Abstract
Japan is facing a markedly high incidence of adolescent suicide. This study examines the relationship between depression and self-rated health, which is a significant factor driving people towards suicide, highlighting the importance of children’s assessments of their health. In this cross-sectional study, an original questionnaire combining text and illustrations was administered to 6421 elementary, junior, and senior high-school students and an effective way of using the questionnaire was proposed. To assess children’s self-rated health, the survey questions were classified into two domains: physical and mental health. The questions were further classified based on symptom duration. Depression assessment was based on the Depression Self-Rating Scale for Children. To provide a basis for the effective use of the self-rated health assessment tool, the respondents were classified into three groups based on physical/mental conditions together with the duration of those conditions, and comparisons were subsequently made. The groups were Favourable Health, Temporarily Poor Health, and Persistently Poor Health, and the results were analysed using an ANOVA. Self-rated health levels decreased, and depressive conditions worsened with age. Although most children led physically and mentally healthy school lives, the mean Depression Self-Rating Scale score was significantly higher for the Persistently Poor Health group than the other two, and the Temporarily Poor Health group scored significantly higher than the Favourable Health group for both physical and mental health (all p < 0.001). As the Temporarily and Persistently Poor Health groups in the domains of physical and mental health are more likely to be depressed, it is important to monitor the health of children in educational settings. In this study, completing this questionnaire was shown to help children understand themselves objectively and help the adults around them comprehend their condition quicker. It is especially important to promptly develop systems for appropriate and organic collaboration between educational settings and medical or welfare services.
Similar content being viewed by others
Introduction
Japan is experiencing increasingly high rates of suicide among young people. It is the only developed country where suicide is the leading cause of death among those aged 15−39, with a particularly high incidence of adolescent suicide. It is also the only country in the industrialised world (G7) where suicide is the leading cause of death among young people (those in their teens and twenties). The mortality rate for teenagers is higher in the USA and Canada than in Japan (Ministry of Health, Labour and Welfare, 2021). Data clarifying the causes of suicide are often unavailable for the 10−14 age group, but depression is frequently reported to be a major contributing factor among senior high-school students. Specifically, the incidence of suicide associated with depression or other mental health disorders is high among female senior high-school students (Ministry of Health, Labour and Welfare, 2020). In Japan, the Minister of Health, Labour and Welfare has designated ‘Suicide Prevention Week’ and ‘Suicide Prevention Month’, and has issued messages, distributed counselling service PR videos and posters, and trained ‘gatekeepers’—people who are able to recognise, talk to, listen to, connect with, and look after those in distress. However, discussions on how to prevent adolescent suicide remains insufficient (Ministry of Education, Culture, Sports, Science and Technology, 2021).
Self-rated health is an index to subjectively assess one’s health condition; it aids in clarifying overall health conditions that are difficult to identify with objective parameters, such as death and prevalence rates. In Europe and the United States, this is known as ‘subjective health’ or ‘self-reported health’. Self-rated health was incorporated into the National Health Interview Survey in the United States in 1972. In Japan, it was first used in the Comprehensive Survey of Living Conditions in 1986 and has since been examined in many social surveys (Hoshi, 1988). Self-rated health is often examined in combination with lifestyle, quality of life, and physical symptoms. Many studies involving older adults report higher survival rates for individuals with higher self-rated health levels, revealing their influence on vital prognoses. The relative risk of all-cause mortality is higher in women than in men when subjective health status is ‘poor’ compared with ‘excellent’ (Kaplan and Camacho, 1983). In addition, the Buzzard model results, which analysed the causal relationship between subjective health and life expectancy, showed that the risk of death was higher and the survival curve lower in both men and women who reported themselves as being ‘unhealthy’ compared to those who reported as ‘very healthy’, ‘fairly healthy’, or ‘not very healthy’ (Okado et al., 2000). Self-rated health, used for autonomous health assessments and to accurately represent lifestyles and related physical health conditions, is an excellent assessment and support tool that may facilitate bidirectional health support (Yamamoto et al., 2009). Additionally, when an objective health assessment is difficult, especially since it is time and cost intensive, subjective health perception is a useful alternative health indicator because it is a simple test with advantages such as being an easy-to-use single-item index (Sugisawa and Sugisawa, 1995). However, existing studies have only investigated adults. A pilot survey involving elementary and junior high-school students and teachers is the only reported study on self-rated child health (Okada et al., 2016).
