Abstract
The relationship between the Systemic Inflammatory Response Index (SIRI) and the Fibrinogen-to-albumin ratio (FAR) has not been extensively investigated. The objective of this study was to determine the independent relationship between FAR and SIRI in people with osteoporotic fractures (OPF). A cross-sectional study was conducted using retrospective data from 3431 hospitalized OPF patients. The exposure variable in this study was the baseline FAR, while the outcome variable was the SIRI. Covariates, including age, gender, BMI, and other clinical and laboratory factors, were adjusted. Cross-correlation analysis and linear regression models were applied. The generalized additive model (GAM) investigated non-linear relationships. Adjusted analysis revealed an independent negative association between FAR and SIRI in OPF patients (β = − 0.114, p = 0.00064, 95% CI − 0.180, − 0.049). A substantial U-shaped association between FAR and SIRI was shown using GAM analysis (p < 0.001). FAR and SIRI indicated a negative association for FAR below 6.344% and a positive correlation for FAR over 6.344%. The results of our study revealed a U-shaped relationship between SIRI and FAR. The lowest conceivable FAR for a bone-loose inflammatory disease might be 6.344%, suggesting that this has particular significance for the medical diagnosis and therapy of persons with OPF. Consequently, the term "inflammatory trough" is proposed. These results offer fresh perspectives on controlling inflammation in individuals with OPF and preventing inflammatory osteoporosis.
Similar content being viewed by others
Introduction
Osteoporosis (OP) is a common bone condition that significantly affects the health and quality of life of individuals worldwide1. On a global scale, OP impacts around 200 million individuals2. According to a 2019 study, the prevalence of OP in Chinese women and men over 50 years was as high as 29.13% and 6.46%, respectively3. Research on reducing the prevalence and determining the causes of OP has become a crucial focus in public health. Researchers have recently shifted their focus towards the crucial role that inflammation plays in the development and origin of OP. There is a strong connection between OP risk and inflammation. Chronic inflammation can potentially raise the risk of both OP and fractures4.
Two recently proposed measures of systemic inflammation are the Fibrinogen-to-albumin ratio (FAR) and the Systemic Inflammatory Response Index (SIRI)5,6. The FAR assesses coagulation and inflammatory status by evaluating the fibrinogen-to-albumin ratio, whereas SIRI evaluates systemic inflammation by considering the ratio of platelets, neutrophils, and lymphocytes7,8. When assessing systemic inflammation and forecasting the prognosis of a disease, the FAR and SIRI are highly relevant and useful9,10. They provide physicians with essential information on the inflammatory status and prognosis of their patients, which aids in the decision-making process about treatment and disease progression. When compared to recognized inflammatory markers, the FAR and SIRI exhibit more therapeutic potential and predictive value11. They provide a more thorough representation of systemic inflammation and more precise recommendations for illness prevention, diagnosis, and therapy at an early stage.
These two are widely used inflammatory markers that have been widely applied in determining inflammatory status and predicting illness outcomes5,6. Nevertheless, there is still additional knowledge to be gained regarding the potential correlation between baseline FAR and SIRI in individuals who have experienced osteoporotic fractures (OPF). This study aims to examine the existing correlation between the indicators of SIRI and FAR to enhance our understanding of their clinical significance and potential applications. It is worth noting that there is a lack of research on the evaluation of these indicators and their predictive capabilities for prognosis.
Materials and methods
Study design and participants
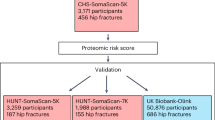
The patient data included in this retrospective study was collected from January 2015 to March 2022. The medical records of patients were acquired from Kunshan Hospital, an institution associated with Jiangsu University in Suzhou, China. The study comprised 3431 OPF patients in total. During their hospital stay, medical blood tests were performed on each of them. OPFs, sometimes referred to as fragility fractures, are low-energy fractures that happen when someone falls from a height of standing or less. They have the potential to significantly raise the risk of further fragility fractures12. The presence of OP and the concurrent absence of other metabolic bone disorders are prerequisites for the diagnosis of OPFs. The following were the inclusion criteria for OP: (1) the diagnosis of OP based on a T-Score of − 2.5 or lower, even in the absence of significant bone fractures; and (2) the incidence of bone instability and fractures without other metabolic bone illnesses, accompanied by physiological bone density (T-Score)13. The following patients have been eliminated from consideration: (1) those who had acute infections that impacted the Fibrinogen-to-albumin ratio level (n = 2); (2) those who had missing FAR data (n = 103); and (3) those who had missing SIRI data (n = 22). A total of 3431 patients all met the study's inclusion criteria after the application of the criteria. Figure 1 shows a schematic diagram of the patient selection procedure. The study adheres to the Helsinki Declaration and received approval from the Kunshan Hospital Ethics Committee at Jiangsu University (Approval No. 2021-06-016-K01). The patients' identities were concealed to facilitate an impartial investigation. Each patient provided written informed consent.
