibiotic apocalypse’, it opens the door for more realistic conceptualisations of what social scientist Christian Haddad terms the ‘eubiotic governance’ (Haddad 2023) of long since exposed microbiota. Moving from emergency response to long-term management (Kirchhelle and Roberts 2022), this new mode of eubiotic governance would aim to mitigate dysbiotic dynamics not only in human and animal health but across all three One Health domains. It would also aim to foster eubiotic relations between humans and microbes whilst acknowledging that eubiotic balance is subject to continuous change and only partially captured by existing metrics of antimicrobial sensitivity. In the short-term, such a shift could take the form of new cost-benefit guidance for farms and clinics that assess antimicrobials’ efficacy against individual microbes alongside wider dysbiotic impacts on local microbiota. Similar guidance for industry could use AMR measurements to factor the microbiota impacts of antimicrobial releases into resulting product costs and local and national regulations. In the medium-term, thinking through the planetary vulnerabilities and different speeds of antimicrobial exposure could pair “microbiome stewardship” (Peixoto et al. 2022) and investment in the remediation of antimicrobial exposures with an acknowledgement of the significant differences with which the Antibiocene’s fallouts have been distributed. Through the lens of the Antibiocene, ecological concepts of eubiotic balance thus become intimately paired with considerations of unequal exposures, temporal shifts, and (in)justice (Ishaq et al. 2021).
(Anti)microbial asymmetries
The centrality of risk distribution to planetary and environmental challenges has long been acknowledged by social scientists and humanities scholars. In his seminal Risk Society from 1986, sociologist Ulrich Beck noted that the prediction, management, and distribution of risk was one of the fundamental organising principles of modern societies and could mirror or even exacerbate pre-existing class inequalities (Beck 1986, 1994, 2007). Since then, a large body of scholarship has expanded and adapted Beck’s risk society concept by highlighting the historically sited nature of risk and examining how processes of exposure, distribution, and the creation of value via remediation have played out in the case of pollutants ranging from lead to persistent pesticides or endocrine disruptors (Vogel 2012; Mohun 2013; Boudia 2014; Boudia et al. 2018; Langston 2010; Vogel 2013; Langston 2014).
In the environmental humanities, questions of latency of exposure, visibility of toxic, radioactive, carcinogenic, and teratogenic risks, and what it means for communities to live in permanently polluted environments have proven particularly productive (Boudia et al. 2018; Boudia and Jas 2014; Creager 2014; Jas 2013; Schwerin 2010; Kirchhelle 2018c). Focusing on calamities such as radioactive fallout or climate change that “patiently dispense their devastation while remaining outside our flickering attention spans,” literary scholar Rob Nixon has developed the influential concept of “slow violence” (Nixon, 2011). In contrast to the direct violence of war or abuse, slow violence is characterised by “anonymous” and “accretive” (Nixon, 2011) processes that expose communities to significant levels of harm but are often initially invisible to scientists, activists, and regulators. Once effects become visible, structural asymmetries in the way certain communities and viewpoints ‘count’ allows negative externalities for these communities to be discounted from dominant risk-benefit calculations and leaves remediation efforts incomplete. Amounting to a permanent state of biochemical “siege” (Mbembé and Meintjes 2003) or “wearing out” (Berlant 2007), slow-violence often spans generations with historic sites of exploitation and deprivation such as former slave plantations and colonial territories hosting repeat waves of ‘violent’ polluting production and waste disposal practices (Hecht 2018; Davies 2018, 2022; Nixon 2011; Brown 2013).
Similar inequalities of exposure to antimicrobials, resulting risks, and opportunities for value creation are also at play within the Antibiocene. Far from being a global leveller, the biological and social effects of AMR have been felt unevenly. At the microbial level, differences in antimicrobial exposures mean that biogeographies of AMR vary significantly with metagenomic analyses of healthy human gut microbiomes indicating a clear correlation between ARG prevalence and regional antimicrobial usage per capita (Lee et al., 2023). At the societal level, vast differences in access to nutrition, healthcare, welfare, water, sanitation, and hygiene systems have moreover created significant inequalities of exposure to dysbiotic microbial environments, immunocompetence, and correlating risks posed by infectious disease and AMR. Often, there are significant multi-generational overlaps between sites of social vulnerability to microbial infection and microbial exposure to antimicrobials and AMR (Tompson and Chandler 2021; Ishaq et al. 2019, 2021). These overlaps of AMR selection and vulnerability – a veritable “stacking of lacks” (Sariola et al. 2022) – not only encompass sites of current antimicrobial usage in medicine and food production, but also the environmental domain in the form of antimicrobial residues in terrestrial, aquatic, and airborne environments.
While an ultimate escape from the impacts of our Antibiocene is impossible, risk mitigation is available at a price. Since the 1930s, consumers in wealthier parts of the world have not only driven antibiotic dependence in global health and food production infrastructures, but have also been able to purchase “quick fixes” (Willis and Chandler, 2019) for resulting exposure and AMR problems. These fixes encompass access to still effective forms of treatment such as reserve antibiotics and transplants of ‘healthy’ faecal microbiota from less exposed humans (Lorimer, 2020) as well as broader forms of risk minimisation or displacement such as ‘antibiotic-free’ food systems (Kirchhelle 2020), infection control and prevention, and the outsourcing of antimicrobial pollution to other parts of the world (see below). Highlighting the accretive and unequal fallouts of chronic multi-generational antimicrobial exposures as well as the economies of microbial value creation and risk mitigation must thus be central to engaging with the biosocial complexities of the Antibiocene as well as any form of ‘eubiotic governance’ and “Just Transition” for AMR (Just Transitions for AMR Working Group et al. 2023).
Unearthing the Antibiocene: studying life at sites of hyperexposure
Although there is no one correct approach to studying a planetary event, comparing interactions of microbes, genes, and macrobes across sites of extreme chronic antimicrobial exposure is a productive way of unearthing the biosocial and spatiotemporal scales of the Antibiocene.
This unearthing is especially important when it comes to understanding the long-term dynamics of antimicrobial exposures and microbiota adaptations in different environments. Despite over 25 years of systematised AMR surveillance in high-income countries and significant recent advances in metagenomics (Kirchhelle 2020), our knowledge of the differential impacts of environmental antimicrobial exposures on human and non-human communities remains limited (Larsson and Flach, 2022). In the case of AMR, microbiologists have highlighted aquatic and terrestrial environments as reservoirs of antibiotic resistance genes (ARGs) and resistant organisms since ca. 1970 (Cycoń, Mrozik, and Piotrowska-Seget 2019; Levy, FitzGerald, and Macone 1977; Regnier and Park 1972; H.W. Smith 1970, 1971; Weary et al. 1972). However, AMR burdens can vary significantly between different biogeographies. Recent global surveys of ARGs seem to confirm the 1934 Baas Becking hypothesis whereby “everything is everywhere, but the environment selects” (De Wit and Bouvier 2006) – but do not always agree on what it is in an environment that selects. A 2022 analysis of 1088 soil metagenomes found that ARGs conferring multidrug resistance were particularly abundant in temperate areas impacted by human habitation, agricultural activity, and associated pollutant and nutrient inputs (Zheng et al. 2022). By contrast, a parallel survey of 757 sewage samples from 101 countries confirmed the global distribution of ARGs but also reported differences in the clustering of ARGs between distinct biogeographies and higher prevalence of ARGs in water samples from hotter than temperate climates (Munk et al. 2022).
