Abstract
Venous thromboembolism (VTE) is the leading cause of preventable death in hospitalized patients. Artificial intelligence (AI) and machine learning (ML) can support guidelines recommending an individualized approach to risk assessment and prophylaxis. We conducted electronic surveys asking clinician and healthcare informaticians about their perspectives on AI/ML for VTE prevention and management. Of 101 respondents to the informatician survey, most were 40 years or older, male, clinicians and data scientists, and had performed research on AI/ML. Of the 607 US-based respondents to the clinician survey, most were 40 years or younger, female, physicians, and had never used AI to inform clinical practice. Most informaticians agreed that AI/ML can be used to manage VTE (56.0%). Over one-third were concerned that clinicians would not use the technology (38.9%), but the majority of clinicians believed that AI/ML probably or definitely can help with VTE prevention (70.1%). The most common concern in both groups was a perceived lack of transparency (informaticians 54.4%; clinicians 25.4%). These two surveys revealed that key stakeholders are interested in AI/ML for VTE prevention and management, and identified potential barriers to address prior to implementation.
Similar content being viewed by others
Introduction
Venous thromboembolism (VTE) is the leading cause of preventable death in hospitalized patients1,2. This has long been recognized as a major public health challenge, with multiple organizations calling for increased awareness and thromboprophylaxis of patients3,4,5. Thromboprophylaxis is known to be safe and effective6, but numerous studies have shown that it is still misused or underused6,7,8,9.The first step in appropriate VTE prophylaxis involves identifying patients at risk for VTE. Prior guidelines recognized the burden of individual risk assessment and recommended a cohort-based approach to VTE prophylaxis5. However, these types of universal strategies have shown minimal impact on reducing VTE rates10,11. Contemporary guidelines emphasize the heterogeneity of hospitalized medical patients and recommend an individualized approach to risk assessment and prophylaxis12.
Multiple risk assessment models (RAMs) have been developed over the years to assist clinicians in risk stratifying patients. These RAMs are effective tools for identifying at-risk patients13, and some studies have shown that incorporating a RAM into the clinical workflow can reduce VTE events14,15. However, there are dozens of validated RAMs with variable risk predictors, making it difficult to determine which RAM a clinician should choose, and in which populations. An ideal RAM would be applicable to diverse patients and recognize that the risk of VTE can change over the course of a hospitalization. The RAM would be easy to use and consider both the risk of bleeding and clotting. These lofty goals make new technologies such as artificial intelligence (AI) and its subbranch, machine learning (ML), particularly promising in the field of VTE prevention. AI/ML is an area of computer science that trains computer algorithms to make predictions based on available data. An effective AI/ML tool would search the medical chart for relevant risk factors, weigh the risk of VTE as well as the risk of bleeding, alert the clinician when that risk changes, and assist the clinician in making a decision about appropriate VTE prophylaxis.
A recent systematic review and meta-analysis of AI/ML tools for VTE prevention showed overall high performance16, but few AI/ML-based models have been implemented in clinical settings17. More research is needed to understand the safe and effective implementation of AI/ML 17. Understanding stakeholder attitudes is an important part of the path to implementation. In this paper, we present two surveys, one directed at clinicians and the other at informaticians, to better understand their views on AI/ML in the field of VTE prevention and management.
Methods
Survey design
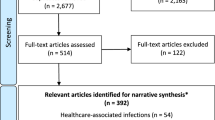
We conducted two cross-sectional electronic surveys about perceptions on the use of AI for VTE prevention among clinicians (Supplementary data 1) and among healthcare informaticians (Supplementary data 2). Both study instruments were designed and administered in REDCap, a secure web-based application18. Both were vetted by a multidisciplinary team with expertise in hematology, informatics, and public health, and refined for clarity, length, and relevance with a survey expert. They were individually approved by the Beth Israel Deaconess Medical Center IRB as exempt protocols and all research was performed in accordance with relevant guidelines and regulations. Informed consent was obtained at the start of each survey via a statement about the voluntary nature of the study.
We defined VTE as deep vein thrombosis (DVT) and/or pulmonary embolism (PE). We defined prophylaxis as including pharmacologic and/or mechanical measures for VTE prevention, and we used the terms prophylaxis and prevention interchangeably. In the healthcare informatician survey, we used the term “blood clot” instead of VTE because not all respondents may be familiar with the term VTE. We defined AI/ML as technologies that mimic human intelligence, and gave an example of technology using a large dataset to train a model that can predict outcomes or help make decisions. We used the terms AI and ML interchangeably.