Outcome variables
The measurements were obtained from the initial fasting blood sample collected within 24 h of admission, using the same device and routine operating procedure, by trained operators. The formula used to calculate SIRI, which was the dependent variable in our investigation, was SIRI = neutrophil count × monocyte count ÷ lymphocyte count14. The Sysmex XN-10 (B4) hematology analyzer was used to measure the number of neutrophils, monocytes, and lymphocytes using nuclear staining and flow cytometry assays.
Exposure variables
In this investigation, the exposure variable was FAR, which was computed as follows: FAR (%) = FIB (g/L)/ALB (g/L) × 100%15. The calculation of the FAR involved dividing the concentrations of fibrinogen and albumin for each patient. The fibrinogen concentrations were quantified through coagulation analysis utilizing the CN-6000 automated coagulation analyzer, while the albumin concentrations were assessed using the Beckman AU5800 biochemical analyzer pipeline using biuret analysis.
Covariates
The variables in the study included age, gender, body mass index (BMI), American Society of Anesthesiologists (ASA) score, calcium, urea nitrogen (UN), creatinine (Cr), uric acid (UA), aspartate aminotransferase (AST), and parathyroid hormone (PTH). Upon admission to the hospital, all clinical variables were measured within 3 days.
Statistics
For continuous and categorical variables, the results are displayed as means ± standard deviations (SDs), median (Q1, Q3), and frequency (%), accordingly. For univariate data measured in absolute values, either Fisher's exact test or Pearson's chi-squared test were utilized. The t-test was employed for continuous variables in standard data, whereas the Mann–Whitney U test was utilized for non-normally distributed continuous data. A univariate linear regression analysis was conducted to evaluate the correlation between the FAR and SIRI in patients with OPF.
The study analyzed patients with OPF to determine if there was a direct relationship between FAR and SIRI. This was done using the generalized estimation equation (GEE) with proper adjustment for covariables. The models that were generated were completely calibrated (model 3/4), partially calibrated (model 2), and not calibrated (model 1). The following criteria were used to determine how these covariates should be adjusted when the collinearity of the covariances was first detected using variance infection factor analysis: Covariates that meet criteria 1 or indicated covariates of P < 0.1 in the univariate model; (1) a change of matching odds ratio (OR) of ≥ 10% was detected when covariates were added to the basic model or removed from the entire model16. Standard 1 and Standard 2 were used to alter Model 3 and Model 4, respectively. Finally, four models were determined: model 1 was not calibrated; Model 2 (partially calibrated) was modified based on factors, such as age, gender, BMI, ASA level; Model 3 is adjusted according to age, gender, BMI, ASA level and UA, Cr, UN, AST; Model 4 was modified based on factors, such as age, gender, BMI, ASA, UA, Cr, UN, AST, PTH, and calcium.
The detection of potential non-linear relationships was performed using a generalized additive model (GAM). A two-piecewise linear regression model was used to identify threshold effects in the smoothing curves when there were significant relationships. An algorithmic approach utilizing a maximum likelihood model was used to recursively calculate the inflection point for these unique ratio curves17. After classifying patients according to specific covariates, we conducted additional studies to evaluate the reliability of the findings and to compare the variations across different groups of patients. The examination of subgroup interactions and modifications was conducted using the likelihood ratio test (LRT).
Empower Stats (www.empowerstats.com, X&Y Solutions, Inc., Boston, MA, USA) was used for all statistical analyses. Additionally, R 3.6.3 (http://www.r-project.org) was utilized. P-values were considered statistically significant if they were less than 0.05.
Ethics approval and consent to participate
We received ethical approval from the Affiliated Kunshan Hospital of Jiangsu University (approval No. 2021-06-015-K01), and was compliant with the Declaration of Helsinki. Patient identification data were hidden from the researchers analyzing the data. The patients signed informed consent.
