Abstract
Seen presently during the global COVID-19 global health crisis are the ways government agencies are enabled by digital data collection through the development of contact tracing technologies (CTT) and mobile-based tracking in their effort to limit the spread of the COVID-19 coronavirus. While recent research has focused on contact tracing and privacy (Simko et al. 2020. Contact tracing and privacy: studying opinion and preferences), contact tracing and data protection (Abeler et al. 2020. JMIR mHealth uHealth 8(4): e19359) contact tracing system and information security considerations (Gvili, 2020. Security analysis of the Covid-19 contact tracing specifications by Apple inc. and Google inc), CTT and the data collected and curated have not been framed to date via their intersections with health-datafication and the research participant. As this article outlines, each is strongly linked to public health, healthcare industries and to modalities of capturing and producing knowledge that is expected to help in addressing public health concerns. Where different countries and regions are implementing a range of social distancing and/or social isolation recommendations, some have introduced contact tracing and quick response (QR) barcodes on mobile device apps. To additionally explore access, uptake and use that accompany such technologies, the International Responses to COVID-19 Contact Tracing: COVID-19 APP Uptake and Use Survey was developed and used with participants living in Singapore, Australia, the United States and the United Kingdom. The article concludes that in the process and counter to the common good or public interest objective that all are kept safe, new forms of risk and exposure are being produced.
Similar content being viewed by others
Ecosystems of contact tracing technology: mobile data and the contagious body
This article critically considers how people become research participants through communication technology when they are customers (of a product or service), ‘patients’ (having a positive COVID-19 test) or using contact tracing apps to ‘check-in’. In their appraisal of the term dataveillance, Ruckenstein and Dow Schüll (2017, p. 264) describe it as a process distributed across multiple interested parties—these including contact tracing technologies (CTT) with aged care services, health data aggregators, government services and agencies, and individuals who have ‘opted-in’ to providing health and other meta information (either voluntarily or inadvertently). The article suggests a convergence has occurred between notions of the patient, the customer, and the research participant as the distinct lines between each are now blurred.
Drawing on international qualitative and quantitative survey data, my goal for this study is to consider the social, research and health benefits of CTT in the context of Big Data and the automation in large-scale data collection and analysis. The present study is guided by the following questions: (a) to what extent are we seeing a change in the way that health research participants are understood and how is this conceptualised?; (b) what assumptions and aspirations are embedded in contact tracing technologies (CTT), and related to this; (c) what indicators exist for where CTT and practices might lead in terms of the datafication of health? The article will discuss the need to recognise information/data and personal privacy alongside concerns for collapsing national economies and the implications for global health. This paper concludes that former techniques of connection to community (traditional health providers for one) and health research are reconfigured through this changing landscape of personal engagement in health-data ecologies of ‘visibility’ and big health-data agglomerations.
International responses to COVID-19 contact tracing
Since the COVID-19 pandemic began, governments internationally sought means to track the spread of the disease, and mobile smart phones as an ideal form of already-there contact tracing technology (CTT), carried on potentially contagious bodies, held some merit.
From March 2020, the respective governments in Italy, Austria and Germany began working with mobile carriers to share users’ aggregated location data to help them monitor whether people were complying with restrictions to movements during the quarantine lockdown and identify potential ‘hot spots’ where people were gathering (Pollina and Busvine, 2020). In turn, the government of Poland required quarantined people to use an app to periodically take and submit geo-located ‘selfies’ to prove that they were at home. If their photographs were not received within 20 min then the police were alerted to attend the homes of people who were not in compliance with the regulations (Hamilton, 2020). England and Wales’ NHS contact tracing app was to have been available for users to download in May 2020 (Leprince-Ringue, 2020) and subsequently launched in September of that year using Apple and Google’s automated contact tracing technology and “tell[s] people to self-isolate if their phone detects they were near someone later determined to have the virus” (Kelion and Cellan-Jones, 2020). From private industry in the US, Google and Apple are working on contact tracing capabilities and apps; however, they are not, at this point, actually making the apps but have begun creating a simple application programming interface (API) (Vaughan-Nichols, 2020). For its own part, albeit not nationally adopted, the US has the Care19 alert app that uses Bluetooth proximity technology provided jointly by Apple and Google Exposure Notification Systems. Director of the US’ National Institute of Allergy and Infectious Diseases, Dr. Anthony Fauci, argued that the combination of scientific research and socio-technological affordances will assist in managing the COVID-19 pandemic in the country (Fauci, 2020, n.p.).
Taiwan implemented a metaphorical ‘geo-fence’ using consumers’ mobile phones whereby the technology alerted authorities when quarantined individuals left their designated ‘shelter locations’ or turned off their mobile devices. The geo-location data on their phones would alert authorities to movement outside of a permitted area (Claburn, 2020). Israel and South Korea used mobilising identification through contact tracing as well as methods of isolation and testing from the early stages of the pandemic’s spread. Singapore’s TraceTogether app for its part had low public take-up rates at around 20 percent of the population, then had a very significant ‘second wave’ of infections (Taylor, 2020, n.p.). Australia modelled their COVIDSafe app on that of TraceTogether and as of 1 June, 2020, 6.13 million people had downloaded the COVIDSafe app onto their mobile phones (Meixner, 2020). However, amid public concerns in the nation for its effectiveness (Greenleaf and Kemp, 2020a, 2020b), quick response (QR) codes read by usually free apps on smartphones—which appear as a square with a grid of smaller squares as a pattern inside it and typically in black and white—were soon being adopted by state and territory governments for hospitals, schools, and the like. The private sector themselves use the QR service in many public locations including shopping malls, bars, cafes and entertainment venues. The problem with the use of QR codes is that there is no uniform approach that each takes to digital privacy as the management of COVID-19 check-ins in public locations is increasingly outsourced.