A previous study examining the risk of suicide among young people based on suicidal behaviour and protective factors revealed that mental health disorders increased suicide risk, as they were present in many adolescents who committed or attempted suicide (Bridge et al., 2006). In a Japanese survey involving those aged 13–18 with a history of suicide attempts, health problems, mainly those due to mental health disorders, were the leading contributing factors of these attempts (Narishige et al., 2012). According to a study investigating cases of suicide among those under 15 over the past decade in New Zealand, suicide risk increased with age, and mental health problems were noted in many cases (Beautrais, 2001). Depression was reported to be the psychiatric risk factor most significantly correlated with adolescent suicide (Brent et al., 1993; Shafii et al., 1988). In a Finnish study comparing males and females who died by suicide between the ages of 13 and 22, mood disorders were present in 68% of females (Marttunen et al., 1995). In another study conducted in Finland, mental health disorders were present in 94% of all suicide cases among those aged 13−19, and there was a strong correlation between adolescent suicide and depression (Marttunen et al., 1991). In a survey investigating suicide among individuals under 20 in New York City, the presence of substance-related disorders, represented by alcoholism, and concomitant mood disorder, which was the main risk factor in both sexes, also increased the risk of suicide (Shaffer et al., 1996). Harrington’s (1994) epidemiological study reported that depressive states lead to depression in children and that the prevalence of these states rapidly and markedly increases during adolescence. Murata et al. (1996) noted that depressive states among students were closely associated with problems related to the education system or school structure. Students in depressive states often go through a process where their self-expectations and ideals are unmet and their self-worth gradually decreases (Murata et al., 1996; Okada et al., 2009). Based on this process, depressive states may be a strong trigger for suicide attempts.
According to a report from Norway, compared with late adolescents (aged ≥ 15 years), fewer early teenagers expressed suicidal intentions, left suicide notes or attempted suicide, and described events that were predictive or precursory to suicide; however, they mentioned the need for caution when depression or other risk factors were detected (Grøholt et al., 1998). Similarly, in Japan, data that would facilitate the identification of causes or motives are unavailable in many cases of suicide among those aged 10−14 (Ministry of Health, Labour and Welfare, 2020). Therefore, it is necessary to identify protective factors for suicidal behaviour at an early stage and screen for an increased risk of suicide in children, as one study analysing risk factors associated with suicide in young people over the past decade concluded that these factors are often mainly explained by psychiatric problems in adolescents (Gould et al., 2003). In addition to such screening, curricula (Gould and Kramer, 2001) and acknowledge-care-tell approaches to detect such risks were reported to be important for suicide prevention (Jacobs et al., 2009). In Japan, in accordance with the Ministry of Education, Culture, Sports, Science and Technology’s (2015) initiative, which highlights the need to review the leadership of managers, the ideal way of conducting school affairs, and the way faculty and staff work so that faculty members and staff with diverse expertise can collaborate as a team by making use of their respective expertise, some schools are trying to connect students in need of assistance to medical care after a comprehensive physical and mental health examination by the school nurse. However, this is a difficult, labour- and time-intensive process. Therefore, we believe that the key to child suicide prevention lies in the school, where the child spends most of the day. If schools have access to tools that are interesting and easily administered to younger children, and that can be used to easily assess children’s status and identify some of the depression symptoms associated with childhood suicide, then schools can independently identify risk factors in students and seek medical care confidently and reliably when depression is suspected. This could go a long way in helping many children.
Based on these perspectives, for the prevention of suicide among young people, this study aims to: (1) analyse children’s self-rated health status; (2) analyse the relationship between self-rated health and depression, which can lead to suicide (this is because if the results of children’s self-assessments can be used to identify depression to some extent, then schools may find it easier to identify childhood depression through easy-to-answer self-assessment questions); and (3) based on (2), propose the use of a self-assessment-based health measurement tool that is effective for the early prevention of childhood suicide.
Methods
Participants
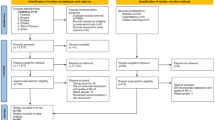
We selected schools located in seven cities in A, B, and C prefectures in Japan, each with a population of 30,000. We believe these were the most representative schools in Japan with regard to school courses, scale, student sex ratio, and academic ability. A questionnaire survey was distributed to 6421 (3262 male, 3159 female) students aged 7–18, of whom, 1962 (1031 male, 931 female) were aged 7–12 from four elementary schools, 2097 (1079 male, 1018 female) were aged 13–15 from five junior high schools, and 2362 (1152 male, 1210 female) were aged 16–18 from four senior high schools. Subsequently, responses from 5641 students (2824 male, 2817 female), of whom 1592 (830 male, 762 female) belonged to elementary schools, 1875 (958 male, 917 female) to junior high schools, and 2174 (1036 male, 1138 female) to senior high schools, who were present on the day of the survey and agreed to complete the entire questionnaire correctly, were analysed (valid response rate: 87.9%). Those (19 primary school students, 28 junior high-school students, 20 senior high-school students, 67 students in total, 1.0%) who expressed ‘disagreement’ with the questionnaire survey were excluded from the analysis.
Study period and procedure
A period between late November 2018 and early June 2019, when neither in-school events nor regular tests took place, was chosen for each school. The survey was conducted during a short morning homeroom session or at lunchtime by homeroom teachers and their assistants on a school-wide basis.
