Abstract
Efficiency within the health system is well recognised as key for achieving Universal Health Coverage (UHC). However, achieving equity and efficiency simultaneously is often seen as a conflicting effort. Using 12 years of data (2003–2014) from the selection of a number of low- and lower middle-income countries (Afghanistan, Bangladesh, Burkina Faso, Ghana, Indonesia, Mongolia, Mozambique, Tajikistan, Togo, Uzbekistan and Yemen Republic), we compute an index of Universal health coverage (UHC), measure the health system’s performance (HSp) and, finally, investigate the cross-dynamics of the resulting HSp and the UHC previously obtained. We find that, with the few exceptions over the statistical sample, the causality between performances of the national health system and the universal health coverage is typically bidirectional. From an empirical standpoint, our findings challenge the idea from economic orthodoxy that efficiency must precede equity in healthcare services. Rather, our findings support the view of simultaneous efforts to improve expansion of the coverage and efficiency of the health system, directing attention towards the importance of organisation of the health system in the country context.
Similar content being viewed by others
Introduction
Sustainable development goals (SDGs) 3 aspires to ensure healthy lives and promote wellbeing for all at all ages. SDG target 3.8 is explicit about Universal Health Coverage (UHC) and is also for realising the goals of any health system. The World Health Report (2010) acknowledges the importance of an efficient health system for achieving the UHC—an appropriate balance between extending coverage to more people, offering more services, and/or covering more of the cost of care in the country context. In this article, we attempt to find the linkage between these two public policy objectives—achieving equity and promoting efficiency—and to examine empirically the question: can equity and efficiency move together?
Promoting equity and achieving efficiency simultaneously are generally seen as conflicting, because giving access to health protection to new social groups of the population, and diverse group of sick persons, is not easy in resource-poor countries and often demands mobilising a considerable amount of resources for a not-so-visible incremental result. The problems of inefficiency in the health system are well recognised as the barrier to UHC (Hurst, 2010; Gilson et al., 2003). Several authors have argued that a fundamental reform of health systems in low -and lower middle-income countries should include improving service delivery first, at the primary care level (Hurst, 2010; WHO, 2008; Laokri et al., 2018). Among other reasons, improved efficiency is an essential source of fiscal space for the health system to perform and, therefore, is often advocated as a precondition for widening coverage (Heller, 2006; Hernandez de Cos and Moral-Benito, 2011). This is recognised as the “prudent” prescription from the viewpoint of economic orthodoxy. However, this statement, “does a health system’s performance indeed precede advancement in equitable access to healthcare?” has not yet been empirically validated in the context of any country.
In this paper, our objective is to establish the empirical relationship between the health system’s performance and progress towards the UHC for low -and lower middle-income countries. Focussing on the mortality of children (age under 5; U5) as the criterion for assessing efficiency, this study empirically examines the direction of causality between the UHC and the health system’s efficiency. We also provide an insight into the trends in the UHC and the health systems’ performance over the period of 12 years (2003–2014) in 12 economies (low -and lower middle-income) of the world.
Data and methods
We used the data from the World Bank (https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups); the World Health Organisation (http://apps.who.int/nha/database and http://apps.who.int/ghodata/) and the United Nations (http://data.un.org/). The paucity of the data availability confined this study to seven low-income countries (LICs) and five lower middle-income countries (LMICs) for 12 years (2003–2014)—Afghanistan, Bangladesh, Burkina Faso, Ghana, Indonesia, Mongolia, Mozambique, Tajikistan, Togo, Uzbekistan and Yemen Republic.
The inequality in U5 mortality is well documented in our study countries. Despite variations in U5 mortality rates between the provinces, and between wealth quintiles within the provinces, the overall patterns of U5 mortality trends show remarkable consistency: there is a clear rank order, with higher mortality in the poorest quintiles (UNFPA—Afghanistan, 2015). Similar trend is observed across the regions in Guinea, Tajikistan, Togo, Uzbekistan and Yemen Republic (Chao et al., 2018). Children from the worse-off households are having on an average 1.17 times higher mortality rate than those from the better-off households (Chowdhury et al., 2017). Coverage of immunisation, skilled birth attendants (SBAs), and post-natal visits are found to be associated with the geographical differences in U5 mortality in Burkina Faso (Millogo et al., 2019). Although the U5 mortality has decreased in all the districts, the distributional differences of U5 mortality across the districts have increased in Ghana between the period of 2000 and 2010 (Arku et al., 2016). The widened relative and absolute inequalities in U5 mortality by geography in Indonesia between 1980 and 2011 is attributed to the low density of healthcare workers with limited access to the health facilities and the healthcare services (Hodge et al., 2014). The situation is no different in Mongolia (Joshi et al., 2017). Income distribution and population density, distribution of the basic infrastructure including provision of the healthcare services, climatic and ecologic factors are suggested to have confounding effects on U5 mortality and so, the observed difference in U5 mortality across regions in Mozambique (Macassa et al., 2012).