Signage in public hospitals in Australia by way of one example provides an Australian privacy policy statement at the point of check-in via QR code using an app. Important too is the notice that visitors must show the completed form to the staff member on duty. The visitors to public hospitals in Australia also have alternate methods to supply their data for the subsequent purposes of contact tracing should a user not have a smart phone. They include entering key contact details on a tablet, or on a desk-top computer to access an online form, or an option to speak directly to a staff member on duty and write their details down on paper.
Conversely to this, a request for data via a QR code in a shopping mall often finds scant explanatory information (in terms of why the data is being collected, who has access and how personal details are collected, stored and deleted) for visitors to the stores. From this study’s qualitative responses, a respondent from the UK commented that in regard to shops and cafes “no one ever checks, and I have seen people just walk right past them [the signs with QR scanners]”. Moreover, for another participant “I do not like privacy invasion services and therefore will not even consider using a COVID-19 Contact Tracing App even though my personal health puts me in a ‘high risk category’ for contracting the virus”.
In the face of arguments in regard to ‘biocapitalism’ whereby personal data is a commodity (Benjamin, 2020; Braidotti, 2013; Rajan, 2006) a number in first and second-world nations are also customers of the services that put such data ‘to work’ (phone companies, wearable device manufacturers such as Fitbit, Oura Ring, Apple Watch, Garmin or Google Fit, medical devices such a pacemakers, as well as social media), and patients (located in and/or using health services or care homes and the like). What is to be found is that in some respects the people that access and use mobile CTT for the purposes of data collection simultaneously act as de facto research participants. This provocation reflects Ruckenstein and Dow Schüll’s (2017) distributed communications across multiple interested parties. There is a building conceptualisation of the nexus between customer, patient and research participant being demonstrated in the global tracing of the COVID-19 disease. This comes as people are monitored via their mobile smart devices for their location, connection to others that have tested positive (using Bluetooth technology on mobiles) and consequent infection with further data collected about the duration of the disease and long-term effects over time (if any) made rapidly available across networks. The implication is that mobile apps that trace and notify people of possible infection could, on the margins and in the right conditions, help direct testing resources to those living in areas at higher risk or warn health officials that necessary steps such as lockdown laws might need to be enforced for the common good.
Stepping away from the ‘giants’ of data aggregation such as Google, Apple and the like, some have themselves begun the process of watching and documenting their personal health data collected on wearable devices before actual flu-like symptoms appear in order to share their information for the purpose of predicting the likely onset of sickness in communities. The opt-in process allows individuals’ data to be anonymously combined and plotted to inform others about the possible geo-spread of infection with linked paths provided on the website for access to all public data. The site Quantified Flu (https://quantifiedflu.org/), for example, states that people can “Report when you got sick and share your wearable device data. We’ll plot your data for you!” The wearable device customers/research participants/potential patients are called to “Sign up for daily check-ins to tell us if you got sick, as well as symptoms and viral test results.” As shown in Fig. 1, the visualised data plots can depict such information as the number of participants reporting spikes in their heart rates that could be connected to pre-flu symptoms over monthly timeframes. The likes of which can be set to use for the detection of potential ‘hot spots’ of infection in communities.
Visualised data plots can depict such information as the number of participants reporting spikes in their heart rates that could be connected to pre-flu symptoms over monthly timeframes. The likes of which can be set to use for the detection of potential ‘hot spots’ of infection in communities. This figure is covered by the Creative Commons Attribution 4.0 International License. Copyright © https://quantifiedflu.org/, all rights reserved.
For this Quantified Flu project, individuals’ accounts are managed via Open Humans, pitched as offering some control by enabling users to themselves “securely store, access, and manage” their wearable, and quite intimate data:
The Open Humans Foundation is a … nonprofit organisation dedicated to empowering individuals and communities around their personal data, to explore and share for the purposes of education, health, and research. The organisation operates and manages Open Humans, a project and community that enables individuals to connect their data with research and citizen science.
Other publicly available points of access away from ‘Googlized’ health research (Sharon, 2019, 2016) find options in open-source data. GitHub for example holds accessible data that can be used with R (free statistical computing software with capacity for graphics output) for the creation of plots and analysis relating to the pandemic such as COVID-19 infections, hospitalisations or deaths over time in a given location. Figure 2 shows a visual representation of data drawn across 2020 to 7 January 2021 as a ‘heatmap’ representing the spread of COVID-19 cases in English cities over a rolling 7-day average of the new confirmed cases and ordered by the date at which they reached their peak number of new cases.
A visual representation of data drawn across 2020 to 7 January 2021 as a ‘heatmap’ representing the spread of COVID-19 cases in English cities over a rolling seven-day average of the new confirmed cases and ordered by the date at which they reached their peak number of new cases. Source: VictimOfMaths, COVID-19 plot of Public Health data (England) (https://github.com/VictimOfMaths/COVID-19) This figure is covered by the Creative Commons Attribution 4.0 International License; copyright © VictimOfMaths, all rights reserved.
