Abstract
This pilot study focusing on Sickle Cell Anemia (SCA) patients offers a comprehensive and integrative evaluation of respiratory, cardiovascular, hemodynamic, and metabolic variables during exercise. Knowing that diastolic dysfunction is frequent in this population, we hypothesize that a lack of cardiac adaptation through exercise might lead to premature increase in blood lactate concentrations in SCA patients, a potential trigger for acute disease complication. SCA patients were prospectively included in PHYSIO-EXDRE study and underwent a comprehensive stress test with a standardized incremental exercise protocol up to 4 mmol L−1 blood lactate concentration (BL4). Gas exchange, capillary lactate concentration and echocardiography were performed at baseline, during stress test (at ∼ 2 mmol L−1) and BL4. The population was divided into two groups and compared according to the median value of percentage of theoretical peak oxygen uptake (%\({\dot{\text{V}}\text{O}}_{2peakth}\)) at BL4. Twenty-nine patients were included (42 ± 12 years old, 48% of women). Most patients reached BL4 at low-intensity exercise [median value of predicted power output (W) was 37%], which corresponds to daily life activities. The median value of %\({\dot{\text{V}}\text{O}}_{2peakth}\) at BL4 was 39%. Interestingly, diastolic maladaptation using echocardiography during stress test along with hemoglobin concentration were independently associated to early occurrence of BL4. As BL4 occurs for low-intensity exercises, SCA patients may be subject to acidosis-related complications even during their daily life activities. Beyond assessing physical capacities, our study underlines that diastolic maladaptation during exercise is associated with an early increase in blood lactate concentration.
Similar content being viewed by others
Introduction
Sickle cell disease (SCD) is the most common inherited blood disorder in the world1. Poor physical capacities are common in patients homozygous for HbS—also called sickle cell anemia (SCA)—as a result of anemia and multiple pulmonary, cardiac, endothelial, muscle, and metabolic dysfunctions2. For these patients, elevated pulmonary arterial pressure, diastolic dysfunction, impaired oxygen transport and delivery3 and early blood lactate accumulation4,5 translate into poor adaptation to physical activities. During an exercise of increasing intensity, significant activation of glycogenolysis and glycolysis leads to muscle lactate production, accumulation and subsequently to an increase in blood concentrations6,7. These exercise-related metabolic changes result in a left shift of the blood lactate (vs. work load) curve, with premature occurrence of the first lactate threshold and of the 4 mmol L−1 blood lactate concentration (BL4). Furthermore, elevation of blood lactate concentrations is accompanied by acidosis8.
Regarding SCA patients, acidosis is well-known for promoting hemoglobin S (HbS) deoxygenation, increasing the risk of polymerization, potentially inducing red blood cell sickling, and ultimately leading to vaso-occlusive crisis and hemolysis9. Therefore, an in-depth analysis of those patients during exercise is crucial to better understand the link between metabolic status and cardiovascular adaptation. Indeed, cardiovascular abnormalities at rest, such as pulmonary hypertension (PH) and diastolic dysfunction, have been identified as the leading cause of mortality and impaired quality of life in SCA patients10,11,12,13,14. These disorders rely on complex mechanisms associating chronic anemia, hemolysis-induced vasculopathy and repeated vaso-occlusive episodes, contributing to a maladaptive cardiovascular remodeling15,16,17. While the diagnosis of cardiac dysfunction is extremely challenging considering the unique hemodynamic features of SCA, recent studies have reported the potential interest of investigating cardiovascular adaptation during exercise, to dynamically unmask latent heart dysfunction and its association with exercise limitation18,19,20. However, there is currently no data available on the link between cardiac impairment, premature lactate accumulation and thus the poor physical capacities of SCA patients during stress test.
This pilot study is designed to comprehensively evaluate multiple exercise parameters by integrating cardiovascular, hemodynamic, respiratory, and metabolic variables. The main hypothesis of this work is that subclinical cardiac diastolic alterations during exercise might lead to premature increase in blood lactate concentrations, assessed by percentage of theoretical peak oxygen uptake (%\({\dot{\text{V}}\text{O}}_{2peakth}\)) at BL4. The secondary objective was to evaluate the safety of the procedure.