Understanding the relationship between the varying cellular, genomic, and metabolic ecosystem-level impacts of antimicrobial exposures on microbial communities becomes even more complicated when one moves to the medium- and long-term. Many studies have explored how microbial communities react to short-term clinical and environmental antimicrobial exposures over the period of days, weeks, and months. However, far less is known about the effects of longer-term microbiota exposure to different antimicrobial concentrations as well as the complex biotic and abiotic dynamics involved in antimicrobial degradation over years and decades. How do initial antimicrobial inputs in one environment change over 50 years or a century? Are there critical concentrations of exposure at which mutation rates and evolutionary adaptation accelerate? How significant was the evolutionary pressure created by the antibiotic era as opposed to already rising levels of antimicrobial selection of heavy metals during the Industrial Era? How do differences in the volume of initial antimicrobial pollution and in the long-term bioavailability of various antimicrobial substances impact local and regional microbiota (Cycoń et al. 2019, Larsson and Flach, 2022)? Can long-term reductions of exposure to certain selection pressures in one region ever lead to a sustained restoration of bacterial sensitivity? Answering these questions is crucial not only for developing more sustainable forms of antimicrobial production, usage, and remediation, but also for exploring how the Antibiocene has already transformed human-microbial relations.
A particularly promising approach to unpacking the described spatiotemporal, genomic, biochemical, and social dynamics of the Antibiocene is to conduct comparative longitudinal analyses of sites of particularly extreme chronic antimicrobial pollution. For decades, certain environments such as landfills and catchment areas collecting liquid or solid waste from hospitals, intensive animal feed operations, or pharmaceutical factories have functioned as sites of hyperexposure where antimicrobial concentrations far exceed those of other environments (Zeeshan Qadar, Thane, and Haworth-Brockman 2021; Kotwani, Joshi, and Kaloni 2021; Taneja and Sharma 2019; Adelowo, Ojo, and Fagade 2009; Anand et al. 2021; Marshall and Levy 2011; Levy, FitzGerald, and Macone 1977). In 2018, Achmon et al. already proposed a microbiological mapping of the Anthropocene through the lens of sealed landfills. Referring to these environments as xeno-ecological niches (XENS), the authors noted that local microbiomes could be analysed for signs of functional adaptation, potential biotechnological remediation pathways, and dating the Anthropocene (Achmon et al 2018). In a similar vein, social and environmental scientists have used investigations of polluted landfills and rivers to explore the multi-species relations of “wasting and exposure that cohere around human detritus” (Hird and Yussof 2019; Hird 2016a, b; Vaverková and Koda 2023; Kraemer, Ramachandran, and Perron 2019; Broom and Doron 2022; Doron and Broom, 2019). However, so far, most investigations have either limited themselves to studying the period after 1945 or failed to engage in the comparative analysis of sites across multiple biogeographies.
Unearthing the spatiotemporal dynamics of the unfolding Antibiocene depends on establishing a broader integrative research agenda that does not limit histories of antimicrobial exposure to the antibiotic era and compares relevant biological, chemical, and historical markers across a range of geographies and societal contexts. At the biochemical level, analysing current antimicrobial activity in different strata alongside historical data on the identity and volume of initial antimicrobial inputs can be used to assess decomposition rates in different environments. Comparing data across sites can also be used to assess the planetary ‘background signal’ left by two centuries of antimicrobial exposures. At the genomic level, relevant markers of the Antibiocene may range from the expanding presence of individual ARGs to shifts in the species composition of microbiota and the presence of mobile genetic elements such as plasmids and integron cassettes, which are particularly likely to confer AMR. Resulting longitudinal data on population structures and genotypes of exposed microbiota can be compared with archived samples in microbial culture collections, historical environmental isolates (e.g. soil archives), as well as data from less exposed sites. At the historical level, genomic and biochemical data on exposures and microbial adaptation can be complemented with a systematic reconstruction of contemporary observational data on shifting human-microbial relations via recorded phenotypes, AMR profiles, and broader microbiota dynamics (see below). Combining the analysis of these biochemical, genetic, and historical markers will help us better understand the spatiotemporal extent of the Antibiocene, its points of genomic and biochemical acceleration, the role of biogeographies in amplifying or muting AMR proliferation, and why – despite decades of antimicrobial exposures – we have not seen more organisms develop pan-resistance to the antibiotics we rely on.
In addition to this excavational research, historical and social sciences analyses of the human communities living at identified sites of hyper-exposure can lead to a better understanding of the adaptations that chronic antimicrobial exposures triggers at the level of the individual and society. As beings who are inhabited by and depend on the trillions of microbial organisms in, on, and around our bodies (Sender, Fuchs, and Milo 2016), this necessarily includes paying equal attention to the human and non-human stories we encounter in the archives and the field. Working with epidemiologists, historians can use archival data to pinpoint likely sites of historical exposure and reveal the practices that led to their initial contamination as well as subsequent remediation attempts. They can also systematically search for resulting health impacts in archived clinical reports and public health data. Moving beyond immediate questions of antimicrobial contamination and therapeutic efficacy, historians and social scientists can also look for broader environmental impacts of the antimicrobial era by creatively examining new types of sources. A good place to start looking for traces of the Antibiocene is in the records and vernacular knowledge of professions tasked with managing microbial processes and waste. In the case of aquatic and terrestrial environments, this may include interviewing and analysing reports and diaries of the engineers, farmers, and planners dealing with the growing global volumes of solid and liquid waste produced by pharmaceutical plants, urban communities, and concentrated animal populations. During the 1960s, engineers at Merck’s Stonewall Plant on the Shenandoah River reported on their ability to handle tens of thousands of tons of biologically active and heavily contaminated wastes with a mix of inorganic and organic processes. They also expressed great interest in the ‘probiotic’ effects of ploughing under vast quantities of antimicrobial wastes on company land as well as the rich amount of micro- and macrobial life proliferating on sewage filters (Horne et al. 1962). Because of engineers’ dependence on microorganisms to break down organic matter in activated sludge, there are many further traces of unexpected antimicrobial impacts such as the need to ‘top up’ industrial waste plants with raw microbe-rich sanitary waste to deal with “strong” (Muss 1951) penicillin residues.