Variables used and descriptions | |
|---|---|
Variables | Definition |
Under-five mortality rate [U5 Mortality per 1000 live births] | Probability of dying between birth and exactly 5 years of age expressed per 1000 live births. |
Total population | Total population counts all residents regardless of legal status or citizenship. The values used are midyear estimates. |
Fertility rate [total births per woman] | Total fertility rate represents the number of children that would be born to a woman if she were to live to the end of her childbearing years and bear children in accordance with age-specific fertility rates of the specified year. |
Percentage of population having access to basic drinking water services | The percentage of people using at least basic water services. This indicator encompasses both people using basic water services, as well as those using safely managed water services. Basic drinking water services is defined as drinking water from an improved source, provided collection time is not more than 30 minutes for a round trip. Improved water sources include piped water, boreholes or tube wells, protected dug wells, protected springs, and packaged or delivered water. |
Percentage of population using at least basic sanitation services | The percentage of people using at least basic sanitation services, that is, improved sanitation facilities that are not shared with other households. This indicator encompasses both people using basic sanitation services, as well as those using safely managed sanitation services. Improved sanitation facilities include flush/pour flush to piped sewer systems, septic tanks or pit latrines; ventilated improved pit latrines, compositing toilets or pit latrines with slabs. |
Percentage of population living below poverty line | National poverty headcount ratio is the percentage of the population living below the national poverty lines. National estimates are based on population-weighted subgroup estimates from household surveys. |
High-burden country | Country with T.B./HIV/Malaria. |
Density [other health workers, nurse/midwives and physician] | Number per 1000 population. |
Prenatal service coverage | Pregnant women receiving prenatal care are the percentage of women attended at least once during pregnancy by skilled health personnel for reasons related to pregnancy. |
TT coverage women | Percentage of pregnant women received Tetanus toxoid vaccines. |
Coverage BCG, DPT and Measles | Percentage of children up to 23 months received BCG, DPT, Measles (1st and 2nd dose). |
Percentage of births attended by SBAs. | The percentage of deliveries attended by personnel trained to give the necessary supervision, care, and advice to women during pregnancy, labour, and the postpartum period; to conduct deliveries on their own; and to care for new-borns. |
Pooling effect of community (public finance) on the health system. | [1 – (OOP/HCE)], OOP = out-of-pocket health expenditure and HCE = total health expenditure. |
A glance of the methods: a 3-step approach
Establishing relationship between the health system’s performance and progress towards the Universal health coverage (UHC) implies examining the direction of causality between these two measures. So, we apply a 3-step approach—Step 1 and Step 2 derive two aggregate measures of the UHC and the health system’s performance respectively. From the methodological standpoint, Step 1 calculates an index of the UHC, inspired by the “mashup” index (Wagstaff et al., 2016), to monitor UHC progress across time and space in the 3 dimensions of the UHC cube (WHO, 2010). Step 2 applies a stochastic frontier analysis (SFA) model to derive time and country-specific health system’s performance indicator (HSp). Finally, having the “efficiency (HSp)” on one side and the “UHC indicator” on the other side, step 3 investigates the cross-dynamics of the resulting HSp and the UHC for the 12 countries (a mix of LICs and LMICs), using Granger non-causality test.