Study items
To assess self-rated health, the Comprehensive Survey of Living Conditions presents the following question: ‘What is your current health condition? Please mark the most appropriate number with a circle’, with response options of ‘1: Good’, ‘2: Relatively good’, ‘3: Normal’, ‘4: Relatively bad’, and ‘5: Bad’. Answers were quantified by scoring ‘Good’ as 5 and ‘Bad’ as 1. However, solely textual response options may not be easy for children, especially elementary school students, to understand. Therefore, upon deliberation, we created original questions by combining words and illustrations that utilised the concept of weather to facilitate understanding (Figs. 1 and 2).
Original questions were created by combining words and illustrations that utilised the concept of weather conditions a metaphor for physical health status: ‘Beautiful Sunny’ is ‘Good’, ‘Sunny’ is ‘Relatively good’, ‘Cloudy occasionally sunny’ is ‘Normal’, ‘rainy’ is ‘Relatively bad’, and ‘Stormy’ is’ ‘Bad’.
Original questions were created by combining words and illustrations that utilised the concept of weather conditions as a metaphor for in mental health status: ‘Beautiful Sunny’ is ‘Good’, ‘Sunny’ is ‘Relatively good’, ‘Cloudy occasionally sunny’ is ‘Normal’, ‘rainy’ is ‘Relatively bad’, and ‘Stormy’ is’ ‘Bad’.
Additionally, considering the necessity of asking about physical health symptoms such as recurring headaches, abdominal pain, and vomiting (Murberg and Bru, 2004; Takamiya et al., 2015; Tanaka et al., 2000; Tanaka et al., 2012), along with mental health symptoms, we classified these questions into two domains and presented them separately, as follows: ‘If your body were the weather, how would it feel?’ and ‘If your heart were the weather, how would it feel?’ (self-rated health assessment tool). We further classified the questions according to the duration of each symptom—‘not persisting for 2 weeks’ and ‘persisting for 2 weeks or longer’—based on the Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition depression criteria (American Psychiatric Association, 2013), where five or more symptoms, including depressive mood or loss of interest or pleasure, persisting for 2 weeks or longer, are required for diagnosis. Furthermore, in the domain of self-rated physical health, we asked the children to describe the body part responsible for and the reason for their condition. In the domain of self-rated mental health, we asked them to identify the cause by circling ‘school’, ‘home’, or ‘other’ and to describe the reason for the marked cause.
Depression assessment was based on Murata et al.’s (1996) Japanese version of the Depression Self-Rating Scale for Children (DSRS-C), originally developed by Birleson (1981). The 18 statements, designed to examine students’ tendencies related to spiritlessness and depression over the past week, were rated on a three-point scale: ‘Most of the time’ (2), ‘Sometimes’ (1), and ‘Never’ (0). The full score is 36, and the cutoff score is 16. Higher scores indicate more markedly depressive states. Firth and Chaplin (1987) demonstrated that the DSRS-C is useful for screening for depressive states. As there are only 18 statements, the scale does not take much time to complete; therefore, there is not much of a burden on elementary and junior/senior high-school students. Statements are easy to understand, with soft expressions to avoid causing mental conflict in participating children.
Ethical considerations
We visited each of the 13 schools and explained the study objective, methods, and privacy protection measures to the students after obtaining consent from their respective principals. Subsequently, we asked the school principals to provide parents with this explanation and seek their approval. For participants under the age of 16 years, each class teacher explained the questionnaires to their parents or guardians, and verbal consent was obtained from them. These participants were asked to choose their own answers to questions at the top of the questionnaire, i.e., whether they would or would not answer the questions in this questionnaire, including the intention of their parents or guardians. To obtain students’ consent before initiating the study, we also asked the homeroom teachers and assistants in charge of distributing the questionnaire to orally explain certain measures to these participants. Students were informed that they would not be at any disadvantage for refusing to participate or being unable to complete the questionnaire. The questionnaire did not have any field for collecting the students’ names. However, consent was required for all individual students to participate. ‘I agree’ and ‘I do not agree’ were listed as options at the top of all questionnaires distributed to students. Since the questionnaires were to be collected by the homeroom teacher on a class-by-class basis, we considered and ensured equality in the collection of the questionnaires so that students who declined participation and did not submit the questionnaires would not be disadvantaged by the attention of other students. Therefore, students who chose ‘I do not agree’ did not complete the questionnaire. We only received answers from students who chose ‘I agree’.
It was clarified that all information would be anonymised to prevent the identification of individuals; there would be no pressure on students, teachers, assistant teachers-in-charge, or others when filling out the questionnaire; students did not need to fill out the questionnaire in front of the teachers; and the statistical processing of all survey results and their use was for this study only. Submitting a questionnaire was regarded as consent from a child. The study was approved by the Medical Ethics Committee of our institution (FY 2018, approval number: 2). All procedures were carried out in accordance with the standards of the institutional ethics committee, the 1964 Helsinki Declaration and its later amendments.