Methods
Study design and patients
This pilot study was carried out in collaboration between the Physiology Department and the Sickle Cell Disease Referral Center, at Henri Mondor University Hospital, Creteil, France. Consecutive SCA adult patients referred by the SCD Referral Center for a cardiovascular pre-rehabilitation assessment were approached to participate in this prospective exploratory study from September 2020 to July 2021. SCA patients ≥ 18 years of age, at steady state condition and with health insurance coverage. Patients under administration of beta-blockers or other bradycardic therapies, or with specific SCD treatments (erythropheresis, hydroxyurea, blood transfusion) were also included. Exclusion criteria were (i) a contraindication for or inability to cycling on ergometer, (ii) patients under guardianship, curatorship, or legal protection, and (iii) pregnant or nursing women. This study was performed in line with the principles of the Declaration of Helsinki. All patients provided written informed consent. The protocol was supervised by a data safety monitoring board and the trial was approved by the ad hoc ethics committee (Comité de Protection des Personnes Ouest III; APHP 201322; EudraCT ID RCB 2020-A02842-37).
Research hypothesis
Exercise intolerance is multifactorial in SCA patients. Through a comprehensive and standardized evaluation of parameters associated with early anaerobic shift, we though to highlight cardiac function adaptation through exercise as a pathophysiological pathway associated with early blood lactates accumulation, ultimately leading to a reduced workload.
Data collection
All participants were interviewed, underwent physical examination and their medical records were examined. Height (cm) and body mass (kg) were recorded, and body mass index was calculated. History of past complications of SCD was documented, including vaso-occlusive crisis, acute chest syndrome (ACS), priapism, skin ulcers, osteonecrosis, chronic organ damage [pulmonary hypertension (PH) documented on right heart catheterization (RHC), cerebral vasculopathy, renal disease, retinopathy] and in intensive care units. Laboratory tests performed in the SCD Referral Center (complete blood count, serum chemistry profile, and lactate dehydrogenase less than a month before the procedure) were collected.
Procedure
All patients underwent the same single session of examination in the Physiology Department (altitude + 50 m), Fig. 1. Investigators led by a cardiologist were blinded to patients’ history. Firstly, patients underwent an echocardiography (VIVID E95—General Electric, Boston, USA) at rest. All patients performed a baseline spirometry to determine the forced expiratory volume in 1 s (FEV1) and the forced vital capacity (FVC). Then, a hyperhemic cold cream (Dolpic, Montbonnot, France) was applied onto the earlobe and removed right before the exercise. After, patients performed a submaximal cardiopulmonary exercise test (CPET) on a stationary electronic cycle ergometer (Koch Evolution-Tech, Le Haillan, France) as previously proposed2. Patients started CPET at a power output of 20 or 30 W (for women and men, respectively), with an increase of 5 W every minute. Exercise was stopped as soon as blood lactate reached a concentration ≥ 4 mmol L−1. At rest and every minute during exercise, samples of 10 µL of arterialized capillary blood were collected from the earlobe and analyzed extemporaneously within 15–20 s (EKF lactate scout 4 reader, Cardiff, United-kingdom) to determine whole blood lactate concentration ([lactate]b, mmol L−1) and establish a blood lactate (vs. work rate) curve for each patient. Stress echocardiography data (VIVID E95—General Electric, Boston, USA) were collected when lactate concentrations reached ∼ 2 mmol L−1 (BL2, which can be interpreted as the first lactic threshold21) and ∼ 4 mmol L−1 (BL4) as well as during the early phase (within 2 min) of recovery (procedure detailed below and in Fig. 1). Two minutes after exercise completion, a blood sample of 80 µL was withdrawn from the earlobe to measure blood gas including pH (ABL90 