The clinician survey explored attitudes and practices around VTE prevention, with a specific section exploring the use of AI/ML for VTE prevention (3 questions). We report the findings of that section here. The healthcare informatician survey explored attitudes and practices around AI/ML in healthcare in general, with a specific section on the use of AI/ML for VTE prevention (21 questions total). We report the findings of the survey in its entirety here.
Survey items included both quantitative and qualitative questions. Quantitative questions used Likert scales and Yes/No/Do not know responses. Several questions provided respondents with a field to write a free-text response. Both surveys asked respondents about general demographics such as age, sex, ethnicity, role, and time in practice (Supplementary data 1 and 2).
Respondents
The surveys were administered to targeted convenience samples between August 2021 and December 2022. Clinical respondents were recruited through social media, professional organizations, and program directors across the United States (US). Clinical trainees could opt to enter a raffle drawing for one of 100 $10 gift cards. There was no incentive provided for other groups. Healthcare informaticians were recruited through professional organizations and a publicly available database listing recipients of National Institutes of Health informatics grant awardees. Due to these methods of recruitment, a response rate could not be accurately calculated. As a descriptive survey utilizing a sample of convenience, we did not perform any a priori sample size calculations.
Analysis
We used descriptive statistics to present responses and respondent characteristics, summarizing data as proportions. Binomial 95% confidence intervals (CI) was included for primary outcomes. We used the chi square test to compare categorical responses between groups. We performed all analyses using SAS, version 9.4 (SAS Institute, Cary, NC, USA).
All clinicians were asked if AI/ML can help with VTE prevention in hospitalized patients; respondents who answered anything other than “definitely yes” were asked what concerns they have about AI/ML and provided a list of options derived from the literature, along with space to write a free-text response. Two researchers (BDL and RP) conducted a qualitative analysis of these answers to batch responses that matched existing categories and to categorize new themes derived from the data. All conflicts were settled by consensus.
All healthcare informaticians were asked if AI/ML can help with management of blood clots. Respondents who answered yes were asked what aspects of blood clot management AI/ML could be useful for. All respondents were asked about potential barriers and what else to consider when using AI/ML to assist with clinical management of blood clots. Two researchers (BDL and RP) conducted a qualitative analysis of these answers. All qualitative analysis for both surveys was done by reviewing responses, developing a codebook, and using the codebook to independently code all free text responses. Themes were derived from the data. Up to two codes were assigned to each response, and the researchers compared their codes and reached consensus for every response. All qualitative coding was completed with Microsoft Excel (Microsoft Corp., Seattle, WA, USA).
Results
Healthcare informatician—respondent characteristics
Of 101 respondents to the healthcare informatician survey, a majority were greater than 40 years old (54.5%), male (62.0%), and white (70.1%) (Table 1). Respondents could identify as more than one role; most were clinicians (44.6%), followed by data scientists (36.6%). Most respondents reported that they had been practicing in informatics for more than 10 years (54.5%).
Most felt they were very well informed (41.6%) or sufficiently informed (48.5%) about AI/ML, with a majority reporting that they had taken coursework on the topic (61.4%) or were doing research on the topic (68.3%). A large portion also reported that they had worked on deploying AI/ML (42.6%).
Clinician survey—respondent characteristics
Of 607 US-based respondents to the clinician survey, a majority were 40 years old or younger (69.9%), female (55.7%), and white (68.2%) (Table 2). Physicians made up 70.7% of respondents, of which 45.4% were trainees. Hospital medicine was the most common specialty (52.1%) followed by hematology (20.8%). A majority of respondents (65.8%) reported making a decision about whether a patient needs VTE prophylaxis every day. Only 20.5% of respondents reported that they had used AI/ML to inform their clinical practice; a majority had not (57.9%) or were unsure (21.6%).
Healthcare informatician—experiences with AI/ML
Most informaticians (62.6%) reported that their organization is using or developing AI/ML for healthcare. Of these 62 respondents, a majority described the status of AI/ML at their organization as implemented with at least one model in use (82.3%), and that their organizations primarily develop the models themselves (81.4%). Less than half (45.8%) reported using third-party vendors or partnering with local universities (28.8%).
Respondents who reported developing AI/ML systems used Python (76.6%), R (45.3%), and toolkits (42.2%). Of the respondents who described what toolkit they prefer, the most commonly cited ones were Scikit-learn and TensorFlow.