Analysis
To clarify overall associations related to self-rated health and mean DSRS-C score, we first performed an ANOVA based on sex and school type using Tukey’s Honestly Significant Difference (HSD) test for multiple comparisons. The significance threshold was set at p < 0.05. We then analysed the differences between boys and girls using the t-test. All data were presented as mean ± SD. To examine the relationship between self-rated health and depressive states, we calculated Pearson correlation coefficients adjusted for school type and sex with significance thresholds of p < 0.05.
Next, for the questionnaire, we regarded ‘Normal’ as a positive answer, thus dividing all answers into two choices: ‘Good/Relatively good/Normal’ and ‘Relatively bad/Bad’ (Baba and Kondo, 2005). We then divided the children’s ratings of their physical health condition as ‘Relatively bad/Bad’ into two groups based on duration (‘not persisting for 2 weeks’ and ‘persisting for 2 weeks or longer’) and performed ANOVA. We similarly analysed data for the domain of self-rated mental health. Following from this result, we compared the three groups of children based on their physical/mental conditions together with the duration of those conditions. The classifications were as follows: Favourable Health: rating their physical/mental health condition as ‘Good/Relatively good/Normal’; Temporarily Poor Health: ‘Relatively bad/Bad’ + ‘not persisting for 2 weeks’; and Persistently Poor Health: ‘Relatively bad/Bad’ + ‘persisting for 2 weeks or longer.’ We used a chi-squared test for comparison of percentages in sex- and school-type-based analysis of self-reported physical and mental health of students. This provided a basis for the effective use of the self-rating assessment tool. Finally, we compared the prevalence of depression among the three groups. In the domain of self-rated physical health, using the mean DSRS-C score for each group, we performed a one-way ANOVA based on students’ sex and school type, using Tukey’s HSD, with significance threshold set at p < 0.05. All the data is presented as mean ± SD. We used a two-tailed Chi-square test to compare the proportions of them. We performed the analyses using SPSS ver. 26 (IBM Japan, Ltd.).
Results
Children’s self-rated health
The results of the sex- and school-type-based analysis of the self-rated physical and mental health of elementary, junior high, and senior high-school students are shown in Tables 1 and 2.
The overall mean ± standard deviation score for self-rated physical health was 3.60 ± 1.06, and males had scored significantly higher than females (t(5639) = 3.733, p < 0.001, r = 0.050). Sex-based differences were not observed for any school type. Elementary school students had significantly higher scores than junior and senior high-school students, and scores of junior high-school students were significantly higher than those of senior high-school students (F(5,5635) = 56.309, p < 0.001, η2 = 0.048). Similarly, the overall mean ± standard deviation score for self-rated mental health was 3.65 ± 1.11, and males had significantly higher scores than females (t(5639) = 5.263, p < 0.001, r = 0.070). As for gender-based differences at each type of school, males had significantly higher scores than females at junior high schools. Elementary school students had significantly higher scores than junior and senior high-school students, and the scores of junior high-school students were significantly higher than those of senior high-school students (F(5,5635) = 74.232, p < 0.001, η2 = 0.062).
Depression
The total DSRS-C scores, representing depression, and the results of the sex- and school-type-based analysis of responses to the DSRS-C are shown in Table 3.
The overall mean ± standard deviation DSRS-C score was 11.82 ± 6.24, and females had significantly higher scores than males (t(5639) = −5.279, p < 0.001, r = 0.070). As for gender-based differences for each type of school, females had significantly higher scores than males in junior high schools. Senior high-school students had significantly higher scores than elementary and junior high-school students (F(5, 5635) = 34.778, p < 0.001, η2 = 0.030).
Relationship between self-rated health and depression
Children’s depressive states may vary depending on their self-rated health levels. Therefore, to examine the relationships of self-rated physical and mental health scores with total DSRS-C score, we calculated Pearson’s and partial correlation coefficients (Table 4). The correlation coefficients in all cases were significant, ranging from 0.40 to 0.60.
Effective use of the tool and the relationship between self-rated health and depression risk
To provide a basis for the effective use of the self-rated health assessment tool, we compared the three groups of children based on their physical/mental conditions together with the duration of those conditions (Favourable Health: rating their physical/mental health condition as ‘Good/Relatively good/Normal’; Temporarily Poor Health: ‘Relatively bad/Bad’ + ‘not persisting for 2 weeks’; and Persistently Poor Health: ‘Relatively bad/Bad’ + ‘persisting for 2 weeks or longer’).