Flex, Radiometer, København, Denmark). Blood pressure was measured automatically every 2 min, while pulse oximetry (peripheral oxygen saturation), 12-lead electrocardiogram, heart rate and gas exchange were continuously monitored. Gas exchange at rest, during exercise and in recovery were analyzed to determine minute ventilation (\({\dot{{\text{V}}}{\text{E}}}\), L min−1), oxygen uptake (\({\dot{{\text{V}}}{\text{O}}}_{2}\), mL min−1 kg−1), carbon dioxide output (\({\dot{{\text{V}}}{\text{CO}}}_{2}\), L min−1) and \({\dot{{\text{V}}}{\text{E}}}\)/\({\dot{{\text{V}}}{\text{CO}}}_{2}\) slope were recorded or calculated. Since peak \({\dot{{\text{V}}}{\text{O}}}_{2}\) and power output (W) are influenced by age, sex, and body mass, percentages of predicted \({\dot{{\text{V}}}{\text{O}}}_{2peakth}\) (%\({\dot{{\text{V}}}{\text{O}}}_{2peakth}\)) and power output (%\({\dot{{\text{W}}}}_{maxth}\)) were also used to adjust study's analyses with regard to these parameters22. Theoretical maximum power output was obtained using the energy cost of a Watt, which averages 10.5 mlO2 W−1 on an electromagnetic ergocycle. The equation for predicting \({\dot{\text{V}}\text{O}}_{2peakth}\) was:
The indexed arteriovenous oxygen difference or O2 extraction (AV-O2Δ in mL O2/L blood/m2 of body surface area) was calculated as the ratio of \({\dot{{\text{V}}}{\text{O}}}_{2}\) to cardiac index (CI) obtained from \({\dot{{\text{V}}}{\text{O}}}_{2}\) and echocardiography data recorded at each level of effort23. Preventive measures for the critical post-exercise period were applied and consisted in 2 min of active recovery followed by at least 8 min of passive recovery, including rehydration5. Patients were clinically monitored for 1 h following the procedure.
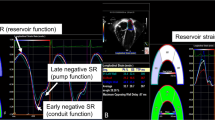
Echocardiography evaluation
Comprehensive 2-dimensional, M-mode, Doppler and tissue Doppler echocardiography were performed according to contemporary guidelines by experienced sonographers blinded to medical record24,25. left ventricular (LV) end-diastolic volume, mass and left atrial volume were indexed to body surface area (LVEDVind, LVMind and LAVind, respectively). Complete echocardiography was performed at rest and LV contractility, cardiac output and diastolic function parameters were evaluated during sub-maximal exercise, at ∼ 2 mmol L−1 of blood lactate concentration, ∼ 4 mmol L−1 (BL4, just before exercise completion) and during the recovery phase. All studies were interpreted offline and in a completely blinded fashion by a cardiologist with extensive experience in resting and exercise echocardiographic assessment. Mitral inflow velocity pattern, peak velocities of early (E) and late (A) waves and E wave deceleration time (DT) were recorded. Tissue Doppler echocardiography was performed to measure early (e′) diastolic tissue velocities at the lateral mitral annulus, a witness of LV compliance. Lateral E/e′ ratio was used as a reflection of LV filling pressure (LVFP)26. Cardiac output (CO) was calculated by multiplying the LV systolic ejection volume (SEV) by the heart rate. SEV was measured by the time-velocity integral of aortic flow multiplied by the area of the ejection orifice. Cardiac index corresponded to the CO indexed to the body surface area. To evaluate cardiac adaptation during sub-maximal exercise, the ratios of values obtained at BL4 over baseline for CI, e′ and E/e′ were computed and analyzed27,28,29. All measures represent the mean of measurements from 3 beats for patients in sinus rhythm and the mean of 5 beats for the single patient in atrial fibrillation.
Control population
A control population of healthy non-SCD subjects matched on age and gender and referred to the Physiology department for stress echocardiography was included. They performed stress echocardiography and blood lactate monitoring without gas exchange measurement. Hemodynamic and echocardiographic data were recorded at BL4 and used for comparison with the study population. Experimental conditions (location, sonographer, material for gas exchange and blood lactate measurement) were the same as the one used for the study population.