Results
Patient characteristics
Table 1 summarizes the baseline characteristics of 3431 patients with OPF who were admitted between January 2015 and March 2022 and were placed within the specified FAR quartiles. The mean age of these patients (31.97% male, 68.03% female) was 69.62 ± 11.80 years. The average FAR was 4.54 ± 1.01, and the average SIRI was 3.44 ± 3.74. Based on FAR (< 5.5875%, 5.5875–6.8018%, 6.8018–8.4130%, 6.4130–19.4871%), patients were grouped into quartiles. SIRI, UA, Cr, UN, AST, PTH, calcium, FEE, MAP, BTX, P1NP, and LDL showed significant differences.
Univariate analyses of SIRI-related factors
Significant correlations between SIRI and factors, such as gender, UA, Cr, UN, AST, PTH, calcium, BTX, P1NP, LDL, and FAR were found in the univariate analysis (Table 2).
Examining the relationship between SIRI and FAR levels
Subsequently, the correlation between FAR and SIRI in patients with OPF was examined using four different models (Table 3). A noteworthy correlation between these factors was noted in unadjusted Model 1 (β = − 0.141, 95% CI − 0.193, − 0.089, P < 0.000001). Adjusted Model 2, which included variables including age, gender, body mass index (BMI), and ASA, showed a similar association (β = − 0.140, 95% CI − 0.191, − 0.088, P < 0.000001). A significant negative connection was also shown by controlled Model 3, which further controlled for UA, CR, UN, and AST (β = − 0.125, 95% CI − 0.176, − 0.073, P < 0.000001). A similar relationship between these parameters was identified in Adjusted Model 4, which also included adjustments for PTH and calcium (β = − 0.114, 95% CI − 0.180, − 0.049, P = 0.00064).
In comparison to Q1, SIRI in Model 4 decreased by 1.037, 1.410, and 1.117 in Q2, Q3, and Q4, respectively. In Q4 and Q3, OP patients showed a statistically significant decline in SIRI across all four models.
Subgroup analyses were conducted to ensure the robustness of Model 4. OPF patients were classified according to age, gender, BMI, ASA, UA, Cr, UN, AST, PTH, and calcium. The findings were then adjusted for the parameters that were not used in stratification. As shown in Table S1, all layers were stable, and a relatively consistent pattern was observed in these data.
Analysis of thresholds and spline smoothing plots
Figure 2 demonstrates the estimated exposure–response curve for FAR and SIRI in OPF patients stratified by BMI status. Once age, gender, ASA, UA, Cr, UN, AST, PTH, and calcium were adjusted for, GAM analysis showed a non-linear connection between FAR and SIRI in patients with BMI < 24 kg/m2, BMI between 24–28 kg/m2, and BMI > 28 kg/m2 (LRT < 0.001, LRT < 0.001, LRT = 0.006) (Table 4). Among the OPF patients included, there was a threshold non-linear connection between FAR and SIRI. Segmented linear regression models were utilized to ascertain the inflection point (K values were 6.667%, 5.151%, and 9.323%). The effect size, 95% confidence interval, and P-value for OPF patients with a BMI of less than 24 kg/m2 were, respectively, − 1.086, − 1.345, − 0.826, and < 0.0001. On the right side of the inflection point, the effect magnitude, 95% CI, and P-value were, in order, 0.130, 0.013, − 0.246, and 0.0294. The effect size, 95% confidence interval, and P-value for OPF patients with BMIs ranging from 24 to 28 kg/m2 were, respectively, − 2.141, − 2.932, − 1.350, and < 0.0001 on the left side of the inflection point. The effect size, 95% CI, and P-value for the positive side of the inflection point were 0.048, − 0.088, − 0.183, and 0.4934, respectively. These values suggest that there is no significant association. For OPF patients with a BMI greater than 28 kg/m2, there was no significant correlation observed on the left side of the inflection point. The effect size, 95% CI, and P-value were − 0.141, − 0.329, − 0.046, and 0.1411, respectively. The effect size, 95% confidence interval, and P-value on the right side of the inflection point were, in that order, 0.325, 0.105, − 0.544, and 0.0043.
The relationship between FAR and SIRI. Adjusted smoothed curves corresponding to the relationship between FAR levels and SIRI. A generalized additive model revealed a thresholded non-linear relationship between FAR and SIRI in OPF patients. The upper and lower curves represent the range of the 95% confidence interval, and the middle curve represents the correlation between FAR and SIRI. Models were adjusted for age, gender, BMI, ASA, UA, Cr, UN, AST, PTH, and calcium. The red curve in Model 4 exhibited an inflection point (K) at 6.344%. FAR fibrinogen-to-albumin ratio, SIRI systemic inflammation response index, BMI body mass index, ASA American Society of Anesthesiologists, UA uric acid, Cr uric acid, UN uric acid, AST aspartate aminotransferase, PTH parathyroid hormone.