Another example of enabling users themselves is one developed in the US as part of the microCOVID Project as an online calculator where a user can add personal details online about one’s daily events/routines, from travel to and from work to picking up a take-away meal, in order to calculate a personalised risk assessment for going out into public spaces (https://www.microcovid.org).
Past research has pointed to the role of social media as an important space for connection, for example danah boyd articulates how social media provides a “networked public” with specific technological architectures and affordances that shape the interactions and dynamics of users on these sites (2010, p. 39). This present article might therefore shed light on the state of these individuals now that their content is being frequently collected/stored/moderated/shared and the consequences therein. In doing so it will be contributing to an understanding of what Gillespie views as powerful backstage elements in terms of the systems of organising content in regard to social media (2010) which is being applied to the ‘technological architectures’ of informedia and CTT in this study. As Myers West argues, gaining user perspectives on these systems is valuable in articulating the contesting private/public understanding of the digital media being used (2017).
Method: Informedia and networked participants
In this article that focuses on contact tracing during the COVID-19 pandemic for health research, I take an overarching examination of the way health data is collected to ask whether there is a consequent change to how participation in health research is understood and the implications therein.
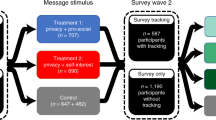
My overall approach is of an exploratory nature; oriented towards access to contact tracing, uptake and use, but also exploring public perceptions and experiences with such. In doing so, I follow Thelwall (2018) who used a mixed methods and exploration-oriented methodology for studies of public user comments made and regarding a social media platform (in their study of Youtube). By way of explorative mixed method for this study, I drew on both qualitative and quantitative data from international participants about their access and use of contact tracing apps in December 2020 through early 2021. Responses were gathered just prior to the widespread roll-out and uptake of COVID-19 vaccinations internationally. An anonymous and voluntary survey was created in Qualtrics and subsequently administered by an international (third-party) research group, Dynata (dynata.com), to conduct the qualitative and quantitative survey to participants due to COVID-19 restrictions on travel that prohibited fieldwork. Consent materials were provided with a Plain Language Statement at the beginning of the survey. Institution ethics approval for data collection was sought and received by the Faculty Human Ethics Advisory Committee (HEAG) under the terms of Deakin University’s Human Research Ethics Committee (DUHREC); approval number HAE-21-008.
It is anticipated that this ongoing work will open up new ways of understanding individuals as networked patients, customers, and research participants via emerging communications technologies over time. The present study is, then, guided by the following research questions: (RQ1) what assumptions and aspirations are embedded in contact tracing technologies (CTT), and related to this; (RQ2) what indicators exist for where CTT and practices might lead in terms of the datafication of health? The study also asks: (RQ3) to what extent are we seeing a change in the way that health research participants are understood? And finally, (RQ4) do those that have had experience with and felt comfortable with wearable media express different perspectives about CTTs?
Survey instrument
An anonymous and voluntary survey, International Responses to COVID-19 Contact Tracing: COVID-19 APP Uptake and Use Survey was designed and created for this project. The study drew on a total of 2000 international participants with 500 people each living in Australia, the United Kingdom (UK), Singapore and the United States (US), respectively. The survey comprised 21 multiple choice and short answer questions. The multiple choice questions and short answer responses would take up to fifteen to twenty minutes to complete.
Screening criteria included responses be in English. The research required broad sweep data on participant CTT practices. To achieve this, the survey included free text sections as well as tick the box questions. The aim of this survey was to establish an understanding of the intersecting uptake of contact tracing, the continuing COVID-19 pandemic and digital information communication technology practices more broadly.
Participants
Participants (n = 2000) were over 18 years of age, but beyond this criterion, they were from a wide range of ages and socio-economic groups. Participants in the study described their gender as Female (n = 978 or 49%), Male (n = 964 or 49%), Non-binary, Intersex, or Unspecified (n = 30 or approximately 1%) or did not wish to disclose (n = 28 people or approximately 1% of the sample).
The possible risks to participants included psychological stress in relation to discussing work or home situations in the current high-stress environment created by the COVID-19 event. Participants were provided with national helpline contacts should they feel any distress resulting from their participation in the research.
Results
Outlined below are the discreet methods of contact tracing data collection, storage and monitoring for analysing Health Data by/for participants. As the survey was conducted with participants living in Australia, Singapore, the United States (US), and the United Kingdom (UK) at the time the research took place, the corresponding official apps were indicated as having been downloaded (Table 1).
Singapore’s TraceTogether appeared to have had the highest take-up rate of noted apps. It was downloaded by 346 out of 488 participants comprising the Singapore sample (71%) with 6 people living in Australia and the US respectively stating they had downloaded TraceTogether and 8 people in the UK had done so. In the Singapore sample, 99 people (20.3%) stated that they had not downloaded a contact tracing app on their smart phone. As noted earlier, Singapore had low initial take-up rates for the contact trace app at the start of the pandemic in early 2020. This was followed by a second wave of infections which might have motivated a number to consequently download the app.
Of those living in the UK, 71 people (14.4%) stated that they had downloaded COVID Tracker with 5.5% of participants in Australia, the US and Singapore, respectively, to also have done so. Some 48 people (9.7%) in the UK sample declared having downloaded COVIDSafe. A total of 267 people (54%) reported not having downloaded a contact tracing app at all. Of those in the UK sample, 89 people (18%) responded to having downloaded another app, for example from the area, NHS COVID app (58 participants), NHS Scotland (2 participants), Northern Ireland COVID app (2 people).