Step 1. UHC progress index
SDG indicator 3.8.1 is for coverage of essential health services, defined as the average coverage of essential services based on tracer interventions that include reproductive, maternal, new-born and child health, infectious diseases and non-communicable diseases, and service capacity, and access among the general and the most disadvantaged population (UN, 2017). The core of UHC to SDG agenda and country contexts are having implications on reproductive, maternal and child health. The core defines the scope of services and population coverage, and the contexts represents the strength of the health system (Boerma et al., 2018). A single, interpretable UHC metric for coverage of essential health services will inevitably be imperfect, especially given the vast array of indicators (Fullman and Lozano, 2018). Although coverage rates of immunisation are high compared to other maternal and child health interventions, many children still die from easily preventable diseases, including pneumonia and diarrhoea (Walker et al., 2013). High rates of malnutrition underlie more than 45% of all deaths in children younger than 5 years. For those children who survive, malnutrition jeopardises their potential for optimum growth and development, with important consequences later in life (Bhutta et al., 2013; Black et al., 2013).
Computation of UHC index
Using the framework of the “mashup” index we develop an index of the UHC for U5 mortality.
UHC index focussing U5 mortality rate included
-
A.
Service coverage indicators [SC]
-
1.
Density of nurses/midwives
-
2.
Density of physician
-
3.
Density of other health workers.
-
1.
-
B.
Population coverage indicators [PC]
-
4.
Prenatal service coverage
-
5.
Tetanus Toxoid coverage
-
6.
Vaccination coverage BCG
-
7.
Vaccination coverage DPT
-
8.
Vaccination coverage Measles
-
9.
Percentage of births attended by skilled birth attendants (SBAs).
-
4.
-
C.
Indicator of Financial protection [FP]
Pooling effect of community (public finances) on the health system.
The UHC index was computed in two steps for each country i (12 countries) at year t (2003, ……, 2014). The first level calculated integrated values for SC (group A) and PC (group B) of indicators using,
where \(\left( {x_{jt}^i} \right)^\prime\) denotes standardised indicator value j = {1,2,3,4,5,6,7,8,9} for country i at time t; j represents all nine indicators used.
The second level computed index of the UHC. This index is a multidimensional weighted average of SC, PC and FP;
Equation 1. \(UHC_t^i = SC_t^i \cdot d_{SC} + PC_t^i \cdot d_{PC} + FP_t^i.d_{FP}\), where “dj” are the weights for each group of indicators. We allocated weights as 0.3, 0.3, 0.4, respectively. The higher the index score [0 < UHC < 1], the better is the coverage.
Step 2. Measuring efficiency: performance of the health systems
Considering multidimensional (levels and distribution) goals of the national health system quantifying the efficiency remains a challenge. Under-5 mortality (Table 1) is acknowledged as one of the high priority health indicators of SDGs (You et al., 2015). Focussing on U5 mortality as the outcome of interest, we identified the main inputs variables of this outcome, for examining efficiency of the health system. We applied Stochastic Frontier Analysis (SFA) model to estimate performance of the health system (Aigner et al., 1977; Greene, 2005). The SFA is often preferred over a non-parametric approach, i.e., data envelopment analysis (DEA), which is limited in the number of allowable inputs and does not separate out “noise” from the inefficiency term.
Empirical model
Equation 2. \(\ln \left( {y_{it}} \right) = \beta _i + \beta _2\ln x_{i\left( {t - 1} \right)} + \mathop {\sum}\nolimits_k {\beta _k} \ln c_{i\left( {t - 1} \right)k} + \gamma \,{{{\mathrm{ln}}}}\,z_{i\left( {t - 1} \right)} + v_{it} - u_{it}\), where yit = U5 mortality for each country at each time period;
xi(t − 1) indicates the ratio of total per capita health expenditure/total per capita GDP at t − 1;
ci(t − 1)k are vectors for each k covariate for list of the confounding factors at period of time [t − 1],
-
total population;
-
population level factor that takes into account, i.e., total fertility rate;
-
percentage of population having access to basic drinking water services;
-
percentage of population using at least basic sanitation services;
-
percentage of population living below poverty line.
zi(t − 1)j represents the vector for country’s disease burden [0 = country without any high-burden disease; 1 = country with one high-burden disease; 2 = country with combination of any two high-burden diseases; 3 = country with all high-burden diseases]. βi is the country fixed-effect that defines the country-specific intercept of the health production frontier. vit is the random error of the model, assumed to be independent and identically distributed \({{{\mathcal{N}}}}\left( {0,\sigma _v^2} \right)\). uit is the inefficiency component assumed to be non-negative, independent and identically distributed. This term follows an exponential distribution. This set of assumptions are done to obtain parameter estimates in SFA modelling.