Discussion
Current research on inflammation and OP mostly focuses on the cellular level, uncovering several regulatory patterns and interactions between mediators of inflammation and osteoblasts and osteoclasts18. Using SIRI and FAR, two inflammatory markers, we performed a retrospective cross-sectional study in a group of OPF patients. Examining the correlation between FAR and SIRI in OPF patients was the aim of the study. For the first time, our results showed a non-linear relationship between FAR and SIRI in the OPF population of the Kunshan region of China. The study investigated the relationship between FAR and SIRI in detail using cross-sectional analysis and retrospective data from 3431 OPF patients. Following adjustments, the analysis showed that FAR and SIRI had a U-shaped association. A rise in FAR has a negative correlation with SIRI when it is less than 6.344%, with an impact size of − 1.062 (95% confidence interval − 1.287 to − 0.837, P < 0.0001). On the other hand, FAR exhibits a positive correlation with SIRI when it is more than 6.344%, with an effect size of 0.125 (95% confidence interval 0.041 to 0.210, P =0.0035). This discovery adds to our understanding of the mechanisms underlying the inflammatory response and offers a fresh viewpoint.
The few research that have examined the relationship between FAR levels and SIRI have not found one. The majority of prior research has looked at the prognostic implications and survival rates of various cancers concerning these two inflammatory markers independently; very few studies have examined the interaction between these two markers19,20,21. FAR is a blood biomarker used for prognostic and inflammatory assessment, as previous research has shown22. Many disease scenarios have been thoroughly examined and applied, such as COVID-19, cardiac issues, pancreatic cancer, hepatocellular carcinoma, bladder cancer, and newborn sepsis. The severity of the disease, patient survival rates, and prognostic indicators have all been connected to the FAR level23. The liver produces fibrinogen (FIB), a serum glycoprotein with a dimeric molecular structure that is essential to the physiology and pathology of inflammation and coagulation24. Fibrinogen production undergoes rapid upregulation during the acute phase of inflammation, encompassing bacterial infections, severe trauma, and surgical procedures25. Furthermore, there is a correlation between increased levels of plasma fibrinogen and persistent low-grade inflammation, platelet activation, greater production of adhesion molecules, stimulation of angiogenesis, and heightened infiltration of macrophages26. The liver produces albumin, which plays a significant role in both the acute inflammatory response and preserving plasma colloid osmotic pressure27. Nutritional and inflammatory circumstances affect its potential for synthesis28. Hypoalbuminemia is thought to be mostly caused by inflammation and malnutrition29. Elevated serum albumin levels inhibit the expression of vascular cell adhesion molecule-1, enhance the elimination of reactive oxygen species, and reduce inflammatory responses and endothelial cell death. The data suggest that albumin acts as an antioxidant and anti-inflammatory agent30. The physiological characteristics of serum albumin include anti-inflammatory, antioxidant, anticoagulant, antiplatelet aggregation, and capillary membrane stability maintenance31. SIRI represents the immune system's response to infection and invasive microorganisms32. This inflammatory index describes the immunological defense system, which comprises neutrophils, monocytes, and lymphocytes. SIRI serves as a prevalent prognostic and assessment indicator for several diseases. It has been extensively utilized in the management of acute pancreatitis, cardiovascular diseases, cancer, and stroke, among various other medical disorders. Physicians can assess a patient's inflammatory state and administer appropriate treatment based on anticipated clinical outcomes by monitoring alterations in the SIRI. Studies have demonstrated that SIRI is a separate predictor of outcome for patients with hepatoblastoma receiving neoadjuvant chemotherapy; the group with high SIRI had a significantly poorer 5-year overall survival than the group with low SIRI33. SIRI and other indicators are included in prognosis models for lower 5-year overall patients, which show great accuracy and reliability and allow prognostic risk assessment in these patients.