Australia’s official COVIDSafe app saw just under half (41.5%) of the Australian sample download the app (203 out of 489 people) leaving 255 people (52.1%) not having downloaded this contact tracing app. A small number had chosen Australian alternative contact registers such as mySA GOV from South Australia (4 people), SafeWA from Western Australia (2 people).
The sample from the US had the lowest reported uptake of contact tracing apps with 403 people (82.4%) from the US sample responding that they had not downloaded a contact tracing app. Participants in the US reported downloading Care19 (10 people or 2% of the sample), Corona-Warn-App (12 people or 2.5% of the sample), but COVIDSafe from Australia found uptake by 41 people living in the US (or 8.4% of the sample) and COVIDTracker had downloads by 29 people living in the US (or 5.9% of the sample). These instances likely by expatriates.
Albeit that contact tracing apps had been downloaded, as is the case with telecommunications and technology generally, access is not the same as use. That is, access to the technology is not the same as having the skills and inclination to use them. Participants were subsequently asked to respond to the question, Q4—If you have Smart Phone access, which things did you use it for since the start of the COVID19 Pandemic and to list all that apply. As shown in Fig. 3, combined data collected from respondents in all four countries revealed that 396 people (12.52%) reported that their activities included connecting with others in a private virtual group to discuss the Pandemic; 1064 (33.63%) reported using social media such as Facebook, Twitter, WhatsApp or Instagram to discuss publicly the Pandemic such as lock-down, personal protective equipment, health concerns for themselves, family and friends; 696 (22%) said that they download a Contact Tracing app (see Table 1 in regard to official contact tracing app by country in the study); while 499 (14.19%) had downloaded a COVID-19 check in platform using a Quick Response (QR) code (see more detail by country in Table 4).
Combined data collected from respondents in all four countries revealed that 396 people (12.52%) reported that their activities included connecting with others in a private virtual group to discuss the Pandemic; 1064 (33.63%) reported using social media such as Facebook, Twitter, WhatsApp or Instagram to discuss publicly the Pandemic such as lock-down, personal protective equipment, health concerns for themselves, family and friends.
Indicative comments revealed that remaining connected was a priority with many stating that since the start of the COVID-19 pandemic that social networks were central to communicate with “Family”, “Friends and Relatives”, “Friends during school”, “Children” and “Colleagues”. Some used social media for information and guidance with another participant stating that they use social media (including one or more of Twitter, Telegram, Tik Tok, WhatsApp, Snapchat, or Instagram) to assess “How accurate the information about the vaccine availability is” (A1). As a form of informedia then, we find participant comments that reveal how a number are going to COVID-19 specific apps for information during periods of Lockdown. Further:
A2: “I use my mobile for the COVID-19 app which has useful help tips to stay healthy”.
A3: “For up-to-date rules and regulations as laid out by the Queensland [Australia] government”.
A4: “Whether the national lockdown should be extended and whether the regional approach is appropriate”.
For others, social media were used to discuss “How stupid it is that we let government dictate our movements” (A5).
The range of topics discussed in online spaces via a computer or Smart Phone are outlined in Table 2 and included the lock-down, personal protective equipment (PPE) in terms of where to buy it and how to use it, health concerns for themselves, family or friends and COVID-19 testing. Some 559 (17.67%) respondents stated that they do not use a Smart Phone at all (Fig. 3) increasing to 37.4% of the total respondent count when computer access was combined with smart phone access for social media use in regard to discussing issues connected to the pandemic (Table 2).
Drilling down into the short answer responses to topics of ‘Lockdown’, ‘Health concerns for you’, ‘Health concerns for family and friends’ and ‘COVID-19 testing’ a further analysis of aggregate data from all countries surveyed saw qualitative comments that specifically commented on worry:
B1: “I worry about catching the virus”.
B2: “I am concerned for my children going back to school and how worried I am about it”.
B3: “I worry about my son who still had to go to work during lockdown”.
B4: “I worry about my family and friends getting sick”.
B5: “Worrying about my daughter’s job and her finances”.
B6: “Some family and friends are needed as essential workers to still go to work. They go on public transport, so I worry for them catching the virus”.
Other concerns reported in regard to the impact of the circulating COVID-19 virus were diminished mental health due to fear and social isolation:
C1: “The impact on the mental health and safety of my children concerns me”.
C2: “Covid-19 has effects on my mental health so I am reaching out for connection to others”.
C3: “I am fearful of catching the virus and have mental health struggles because of this”.
C4: “My mental health has gone down due to social isolation”.
A number of participants sought help in addressing public health concerns using COVID-19 contact tracing apps:
D1: “I use this contact tracing app for whether I need to be tested”.
D2: “I used an app to show me where I can check-in to the nearest testing station to me”.
D3: “I have an app on which I have to record each morning how I feel and do I have any COVID symptoms, as a result of a COVID test that I had back in March and it was negative.