Similarly revealing discussions about the Antibiocene are present in documents deposited by industries, who depended on harnessing microbial labour. Workers at dairies, breweries, and pharmaceutical plants were quick to notice changes in the performance of the microbial cultures they employed. They were also amongst the first to engage in what anthropologist Anna Lowenhaupt Tsing has called “salvage accumulation” (Tsing 2015) by finding ways of integrating resistant organisms and ARGs into capitalist supply chains. In the case of dairies, complaints about antimicrobial impacts on microbial fermentation, the need for resistant starter cultures, and concerns about resistant pathogens such as staphylococci and streptococci in cheese became common place from the 1950s onwards (Smith-Howard 2010; Trembath 1950; Thatcher and Simon 1955; Thatcher and Ross 1960). In the brewing industry, the observation that many industrial microorganisms were resistant to biological antibiotics led to great interest in using antibiotics to purify brewing yeasts and preserve beer and monitoring for AMR selection (Green 1955; Portno 1968). Meanwhile, the ability to isolate, manipulate, and transfer, and patent formerly ‘wildtype’ ARGs has come to underpin a global recombinant infrastructure of microbial cell factories producing substances ranging from human insulin to acetone and monoclonal antibodies (Rasmussen 2014). Once one starts searching, traces and human impacts of the Antibiocene appear throughout the archives of modern industry, agriculture, medicine, science, and government.
Social scientists and historians can also use investigations of sites of antimicrobial hyperexposure to decipher how societies have made sense of resulting risks. In line with geographer Steve Hinchliffe’s call to integrate postcolonial with ‘post-colony’ approaches to health and microbes (Hinchliffe 2022), researchers are already studying how expert and vernacular perceptions of ecological change, disease risks, and AMR exposure influence “environmental imaginaries” (Helliwell et al. 2021) and societal behaviours such as altered antimicrobial usage, production and health care practices, or resource use (Broom et al. 2020; Doron and Broom 2019; Hinchliffe, Butcher, and Rahman 2018; Kirchhelle 2020; Nayiga et al. 2022). Adopting this ‘post-colony’ framework is also useful when it comes to studying the shifting geographies of antimicrobial pollution. While early antimicrobial manufacturing sites were primarily located in high- and medium-income countries, cost pressures, patent expiries, and development plans led to a relocation of active pharmaceutical ingredient (API) production and packaging to emerging economies from the 1970s (Wellcome Trust & Boston Consulting Group 2022; Greene 2014; Mackintosh et al. 2016; Nishino 2022; Rajan 2017). The outsourcing of production capacities opened new revenue streams for low- and middle-income countries (WHO 2017; Greene 2014) but also exposed poor communities in former colonial settings to some of the most extreme human-made antimicrobial environments on earth (Lübbert et al. 2017; Doron and Broom 2019). Studying resulting ecological and health impacts and community-level adaptations is crucial to mapping both the ‘slow violence’ of globalised antimicrobial pollution and how local action can mitigate resulting fallouts. Learning from vernacular practices of managing disease and AMR risks in farming and health care can be an effective way to adapt and add value to frequently context-devoid international stewardship efforts (Hinchliffe, Butcher, and Rahman 2018; Doron and Broom 2019; Broom and Doron 2022; Sariola et al. 2022). This is certainly true for antimicrobial pollution. In 2020, India reacted to sustained local and international activism by becoming the first country to challenge industry-set wastewater standards and devise statutory limits on antimicrobials in water (ReACT Group, 2020). With a growing number of countries onshoring antibiotic production (Anon 2021; EU Parliament 2021), Indian experiences in highly exposed locations such as Hyderabad will hold important lessons for international debates on antimicrobial pollution mitigation and challenge entrenched ‘North-South’ flows of antimicrobial policy (Gradmann and Kirchhelle 2023).
From apocalypse to remediation?
Much ink has already been spilt on the Anthropocene – as well as the various linguistic offshoots it has created (Hickmann et al. 2019). While some readers will undoubtedly disagree with the proposed concept of an Antibiocene, there is little to be lost in expanding narrow traditional understandings of AMR as treatment failure. Studying AMR as a pheno- and genotypic signal of a new era of human-microbial relations characterised by multiple accelerating antimicrobial exposures is not to deny the urgent need to address the threat to lives and livelihoods posed by resistant pathogens. Rather, it is to create an integrative framework that pays appropriate attention to the broader ecosystems challenge posed by two centuries of accelerating pharmaceutical and non-pharmaceutical antimicrobial exposures, the startling inequalities with which health and environmental fallouts have been distributed, and the need to reorientate short-termist antibiotic stewardship to respond to these long-term challenges.
Such an integrative framework should not automatically prioritise traditional clinical or productivity viewpoints but merge perspectives from across the biological, medical, and social sciences as well as the humanities. Learning from academic and policy responses to other Anthropocene-related challenges, it should also actively engage with questions of social equity, risk distribution, and the slow violence of chronic antimicrobial exposures. Paying attention to the inequalities and variability of selective exposures within the Antibiocene relativises the long-standing dominance of high-income perspectives on AMR and international antimicrobial policies. It also allows us to take seriously and learn from the lived experiences of many often marginalised communities when it comes to living with and adapting to chronic antimicrobial exposures.
As proposed in this thought piece, one way of achieving the required interlayering of disciplinary, societal, and geographic perspectives may be to systematically investigate and compare sites of past and present antimicrobial hyperexposure across multiple biogeographies. Resulting data can shed important light on the interrelation of antimicrobial exposures, AMR selection, and broader microbiota shifts – as well as on how macrobial communities have adapted to, remediated, and in some cases engaged in salvage accumulation within permanently altered microbial environments. By revealing the extent to which our various biogeographies have already been altered and what future dynamics of the Antibiocene may look like, these interdisciplinary investigations can challenge notions of ‘indifferent’ microbial time and give rise to a new contextual mode of policy-making: if we cannot return to a pre-antibiotic era, how do we manage the microbial commons as well as orientate (anti)microbial stewardship and remediation efforts moving forward? Answers will not be straightforward either from a microbiological or societal perspective and microbial eubiosis for one community may well entail dysbiosis or socio-economic burdens for another. However, after almost two centuries of accelerating antimicrobial exposures, it is time to move from merely conserving pharmaceutical efficacy to stewarding our wider microbial biosphere.
Data availability
Data sharing is not applicable to this research as no data were generated or analysed.
Notes
The Antibiocene is a portmanteau consisting of a the prefix “antibio-“ from the word antibiosis meaning the antagonism resulting from the toxicity of secondary metabolites produced by one organism for other microorganisms and the suffix “-cene” from the Greek kainos meaning recent.
In the US alone, over 10,449 tons of antimicrobial drugs were actively marketed to food-producing animals in 2020 (FDA 2021).