The liver responds to inflammation in its early stages by producing albumin, which has anti-inflammatory qualities and aids in the stability of capillary membranes34. Serum albumin levels consequently see a brief rise. Fibrinogen and serum albumin have a negative correlation27, and fibrinogen levels do not rise or slightly fall temporarily. As a result, FAR is decreased in the initial stages of inflammation. Lymphocytes migrate to the site of inflammation from the bloodstream as a result of the release of inflammatory cytokines and the actions of inflammatory mediators. Consequently, lymphocytes tend to decrease in number during the initial phases of inflammation35. This migratory process may cause the blood's lymphocyte numbers to momentarily drop, which would cause a brief rise in SIRI. Therefore, when FAR is less than 6.344% in the early phases of inflammation, there is a negative association between FAR and SIRI. Serum albumin levels dramatically drop in the ultimate stage of inflammation. This results in decreased albumin synthesis or increased loss and is caused by prolonged inflammatory activation and metabolic alterations36. Moreover, inflammation may enhance vascular permeability, which may facilitate albumin loss and leakage37. As a result, the level of plasma albumin may decrease even further during advanced stages of inflammation. Hypoalbuminemia in late-stage inflammation leads to an increase in the production of lipoproteins and procoagulant factors such as factor V, factor VIII, and fibrinogen as a compensatory reaction, due to the negative association between serum albumin and fibrinogen. As a result, hyperlipidemia occurs, leading to an increased risk of blood clotting due to considerably raised levels of fibrinogen27,38. FAR is hence raised in late-stage inflammatory conditions. White blood cell counts, especially those of neutrophils, usually rise in the latter stages of inflammation39. As a component of the immune system, WBCs are primarily responsible for recognizing and getting rid of infections, cleaning up injured tissue, and controlling the inflammatory response40. When inflammation arises, the bloodstream carries WBCs to the inflammatory site, where they contribute to tissue repair and the regulation of the inflammatory response41. WBCs are drawn to the area of inflammation by the release of inflammatory mediators including chemokines and cytokines, which cause the circulation to diverge42. White blood cells penetrate the inflammatory region by adhering to endothelial cells and navigating the artery wall43. In response to inflammatory stimuli, hematopoietic stem cells and precursor cells in the bone marrow can proliferate and develop to produce more WBC, including neutrophils, lymphocytes, monocytes, etc.44. SIRI significantly rises as a result of this. Consequently, FAR is positively connected with SIRI in the late stage of inflammation, when FAR is greater than 6.344%. Systemic inflammation and fibrinogen have been found to positively correlate in previous research, whereas albumin and systemic inflammation have been found to negatively correlate45. As a result, while FAR is strongly associated with systemic inflammation and SIRI measures the extent of systemic inflammation, additional evidence supports the direct correlation between FAR and SIRI in advanced stages of inflammation.
One of the main factors contributing to the development of OP is inflammation. Serum levels of IL-1β, IL-6, and F-I type collagen N-terminal peptide (NTx) were found to be considerably higher in postmenopausal women with OP compared to the control group in a study conducted by Al-Daghri and colleagues46. These investigations have shown that inflammation, which is controlled by patterns of cytokines, plays a crucial role in the development and progression of OP. Persistent systemic inflammation increases the probability of acquiring many diseases, such as periodontal and cardiovascular conditions. Chronic inflammation has been linked to several elements essential to bone physiology and may be a risk factor for OP, according to a study by several scientists47. Important inflammatory mediators such as IL-1, IL-6, and tumor necrosis factor-alpha (TNF-α) are secreted by a variety of cells, including neutrophils and macrophages. The primary factors that activate osteoclasts are TNF-α and IL-1, although IL-6 works in concert with other factors that promote bone48. Furthermore, a negative connection was noted by Ganesan et al. between bone mineral density (BMD) and high-sensitivity C-reactive protein (hs-CRP), which is produced by IL-649. In addition, they proposed a correlation between OP and inflammation. Additionally, hs-CRP levels and BMD were reported to be negatively correlated by Koh et al.49. The expanding body of evidence that supports the association between inflammation and OP is bolstered by these findings. Consequently, by employing two novel inflammation indicators, FAR and SIRI, we are capable of assessing the levels of systemic inflammation within a specific population and implementing timely measures to mitigate the likelihood of OP. The body is in the early stages of inflammation and needs prompt intervention to lower inflammation levels and avoid inflammatory OP when FAR is less than 6.344% and SIRI is higher.
This is the first study of its kind in China to investigate the independent correlation between the SIRI and FAR of an OPF individual. Our research might have immediate implications for clinical practice. One potential implication of the observed nonlinear correlation between FAR and SIRI is that elevated FAR levels should be considered in the assessment of inflammatory markers, in addition to elevated SIRI levels. Assessing the progression of inflammation is dependent upon this critical marker. Early-stage inflammation is suggested when SIRI is high and FAR is less than 6.344%. Inflammation occurs either in the chronic or terminal state when FAR is more than 6.344% and SIRI is high. Considering these conditions, we propose the concept of an "inflammatory trough," which denotes the stage at which patients with OPF are expected to encounter the least amount of inflammation, as indicated by a FAR of 6.344%. Understanding this particular facet has significant implications for the medical diagnosis and treatment of patients with OPF. These markers could also be included in the clinical evaluation of patients' OPF risk prediction50. Moreover, this finding provides direction for clinical interventions that attempt to mitigate inflammation in patients with osteoporosis. Additionally, it can aid in the development of clinical procedures and treatment protocols that are appropriate for specific OP patients.