Our model, “True fixed effects—SFA model” allowed us to disentangle time-varying inefficiency (uit) from country-specific time-invariant unobservable heterogeneity (βi). We assumed an exponential distribution for inefficiency, rather than half/truncated normal distribution, to ensure that the mean and the variance of the technical inefficiencies are strictly positive. The rationale for such an assumption is that the countries in the sample are heterogeneous, not only by their health production frontier (through the intercept βi), but also by their inefficiency (uit) and there is no reason that the distribution of these inefficiencies uit follow any (reduced or centred) normal law. The model was estimated using maximum likelihood estimator (MLE) (Aigner et al., 1977). The Wald-test and the log-likelihood ratio validate data fitness with the model used.
Step 3. Causality between the UHC and efficiency of the health system
It is assumed that performance of the health system (HSp) is having some explanatory power on the UHC and vice-versa. We applied Granger non-causality test for heterogeneous panel data model. This approach accounts both dimensions of the heterogeneity—the heterogeneity of causal relationship and the heterogeneity of data generating process (Hurlin and Venet, 2011).
For each country i ∈[1, N], two covariance stationaries denoted by x and y, observed on T periods. The variable xit is causing yit, if we are better able to predict yit using all available information, than if the information apart from xit had been used. In practice, it is not possible to use optimum predictors completely, so, we estimate the model of vector autoregression (VAR) coefficients for panel data. For each cross-section unit i and time period t, the model is
Equation 3. \(y_{it} = \mathop {\sum}\nolimits_{k - 1}^p {\beta _ky_{i,\,t - k}} + \mathop {\sum}\nolimits_{k = 0}^p {\theta _kx_{i,\,t - k} + u_{it}}\), u is normally distributed with uit = αi + εit , p is the number of lags and εit are independently, identically and normally distributed and free from heteroscedasticity and autocorrelation (0, σ2).
Assumptions are the autoregressive coefficients βk are identical for all individual countries, while, θk captures country-specific dimension. Since θk differed among countries, we tested heterogeneous non-causality hypothesis (HENC), i.e.,
We tested HENC hypothesis with the following statistics
\(F_{{\mathrm{HENC}}} = \frac{{\left( {{\mathrm{SSR}}_r - {\mathrm{SSR}}_u} \right)/p}}{{{\mathrm{SSR}}_u/\left[ {{\mathrm{NT}} - N\left( {1 \,+\, 2p} \right)\, +\, p} \right]}}\) , where SSRu denotes the sum of squared residuals for the model (Eq. 3) and SSRr, squared residuals found in Eq. 3 when the nullity of the k coefficients are imposed. If the country effects, αi, are assumed to be fixed, SSRu and SSRr are SSR obtained from the maximum likelihood (ML) estimation that corresponds to the fixed-effect estimator (FE). We estimated these two models for each of the 12 countries, Eqs. 4 and 5,
Covariance of the error terms were not correlated across the equations. We selected the number of lag using Akaike Information Criterion (AIC), Hannan–Quinn information Criterion (HQIC) and Schwarz Bayesian information Criterion (SBIC). We choose the lag that was significant for at least two of these three criteria. Adoption of such an approach for selecting lag exerted an impact with objectivity in the conclusion of the test.
Results
Table 2 presents the UHC attainment for the U5 mortality. A cluster of countries, namely, Afghanistan, Burkina Faso, Mozambique and Yemen Republic registered a substantial progress while we found setback in Guinea, Mongolia, Tajikistan, Togo and Uzbekistan over the period of 12 years. However, the coverage exhibited a fluctuating trend for all the countries during the study period (Table 2).
Table 3 presents the MLE of parameters of the stochastic frontier production function. A significant negative effect of the ratio between per capita health expenditure and total per capita GDP, and the total fertility rate emerged as the important drivers of the U5 mortality reduction.
Further, the coefficients with negative sign (the statistical significance at 10% level) of the high-burden country (combination of all three of T.B./HIV/Malaria) in SFA output captured intuitively the efforts to combat the problem not the prevalence affecting the performance of the health system.