In the domain of self-rated physical health, 85.3% of all children belonged to the Favourable Health group, whereas those belonging to the Temporarily and Persistently Poor Health groups accounted for 8.1% and 6.6%, respectively. There were significant differences related to school type (χ2(4) = 37.546, p < 0.001, Cramer’s V = 0.058), but no sex-based differences were observed (χ2(2) = 0.387, p = 0.824, Cramer’s V = 0.008). In the domain of self-rated mental health, 85.7% of all children belonged to the Favourable Health group, whereas those belonging to the Temporarily and Persistently Poor Health groups accounted for 5.4 and 8.9%, respectively. There were significant differences related to both sex (χ2(2) = 13.014, p = 0.001, Cramer’s V = 0.048) and school type (χ2(4) = 46.962, p < 0.001, Cramer’s V = 0.065) (Table 5).
Next, we compared the prevalence of depression among the three groups. In the domain of self-rated physical health, the mean DSRS-C score for each group was as follows: Favourable Health: 11.11 ± 5.92, Temporarily Poor Health: 14.71 ± 6.12, and Persistently Poor Health: 17.36 ± 6.68. The Persistently Poor Health group had significantly higher DSRS-C scores than the Temporarily Poor and Favourable Health groups, while the scores for the Temporarily Poor Health group were significantly higher than those for the Favourable Health group (F(2,5638) = 247.222, p < 0.001, η2 = 0.081). Similarly, in the domain of self-rated mental health, the mean DSRS-C score for each group was as follows: Favourable Health: 10.77 ± 5.61, Temporarily Poor Health: 16.50 ± 5.81, and Persistently Poor Health: 19.09 ± 6.12. The Persistently Poor Health group had significantly higher scores than the Temporarily Poor and Favourable Health groups, while the scores for the Temporarily Poor Health group were significantly higher than those for the Favourable Health group. As for the DSRS-C cutoff (16), the Persistently Poor Health group had higher self-rated physical health scores, and the Temporarily Poor Health and Persistently Poor Health groups had higher self-rated mental health scores (F(2,5638) = 598.277, p < 0.001, η2 = 0.175) (Tables 6 and 7).
When asked about their physical health conditions, many children in the Persistently Poor Health group answered that the body part responsible was their ‘head’ (17.7%), ‘abdomen, stomach, intestines’ (11.8%), or ‘low back, shoulder, neck, whole body’ (25.1%). Common reasons included: ‘I have abdominal pain’, ‘I have a headache’, ‘I can’t sleep’, ‘I have a stiff neck and shoulders’, ‘I often vomit’, and ‘I get tired easily’. The leading cause of poor mental health in this group was ‘school’ (58.9%), followed by ‘home’ (15.8%), and ‘other’ (including N/A) (25.3%). The most common reasons included: ‘I feel tired’, ‘I feel gloomy’, ‘There are many things to worry about’, ‘I care about what other people think’, ‘Stress’, ‘Anxiety’, ‘No fun at all’, ‘Bullying’, and ‘I don’t understand what I study’. ‘School’ (59.8%) was the leading cause in the Temporarily Poor Health group as well, followed by ‘home’ (10.8%), and ‘other’ (including N/A) (29.5%). There were no significant differences between these groups (χ2(2) = 4.984, p = 0.083, Cramer’s V = 0.079) (Table 8).
Discussion
Relationship between children’s self-rated physical/mental health and depression
In this study, we used an original self-rated health assessment tool for children. In both domains, males’ scores were higher than females’, and self-rated health levels decreased with age. Depressive states were more prevalent among females than males, and this worsened with age.
Comparisons between the three groups of children—the Favourable, Temporarily Poor, and Persistently Poor Health groups—revealed that the majority of elementary, junior high, and senior high-school students lead a physically and mentally healthy school life, as more than 85% of all children belonged to the Favourable Health group. However, ~15% belonged to the Temporarily or Persistently Poor Health groups, which included those with suspected depression. Thus, some children may have been experiencing poor mental and physical health.
In the domain of self-rated physical health, children belonging to the Persistently Poor Health group had DSRS-C scores higher than 16, which is the DSRS-C cutoff, and the ‘head’ and ‘abdomen, stomach, intestines’ were the most common body parts responsible for their poor physical health conditions. Their poor mental health may have been caused by poor physical health; however, the reverse may also be possible. Furthermore, 60% of them selected ‘school’ as the cause of their poor mental health conditions, suggesting a significant correlation between their psychophysiological symptoms and difficult relationships with school friends, worries about academic achievement, study pressure, and conflicts with parents and teachers (Murberg and Bru, 2004). The presence of chronic headaches may also suggest a typical psychophysiological disorder strongly correlated with school dislike (Tanaka et al., 2012). In the domain of self-rated mental health, it should be noted that not only the Persistently Poor Health group but also the Temporarily Poor Health group had scores higher than the DSRS-C cutoff of 16. Specifically, the mean DSRS-C score in the Persistently Poor Health group was 19, significantly exceeding the cutoff value and indicating the necessity of early intervention. Furthermore, as more than half of the children selected ‘school’ as the cause of their poor condition, the possibility of schools, where children spend most of their time, causing psychophysiological and depressive symptoms owing to difficulties related to studies, conflict in interpersonal relationships, and poor adaptation to school culture, is undeniable.