Healthcare informatician—attitudes towards AI/ML
A majority of informaticians agreed that AI/ML can have a positive impact on the care of patients (95.0%), can help healthcare organizations meet regulatory requirements (95.0%), and can have a positive economic impact on their healthcare organization (81.0%) (Fig. 1, Supplementary Table 1). Informaticians mostly agreed that AI/ML has the potential to perform better than humans (76.3%) and will replace human employees in some jobs (60.4%). Respondents found AI/ML to be overall reliable (58.5%) and would trust their own care to an AI/ML system (49.5%). However, less than half would trust a closed proprietary system (39.7%). Most informaticians agreed that AI/ML should be independently vetted and standardized prior to use in a clinical setting (96.0%), regulated (95.6%), and evaluated in randomized controlled trials (81.2%).
The three most common reasons respondents identified as barriers to the successful development of AI/ML in healthcare were data quality (67.3%), lack of standardization (39.8%), and difficulty of acceptance by healthcare providers (35.7%).
Healthcare informatician—attitudes towards AI/ML for the management of blood clots
A majority of informaticians agreed that AI/ML can be used for clinical management of blood clots (56.0% 95% CI 46–66%). Of these 56 respondents, most agreed that AI/ML can be used for risk stratification (94.6%), radiologic accuracy (87.5%), surveillance (80.4%), diagnosis (73.2%), and treatment (73.2%) (Fig. 2). Four respondents proposed potential additional uses for AI/ML: monitoring the process of clot dissolution, warfarin dosing, shared decision-making, and treatment during acute versus chronic recovery phases. All respondents were asked about perceived barriers, and the most commonly cited barriers were a lack of transparency with AI/ML systems (48.5%), concern that clinicians would not use an AI/ML system (34.7%), and concerns around liability (24.8%) (Supplementary Table 2). Informaticians who identified as clinicians were more likely to think that AI can help with VTE compared to those who did not identify as clinicians, though the difference was not statistically significant (66.7% vs. 47.3%, respectively; p = 0.052). Respondents at organizations that have implemented AI were not significantly more likely to think that AI can help with VTE compared to those at organizations that had not implemented AI (59.0% vs. 48.7%; p = 0.32).
All respondents were asked the free-text question, “What else should be considered when using AI/ML to assist in the clinical management of blood clots?” There were 37 responses, six of which were removed from analysis because they did not answer the questions. Of the remaining 31 responses, nearly all were related to validation of the system and discussed factors related to testing, bias, and transparency. Several responses discussed deployment, and a few responses touched on the importance of clinician oversight (themes in Table 3; coding tree in Supplementary Table 3).
Clinician attitudes towards AI/ML for the management of blood clots
Most respondents (70.1%, 95% CI: 66.6–73.6) believed that AI/ML probably or definitely can help with VTE prevention. Respondents who had used AI in clinical practice were more likely to agree that AI can help (RR: 1.45, 95% CI: 1.33–1.58) compared to non-AI users. Respondent age and physician training status were not associated with the belief that AI can help (both p ≥ 0.05).
Respondents who answered anything other than “definitely yes” to whether AI/ML can help with VTE prevention were asked about their concerns. The three most common concerns were a lack of transparency (25.4%), that AI/ML is not ready for clinical use (25.0%), and that AI/ML is not accurate enough (22.7%). Seventy respondents provided free-text responses. A total of 34 comments were removed (16 responses were removed for comments such as “I don’t have enough knowledge in this area,” 13 responses were removed for comments such as “I have no concerns,” and 5 responses were removed for comments requesting more information about a specific AI/ML system.) The remaining 36 comments were categorized into the following themes: the importance of clinical judgment, concerns around how the AI/ML system is validated, and concerns around deployment of the system and the possibility of technology fatigue (themes in Table 4; coding tree in Supplementary Table 4).
Discussion
Although informaticians expressed concern that clinicians would not be willing to use AI/ML, a majority of clinician respondents in our survey believed that AI/ML can be helpful in the field of VTE prevention and management. This is consistent with surveys evaluating clinician attitudes towards AI/ML in other specialties; generally, clinicians have reported that AI/ML will have a positive impact on their field19,20,21. Surveys have found that some specialists may be less likely to perceive benefits from AI/ML22. As AI/ML technology advances and becomes more accessible, further research into clinician and other stakeholder views is critical in order to understand how AI/ML can positively and safely impact care.