Important in terms of a public health policy is ensuring that all have access to the important information about hygiene, testing, symptoms, isolation, regulations and so forth in their own language. Participants in the study were asked if information on official contact tracing apps was in their first language (Table 3). The question required a broad response and was not specifically tied to whether a participant had first downloaded the app or not. Indeed, language is a motivating factor, and a number might not have downloaded the app because it was not in their first language. For those participants with access to a contact tracing app in the UK, 404 responded that they had access to such a service in their first language (81.8%), but a number (90 people) did not (18.2%); respondents in the sample from Singapore (431 people) had official health related information via contact tracing apps in their first language (88.3%) while 57 responded that they did not (11.7%). Some 370 participants in Australia noted that they had access in their first language (75.7%), but 119 respondents (24.3%) did not. In the US, 308 people said that information on an official contact tracing app was in their first language (63%) with 181 people responding that official information was not in their first language (37%).
In terms of contact tracing, it is presently an individual choice to opt-in in many countries, but with emphasis on achieving widespread uptake of the CTT for the health of communities, narratives are frequently underscoring such action as being for the collective, common good—though, it is not clear if more will have access to key information and tracing via CTT in a range of languages or how they might serve those with special needs, thus effecting use and access.
By way of comparison with regard to methods of contact tracing in communities, respondents were also asked if they had instead been required to use a quick response (QR) code on their smart phone when attending public places including hospitals, healthcare providers, shopping centres, restaurants and cafes, entertainment venues, other government institutions or places of education. Table 4 shows that from the sample, in Singapore, 44.5% of people had been required to ‘check-in’ with a QR barcode scanner, 28% of respondents living in Australia had been asked to do so, 20% of people in the UK had and only 7% of people in the US reported that they had been asked to use a quick response (QR) barcode scanner.
Returning to the issues of access and choice, respondents were asked whether they had ever been given an option to instead provide their name and contact details written on a piece of paper instead of using a QR barcode scanner in a public place (Table 5). Some 41.3% of people in Australia were given that option (48.5% said they had not), 28.1% in the UK had been given a choice but 64% responded that they had not, and; 24.8% in Singapore noted that they were given an optional way to check-in (62.9% had not), with just 4.5% of people in the US given the alternate check-in option with 90.8% responding that they had not been offered this choice.
A further question about the types of data being collected by QR codes found that in the sample 27.2% of people in Singapore, 19% of participants living in the UK, 18.2% of respondents in the US, and 12.9% of the respondents in Australia stated that an official Contact Tracing app or QR code app had asked for their race or ethnicity.
Examining a different tracing technology via wearable devices for personal health monitoring found the same spread of uptake rates as for CTT and QR scanner check-in rates. Singapore had the highest uptake and use rates whereas the US and Australia recorded the lowest. As outlined in Table 6, while a number of people do not use a wearable device as recorded in this study (1202 people or 61.3% of the total sample), 20.7% of respondents did report using wearable devices for monitoring their heart rate (highest count was Singapore with 36.1% of its sample and the lowest was Australia with 11.2%); exercise levels at 19% or 372 people of the total sample (highest count was again in Singapore with 27.7% and the lowest was in the US with 15.1% closely followed by Australia at 15.7% of the countries’ respective samples); calories burned saw 15.8% of the total sample respond (309 people) and again respondents in Singapore recorded the burn rate of calories to a greater degree (21.1%) than did Australia (12.1%) or the US (14.7%). The data here suggests that participants in Singapore report being health conscious at a higher rate than Australian or American-based participants.
Recording data for intimate categories such as the menstrual cycle (4.5%, 88 people) and fertility cycle (1.1%, 22 people), however, saw an inverse of findings with the US recording higher activity rates for the variable ‘menstrual cycle’ (6.1%) and Singapore the lowest (3.5%) and for the variable ‘fertility cycle’ responses from those in the US were at 2% compared to 0.4% in the UK and 1% in Singapore and Australia respectively.
The findings regarding cross-countries comparisons on key questions such as wearable uptake and use, cultural diversity, and the general mobile media culture in this section indicates that a number are indeed cognitively and emotionally labouring through their personal investment in recording daily activities related to the collection (at least) of health-related data.
Discussion
There were two main limitations associated with the study. First, the survey was conducted in English leaving potentially rich insights unrepresented. This is a bias that might be addressed in future studies so that there is greater representation from non-English speaking participants. Second, there are many variables that impact on the spread of the COVID-19 virus and this study mainly focused on the uptake and use of CTT (COVID apps or QR barcode scanners) for transmission prevention.
While it is reasonable to argue that a hospital or school requires stringent health measures for those within and a detailed policy (for check-in directions, monitoring, data collection processes), the virus is not limited to spreading in these locations alone. The wider community is potentially put at risk when there is no consistency in confirming that when a person enters a site—be it a shop, restaurant, children’s play centre or workplace—that they actually do check-in properly so that they can be contacted if concern for a potential COVID-19 infection is raised. Checking-in has become a moral action (for the common good) and verification of such a de facto policing measure by private citizens. These come with their own stress when people act for or against their deeply held morals increasing emotions directed at oneself like guilt, shame or anger (Shay, 1994). This at a time of heightened concern as noted by the participants’ comments citing “worry”, fear and decreased mental health. In the long run, a number might lose trust in the political state.
The study found that CTT use differed across nations. People might not act in accordance with social expectations, for reasons of: (1) not understanding the instructions (an issue if information is not in their first language. As we saw, the US had lower CTT updake and also that official information was not in users’ first language (37%); (2) not completing all steps such as filling in their data after being directed to a website via a QR code; (3) not having a phone to check-in; (4) service staff overlooking the fact and allowing entrance to a public venue regardless; (5) people being conscientious objectors due to privacy concerns for example and pretending to check-in. Apart from the health and wellbeing concerns, the possible implications for data privacy are that marketing, and data companies operating under opaque rules about how personal data is stored and used, might take advantage.