Statistical analysis
The cohort was designed so that it could be divided into two groups based on the median of the occurrence of BL4 expressed as %\({\dot{{\text{V}}}{\text{O}}}_{2peakth}\). As such, it enabled the evaluation of multiple variables associated with the earliness of reaching a blood lactate concentration of 4 mmol L−1 and explore diastolic cardiac adaptation impairment (defined in the “Echocardiography evaluation” section). Considering the observational nature of the study, regardless of any preconceived hypothesis and previous literature to build on, sample size calculations relied on the minimal magnitude of the effect sizes of both the differences between the two groups (based on BL4) but also the correlations between %\({\dot{{\text{V}}}{\text{O}}}_{2peakth}\) at BL4 and patient’s characteristics. The inclusion of at least 26 subjects (i.e. 13 patients per group) allows the detection of statistically significant differences with a minimal effect size of 1 standard deviation, as well as the identification of Pearson correlation coefficients ≥ 0.5, with 80% power at 5% one-sided risk30,31. Descriptive results were expressed as mean (SD) or median [IQR] for continuous variables, and as numbers (%) for categorical variables. In accordance with our objective to associate cardiac diastolic impairment with early anaerobic shift, unadjusted group comparisons of continuous variables were performed using t tests or Mann–Whitney tests according to the normality of their distributions. Categorical variables were compared with the χ2 test. In addition to using our variable of interest (%\({\dot{{\text{V}}}{\text{O}}}_{2peakth}\) at BL4) as a binary endpoint, we further analyzed it as a continuous variable using one-tailed Pearson correlation to evaluate relationships between BL4 occurrence with hemodynamic, cardiac respiratory and biological data. To identify factors independently associated with early BL4, multivariate analysis was then performed using binary logistic regression on parameters available in all the patient and significantly associated with or trending toward (p < 0.1) early vs. late BL4 occurrence (categorical variable based on the median of \(\%{\dot{{\text{V}}}{\text{O}}}_{2peakth}\) at BL4). Notably, despite p < 0.1, documented PH and A wave on TTE were not included in the model since less than half of the patients had a RHC and A wave could not be measured in two patients due to AF or atrial hyperexcitability. Odds ratios (ORs) are presented with their 95% confidence intervals. A p value < 0.05 indicates statistical significance. Analyses were computed using SPSS 26 (IBM, Armonk, New York).
Data sharing statement
For additional original data, please contact Thomas.dhumieres@aphp.fr.
Results
Population characteristics
Between September 2020 and July 2021, 30 SCA patients participated in the study. Twenty-nine patients reached 4 mmol L−1 of [lactate]b during sub-maximal exercise and were included in the analysis. One patient had to stop exercise prematurely because of osteoarticular pain and was further excluded from the analysis. The baseline clinical, echocardiography and laboratory characteristics are summarized in Table 1. Briefly, mean age was 42 ± 12 years and 52% were men. Patients had frequent organ involvement (pulmonary hypertension, cerebral vasculopathy, chronic kidney disease, Table 1). Most of them (72%) were treated with hydroxyurea and 35% were included in an erythrocytapheresis program. Left ventricular ejection fraction was normal (LVEF = 62 ± 5%) for all patients. Left cardiac cavities were dilated (LVEDVind = 76 ± 16 mL m−2 and LAVind = 48 ± 26 mL m−2). Right ventricular function was preserved (TAPSE = 28 ± 5 mm). One patient was in atrial fibrillation. No sign of pulmonary obstructive disease was observed on the spirometry.
Exercise responses and physical capacity indexes
Baseline lactatemia was 1.4 ± 0.5 mmol L−1 and exercise was stopped at 4.1 ± 0.1 mmol L−1. Cardiopulmonary (including gas exchange), and absolute or normalized to baseline echocardiography and hemodynamic data at BL2 and BL4 are summarized in Table 2. There was a great variability in the power outputs reached at BL4, with values ranging from 23 to 58% of %\({\dot{{\text{W}}}}_{maxth}\) adjusted over age, sex, and body weight (Fig. 2). As expected, SCA patients displayed significant exercise intolerance as testified by the low \({\dot{{\text{V}}}{\text{O}}}_{2}\) values at BL2 (10.7 ± 3.13 mL kg−1 min−1, corresponding to 29.8 ± 7.9% of %\({\dot{{\text{V}}}{\text{O}}}_{2peakth}\)) and BL4 (14.6 ± 3.4 mL kg−1 min−1, 40.5 ± 8.5% of %\({\dot{{\text{V}}}{\text{O}}}_{2peakth}\)) as well as the corresponding power output at BL4 (71.2 ± 20.7 W, corresponding to 38.1 ± 9.0% of %\({\dot{{\text{W}}}}_{maxth}\)). For the reader's interest, detailed individual data on respiratory and hemodynamic parameters at BL2 and BL4 are provided in supplemental data.