As expected, the mean and the variance of uit are both strictly positive. This confirms, for the countries in our sample, presence of technical inefficiency, and that the differences between the observed (actual) and the frontier (potential) output were caused by a systematic decay (not the chance alone). Furthermore, the rejection of the null hypothesis (Wald-test) confirmed model appropriateness that included inefficiency term to explain the health system’s performance. The post-estimation test did not validate the normality of residual vit; this is possibly attributed to the limited number of data points in our study.
However, as the partition of the whole variability (vit + uit) between vit and uit is predetermined by the SFA modelling, the inferences on uit and the tests made on uit remain valid—which is the main purpose of the SFA application.
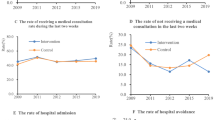
Figure 1 illustrates the trends of the health system’s performance (inefficiency) and the UHC, and cross-dynamics between the health system’s performance (i.e., HSp) and the UHC. A consistent progress of the UHC attainment was only in Afghanistan, Ghana, and Yemen Republic albeit with fluctuations. The UHC score was decreasing at a relatively fast pace between 2003 and 2005, and between 2009 and 2013 in Tajikistan, Togo and Guinea (towards the end of the study period), such observation could be attributable to the country-specific random effect, that was indeed substantial (Fig. 1).
The index of inefficiency was almost at the same level in Afghanistan, Bangladesh, Guinea, Togo and Yemen Republic during the study period. We observed a steep increase of the health system’s inefficiency for Mongolia compared to the score of the UHC (Fig. 1).
The Granger non-causality test for the heterogeneous panel data model revealed (Table 4) causality from HSp ⇒ UHC for Burkina Faso, Indonesia and Mozambique, and from UHC ⇒ HSp for Bangladesh only. The bidirectional causality HSp ⇔ UHC was found in Ghana, Mongolia, Tajikistan, Togo, Uzbekistan and Yemen Republic. Our result could not find any causality between the HSp and the UHC or vice-versa for Afghanistan and Guinea. All the causality effects were at 1% (probability of rejecting HENC hypothesis) level of statistical significance. We noted that the signs of the “betas” were not homogeneous across the countries (column 4); for instance, when a causality was for HSp ⇒ UHC (unidirectional and bidirectional), the sign was negative in four cases, and positive in five cases; when a causality was for UHC ⇒ HSp (unidirectional and bidirectional), the sign was negative in five cases, and positive in two cases.
Discussion
This study attempted to examine direction of causality between the Universal Health Coverage and the performance of the health system for U5 mortality in seven LICs and five LMICs over the period of 12 years (2003–2014). Coverage of essential health services for child health are established as one of the tracer indicators to track the UHC. Inspired from the approach of “mashup” index, we first developed the UHC index for U5 mortality in the framework of the UHC cube (where we have allocated weights as 30% for each of the service coverage and the population coverage, and 40% weight for the financial protection). We applied a 3-step approach—first, we derived the UHC index for seven LICs and five LMICs showing levels of the UHC attainment, and changes and trends therein. Second, using SFA methods, we generated scores of efficiencies for the 12 countries under this study and obtained the result of extent of inefficiency in the performance of the national health system. Finally, we applied Granger non-causality test to a heterogeneous panel data model with fixed coefficients to ascertain the direction of causality between the UHC and the HSp.
A bidirectional causality HSp ⇔ UHC was found for six of the twelve countries in our sample, but with the mix of a negative sign (3 countries), and a positive sign (3 countries). Togo and Yemen reflected that the efficiency and the equity can evolve simultaneously, rather than in any opposite direction. The conventional view that efficiency and equity contradict each other were found to be true in three cases: Ghana, Tajikistan and Uzbekistan. “Inefficiency” also affects the coverage without any discrimination or selectivity. In Mongolia, although increased efficiency of the health system was associated with the improved UHC, the reverse was not true, i.e., an improved UHC was not associated with a better performing national health system. The scenario that the efficiency indeed precedes the equity was found only in two countries (unidirectional, HSp ⇒ UHC), i.e., in Burkina Faso and Indonesia). Lastly, the negative unidirectional causality relationship for Bangladesh (UHC ⇒ HSp), implied that the equity efforts were not without the expense of the efficiency (WHO, 2000).