Both clinicians and informaticians cited transparency as their number one concern when considering AI/ML systems for the management of blood clots. Though transparency has been cited as a barrier in other clinician surveys, it was not the main concern. As AI/ML moves closer to the bedside, concerns around the “black box” nature of AI/ML may increase. In a landmark paper from 2017, Doshi-Velez and Kim discuss how different measures of success have emerged as AI/ML becomes more ubiquitous23. Initially, models were optimized for performance, but now there are efforts to optimize models for other important criteria such as safety and nondiscrimination. In order to evaluate for and reinforce these criteria, experts have called for increased interpretability of AI/ML. Doshi-Velez and Kim define interpretability as “the ability to explain or to present in understandable terms to a human” and discuss how interpretability can allow humans to learn, ensure the model is safe and ethical, and weigh competing objectives23. These factors may be particularly important in the field of medicine, where care needs to be personalized not only to each individual’s health history, but also to their values and preferences. Interpretability may allow clinicians to readily weigh their own clinical judgment, a factor that both clinicians and informaticians identified as important. Efforts are being made to further define what it means for AI/ML systems to be interpretable, and how that can be technically accomplished24.
Both informaticians and clinicians discussed the importance of how AI/ML systems are validated and deployed, touching on subjects such as the quality of electronic health record data, whether the system can be applied to patient populations other than which it was trained , how to avoid perpetuating bias, and how the system will fit into the clinical workflow. Organizations are working to define standards for how AI/ML studies report their data and how these models might be evaluated in clinical trials25,26. Leaders also recognize the numerous factors that need to be addressed before AI/ML is brought to the bedside including safety, ethical, and security considerations27,28,29, and guidelines are being developed to support healthcare organizations looking to deploy these systems30.
When asked about potential concerns around the use of AI/ML in VTE prevention, several clinicians shared that they did not know enough about the field of AI/ML to comment. This self-identified knowledge gap has been voiced in other studies20, and some experts argue that clinicians will need to learn more about the field given AI/ML’s inevitable arrival in healthcare31. Clinicians will be needed to serve as peer reviewers and clinical trial leaders, as well as to make the ultimate decision as to whether a new system has a clinically relevant impact on their patients31. While clinicians cannot be expected to become experts in every aspect of medicine, it is clear that we will need leaders in this area in order to ensure that AI/ML enters healthcare in a safe, clinically effective, and ethical manner.
There are several limitations to our study. We used online platforms such as message boards and social media websites for survey distribution, which allowed for wide dissemination but did not allow for an accurate response rate calculation, which can underestimate or obscure sampling bias. Given participation was voluntary, the respondents who elected to participate may be more comfortable with technology and more likely to view AI/ML positively. The majority of clinician respondents were younger than 40 years old, and while these findings may reflect the views of a new generation of practitioners, they may not reflect the views of older clinicians in leadership roles who have the ability to effect change today. We used broad terms such as "blood clot” and “AI/ML” in our surveys in order to assess general attitudes and account for respondents who may not have a clinical or technical background, respectively. Several respondents commented on the difficulty of assessing these broad fields, and further research will need to be done evaluating specific algorithms in specific clinical contexts. Additionally, further studies evaluating the opinions and preferences of patients will need to be done21.
Conclusion
A majority of clinicians and healthcare informaticians believe AI/ML can help with VTE management. Both groups raised concerns around how the AI/ML system is validated, how the system is ultimately deployed in the clinical setting, and the importance of clinical judgment. Further studies of specific AI/ML systems are needed to understand how they can impact clinical care.
Data availability
Data is available upon request; researchers interested in reviewing our data should contact Rushad Patell at rpatell@bidmc.harvard.edu.
References
Shahi, A. et al. The incidence and economic burden of in-hospital venous thromboembolism in the United States. J. Arthroplasty 32(4), 1063–1066. https://doi.org/10.1016/j.arth.2016.10.020 (2017).
Smith, S. B. et al. Analysis of national trends in admissions for pulmonary embolism. Chest 150(1), 35–45. https://doi.org/10.1016/j.chest.2016.02.638 (2016).
Day ISCfWT. Thrombosis: A major contributor to global disease burden. Thromb. Res. 134(5), 931–938 https://doi.org/10.1016/j.thromres.2014.08.014 (2014).