This analysis contains several limitations. Firstly, as this was a retrospective cross-sectional study, there is no evidence of a causal relationship between FAR and SIRI. Furthermore, even though several covariates were considered, only the association between FAR and SIRI was investigated, meaning that residual confounding variables such as the effects of medication cannot be completely excluded from the research. Further planned and stratified cohort studies, appropriate control groups, and confounding factor accounting are needed to further understand the relationship between FAR and SIRI. Third, because of the single-center design and very small sample size, it was not possible to extrapolate the findings to other ethnic groups. This study highlights the need for more research using big studies that involve people of varied ethnicities, multi-center RCTs, and other biochemical indicators to better assure the reliability of these study results.
Conclusion
In summary, the results of our investigation indicate that there is a U-shaped relationship between FAR and SIRI in people with OPFs. When FAR is less than 6.344%, there is a negative correlation between FAR and SIRI. Conversely, when FAR exceeds 6.344%, there is a positive correlation between FAR and SIRI. Thus, in the context of diagnosing and treating OP patients, we propose the concept of an "inflammatory trough," which is the lowest inflammatory state that is likely to be observed in OPF patients with a FAR of 6.344%. The findings enable the early identification of people who may be at risk for OP and allow early preventive actions to be implemented to lower the risk of OP. However, additional follow-up studies involving a larger patient population would be required to validate these findings.
Data availability
Data is provided within the manuscript or supplementary information files.
References
Chen, Y., Bai, R., Chen, W., Li, S. & Jiang, Y. Zhuang-gu-fang treats osteoporosis in ovariectomized rats by increasing the osteogenesis-related factors leptin, ghrelin, and PYY. Evid.-Based Compl. Alt. 2020, 8164064 (2020).
Yan, C. et al. Mitochondrial quality control and its role in osteoporosis. Front. Endocrinol. 14, 1077058 (2023).
Zheng, M. et al. Differences in the prevalence and risk factors of osteoporosis in Chinese urban and rural regions: A cross-sectional study. BMC Musculoskel. Dis. 24, 46 (2023).
Zhou, Y. et al. Association between dietary inflammatory index and bone density in lactating women at 6 months postpartum: A longitudinal study. BMC Public Health 19, 1076 (2019).
Wang, L., Qin, X., Zhang, Y., Xue, S. & Song, X. The prognostic predictive value of systemic immune index and systemic inflammatory response index in nasopharyngeal carcinoma: A systematic review and meta-analysis. Front. Oncol. 13, 1006233 (2023).
Zhai, M. et al. The relationship between the fibrinogen to albumin ratio and early outcomes in patients with acute pontine infarction. Clin. Appl. Thromb. Hemost. 28, 1319718532 (2022).
Chu, M. et al. Systemic inflammation response index predicts 3-month outcome in patients with mild acute ischemic stroke receiving intravenous thrombolysis. Front. Neurol. 14, 1095668 (2023).
Kim, K. S., Oh, A. R., Park, J. & Ryu, J. A. Association between fibrinogen-to-albumin ratio and prognosis in patients admitted to an intensive care unit. J. Clin. Med. 12, 1407 (2023).
Silva-Vaz, P. et al. Evaluation of prognostic factors of severity in acute biliary pancreatitis. Int. J. Mol. Sci. 21, 4300 (2020).
Jiang, B. et al. Are the preoperative albumin levels and the albumin to fibrinogen ratio the risk factors for acute infection after primary total joint arthroplasty?. Front. Surg. 9, 1043242 (2022).
Yu, T., Liu, H., Liu, Y. & Jiang, J. Inflammatory response biomarkers nomogram for predicting pneumonia in patients with spontaneous intracerebral hemorrhage. Front. Neurol. 13, 1084616 (2022).
Black, D. M. et al. The interaction of acute-phase reaction and efficacy for osteoporosis after zoledronic acid: HORIZON pivotal fracture trial. J. Bone Miner. Res. 37, 21 (2022).
Camacho, P. M. et al. American association of clinical endocrinologists/American college of endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis-2020 update. Endocr. Pract. 26, 1 (2020).