Certain negative ‘systems’ are amplified for a number as Benjamin (2020, n.p.) notes with regard to marginalised groups in this moment of crisis and “we need to change the rules”. Falling upon neo-liberal ‘technological solutionism’ (Morozov, 2014), where technologies are flagged as bio-political ‘fixes’ in the public interest, Benjamin (n.d.) adroitly points to global instances of engineered inequality and default discrimination that consequently result. This has played out worryingly during the recent COVID-19 pandemic where algorithms determining locations of needed care, and conferring mediated health services, are called on to codify a ‘survival of the fittest’ approach to human life in which “ableism, racism and classism operate together to make poor, racialized and disabled people’s lives expendable. Not inevitably, but predictably” (Benjamin, 2020, n.d.). The spread of COVID-19 and subsequent periods of state-enforced lockdowns are events often most keenly felt by the working classes that do not have the capacity to have their work shifts covered by others, to work from home, work/live in a second coast or country home instead of in crowded cities or take extended periods away from employment using personal savings to support themselves. This leaves them and their children vulnerable as a result. The public interest requirement for individuals to have health certification for public health purposes as they move about the community already exists in many contexts around the world but proposed ‘immunity passports’ would come with deeper issues for potential discrimination.
During periods of lockdown, immunity passports “could allow immune individuals to follow less stringent requirements around physical distancing and travel, perhaps permitting them to return to work, care for those at risk, visit friends and relatives, or undertake other activities that expose them to the virus” (Brown et al., 2020, p. 1). Immunity passports could take the form of a wristband or physical documents as in the US that certify that an individual has either been infected and is purportedly immune to coronavirus ‘SARS-CoV-2’ or is at a low risk of acquiring or transmitting severe acute respiratory syndrome coronavirus 2 (Brown et al., 2020). Emerging in late 2021 are such digital vaccine certificates. In Australia for example this is via a mobile device app featuring a green tick of validity or a digital/printable COVID certificate in Europe. Such administrations by government, however, according to Alexandra L Phelan, Center for Global Health Science and Security, Georgetown University Medical Center, and the O’Neill Institute for National and Global Health Law, Georgetown University Law Center in Washington, DC:
might create a perverse incentive for individuals to seek out infection, especially people who are unable to afford a period of workforce exclusion, compounding existing gender, race, ethnicity, and nationality inequities … Existing socioeconomic, racial, and ethnic inequities might be reflected in the administration of such certification, governing who can access antibody testing, who is front of the queue for certification, and the burden of the application process. By replicating existing inequities, use of immunity passports would exacerbate the harm inflicted by COVID-19 on already vulnerable populations. (Phelan, 2020, p. 1596).
This suggests that some form of social safety-net to financially support those unable to work for periods of time, payments for health services if not covered by public funding, along with counselling services (violence in the home often comes with such pressurised circumstances) as well as fair and equitable access to vaccination and testing regimes, would overlap with such a policy for the management of public health for the common good.
Drawing attention back to the comparative analysis of CTT across nations, Singapore for its part had low initial download rates for its contact trace app at the start of the pandemic in early 2020, followed by a second wave of infections and a probable factor in Singapore’s TraceTogether having a higher subsequent take-up rate for it and QR barcode scanners as the public strove to keep communities healthy. Australia at the time of writing saw just under half the Australian sample download its official app and 28% downloaded a QR barcode scanner for contact tracing. The sample from the US had the lowest reported uptake of contact tracing apps and QR barcode scanner access. Again, access is not the same as use where a downloaded app might remain still unused. Low take-up rates might signal important underlying factors.
For a number of networked individuals, the affordances of mobile devices as conduits for both contact tracing technology (CTT) and informedia, the term I have used here for information available from apps on digital media that have COVID-19 specific or other health updates, also highlight concerns for individual privacy (such as for location, infection and close-contact data), as well as use and even recording ethnicity. Countless private storage spaces contain the publics’ metadata without most knowing where such is located nor if/how one might change it they do. That is, one is composing/contributing to an empirical digital identity as exemplified in, for example, the data collected by CTT being potentially shared and collected in a networked ecology of app-mediated connection as well as wearables and their associated social media spaces. It seems that the contact tracing apps, wearable devices and variety of social media we download, albeit that they can offer health protection and increase our individual and collective security, are creating new datasets about us from our data willingly or unwillingly shared. They also give up our privacy and are to be potentially exploited—often by unknown entities without our knowledge, or informed consent—and the risk continues in perpetuity.
Büchi et al. (2017) argued that while individuals might be aware of online privacy, caring on its own does not automatically equate with adequate self-protection. Furthermore, a study by Van den Broeck et al. (2015) found individuals in young and middle adulthood are more at risk in relation to privacy protection compared to teenagers. In addition, the middle adulthood group had the greatest concern for their privacy yet took the least steps to protect it. There is the imperative to also evaluate how individuals’ privacy concerns fit into the broad CTT ecologies comprising now certain health benefits and privacy protection drawbacks via smart phones and the like. So much so that multiple sites now “implicitly contain a rich array of personal information, including cues to a speaker’s bio-metric identity, personality, physical traits, geographical origin, emotions, level of intoxication and sleepiness, age, gender, and health condition” (Kröger et al., 2020, p. 242).