References
Abrudan MI, Smakman F, Grimbergen AJ, Westhoff S, Miller EL, Van Wezel GP, Rozen DE (2015) Socially mediated induction and suppression of antibiosis during bacterial coexistence. PNAS 112(35):11054–11059
Achmon Y, Achmon M, Dowdy FR, Spiegel O, Claypool JT, Toniato J, Simmons CW (2018) Understanding the Anthropocene through the lens of landfill microbiomes. Frontiers in Ecology and the Environment 16(6):354–360
Adelowo OO, Ojo FA, Fagade OE (2009) Prevalence of multiple antibiotic resistance among bacterial isolates from selected poultry waste dumps in Southwestern Nigeria. World Journal of Microbiology and Biotechnology 25(4):713–719
Anand U, Reddy B, Singh VK, Singh AK, Kesari KK, Tripathi P, Kumar P, Tripathi V, Simal-Gandara J (2021) Potential environmental and human health risks caused by antibiotic-resistant bacteria (ARB), antibiotic resistance genes (ARGs) and emerging contaminants (ECs) from municipal solid waste (MSW) landfill. Antibiotics 10(4):374
Anon (1966) Infectious drug resistance. New England Journal of Medicine 275(5):277
Anon (2021) US Onshoring Essential Antibiotics Act Seeks to Re-Localize Production of Essential Antibiotics. Eversana, 28.04.2021, https://www.eversana.com/2021/04/28/us-onshoring-essential-antibiotics-act-seeks-to-re-localize-production-of-essential-antibiotics/
Baker S, Thomson N, Weill F-X, Holt KE (2018) Genomic insights into the emergence and spread of antimicrobial-resistant bacterial pathogens. Science 360(6390):733–738
Barad K (2007) Meeting the Universe Halfway. Quantum Physics And The Entanglement Of Matter And Meaning. Duke University Press, Durham
Beck U (1986) Risikogesellschaft. Auf dem Weg in eine andere Moderne. Suhrkamp, Frankfurt a. M
Beck U (1994) The Reinvention of Politics: Towards a Theory of Reflexive Modernization. In: Beck U (ed) Reflexive Modernization. Politics, Tradition and Aesthetics in the Modern Social Order. Stanford University Press, Stanford, p 1–55
Beck U (2007) Weltrisikogesellschaft. Auf der Suche nach der verlorenen Sicherheit. Suhrkamp, Frankfurt am Main
Berg G, Rybakova D, Fischer D, Cernava T, Vergès M-CC, Charles T, Chen X, Cocolin L, Eversole K, Corral GH (2020) Microbiome definition re-visited: old concepts and new challenges. Microbiome 8(1):1–22
Berlant L (2007) Slow death (sovereignty, obesity, lateral agency). Critical inquiry 33(4):754–780
Boudia S, Creager ANH, Frickel S, Henry E, Jas N, Reinhardt C, Roberts J (2018) Residues: rethinking chemical environments. Engaging Science, Technology, and Society 4:165–178
Boudia S (2014) Managing Scientific and Political Uncertainty. Environmental Risk Assessment in a Historical Perspective. In: Boudia S, Jas N (eds) Powerless Science? Science and Politics in a Toxic World. Berghahn, New York and Oxford, p 95–112
Boudia S, Jas N (eds) (2014) Powerless Science? Science and Politics in a Toxic World. Berghahn, New York and Oxford
Braudel F, Wallerstein I (2009) History and the social sciences: the longue durée. Review (Fernand Braudel Center) 32(2):171–203
Brives C (2021) Plurbiosis and the never-ending microgeohistories. In: Brives C, Rest M, Sariola S (eds) With Microbes. Mattering Press, Manchester, p 247–267
Broom A, Doron A (2022) Resistant bugs, porous borders and ecologies of care in India. Social Science & Medicine 292:114520
Broom A, Kenny K, Kirby E, George N, Chittem M (2020) Improvisation, therapeutic brokerage and antibiotic (mis)use in India: a qualitative interview study of Hyderabadi physicians and pharmacists. Critical Public Health 30(1):16–27
Brown KL (2013) Plutopia: Nuclear families, atomic cities, and the great Soviet and American plutonium disasters. Oxford University Press, Oxford
Bud R (2007) Penicillin: triumph and tragedy. Oxford University Press, Oxford
Castree N (2003) Environmental issues: relational ontologies and hybrid politics. Prog Hum Geogr 27(2):203–211
Chakrabarty D (2009) The climate of history: four theses. Critical Inquiry 35(2):197–222
Chakrabarty D (2018) Anthropocene time. History and Theory 57(1):5–32
Chakrabarty D (2021) The climate of history in a planetary age. University of Chicago Press, Chicago
Chandler CIR (2019) Current accounts of antimicrobial resistance: stabilisation, individualisation and antibiotics as infrastructure. Palgrave communications 5:1
Chandler CIR, Hutchinson E, Hutchison C (2016) Addressing antimicrobial resistance through social theory: an anthropologically oriented report. London School of Hygiene & Tropical Medicine, London
Chandler D (2018) Ontopolitics in the Anthropocene: An Introduction to Mapping, Sensing, and Hacking. Taylor & Francis, London
Changing Markets and Ecostorm (2016) Superbugs in the Supply Chain: How pollution from antibiotics factories in India and China is fuelling the global rise of drug-resistant infections. https://epha.org/wp-content/uploads/2016/10/Superbugsinthesupplychain_CMreport.pdf
Clark N (2011) Inhuman nature: sociable living on a dynamic planet. SAGE Publications, Thousand Oaks
Clemente JC, Erica CP, Blaser MJ, Kuldip S, Zhan G, Wang B, Magris M, Hidalgo G, Contreras M, Noya-Alarcón Ó, Lander O, McDonald J, Cox M, Walter J, Phaik LO, Rulz JF, Rodriguez S, Shen N, Song SJ, Metcalf J, Knight R, Dantas G, Dominguez-Bello MG (2015) The microbiome of uncontacted Amerindians. Science Advances 1(3):1–12
Cockell CS (2011) Microbial rights? EMBO reports 12(3):181
Cockell CS, Jones HL (2009) Advancing the case for microbial conservation. Oryx 43(4):520–526
Cohen ML (1992) Epidemiology of drug resistance: implications for a post—antimicrobial era. Science 257(5073):1050–1055
Creager ANH (2014) The Political Life of Mutagens. A History of the Ames Test. In: Boudia S, Jas N (eds) Powerless Science? Science and Politics in a Toxic World. Berghahn, New York and Oxford, p 46–64
Crutzen PJ (2006) The ‘Anthropocene’. In: Eckart E, Krafft T (eds) Earth System Science in the Anthropocene. Springer, Berlin, Heidelberg and New York, p 13–18
Cycoń M, Mrozik A, Piotrowska-Seget Z (2019) Antibiotics in the soil environment—degradation and their impact on microbial activity and diversity. Front Microbiol 10:338
D’Abramo F, Landecker H (2019) Anthropocene in the Cell. Technosphere Magazine (20.03.2019): 1–7, https://www.anthropocene-curriculum.org/contribution/anthropocene-in-the-cell
Davies S (2013b) Annual Report of the Chief Medical Officer. Volume Two, 2011: Infections and the rise of antimicrobial resistance. Department of Health, London
Davies S (2013a) The Drugs Don’t Work: A Global Threat. Penguin Books, London
Davies T (2018) Toxic space and time: Slow violence, necropolitics, and petrochemical pollution. Annals of the American Association of Geographers 108(6):1537–1553
Davies T (2022) Slow violence and toxic geographies:‘Out of sight’to whom? Environment and Planning C: Politics and Space 40(2):409–427
De Wit R, Bouvier T (2006) Everything is everywhere, but, the environment selects’; what did Baas Becking and Beijerinck really say? Environ Microbiol 8(4):755–758