Such a mixed findings implied that the context matters to conclude the existence of a “rivalry effect” between equity and efficiency. The findings from Togo and Yemen established the importance of examining combined effects of interactions between and within determinants to achieve health policy goals. From an empirical standpoint, the statistical findings critically challenged the idea, driven by the economic orthodoxy, that efficiency must precede equity in healthcare services. Rather, our findings mostly supported the view of simultaneous efforts for improvement in the expansion of coverage and the health system’s efficiency, directing attention towards the importance of organisation of the health system in the country context. Quantifying multidimensional goals of the national health system is always a challenge and so, this study has demonstrated an approach to overcome such a challenge using an illustration with U5 mortality.
We have presented a framework to examine and monitor cross-dynamicity of the health system’s performance and the universal health coverage, and thereby, this study objectively contributes to the debates and the contestation in decision making for public health development. With this effort to have plausible results, this study was limited to the countries where data availability source was common both over time within a country and across countries; this led us to restrict the sample to only 12 countries over 12 years. This short time-horizon was probably the most thwarting limitation in this study, with possible consequences for the confirmation of few technical assumptions (but not for the validation of the model used). Further, the paucity of the consistency in the data availability across the countries did not allow post-natal care coverage to be included in the population coverage of the UHC cube. In addition, the almost similar economic, social and other macro context of the countries studied restricted the generalisability of the findings, although ensured a reasonable comparability.
Despite these limitations, this study has used advanced methodological approaches on the data from multilateral organisations and presents a novel insight for understanding contributions of universal health coverage on under-5 mortality level attainment. In addition, this study has captured the role of determinants for the health systems to be efficient. Our methodological approach for measuring “inefficiency” has picked up all time-invariant effects (e.g., effect of investment in the health system as a ratio between per capita health expenditure and per capita GDP, and fertility rates), as well as possible inter-country unobserved heterogeneity, and thus, the “inefficiency” was estimated as an unstructured time-varying effect.
Conclusions
Besides other mechanisms, the policy coherence for SDGs calls for an adoption of an integrated approach interlinking different sectors. This study demonstrates the relevance of our approach for U5 mortality in the context of the “agenda 2030”. To conclude, this study presents the need for SDGs target-specific data generation and more specifically, examining interlinkages and interactions between and within the SDG targets for estimating the combined efficiency/equity effects of interventions in the context of resource-poor countries with consideration of the effect of organisation of the respective health system. Our data can also be used as a starting point to develop an information system for tracking the effect of cross-dynamicity between the health system’s performance and the Universal Health Coverage on U5 mortality.
Data availability
Data used in this study are taken from the World Bank (https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups); and the World Health Organisation (http://apps.who.int/nha/database and http://apps.who.int/ghodata/); and United Nations (http://data.un.org/).
References
Aigner D, Lovell C, Schmidt P (1977) Formulation and estimation of stochastic frontier production function models. J Econome 6:21–37
Arku RE, Bennett JE, Castro MC, Agyeman-Duah K, Mintah SE et al. (2016) Geographical inequalities and social and environmental risk factors for under-five mortality in Ghana in 2000 and 2010: Bayesian spatial analysis of census data. PLOS Med 13(6):e1002038
Bhutta ZA, Das JK, Rizvi A, and the Lancet Nutrition Interventions Review Group, and the Maternal and Child Nutrition Study Group et al. (2013) Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost? Lancet 382:452–477
Black RE, Victora CG, Walker SP, the Maternal and Child Nutrition Study Group et al.(2013) Maternal and child undernutrition and overweight in low-income and middle-income countries Lancet 382:427–451
Boerma T, Requejo J, Victora CG, Amouzou A, George A, and the Countdown to 2030 Collaboration group et al. (2018) Countdown to 2030: tracking progress towards universal coverage for reproductive, maternal, newborn, and child health Lancet, 391:1538–1548
Chao F, You D, Pedersen J et al. (2018) National and regional under-5 mortality rate by economic status for low-income and middle-income countries: a systematic assessment. Lancet Glob Health 6:e535–547