Younger children are particularly subject to physical deconditioning. In this study, the reasons for poor physical health conditions such as ‘I can’t sleep’ and ‘I get tired easily’ suggest sleeplessness and fatigue. Sleeplessness may indicate depression symptoms and pain such as headaches and stomach aches, whereas general malaise suggests the presence of psychophysiological disorders (Takamiya et al., 2015). These conditions are difficult to screen for only through self-rated mental health assessments. Therefore, when assessing children, it may be necessary to address both physical and mental health.
Effective use of the self-rated health assessment tool
When using the self-rated health assessment tool, it may be effective to focus on the Persistently Poor Health group in the domain of physical health and both the Temporarily and Persistently Poor Health groups in the domain of mental health and provide early intervention to prevent suicide. In Japan, without such screening at school, children’s physical complaints are frequently overlooked. In a survey on the mental health conditions of elementary and junior high-school students, a gap was found between the results of the assessment by homeroom teachers and children’s actual mental conditions (Okada et al., 2016). Considering that children spend a large amount of time at school, schoolteachers, as the adults closest to them, should regularly conduct screening tests and make commitments to children based on their results. However, in this case, there is a concern that children will respond according to how they think adults want them to answer, i.e., children will answer considering the teacher’s wishes and expectations. Therefore, there is a risk of obtaining an inaccurate picture of the children’s situations if their answers depend on their relationship with their teacher. Thus, this tool should be administered by someone other than the teacher, such as a school nurse or a school counsellor, who is not involved in the assessment of the children. For individual use, it may be useful for the school nurse to administer this tool to the children as and when visiting the health centre, to observe the child using the sheet and actually listen to the child. Through this tool, children may have the opportunity to talk to a trusted adult and their voices may provide us with the possibility of identifying and responding to risk factors that lead to suicide, of which the children themselves are not aware.
In addition, the tool helps children to objectively understand themselves. With a growing number of people showing signs of depression, there are currently global concerns over increased suicide risk. In such a situation, the tool may be useful not only for teachers and other people around children to recognise their physical and mental conditions, but also for children to understand themselves. Conceptualisation of their body/heart as the weather may help them develop objective insight into their physical and mental conditions. The children can then analyse their own situation based on the weather they have chosen and the reason they have provided and may be able to find a solution for themselves. For example, if a child chooses the ‘rainy’ weather, considering it ‘Relatively bad’, and the reason they provide being that they had an argument with a friend, they may be able to analyse the cause of the argument and find a way to resolve it. If the children are unable to find a solution themselves, this tool may provide them with an opportunity to, at least, talk to a trusted adult about it. Additionally, if they choose the ‘stormy’ weather, which is ‘Bad’, for more than 2 weeks and the children cannot find a reason on their own, it may be helpful to set up a system where they can talk to a trusted adult whom they can then turn to.
As this study is based on results before the COVID-19 pandemic, we would like to use these results as a basis for further research.
Limitations
Despite the abovementioned strengths, this study has some limitations. The participants were limited to students from elementary, junior high, and senior high schools in three prefectures, rather than throughout Japan. Assessment methods other than a questionnaire survey, such as interviews, could have been considered. We could also have considered the possible influence of assessment time on disorders with diurnal variations, represented by depression and orthostatic disturbance. Further, the results may be related to Japan’s unique culture, so it would be necessary to conduct research in other countries. A future challenge is to further examine methods to effectively use the self-rated health assessment tool and promote organic collaboration with external support institutions. It is especially important to promptly develop systems for appropriate and organic collaboration between educational settings and medical or welfare services.
Data availability
All data generated or analysed during this study are included in this published article.