Chao, B., Ju, X., Zhang, L., Xu, X. & Zhao, Y. A novel prognostic marker systemic inflammation response index (SIRI) for operable cervical cancer patients. Front. Oncol. 10, 766 (2020).
Ma, K. et al. Development and validation of a risk nomogram model for predicting contrast-induced acute kidney injury in patients with non-ST-elevation acute coronary syndrome undergoing primary percutaneous coronary intervention. Clin. Interv. Aging 17, 65 (2022).
Kernan, W. N. et al. Phenylpropanolamine and the risk of hemorrhagic stroke. N. Engl. J. Med. 343, 1826 (2000).
Liu, S. et al. The effects of intraoperative cryoprecipitate transfusion on acute renal failure following orthotropic liver transplantation. Hepatol. Int. 7, 901 (2013).
McGregor, N. E. et al. IL-6 exhibits both cis- and trans-signaling in osteocytes and osteoblasts but only trans-signaling promotes bone formation and osteoclastogenesis. J. Biol. Chem. 294, 7850 (2019).
Zhou, Q. et al. Systemic inflammation response index as a prognostic marker in cancer patients: A systematic review and meta-analysis of 38 cohorts. Dose-Response 19, 1485814696 (2021).
Sun, D. W., An, L. & Lv, G. Y. Albumin-fibrinogen ratio and fibrinogen-pre albumin ratio as promising prognostic markers for cancers: An updated meta-analysis. World J. Surg. Oncol. 18, 9 (2020).
Ying, H. Q. et al. The value of circulating fibrinogen-to-pre-albumin ratio in predicting survival and benefit from chemotherapy in colorectal cancer. Ther. Adv. Med. Oncol. 13, 17532378 (2021).
Zhang, J. et al. Combining the fibrinogen/albumin ratio and systemic inflammation response index predicts survival in resectable gastric cancer. Gastroent. Res. Pract. 2020, 3207345 (2020).
Li, Q. et al. Preoperative fibrinogen albumin ratio is an effective biomarker for prognostic evaluation of gallbladder carcinoma after radical resection: A 10-year retrospective study at a single center. J. Inflamm. Res. 16, 677 (2023).
Xu, Q. et al. A novel inflammation-based prognostic score: The fibrinogen/albumin ratio predicts prognoses of patients after curative resection for hepatocellular carcinoma. J. Immunol. Res. 2018, 4925498 (2018).
Bunch, C. M. et al. Preventing thrombohemorrhagic complications of heparinized COVID-19 patients using adjunctive thromboelastography: A retrospective study. J. Clin. Med. 10, 3097 (2021).
Kryczka, K. E., Kruk, M., Demkow, M. & Lubiszewska, B. Fibrinogen and a triad of thrombosis, inflammation, and the renin-angiotensin system in premature coronary artery disease in women: A new insight into sex-related differences in the pathogenesis of the disease. Biomolecules 11, 1036 (2021).
Li, M. et al. Relation of fibrinogen-to-albumin ratio to severity of coronary artery disease and long-term prognosis in patients with non-ST elevation acute coronary syndrome. Biomed. Res. Int. 2020, 1860268 (2020).
Suzuki, S. et al. Prognostic significance of serum albumin in patients with stable coronary artery disease treated by percutaneous coronary intervention. PLOS ONE 14, e219044 (2019).
Kanda, E., Tsuruta, Y., Kikuchi, K. & Masakane, I. Use of vasopressor for dialysis-related hypotension is a risk factor for death in hemodialysis patients: Nationwide cohort study. Sci. Rep. 9O, 3362 (2019).
Wang, P. et al. High fibrinogen-to-albumin ratio with type 2 diabetes mellitus is associated with poor prognosis in patients undergoing percutaneous coronary intervention: 5-year findings from a large cohort. Cardiovasc. Diabetol. 21, 46 (2022).
Arques, S. Human serum albumin in cardiovascular diseases. Eur. J. Intern. Med. 52, 8 (2018).
Urbanowicz, T. et al. Neutrophil counts, neutrophil-to-lymphocyte ratio, and systemic inflammatory response index (SIRI) predict mortality after off-pump coronary artery bypass surgery. Cells 11, 1124 (2022).
Zheng, C., Ye, S., Liu, W., Diao, M. & Li, L. Prognostic value of systemic inflammation response index in hepatoblastoma patients receiving preoperative neoadjuvant chemotherapy. Front. Oncol. 13, 1276175 (2023).
Sciacqua, A. et al. Impaired clinical efficacy of aspirin in hypoalbuminemic patients with diabetes mellitus. Front. Pharmacol. 12, 695961 (2021).