Destoumieux-Garzón D, Mavingui P, Boetsch G, Boissier J, Darriet F, Duboz P, Fritsch C, Giraudoux P, Roux FL, Morand S (2018) The one health concept: 10 years old and a long road ahead. Front Vet Sci 5:14
Doron A, Broom A (2019) The Spectre of Superbugs: Waste, Structural Violence and Antimicrobial Resistance in India. Worldwide Waste: Journal of Interdisciplinary Studies 2(1):1–10
Druschel GK, Kappler A (2015) Geomicrobiology and microbial geochemistry. Elements 11(6):389–394
Dubos R (1942) Microbiology. Annual Review of Biochemistry 11:659–678
Dubos R (1987) Mirage of Health: Utopias, Progress and Biological Change. Rutgers University Press, New Brunswick, [1959]
Dubos R (1985 [1965]) Man Adapting. Yale University Press, New Haven
EU Parliament (2021) Post Covid-19 value chains: options for reshoring production back to Europe in a globalised economy. EU Parliament: Policy Department for External Relations Directorate General for External Polices of the Union, Brussels
FAO/WHO (2019) Joint FAO/WHO Meeting in collaboration with OIE on Foodborne Antimicrobial Resistance: Role of the Environment, Crops and Biocides. Food and Agriculture Organisation, Rome
FAO, OIE, WHO, and UNEP (2022) Together For One Health. Strategic Framework for collaboration on antimicrobial resistance. World Health Organisation, Geneva
FDA (2021) 2020 - Summary Report on Antimicrobials Sold or Distributed for Use in Food-Producing Animals. Food and Drugs Administration, Washington DC
Gibson B, Wilson DJ, Feil E, Eyre-Walker A (2018) The distribution of bacterial doubling times in the wild. Proceedings of the Royal Society B 285(1880):20180789
Gille Z, Lepawsky J (eds) (2022) The Routledge Handbook of Waste Studies. Routledge, New York and Abingdon
Gillings MR, Paulsen IT (2014) Microbiology of the Anthropocene. Anthropocene 5:1–8
Gradmann C (2011) Magic bullets and moving targets: antibiotic resistance and experimental chemotherapy, 1900-1940. Dynamis 31(2):305–321
Gradmann C, Kirchhelle C (2023) Pills and Politics – a historical analysis of international antibiotic regulation since 1945. In: Rubin O, Bækkeskov E, Munkholm L (eds) Steering against Superbugs – The Global Governance of Antimicrobial Resistance. Oxford University Press, Oxford, p 19-42
Gradmann C (2018) From lighthouse to hothouse: hospital hygiene, antibiotics and the evolution of infectious disease, 1950-1990. Hist Philos Life Sci 40:1–25
Green SR (1955) A review of differential techniques in brewing microbiology. Proceedings. Annual meeting-American Society of Brewing Chemists 13(1):107–119
Greene JA (2014) Generic: The unbranding of modern medicine. Johns Hopkins University Press, Baltimore
Greenhough B (2012) Where species meet and mingle: Endemic human-virus relations, embodied communication and more-than-human agency at the Common Cold Unit 1946–90. Cult Geogr 19(3):281–301
Grenni P (2022) Antimicrobial resistance in rivers: a review of the genes detected and new challenges. Environmental Toxicology and Chemistry 41(3):687–714
Guerra CA, Delgado‐Baquerizo M, Duarte E, Marigliano O, Görgen C, Maestre FT, Eisenhauer N (2021) Global projections of the soil microbiome in the Anthropocene. Global Ecology and Biogeography 30(5):987–999
Haddad C (2023) Beyond control: from antibiotics crises to ‘eubiotic politics’ in the post-pharmaceutical era. Presentation at the Medical Anthropology Seminar, London School of Hygiene and Tropical Medicine, 9 May, 2023. Recording available at: https://www.lshtm.ac.uk/newsevents/events/beyond-control-antibiotics-crises-eubiotic-politics-post-pharmaceutical-era
Haraway DJ (2013) When Species Meet. University of Minnesota Press, Minneapolis, [2008]
Häusler T (2006) Viruses vs. Superbugs. A Solution To The Antibiotics Crisis. Macmillan, New York and Basingstoke
Hecht G (2018) Interscalar vehicles for an African Anthropocene: On waste, temporality, and violence. Cultural Anthropology 33(1):109–141
Helliwell R, Raman S, Morris C (2021) Environmental imaginaries and the environmental sciences of antimicrobial resistance. Environment and Planning E: Nature and Space 4(4):1346–1368
Hickmann Thomas, Partzsch Lena, Pattberg Philipp, Weiland Sabine (eds) (2019) The anthropocene debate and political science. Routledge, Abingdon and New York
Hinchliffe S (2022) Postcolonial global health, post-colony microbes and antimicrobial resistance. Theory, Culture & Society 39(3):145–168
Hinchliffe S, Butcher A, Rahman MM (2018) The AMR problem: demanding economies, biological margins, and co-producing alternative strategies. Palgrave Commun 4
Hird MJ (2010) Indifferent globality. Theory, Culture & Society 27(2-3):54–72
Hird MJ (2016b) The Phenomenon of Waste-World-Making. Rhizomes: Cultural Studies in Emerging Knowledge 30:2016
Hird MJ (2016a) Burial and resurrection in the Anthropocene: Infrastructures of waste. In: Harvey P, Jensen C, Morita A (eds) Infrastructures and Social Complexity: A Routledge Companion. Routledge, London, p 242–252
Hird MJ, Yusoff K (2019) Lines of Shite. In: Braidotti R, Bignall S (eds) Posthuman Ecologies: Complexity and Process after Deleuze. Rowan & Littlefield, London & New York, p 265–281
Holt KE, Parkhill J, Mazzoni CJ, Roumagnac P, Weill F-X, Goodhead I, Rance R, Baker S, Maskell D, Wain J, Dolecek C, Achtman M, Dougan G (2008) High-through-put sequencing provides insights into variation and evolution in Salmonella Typhi. Nat Genet 40:987–93
Horne WR, Hartman HE, Rinaca US, St. Clair SL (1962) Biological treatment of fine chemical plant wastes. J Water Pollut Control Fed 34(8):833–846
Huang R, Ding P, Huang D, Yang F (2015) Antibiotic pollution threatens public health in China. Lancet 385(9970):773–774
Ishaq SL, Rapp M, Byerly R, McClellan LS, O’Boyle MR, Nykanen A, Fuller PJ, Aas C, Stone JM, Killpatrick S (2019) Framing the discussion of microorganisms as a facet of social equity in human health. PLoS biology 17(11):e3000536
Ishaq SL, Parada FJ, Wolf PG, Bonilla CY, Carney MA, Benezra A, Wissel E, Friedman M, DeAngelis KM, Robinson JM (2021) Introducing the Microbes and Social Equity Working Group: considering the microbial components of social, environmental, and health justice. MSystems 6(4):e00471–21
Jara D, Bello-Toledo H, Domínguez M, Cigarroa C, Fernández P, Vergara L, Quezada-Aguiluz M, Opazo-Capurro A, Lima CA, González-Rocha G (2020) Antibiotic resistance in bacterial isolates from freshwater samples in Fildes Peninsula, King George Island, Antarctica. Scientific Reports 10(1):1–8
Jas N (2013) Adapting To ‘Reality’: The Emergence Of An International Expertise On Food Additives And Contaminants In The 1950s And Early 1960s. In: Jas N, Boudia S (eds) Toxicants, Health and Regulation Since 1945. Pickering & Chatto, London, p 47–69
Just Transitions for AMR Working Group (2023) A Just Transition for AMR: Planning for an equitable and sustainable future with antimicrobial resistance. Lancet