References
American Psychiatric Association (2013) DSM-5: Diagnostic and statistical manual of mental disorders. American Psychiatric Publishing, Arlington. DSM-5 Seishinshikkan no shindan・toukei manyuaru Translated by Takahashi S, Ohno Y. Igaku-Shoin Ltd, Tokyo, pp. 155–186
Baba Y, Kondo K (2005) Jseinoroudou to shukanntekikennkoukann – shuugyoukeitai joukyoubetubunnseki [Women’s labor and subjective health: an analysis by employment type and situation]. Inst Res Household Econ 65:51–59. http://kakeiken.org/journal/jjrhe/65/065_06.pdf
Beautrais AL (2001) Child and young adolescent suicide in New Zealand. Austr N Zealand J Psychiatr 35(5):647–653. https://doi.org/10.1080/0004867010060514
Birleson P (1981) The validity of depressive disorder in childhood and the development of a self-rating scale: a research report. J Child Psychol Psychiatr 22(1):73–88. https://doi.org/10.1111/j.1469-7610.1981.tb00533.x
Brent DA, Perper JA, Moritz G et al. (1993) Psychiatric risk factors for adolescent suicide: a case-control study. J Am Acad Child Adolesc Psychiatr 32(3):521–529. https://doi.org/10.1097/00004583-199305000-00006
Bridge JA, Goldstein TR, Brent DA (2006) Adolescent suicide and suicidal behavior. J Child Psychol Psychiatr 47(3–4):372–394. https://doi.org/10.1111/j.1469-7610.2006.01615.x
Firth MA, Chaplin L (1987) Research note: the use of the Birleson Depression Scale with a non-clinical sample of boys. J Child Psychol Psychiatr 28(1):79–85. https://doi.org/10.1111/j.1469-7610.1987.tb00653.x
Gould MS, Greensberg T, Velting DM et al. (2003) Youth suicide risk and preventive interventions: a review of the past 10 years. J Am Acad Child Adolesc Psychiatr 42(4):386–405. https://doi.org/10.1097/01.CHI.0000046821.95464.CF
Gould MS, Kramer RA (2001) Youth suicide prevention. Suicide Life-Threat Behav 31:6–31
Grøholt B, Ekeberg O, Wichstrøm L et al. (1998) Suicide among children and younger and older adolescents in Norway: a comparative study. J Am Acad Child Adolesc Psychiatr 37(5):473–481. https://doi.org/10.1097/00004583-199805000-00008
Harrington R (1994) Affective disorders. In: Rutter M, Taylor E, Hersov L (eds.) Child and adolescent psychiatry: modern approaches, 3rd edn. Blackwell Science, Salt Lake City, pp. 330–350
Hoshi T (1988) Kenkoushihyo to QOL [Health indicator: qualities of life and health care]. Jpn J Health Behav Sci 3:59–68
Jacobs D, Walsh BW, McDade M et al. (2009) Signs of self-injury prevention manual. Screening for Mental Health, Wellesley Hills Gakkouniokeru jisatuyobou-「jishouno sain」puroguramujisshimanyuaru. T. Matsumoto, Trans.). Kongoshuppan, Tokyo
Kaplan GA, Camacho T (1983) Perceived health and mortality: a nine-year follow-up of the human population laboratory cohort. Am J Epidemiol 117(3):292–304. https://doi.org/10.1093/oxfordjournals.aje.a113541
Marttunen MJ, Aro HM, Henriksson MM et al. (1991) Mental disorders in adolescent suicide. DSM-III-R Axes I and II diagnoses in suicides among 13- to 19-year-olds in Finland. Arch Gen Psychiatr 48(9):834–839. https://doi.org/10.1001/archpsyc.1991.01810330058009
Marttunen MJ, Henriksson MM, Aro HM et al. (1995) Suicide among female adolescents: characteristics and comparison with males in the age group 13 to 22 years. J Am Acad Child Adolesc Psychiatr 34(10):1297–1307. https://doi.org/10.1097/00004583-199510000-00015
Ministry of Education, Culture, Sports, Science and Technology (2015) How schools should be as a team and future improvement measures. Central Education Council, Ministry of Education. Tokyo. https://www.mext.go.jp/b_menu/shingi/chukyo/chukyo0/toushin/__icsFiles/afieldfile/2016/02/05/1365657_00.pdf
Ministry of Health, Labour and Welfare (2021) Chapter 3: White Paper on Suicide Prevention; Suicides by age group. Available at https://www.mhlw.go.jp/content/1-1-03.pdf. Accessed 28 Dec 2021
Ministry of Health, Labour and Welfare (2020) Chapter 2: White paper on suicide control; Chapter 3: Status of youth suicide. Available at https://www.mhlw.go.jp/wp/hakusyo/jisatsu/19-2/dl/2-3.pdf. Accessed 28 Dec 2021
Ministry of Education, Culture, Sports, Science and Technology (2021) Research Collaborators’ Meeting on Suicide Prevention for Students (2nd meeting) https://www.mext.go.jp/b_menu/shingi/chousa/shotou/164/gijiroku/1413457_00005.htm. Accessed 28 Dec 2021
Murata T, Shimizu A, Mori Y et al. (1996) Gakkouni okeru kodomo no utsubyou Birleson no shouniki ustubyousukeeru kara no kentou [Childhood depressive state in the school situation-Consideration from the Birleson’s Scale]. Jpn J Psychiatr 1:131–138
Murberg TA, Bru E (2004) School-related stress and psychosomatic symptoms among Norwegian adolescents. Sch Psychol Int 25(3):317–332. https://doi.org/10.1177/0143034304046904