Kim, E. H. et al. Coinfection with SARS-CoV-2 and influenza A virus increases disease severity and impairs neutralizing antibody and CD4(+) T cell responses. J. Virol. 96, e187321 (2022).
Zekri-Nechar, K. et al. Albumin binds COVID-19 spike 1 subunit and predicts in-hospital survival of infected patients-possible alteration by glucose. J. Clin. Med. 11, 587 (2022).
Liu, G., Wang, S. & Du, Z. Risk factors of intravenous immunoglobulin resistance in children with kawasaki disease: A meta-analysis of case-control studies. Front. Pediatr. 8, 187 (2020).
Barbano, B., Gigante, A., Amoroso, A. & Cianci, R. Thrombosis in nephrotic syndrome. Semin. Thromb. Hemost. 39, 469 (2013).
DeKay, J. T. et al. DEspR(high) neutrophils are associated with critical illness in COVID-19. Sci. Rep. 11, 22463 (2021).
Alivernini, S. et al. Driving chronicity in rheumatoid arthritis: Perpetuating role of myeloid cells. Clin. Exp. Immunol. 193, 13 (2018).
Gu, T. et al. Effects of immunopotentiators on biochemical parameters, proinflammatory cytokine, and nonspecific immune responses in Shaoxing ducklings. Poultry Sci. 99, 5461 (2020).
Qin, Y. et al. GIMAP7 as a potential predictive marker for pan-cancer prognosis and immunotherapy efficacy. J. Inflamm. Res. 15, 1047 (2022).
Chlastakova, A. et al. Iripin-1, a new anti-inflammatory tick serpin, inhibits leukocyte recruitment in vivo while altering the levels of chemokines and adhesion molecules. Front. Immunol. 14, 1116324 (2023).
Ivanov, K., Garanina, E., Rizvanov, A. & Khaiboullina, S. Inflammasomes as targets for adjuvants. Pathogens 9, 252 (2020).
Wang, X. et al. Predictive impact of fibrinogen-to-albumin ratio (FAR) for left ventricular dysfunction in acute coronary syndrome: A cross-sectional study. Eur. J. Med. Res. 28, 68 (2023).
Sun, Y., Hong, L. & Gao, C. The association among 14-3-3eta protein, inflammation, bone remodeling, and osteoporosis in patients with rheumatoid arthritis. Pak. J. Med. Sci. 36, 872 (2020).
Wang, S. Y. et al. Interleukin 6 promotes BMP9-induced osteoblastic differentiation through Stat3/mTORC1 in mouse embryonic fibroblasts. Aging 15, 718 (2023).
Yokota, K. et al. Characterization and function of tumor necrosis factor and interleukin-6-induced osteoclasts in rheumatoid arthritis. Arthritis Rheumatol. 73, 1145 (2021).
Koh, J. M. et al. Higher circulating hsCRP levels are associated with lower bone mineral density in healthy pre-and postmenopausal women: evidence for a link between systemic inflammation and osteoporosis. Osteoporosis Int. 16, 1263 (2005).
Briot, K., Geusens, P., Em, B. I., Lems, W. F. & Roux, C. Inflammatory diseases and bone fragility. Osteoporosis Int. 28, 3301 (2017).
Funding
The study was supported by China Postdoctoral Science Foundation (CN) (2022M711439), Elderly Health Research Project of Jiangsu Province (CN) (LKZ2022020), Special Funding for Jiangsu Province Science and Technology Plan (Key Research and Development Program for Social Development) (CN) (BE2023738) and Suzhou Collaborative Innovation Research Project of Medical and Industrial Integration (CN) (SLJ2022023).
Author information
Authors and Affiliations
Contributions
Study design: KL and CL. Study conduct: CL and KL. Data collection: XJZ,KL,ZHL and MZX. Data analysis: XJZ. Data interpretation: XJZ and KL. Drafting manuscript: XJZ. Revising manuscript content: KL and CL. Approving final version of manuscript: XJZ, CL, and KL.XJZ and KL take responsibility for the integrity of the data analysis. XJZ and KL took responsibility for the integrity of the data analysis. XJZ and KL contributed equally to this work and should be considered co-first authors. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhou, Xj., Lu, K., Liu, Zh. et al. U-shaped relationship found between fibrinogen-to-albumin ratio and systemic inflammation response index in osteoporotic fracture patients. Sci Rep 14, 11299 (2024). https://doi.org/10.1038/s41598-024-61965-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-61965-9
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.