Bergmann, J. F. & Kher, A. Venous thromboembolism in the medically ill patient: A call to action. Int. J. Clin. Pract. 59(5), 555–561. https://doi.org/10.1111/j.1368-5031.2005.00529.x (2005).
Geerts, W. H. et al. Prevention of venous thromboembolism: American College of Chest Physicians evidence-based clinical practice guidelines (8th edition). Chest 133(6 Suppl), 381S-453S. https://doi.org/10.1378/chest.08-0656 (2008).
Kahn, S. R. et al. Multicenter evaluation of the use of venous thromboembolism prophylaxis in acutely ill medical patients in Canada. Thromb. Res. 119(2), 145–155. https://doi.org/10.1016/j.thromres.2006.01.011 (2007).
Cohen, A. T. et al. Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): A multinational cross-sectional study. Lancet 371(9610), 387–394. https://doi.org/10.1016/S0140-6736(08)60202-0 (2008).
Deheinzelin, D. et al. Incorrect use of thromboprophylaxis for venous thromboembolism in medical and surgical patients: Results of a multicentric, observational and cross-sectional study in Brazil. J. Thromb. Haemost. 4(6), 1266–1270. https://doi.org/10.1111/j.1538-7836.2006.01981.x (2006).
Forgo, G. et al. An update on the global use of risk assessment models and thromboprophylaxis in hospitalized patients with medical illnesses from the World Thrombosis Day steering committee: Systematic review and meta-analysis. J. Thromb. Haemost. 20(2), 409–421. https://doi.org/10.1111/jth.15607 (2022).
Flanders, S. A. et al. Hospital performance for pharmacologic venous thromboembolism prophylaxis and rate of venous thromboembolism: A cohort study. JAMA Intern. Med. 174(10), 1577–1584. https://doi.org/10.1001/jamainternmed.2014.3384 (2014).
Mahan, C. E. et al. Thromboprophylaxis patterns, risk factors, and outcomes of care in the medically ill patient population. Thromb. Res. 132(5), 520–526. https://doi.org/10.1016/j.thromres.2013.08.013 (2013).
Schünemann, H. J. et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: Prophylaxis for hospitalized and nonhospitalized medical patients. Blood Adv. 2(22), 3198–3225. https://doi.org/10.1182/bloodadvances.2018022954 (2018).
Zhou, H. et al. Assessment of the risk of venous thromboembolism in medical inpatients using the Padua prediction score and Caprini risk assessment model. J. Atheroscler. Thromb. 25(11), 1091–1104. https://doi.org/10.5551/jat.43653 (2018).
Cassidy, M. R., Rosenkranz, P. & McAneny, D. Reducing postoperative venous thromboembolism complications with a standardized risk-stratified prophylaxis protocol and mobilization program. J. Am. Coll. Surg. 218(6), 1095–1104. https://doi.org/10.1016/j.jamcollsurg.2013.12.061 (2014).
Catterick, D. & Hunt, B. J. Impact of the national venous thromboembolism risk assessment tool in secondary care in England: Retrospective population-based database study. Blood Coagul. Fibrinol. 25(6), 571–576. https://doi.org/10.1097/MBC.0000000000000100 (2014).
Wang, Q., Yuan, L., Ding, X. & Zhou, Z. Prediction and diagnosis of venous thromboembolism using artificial intelligence approaches: A systematic review and meta-analysis. Clin. Appl. Thromb. Hemost. 27, 10760296211021162. https://doi.org/10.1177/10760296211021162 (2021).
Topol, E. J. High-performance medicine: The convergence of human and artificial intelligence. Nat. Med. 25(1), 44–56. https://doi.org/10.1038/s41591-018-0300-7 (2019).
Harris, P. A. et al. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 42(2), 377–381. https://doi.org/10.1016/j.jbi.2008.08.010 (2009).
Scheetz, J. et al. A survey of clinicians on the use of artificial intelligence in ophthalmology, dermatology, radiology and radiation oncology. Sci. Rep. 11(1), 5193. https://doi.org/10.1038/s41598-021-84698-5 (2021).
Waymel, Q., Badr, S., Demondion, X., Cotten, A. & Jacques, T. Impact of the rise of artificial intelligence in radiology: What do radiologists think?. Diagn. Interv. Imaging 100(6), 327–336. https://doi.org/10.1016/j.diii.2019.03.015 (2019).