While useful for protecting communities, how data is collected, stored and accessed, raises difficult issues of human ethics, informed consent, and digital privacy. Further is that where paper-based alternatives are not available to them individuals without a mobile smart device with the requisite COVID-19 app installed using their own language might be disadvantaged for check-in purposes or vaccine verification. Both are increasingly mandatory to work and move around communities. Where there is a common expectation now of smart phone access and use, staff overseeing check-in obligations for their own business or that of an employer might not be aware that a digital divide exists (van Dijk, 2020), and that not all have access. This bias, albeit unintended, leaves those from lower socio-economic groups and/or with a disability, disadvantaged.
Conclusion
This paper explored the main ways that health data is presently collected in the United Kingdom, Singapore, Australia and the United States via contact tracing technologies (CTT) and QR barcode scanners. Inherent in CTT are the socio-political compromises made between the public and private interest. Brought to bear in this context of health-data ecologies of visibility, big health-data agglomerations and personal engagement with digital technologies, is the important need to recognise that information/data and personal privacy sit alongside concerns for national economies impacted by the pandemic and the implications for global health where former techniques of connection to community (traditional health providers for one) with ongoing health research are being re-evaluated. Apple and Google for their part are giving public health institutes the tools they need for app-mediated contact tracing, but this means that “they will need to build the apps and the required databases for this new coronavirus approach to work” (Vaughan-Nichols, 2020, n.p.). In such contexts, the weighty decisions about civil liberties are largely taken away from democratically elected governments and are instead placed in the hands of private technology companies. Such case examples as the ones noted in this article are underscoring the additional disquiet about the intrinsic teleology of electronically enabled global communication.
Because many social media accounts are publicly available (i.e., not protected) they are seen by many as a rich source of data yielding insights into peoples’ lives, and also the way they are using social media platforms to communicate. There is now a growing body of literature related to the collection (scraping) and analysis of social media data and networks and the ethics therein of doing so for the issues of ensuring informed consent and privacy (Bhatia-Lin et al., 2019; Wasim and Sergej, 2019; Kennedy, 2016). What is worth bearing in mind is that the data entered into a system or shared might also be inaccurate when mistakes are made, out of date or intentionally false. Paradoxically, then, one’s empirical digital identity might itself be obfuscated in such networked ecologies that store and use data. The result this article aimed to highlight, is that the narrative of personal health data is a thought-provoking account of how individuals have been encouraged to contribute to the health of their communities and be inspired to take charge of their personal health-related data. This is positioned against the backdrop of government/corporate control, issues of access and digital privacy. For those engaged in the now everyday practice of using QR codes, CTT and associated social media for compiling, circulating and using data to protect their health and that of their communities—taking custodianship of the collective benefit for the common good—it is both, and more.
Data availability
The datasets generated and analysed during the current study are not publicly available but are available from the corresponding author on reasonable request.
References
Abeler J, Bäcker M, Buermeyer U, Zillessen H (2020) COVID-19 contact tracing and data protection can go together. JMIR mHealth uHealth 8(4):e19359
Bhatia-Lin A, Boon-Dooley A, Roberts MK, Pronai C, Fisher D, Parker L, Engstrom A, Ingraham L, Darnell D (2019) Ethical and regulatory considerations for using social media platforms to locate and track research participants. Am J Bioeth 19(6):47–61
Benjamin R (2020) Black skin, white masks: racism, vulnerability & refuting black pathology. Available via https://aas.princeton.edu/news/black-skin-white-masks-racism-vulnerability-refuting-black-pathology Retrieved 19 May 2020.
Benjamin R (n.d.) Are robots racist? Reimagining the default settings of technology and society, guest lecture, (23:24). Available via https://www.dropbox.com/s/ia5j8ao5ycllyzd/Ruha%20Benjamin%20Guest%20Lecture.mp4?dl=0 Retrieved 19 May 2020.
boyd d (2010) Social network sites as networked publics: affordances, dynamics, and implications. In: Papacharissi’s Zizi (ed.) Networked self: identity, community, and culture on social network sites. Routledge, London, pp. 39–58
Braidotti R (2013) The posthuman. Polity, Cambridge
Brown RCH, Kelly D, Wilkinson D, Savulescu J (2020) The scientific and ethical feasibility of immunity passports. The Lancet https://doi.org/10.1016/S1473-3099(20)30766-0
Büchi M, Just N, Latzer M (2017) Caring is not enough: the importance of Internet skills for online privacy protection. Inf Commun Soc 20(8):1261–1278
Claburn T (2020). Taiwan collars coronavirus quarantine scofflaws with smartphone geo-fences. So, which nation will be next? Personal Tech, The Register. Available via https://www.theregister.com/2020/03/24/coronavirus_quarantine_cellphone/ Accessed 24 Oct 2020
Fauci A 2020 Coronavirus Q&A with Anthony Fauci, MD. Youtube (5:50) 8 April. Available via https://www.youtube.com/watch?v=c0cYneu-hlc&feature=youtu.be Accessed 8 April 2020.
Gillespie T (2010) The politics of ‘platforms. New Media Soc 12(3):347–364
Greenleaf G, Kemp K (2020a) Australia’s COVIDSafe App: an experiment in surveillance, trust and law, University of New South Wales Law Research Series 999 [Draft]. Available via https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3589317 Accessed 30 Apr 2020
Greenleaf G, Kemp K (2020b). Australia’s COVIDSafe Experiment, Phase III: Legislation for trust in contact tracing, University of New South Wales Law Research Series. Available via https://ssrn.com/abstract=3601730. Accessed 12 Nov 2020.