Chowdhury AH, Hanifi SMA, Mia MN, Bhuiya A (2017) Socioeconomic inequalities in under-five mortality in rural Bangladesh: evidence from seven national surveys spreading over 20 years. Int J Equit Health 16:197
Fullman N, Lozano R (2018) Towards a meaningful measure of universal health coverage for the next billion. Lancet 6:e122–e123
Gilson L, Doherty J, Lake S, McIntyre D, Mwikisa C et al. (2003) The SAZA study: implementing health financing reform in South Africa and Zambia. Health Policy Plan 18:31–46
Greene W (2005) Fixed and random effects in stochastic frontier models. J Prod Anal 23:7–32
Heller PS (2006) The prospects of creating ‘fiscal space’ for the health sector. Health Policy Plan 21:75–79
Hernandez de Cos P, Moral-Benito E (2011) Health expenditure in the OECD countries: efficiency and regulation. Bank of Spain Occasional Documents No. 1107:2011
Hodge A, Firth S, Marthias T, Jimenez-Soto E (2014) Location matters: trends in inequalities in child mortality in Indonesia. Evidence from repeated cross-sectional surveys. PLoS ONE 9(7):e103597
Hurlin C, Venet B (2011) Granger causality tests in panel data models with fixed coefficients. mime’o. University Paris IX
Hurst J (2010) Effective ways to realise policy reforms in health systems. OECD Health Working Papers. Organisation for Economic Cooperation and Development, Paris
Joshi N, Bolorhon B, Narula I et al. (2017) Social and environmental determinants of child health in Mongolia across years of rapid economic growth: 2000-2010. Int J Equit Health 16:189
Laokri S, Soelaeman R, Hotchkiss DR (2018) Assessing out-of-pocket expenditures for primary health care: how responsive is the Democratic Republic of Congo health system to providing financial risk protection? BMC Health Serv Res 18:451
Macassa G, Ghilagaber G, Charsmar H, Walander A, Sundin Ö, Soares J (2012) Geographic differentials in mortality of children in Mozambique: their implications for achievement of Millennium Development Goal 4. J Health Popul Nutr 30(3):331–345
Millogo O, Doamba JEO, Sié A, Utzinger J, Vounatsou P (2019) Geographical variation in the association of child, maternal and household health interventions with under-five mortality in Burkina Faso. PLoS ONE 14(7):e0218163
UNFPA–Afghanistan (2015) Socio-Demographic and Economic Survey–Child Mortality. UNFPA–Afghanistan
Wagstaff A, Cotlear D, Eozenou PH, Buisman LR (2016) Measuring progress towards universal health coverage: with an application to 24 developing countries. Oxf Rev Econ Policy 32(1):147–189
Walker CL, Rudan I, Liu L et al. (2013) Global burden of childhood pneumonia and diarrhoea. Lancet 81:1405–1416
WHO (2008) The World health report: primary health care, now more than ever. World Health Organization, Geneva
World Health Organization (2000) World Health Report 2000-Health systems: improving performance. World Health Organization, Geneva, p 56
World Health Organization (2010) Health systems financing-the path to universal coverage. World Health Organization, Geneva [Available: http://www.who.int/whr/2010/en/index.html. Accessed 7 Jul 2019]
You D, Hug L, Ejdemyr S et al. (2015) Global, regional, and national levels and trends in under‐5 mortality between 1990 and 2015, with scenario‐based projections to 2030: a systematic analysis by the UN Inter‐agency Group for Child Mortality Estimation. Lancet 386:2275–2286
Acknowledgements
The Article Processing Charge of Springer Nature Group is paid from the “France 2030” investment plan managed by the French National Research Agency (reference: ANR-17-EURE-0020) and from Excellence Initiative of Aix-Marseille Université - A*MIDEX.
Author information
Authors and Affiliations
Contributions
PP: concept development; literature review; study design; data acquisition and organisation; data analysis; interpretation of results from the analysis and writing the manuscript. UN: software syntax development. AN: contributed for choosing the right econometric model for examining health systems’ performance. NK: construction of mathematical expressions and validation of the models used. BV: conceptualisation of the study; development of the analytical approach; providing critical comments; revising with important intellectual contents and final reviewing of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Not applicable. This article does not contain any studies with human participants performed by any of the authors.
Informed consent
Not applicable. This article does not contain any studies with human participants performed by any of the authors. This study uses administrative data with no individual identification identifiable by the user.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Paul, P., Nguemdjo, U., Ngami, A. et al. Do efficiency and equity move together? Cross-dynamics of Health System performance and Universal Health Coverage. Humanit Soc Sci Commun 9, 293 (2022). https://doi.org/10.1057/s41599-022-01271-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1057/s41599-022-01271-9