Karlsson O, Rocklöv J, Lehoux AP, Bergquist J, Rutgersson A, Blunt MJ, Birnbaum LS (2021) The human exposome and health in the Anthropocene. International Journal of Epidemiology 50(2):378–389
Kirchhelle C (2018b) Swann Song. British antibiotic regulation in livestock production (1953-2006). Bulletin of the History of Medicine 92(2):317–350
Kirchhelle C (2018c) Toxic Tales—Recent Histories of Pollution, Poisoning, and Pesticides (ca. 1800–2010). NTM Zeitschrift für Geschichte der Wissenschaften, Technik und Medizin 26(2):213–229
Kirchhelle C (2020) Pyrrhic Progress: Antibiotics in Anglo-American Food Production (1949-2018). Rutgers University Press, New Brunswick
Kirchhelle C, Roberts AP (2022) Embracing the monsters: moving from infection control to microbial management. Lancet Microbe 3(11):e806–7
Kirchhelle C, Atkinson P, Broom A, Chuengsatiansup K, Ferreira JP, Fortané N, Frost I, Gradmann C, Hinchliffe S, Hoffman SJ (2020) Setting the standard: multidisciplinary hallmarks for structural, equitable and tracked antibiotic policy. BMJ Global Health 5(9):e003091
Kirchhelle C (2018a) Pharming animals: a global history of antibiotics in food production (1935–2017). Palgrave Commun 4
Knapp CW, Dolfing J, Ehlert PAI, Graham DW (2010) Evidence of increasing antibiotic resistance gene abundances in archived soils since 1940. Environ Sci Technol 44(2):580–587
Koselleck R (2003) Zeitschichten. Studien zur Historik. Suhrkamp, Frankfurt aM
Kotwani A, Joshi J, Kaloni D (2021) Pharmaceutical effluent: a critical link in the interconnected ecosystem promoting antimicrobial resistance. Environmental Science and Pollution Research 28(25):32111–32124
Kraemer SA, Ramachandran A, Perron GG (2019) Antibiotic pollution in the environment: from microbial ecology to public policy. Microorganisms 7(6):180
Kümmerer K (2009) Antibiotics in the aquatic environment–a review–part II. Chemosphere 75(4):435–441
Landecker H (2016) Antibiotic Resistance and the Biology of History. Body & Society 22(4):1–34
Landecker H (2019) Antimicrobials before antibiotics: war, peace, and disinfectants. Palgrave Commun 5(1)
Langston N (2010) Toxic bodies. Hormone Disruptors and the legacy of DES. Yale University Press, New Haven and London
Langston N (2014) Precaution and the History of Endocrine Disruptors. In: Boudia S, Jas N (eds) Powerless Science? Science and Politics in a Toxic World. Berghahn, New York and Oxford, p 29–45
Larsson DGJ, Flach C-F (2022) Antibiotic resistance in the environment. Nature Reviews Microbiology 20(5):257–269
Lee K, Raguideau S, Sirén K, Asnicar F, Cumbo F, Hildebrand F, Segata N, Cha C-J, Quince C (2023) Population-level impacts of antibiotic usage on the human gut microbiome. Nature Communications 14(1):1191
Lenski R (2020) We Interrupt this Nasty Virus with Some Good News about Bacteria. In: Teliamed Revisited (Blog). 24.02.2020. https://telliamedrevisited.wordpress.com/2020/02/24/we-interrupt-this-nasty-coronavirus-with-some-good-news-about-bacteria/
Lesch JE (2007) The First Miracle Drugs. How The Sulfa Drugs Transformed Medicine. Oxford University Press, Oxford
Liu G, Thomsen LE, Olsen JE (2022) Antimicrobial-induced horizontal transfer of antimicrobial resistance genes in bacteria: A mini-review. Journal of Antimicrobial Chemotherapy 77(3):556–56
Locey KJ, Lennon JT (2016) Scaling laws predict global microbial diversity. PNAS 113(21):5970–5975
Locher F, Fressoz J-B (2012) Modernity’s Frail Climate: A Climate History of Environmental Reflexivity. Critical Inquiry 38(3):579–598
Lorimer J (2012) Multinatural geographies for the Anthropocene. Prog Hum Geogr 36(5):593–612
Lorimer J (2020) The Probiotic Planet: Using Life to Manage Life. University of Minnesota Press, Minneapolis
Lübbert C, Baars C, Dayakar A, Lippmann N, Rodloff AC, Kinzig M, Sörgel F (2017) Environmental pollution with antimicrobial agents from bulk drug manufacturing industries in Hyderabad, South India, is associated with dissemination of extended-spectrum beta-lactamase and carbapenemase-producing pathogens. Infection 45(4):479–491
Mackintosh M, Banda G, Tibandebage P, Wamae W (eds) (2016) Making Medicines in Africa. The Political Economy of Industrializing for Local Health. Palgrave Macmillan, Houndsmills Basingstoke
Margulis L, Sagan D (2007) Dazzle gradually: Reflections on the nature of nature. Chelsea Green Publishing, White River Junction
Marinelli F, Genilloud O (2013) Antimicrobials: new and old molecules in the fight against multi-resistant bacteria. Springer Science & Business Media, Heidelberg
Marshall BM, Levy SB (2011) Food Animals and Antimicrobials: Impacts on Human Health. Clinical Microbiology Reviews 24(4):718–733
Mbembé J-A, Meintjes L (2003) Necropolitics. Public Cult 15(1):11–40
McKenna M (2010) Superbug. The Fatal Menace of MRSA. Free Press, New York
McKibben B (2011) Eaarth. Making A Life On A Tough Planet. St. Martin’s Griffin Edition, New York
McKie R (2017) Antibiotic apocalypse. The Guardian 08.10.2017
McNeill JR, Engelke P (2016) The Great Acceleration: An Environmental History of the Anthropocene Since 1945. Harvard University Press, Cambridge M.A
McNeill JR (2008) Can History Help Us With Global Warming? In: Campbell Kurt (ed) Climatic Cataclysm: The Foreign Policy and National Security Implications of Climate Change. Brookings Institution Press, Washington D.C., p 26–48
Mcneill JR (2015) Energy, population, and environmental change since 1750: entering the Anthropocene. In: McNeill J, Pomeranz K (eds) The Cambridge World History. Vol. 7. Production, Destruction and Connection, 1750–Present, Part 1: Structures, Spaces, and Boundary Making. Cambridge University Press, Cambridge, p 51–82
Mohun AP (2013) Risk. Negotiating Safety in American Society. Johns Hopkins University Press, Baltimore
Munk P, Brinch C, Duus Møller F, Petersen TN, Hendriksen RS, Mette Seyfarth A, Kjeldgaard JS, Aaby Svendsen C, Van Bunnik B, Berglund F (2022) Genomic analysis of sewage from 101 countries reveals global landscape of antimicrobial resistance. Nature Communications 13(1):1–16
Murray CJL, Ikuta KS, Sharara F, Swetschinski L, Aguilar GR, Gray A, Han C, Bisignano C, Rao P, Wool E et al. (2022) Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet 399(10325):629–655
Muss DL (1951) The treatment of penicillin wastes. Sewage and Industrial Wastes 486–496
Nayiga S, Willis LD, Staedke SG, Chandler CIR (2022) Reconciling imperatives: Clinical guidelines, antibiotic prescribing and the enactment of good care in lower-level health facilities in Tororo, Uganda. Global Public Health 17(2):1–12
Nishino A (2022) The great medicines migration. How China took control of key global pharmaceutical supplies. In: Nikkei Asia, 05.04.2022. https://asia.nikkei.com/static/vdata/infographics/chinavaccine-3/
Nixon R (2011) Slow Violence and the Environmentalism of the Poor. Harvard University Press, Cambridge (M.A.)