Bhandari, A., Purchuri, S. N., Sharma, C., Ibrahim, M. & Prior, M. Knowledge and attitudes towards artificial intelligence in imaging: A look at the quantitative survey literature. Clin. Imaging 80, 413–419. https://doi.org/10.1016/j.clinimag.2021.08.004 (2021).
Doraiswamy, P. M., Blease, C. & Bodner, K. Artificial intelligence and the future of psychiatry: Insights from a global physician survey. Artif. Intell. Med. 102, 101753. https://doi.org/10.1016/j.artmed.2019.101753 (2020).
Finale Doshi-Velez, B.K. Towards a Rigorous Science of Interpretable Machine Learning. arXiv (2017).
Markus, A. F., Kors, J. A. & Rijnbeek, P. R. The role of explainability in creating trustworthy artificial intelligence for health care: A comprehensive survey of the terminology, design choices, and evaluation strategies. J. Biomed. Inform. 113, 103655. https://doi.org/10.1016/j.jbi.2020.103655 (2021).
Ibrahim, H. et al. Reporting guidelines for clinical trials of artificial intelligence interventions: The SPIRIT-AI and CONSORT-AI guidelines. Trials 22(1), 11. https://doi.org/10.1186/s13063-020-04951-6 (2021).
Collins, G. S. et al. Protocol for development of a reporting guideline (TRIPOD-AI) and risk of bias tool (PROBAST-AI) for diagnostic and prognostic prediction model studies based on artificial intelligence. BMJ Open 11(7), e048008. https://doi.org/10.1136/bmjopen-2020-048008 (2021).
Cheng, J. Y., Abel, J. T., Balis, U. G. J., McClintock, D. S. & Pantanowitz, L. Challenges in the development, deployment, and regulation of artificial intelligence in anatomic pathology. Am. J. Pathol. 191(10), 1684–1692. https://doi.org/10.1016/j.ajpath.2020.10.018 (2021).
Ngiam, K. Y. & Khor, I. W. Big data and machine learning algorithms for health-care delivery. Lancet Oncol. 20(5), e262–e273. https://doi.org/10.1016/S1470-2045(19)30149-4 (2019).
He, M., Li, Z., Liu, C., Shi, D. & Tan, Z. Deployment of artificial intelligence in real-world practice: Opportunity and challenge. Asia Pac. J. Ophthalmol. (Phila) 9(4), 299–307. https://doi.org/10.1097/APO.0000000000000301 (2020).
Scott, I., Carter, S. & Coiera, E. Clinician checklist for assessing suitability of machine learning applications in healthcare. BMJ Health Care Inform. https://doi.org/10.1136/bmjhci-2020-100251 (2021).
Quer, G., Arnaout, R. & Henne, M. Machine learning and the future of cardiovascular care: JACC state-of-the-art review. J. Am. Coll. Cardiol. 77(3), 300–313. https://doi.org/10.1016/j.jacc.2020.11.030 (2021).
Acknowledgements
The authors would like to thank Dr. Deirdra Terrell, PhD for her expertise in reviewing the survey instruments.
Author information
Authors and Affiliations
Contributions
BDL, WR, RPR, LL, AA, NR, KA, ISV, JIZ, and RP contributed to the conception/design of the study. BDL, WR, LL, SD, PE, and RP were involved in data acquisition. BDL, LED, and SZ were involved in analysis/interpretation of the data. All authors were involved in manuscript writing and/or critically reviewing the manuscript and approving the final version for submission.
Corresponding author
Ethics declarations
Competing interests
Funding source: This study was supported by the Centers for Disease Control and Prevention (CDC), Atlanta, GA USA Cooperative Agreement #DD20-2002. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. Rachel P. Rosovsky, MD, MPH has received research funding from Bristol Myers Squibb and Janssen; consultancy/advisory board participation with Abbott, Bristol Myers Squibb, Janssen, Inari, and Penumbra. Jeffrey I. Zwicker, MD has received research funding from Incyte, Quercegen, and the National Heart, Lung, and Blood Institute; provided consultancy services to Sanofi, CSL, and Parexel; and received honoraria from/advisory board participation with Pfizer/Bristol Myers Squibb, Portola, Daiichi. All other authors report no conflicts of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lam, B.D., Dodge, L.E., Zerbey, S. et al. The potential use of artificial intelligence for venous thromboembolism prophylaxis and management: clinician and healthcare informatician perspectives. Sci Rep 14, 12010 (2024). https://doi.org/10.1038/s41598-024-62535-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-62535-9
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.