Narishige R, Kawashima Y, Saito T et al. (2012) Jidou・seinenki no jisatsumisuisha no genin・douki ni kansuru kentou [Examination of the causes and motives for suicide attempts in childhood and adolescence]. Jpn J Child Adolesc Psychiatr 53:46–53
Okada M, Nakadoi Y, Fujikawa A (2016) 2fundedekiru Kodomono Mentaruherusu Chekkushiito [Children’s mental health check sheet that can be done in 2 minutes]. Gakuji Press, Tokyo
Okada M, Suzue T, Tamura Y, Katayama H et al. (2009) Investigation on the rate and state of self-reported depressive symptoms in high school sample of Japanese adolescents: using the Birleson depression self-rating scale for children (DSRS-C). Jpn J Child Adolesc Psychiatr 50:57–68
Okado J, Hoshi T, Hasegawa A et al. (2000) Shukantekikenkoukan no igakuteki igi to kenkoushien katsudou [Total review of subjective health and its supportive system]. Comprehensive. Urban Stud 73:125–133
Shaffer D, Gould MS, Fisher P et al. (1996) Psychiatric diagnosis in child and adolescent suicide. Arch Gen Psychiatr 53(4):339–348. https://doi.org/10.1001/archpsyc.1996.01830040075012
Shafii M, Steltz-Lenarsky J, Derrick AM et al. (1988) Comorbidity of mental disorders in the post-mortem diagnosis of completed suicide in children and adolescents. J Affect Disord 15(3):227–233. https://doi.org/10.1016/0165-0327(88)90020-1
Sugisawa A, Sugisawa H (1995) Kenkou jikohyouka ni kansuru kenkyuu no tenkai-beikoku no kennkyu jirei wo chuushin ni [Development of research on health self-evaluation: focusing on U.S. research cases]. In: Sonoda K (ed) Changing paradigms in health. University of Tokyo Press, Tokyo, pp. 73–83
Takamiya S, Kawamura M, Ishikawa S et al. (2015) Kodomo no mentaruherusu to shinshinshou [Children’s mental health and psychosomatic disorders]. Jpn J Psychosomat Med 55:1323–1328
Tanaka H, Tamai H, Terashima S et al. (2000) Psychosocial factors affecting psychosomatic symptoms in Japanese school children. Pediatr Int 42(4):354–358. https://doi.org/10.1046/j.1442-200x.2000.01243.x
Tanaka H, Terashima S, Borres MP et al. (2012) Psychosomatic problems and countermeasures in Japanese children and adolescents. BioPsychoSocial Med 6:6. https://doi.org/10.1186/1751-0759-6-6
Yamamoto H, Fukushima H, Yamada F (2009) Daigakusei no kenkoushindanji ni shukanntekikenkoukan wo toukoto no igi [The significance of questioning subjective health views during medical examinations of university students]. J Jpn Mibyo Syst Assoc 15:341–344
Acknowledgements
We would like to thank all the participants, our colleagues, and Professor Harumi Katayama from Hamamatsu Medical University who provided us with guidance about a necessary and sufficient method to create a questionnaire for this study.This study was supported by JSPS KAKENHI grant numbers JP18H05748, 19K20944, and JP20H01630. The funding body had no role in the design of the study or collection, analysis, and interpretation of data or in writing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
All procedures were carried out in accordance with the standards of the institutional ethics committee, the 1964 Helsinki Declaration and its later amendments. The study was approved by the Medical Ethics Committee of our institution (FY 2018, approval number: 2).
Informed consent (consent to participate)
Although we obtained consent from the students’ respective principals, each student was required to provide his/her own consent before participation. Written informed consent—such as, providing one’s name for indicating consent—was not sought from the participants and parents or guardians. While the questionnaire had no field for students to write their names, all the questionnaires distributed to students included the options “I agree” and “I do not agree” to choose from at the top. Therefore, students who chose “I do not agree” did not complete the questionnaire. We only received answers from students who chose “I agree.” For participants under the age of 16 years, each class teacher explained the questionnaires to their parents or guardians, and verbal consent was obtained from them. These participants were asked to choose their own answers to questions at the top of the questionnaire, i.e., whether they would or would not answer the questions in this questionnaire, including the intention of their parents or guardians.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Okada, M., Nakadoi, Y. & Fujikawa, A. Relationship between self-rated health and depression risk among children in Japan. Humanit Soc Sci Commun 9, 136 (2022). https://doi.org/10.1057/s41599-022-01148-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1057/s41599-022-01148-x
This article is cited by
-
Prevalence and Correlates of Depressive and Generalised Anxiety Symptoms Among Female Adolescents in Nepal: Results of a Cross-sectional National Population-Based Survey in 2022
Child and Adolescent Social Work Journal (2024)