Ogyu A, Chan O, Littmann J, Pang HH, Lining X, Liu P, Matsunaga N, Ohmagari N, Fukuda K, Wernli D (2020) National action to combat AMR: a One-Health approach to assess policy priorities in action plans. BMJ Global Health 5(7):e002427
O’Neill Review (2016) Tackling Drug-Resistant Infections Globally: Final Report and Recommendations. The Review on Antimicrobial Resistance, London
Overton K, Fortané N, Broom A, Raymond S, Gradmann C, Orubu ESF, Podolsky SH, Rogers S, Katwyk V, Zaman MH, Kirchhelle C (2021) Waves of attention: patterns and themes of international antimicrobial resistance reports, 1945–2020. BMJ global health 6(11):e006909
Padilla LA (2021) Sustainable Development in the Anthropocene: Towards a New Holistic and Cosmopolitan Paradigm. Springer International Publishing, New York
Paxson H (2008) Post‐Pasteurian cultures: The microbiopolitics of raw‐milk cheese in the United States. Cult Anthropol 23(1):15–47
Peixoto RS, Voolstra CR, Sweet M, Duarte CM, Carvalho S, Villela H, Lunshof JE, Gram L, Woodhams DC, Walter J (2022) Harnessing the microbiome to prevent global biodiversity loss. Nat Microbiol 7(11):1–10
Podolsky SH (2015) The Antibiotic Era. Reform, Resistance and the Pursuit of a Rational Therapeutic. Johns Hopkins University Press, Baltimore
Podolsky S (2018) The evolving response to antibiotic resistance (1945-2018). Palgrave Commun 4
Portno AD (1968) Pasteurization and sterilization of beer—a review. Journal of the Institute of Brewing 74(3):291–300
Rajan KS (2017) Pharmocracy: Value, Politics, and Knowledge in Global Biomedicine. Duke University Press, Durham
Rasmussen N (2014) Gene Jockeys: Life Science and the Rise of Biotech Enterprise is a book by Nicolas Rasmussen. Johns Hopkins University Press, Baltimore
ReACT Group (2020) Antibiotic pollution: India scores a global first with effluent limits. ReACT News and Views. 20.04.2020, https://www.reactgroup.org/news-and-views/news-and-opinions/year-2020/antibiotic-pollution-india-scores-a-global-first-with-effluent-limits/
Redford KH (2023) Extending conservation to include Earth’s microbiome. Conserv Biol e14088
Reese AT, Dunn RR (2018) Drivers of microbiome biodiversity: a review of general rules, feces, and ignorance. MBio 9(4):e01294–18
Regnier AP, Park RWA (1972) Faecal pollution of our beaches—how serious is the situation? Nature 239(5372):408–410
Rose DB, van Dooren T, Chrulew M, Wolfe C (eds) (2017) Extinction Studies: Stories of Time, Death, and Generations. Columbia University Press, New York
Rossi F, Péguilhan R, Turgeon N, Veillette M, Baray J-L, Deguillaume L, Amato P, Duchaine C (2023) Quantification of antibiotic resistance genes (ARGs) in clouds at a mountain site (puy de Dôme, central France). Science of the Total Environment 865:161264
Roumagnac P, Weill F-X, Dolecek C, Baker S, Brisse S, Chinh NTN, Hong Le TA, Acosta CJ, Farrar J, Dougan G, Achtman M (2006) Evolutionary history of Salmonella Typhi. Science 314:1301–1304
Sariola S, Gilbert SF (2020) Toward a symbiotic perspective on public health: recognizing the ambivalence of microbes in the Anthropocene. Microorganisms 8(5):746
Sariola S, Butcher A (2022) In critique of anthropocentrism: a more-than-human ethical framework for antimicrobial resistance. Medical Humanities 48:e16
Sariola, S, Butcher A, Cañada JA, Aïkpé M, Compaore A (2022) Closing the GAP in Antimicrobial Resistance Policy in Benin and Burkina Faso. Msystems e00150-22
Schwerin AV (2010) Low Dose Intoxication and a Crisis of Regulatory Models. Chemical Mutagens in the Deutsche Forschungsgemeinschaft (DFG), 1963-1973. Ber. Wissenschaftsgeschichte 33:401–418
Sender R, Fuchs S, Milo R (2016) Revised estimates for the number of human and bacteria cells in the body. PLoS biology 14(8):e1002533
Sheinman M, Arkhipova K, Arndt PF, Dutilh BE, Hermsen R, Massip F (2021) Identical sequences found in distant genomes reveal frequent horizontal transfer across the bacterial domain. Elife 10:e62719
Silbergeld EK (2016) Chickenizing Farms & Food. How Industrial Meat Production Endangers Workers, Animals, and Consumers. Johns Hopkins University Press, Baltimore
Singer AC, Shaw H, Rhodes V, Hart A (2016) Review of antimicrobial resistance in the environment and its relevance to environmental regulators. Front Microbiol 7:1728
Smith DFQ, Casadevall A (2022) Disaster Microbiology—a New Field of Study. Mbio 13(4):e01680–22
Smith HW (1970) Incidence in river water of Escherichia coli containing R factors. Nature 228:1286–8
Smith HW (1971) Incidence of R+ Escherichia coli in coastal bathing waters of Britain. Nature 234(5325):155–156
Smith MS, Horrocks L, Harvey A, Hamilton C (2011) Rethinking adaptation for a 4° C world. Philos Trans R Soc 369:196–216
Smith-Howard K (2010) Antibiotics and Agricultural Change: Purifying Milk and Protecting Health in the Postwar Era. Agricultural History Society 84(3):327–351
Taneja N, Sharma M (2019) Antimicrobial resistance in the environment: The Indian scenario. The Indian J of Med Res 149(2):119
Tenaillon O, Jeffrey EB, Ribeck N, Deatherage DE, Blanchard JL, Dasgupta A, Wu GC, Wielgoss S, Cruveiller S, Médigue C (2016) Tempo and mode of genome evolution in a 50,000-generation experiment. Nature 536(7615):165–170
Thatcher FS, Simon W (1955) The Resistance of Staphylococci and Streptococci Isolated from Cheese to Various Antibiotics. Canadian Journal of Public health 46:407–409
Thatcher FS, Ross D (1960) Multiplication of staphylococci during cheese making: the influence of milk storage temperatures and of antibiotics. Canadian Journal of Public Health/Revue Canadienne de Santé Publique 226-234
Tompson AC, Chandler CIR (2021) Addressing antibiotic use: insights from social science around the world. Antimicrobial Resistance Centre, London School of Hygiene & Tropical Medicine, London