Gvili Y (2020) Security analysis of the Covid-19 contact tracing specifications by apple inc. and google inc. Cryptology ePrint Archive: Report 2020/428. IACR. http://eprint.iacr.org/2020/428. Accessed 26 November 2020.
Hamilton IA (2020) Poland made an app that forces coronavirus patients to take regular selfies to prove they’re indoors or face a police visit. Business Insider. Available via https://www.businessinsider.com/poland-app-coronavirus-patients-mandaotory-selfie-2020-3?r=US&IR=T Accessed 12 Nov 2020.
Kelion L, Cellan-Jones R (2020) NHS Covid-19 app: how England and Wales’ contact-tracing service works’, BBC online, September 23. Available via https://www.bbc.com/news/technology-54250736. Accessed 12 Nov 2020
Kennedy H (2016) Post, mine, repeat: social media data mining becomes ordinary. Springer Nature, London
Kröger JL, Hans-Martin Lutz O, Raschke P (2020) Privacy implications of voice and speech analysis—information disclosure by inference. In: Friedewald M, Önen M, Lievens E, Krenn S, Fricker S (eds) IFIP International Summer School on Privacy and Identity Management. Springer, Cham, pp. 242–258
Leprince-Ringue D (2020) Contact-tracing: still no firm date for when the UK’s app will arrive. ZDNET. Available via https://www.zdnet.com/article/contact-tracing-still-no-firm-date-for-when-the-uks-app-will-arrive/ Accessed 13 June 2020.
Meixner S (2020) How many people have downloaded the COVIDSafe app and how central has it been to Australia’s coronavirus response? ABCNews, online. Available via https://www.abc.net.au/news/2020-06-02/coronavirus-COVID19-COVIDsafe-app-how-many-downloads-greghunt/12295130. Accessed 13 June 2020.
Morozov E (2014) To save everything, click here: the folly of technological solutionism. Public Affairs, New York
Myers West S (2017) Rage against the machine: network gatekeeping and collective action on social media platforms. Media Commun 5(3):28–36
Phelan AL(2020) COVID-19 immunity passports and vaccination certificates: scientific, equitable, and legal challenges, Comment The Lancet 395:1595–1597. https://doi.org/10.1016/S0140-6736(20)31034-5
Pollina E, Busvine D (2020) European mobile operators share data for coronavirus fight. Technology News, Reuters. Available via https://www.reuters.com/article/us-health-coronavirus-europe-telecoms/european-mobile-operators-share-data-for-coronavirus-fight-idUSKBN2152C2 Accessed 3 June 2020
Rajan KS (2006) Biocapital: the constitution of postgenomic life. Duke University Press, Durham, NC
Ruckenstein M, Dow Schüll N (2017) The datafication of health. Annu Rev Anthropol 46:261–278
Sharon T (2016) The Googlization of health research: from disruptive innovation to disruptive ethics. Personalized Med 13(6):563–574
Sharon T (2019) Data-driven decision making, AI and the Googlization of health research, data-driven decision making. Law Eth Robot Health 39:39–47
Shay J (1994) Achilles in Vietnam: combat trauma and the undoing of character. Scribner, New York
Simko L, Calo R, Roesner F, Kohno T (2020) COVID-19 contact tracing and privacy: studying opinion and preferences. Available via https://seclab.cs.washington.edu/wp-content/uploads/2020/05/contact-tracing-user-privacy.pdf. Accessed 20 December 2020.
Taylor J (2020) Coronavirus apps: how Australia’s COVIDsafe compares to other countries’ contact tracing technology. The Guardian, Australian edition. Available via https://www.theguardian.com/australia-news/2020/may/03/coronavirus-apps-how-australias-COVIDsafe-compares-to-other-countries-contact-tracing-technology. Accessed 3 Jun 2020.
Thelwall M (2018) Social media analytics for YouTube comments: potential and limitations. Int J Soc Res Methodol 21(3):303–316
Van den Broeck E, Poels K, Walrave M (2015) Older and wiser? Facebook use, privacy concern, and privacy protection in the life stages of emerging, young, and middle adulthood. Soc Media Soc 1(2):1–11
Vaughan-Nichols S (2020) How Apple and Google coronavirus contact tracing will work. ZDNet. Available via https://www.zdnet.com/article/how-apple-and-google-coronaviruscontact-tracing-will-work/. Accessed 15 April 2020.
van Dijk J (2020) The digital divide. John Wiley & Sons, Hoboken
Wasim A, Sergej L (2019) Social media analytics: analysis and visualisation of news diffusion using NodeXL. Online Inf Rev 43(1):149–160
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Institution ethics approval for data collection was sought and received by the Faculty Human Ethics Advisory Committee (HEAG) under the terms of Deakin University’s Human Research Ethics Committee (DUHREC); approval number HAE-21-008. The approval conforms to the broad principles of the Declaration of Helsinki.
Informed consent
All participants in this study gave informed consent.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cinque, T. Protecting communities during the COVID-19 global health crisis: health data research and the international use of contact tracing technologies. Humanit Soc Sci Commun 9, 99 (2022). https://doi.org/10.1057/s41599-022-01078-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1057/s41599-022-01078-8