Tran-Dien A, Hello SL, Bouchier C, Weill F-X (2017) Early transmissible ampicillin resistance in zoonotic Salmonella enterica serotype Typhimurium in the late 1950s: a retrospective, whole-genome sequencing study. Lancet 18(2):207–214
Trembath R (1950) Effect of penicillin in milk on starter cultures. Australian Journal of Dairy Technology 5(4):143–46
Trevelline BK, Fontaine SS, Hartup BK, Kohl KD (2019) Conservation biology needs a microbial renaissance: a call for the consideration of host-associated microbiota in wildlife management practices. Proceedings of the Royal Society B 286(1895):20182448
Tsing AL (2015) The Mushroom at the End of the World: On the Possibility of Life in Capitalist Ruins. Princeton University Press, Princeton and London
UNEP (2022) Environmental Dimensions of Antimicrobial Resistance. United Nations Environment Programme, Nairobi
UNEP (2023) Bracing for Superbugs. Strengthening environmental action in the One Health response to antimicrobial resistance, United Nations Environmental Programme, Nairobi
US Senate(2010) Emergence Of The Superbug: Antimicrobial Resistance In The United States. S. Hrg, Washington, United States Senate, p 110–989
Valliere JM, Wong WS, Nevill PG, Zhong H, Dixon KW (2020) Preparing for the worst: Utilizing stress‐tolerant soil microbial communities to aid ecological restoration in the Anthropocene. Ecological Solutions and Evidence 2:e12027
Vaverkov MD, Koda E (2023) Why landfill deposits are a distinguishing feature of the Anthropocene. Anthr Rev 10(2):20530196231170370
Vogel D (2012) The Politics of Precaution. Regulating Health, Safety and Environmental Risks in Europe and the United States. Princeton University Press, Princeton and Oxford
Vogel SA (2013) Is It Safe? BPA And The Struggle To Define The Safety Of Chemicals. University of California Press, Berkeley
Levy, SB, FitzGerald GB, Macone AB (1977) Effect of an Antibiotic-Supplemented Feed on the Ecology of E. coli on a Farm. In: R-Factors: Their Properties and Possible Control. Springer, Heidelberg, p 43–60
Weary TW, Sturtevant Jr AB, Lankford J (1972) Antibiotic-Resistant Coliforms in Fresh and Salt Water. Archives of Environmental Health: An International Journal 25(3):215–220
Webster E, Mai L (2021) Transnational Environmental Law in the Anthropocene: Reflections on the Role of Law in Times of Planetary Change. Routledge, London
Weinbauer MG, Rassoulzadegan F (2007) Extinction of microbes: evidence and potential consequences. Endangered Species Research 3(2):205–215
Wellcome Trust & Boston Consulting Group (2022) Understanding the antibiotic manufacturing ecosystem. A view of global supply chains, pressure points, and implications for antimicrobial resistance response. Wellcome Trust, London
WHO (2015) Global Action Plan on Antimicrobial Resistance. World Health Organisation, Geneva
WHO (2017) Norms and standards. 70 years of WHO standards on medicines quality. WHO Drug Information 31(1):15–26
WHO One Health Global Health Leaders Group on Antimicrobial Resistance (2022) Reducing Antimicrobial Discharges from Food Systems, Manufacturing Facilities and Human Health Systems into the Environment. World Health Organisation, Geneva
Wilkinson JL, Boxall ABA, Kolpin DW, Leung KMY, Lai RWS, Galbán-Malagón C, Adell AD, Mondon J, Metian M, Marchant RA (2022) Pharmaceutical pollution of the world’s rivers. PNAS 119(8):e2113947119
Willis LD, Chandler C (2019) Quick fix for care, productivity, hygiene and inequality: reframing the entrenched problem of antibiotic overuse. BMJ Glob Health 4(4):e001590
Yim G, Wang HH, Frs JD (2007) Antibiotics as signalling molecules. Philosophical Transactions of the Royal Society B: Biological Sciences 362(1483):1195–1200
You Y, Silbergeld EK (2014) Learning from agriculture: understanding low-dose antimicrobials as drivers of resistome expansion. Front Microbiol 5:284
Yusoff K (2016) Anthropogenesis: Origins and Endings in the Anthropocene. Theory, Culture, and Society 33(2):3–28
Zeeshan Qadar SM, Thane G, Haworth-Brockman M (2021) A call to Action: An Evidence Review on Pharmaceutical Disposal in the Context of Antimicrobial Resistance in Canada. Manitoba, National Collaborating Centre for Infectious Disease, University of Manitoba
Zheng D, Yin G, Liu M, Hou L, Yang Y, Van Boeckel TP, Zheng Y, Li Y (2022) Global biogeography and projection of soil antibiotic resistance genes. Sci Adv 8(46):eabq8015
Zhou Z, Shuai X, Lin Z, Yu X, Ba X, Holmes MA, Xiao Y, Gu B, Chen H (2023) Association between particulate matter (PM) 2·5 air pollution and clinical antibiotic resistance: a global analysis. Lancet Planetary Health 7:e649–659
Zhu Y‐G, Penuelas J (2020) Changes in the environmental microbiome in the Anthropocene. Global Change Biology 26(6):3175–3177
Acknowledgements
I am grateful to Adam P. Roberts (Liverpool School of Tropical Medicine), Andrew Singer (UK Centre for Ecology and Hydrology), Clare I.R. Chandler and Rebecca Glover (London School of Hygiene and Tropical Medicine), Steve Hinchliffe (University of Exeter), Emily Webster (Durham University), and Andrea Butcher (University of Helsinki) for their thoughtful comments on different versions of this manuscript. Research on this paper was funded by a Wellcome Trust University Award (No. 218118_Z_19_Z).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The author declares no competing interests.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Informed consent
This article does not contain any studies with human participants performed by any of the authors.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kirchhelle, C. The Antibiocene – towards an eco-social analysis of humanity’s antimicrobial footprint. Humanit Soc Sci Commun 10, 619 (2023). https://doi.org/10.1057/s41599-023-02127-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1057/s41599-023-02127-6