Comparison with healthy non-SCD control group
Ten subjects composed the control group and were comparable to the SCA study population in terms of age and sex ratio (Supplemental data). Baseline mean arterial pressure was lower in the study population while cardiac index was higher (99 ± 14 vs. 111 ± 13 mmHg, p = 0.03 and 3.9 ± 0.7 vs. 2.7 ± 0.6 L min−1 m−2, p < 0.001 respectively). At BL4, power output expressed as % of the maximum predicted was much lower in the study population (38 ± 9 vs. 80 ± 24 of %\({\dot{{\text{W}}}}_{maxth}\), p < 0.001). Diastolic adaptation at BL4 as assessed by the normalized to baseline e′ and E/e′, two key parameters of diastolic function was similar in the two groups, with a higher variability in the study population (Supplementary Data).
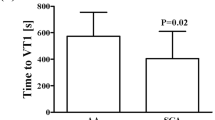
Univariate analysis comparing two groups of SCA patients based on their %\({\dot{V}O}_{2peakth}\) at BL4
The study population was then divided into two groups based on the median of the occurrence of BL4 expressed as %\({\dot{{\text{V}}}{\text{O}}}_{2peakth}\) that was calculated at 39%. Fourteen patients constituted the lower exercise level group (BL4 < 39% group, %\({\dot{{\text{V}}}{\text{O}}}_{2peakth}\)= 34.4 ± 5.4%) and 15 patients were included in the upper exercise level group (BL4 ≥ 39% group, %\({\dot{{\text{V}}}{\text{O}}}_{2peakth}\) = 46.2 ± 6.8%). Baseline clinical, biological and echocardiographic data of these two groups are reported in Table 3. In univariate analysis, hemoglobin (8.1 ± 1.1 vs. 9.2 ± 1.1 g dL−1, p = 0.009) and beta-blocker use [7 (50%) vs. 1 (13%), p = 0.03] were the only two baseline variables associated with early occurrence of BL4. None of the echocardiography data assessed at rest could discriminate the two groups. As expected, the BL4 < 39% group developed less power output and MET at BL4 than the BL4 ≥ 39% one (33 ± 4.7 vs. 42.8 ± 9.6% of \({\dot{{\text{W}}}}_{maxth}\), p = 0.002 and 3.6 ± 0.6 vs. 4.7 ± 1 MET, p = 0.003, respectively; Table 4). Notably, the BL4 < 39% group showed abnormal diastolic adaptation at BL4 as assessed by the normalized to baseline e′ and E/e′ (e′BL4/e′rest = 1.4 ± 0.2 vs. 1.6 ± 0.3, p = 0.039 and E/e′BL4/ E/e′rest = 1.2 ± 0.2 vs. 1.0 ± 0.2, p = 0.003). The BL4 < 39% group also had a trend for poorer peripheral oxygen extraction at BL4 (AV-O2Δ: 112 ± 33 vs. 147 ± 59 mL L m−2, p = 0.07) while increases in blood pressure, heart rate, and cardiac output were similar between the two groups (Table 4).
Multivariate analysis using logistic regression
Baseline hemoglobin, beta-blocker use, oxygen saturation at rest, AV-O2Δ at BL4, and BL4 to baseline ratio of e′ and E/e′ were entered into multivariate analysis (Table 5). Baseline hemoglobin (OR = 3.5 [1; 13], p = 0.05) and E/e′ ratio (OR = 10–3 [10–4; 0.6], p = 0.04) were independently associated with early occurrence of BL4.
Correlations between %\({\dot{V}O}_{2peakth}\) at BL4 and parameters of interest based on group comparison
Consistently with previous analysis, E/e′ and hemoglobin where the only parameters that showed moderate correlation to %\({\dot{{\text{V}}}{\text{O}}}_{2peakth}\) at BL4 (r = 0.39, p = 0.02 and r = − 0.30, p = 0.05, respectively; supplemental data). Notably, correlations were also sought with all continuous variables presented in Table 1 along with BL4 hemodynamic and echocardiography data shown in Table 2. Total bilirubin level correlated with %\({\dot{{\text{V}}}{\text{O}}}_{2peakth}\) at BL4 (r = − 0,33, p = 0.04) while no other parameter did (data not shown).
Protocol safety
No severe clinical events occurred during the stress test. Electrocardiogram abnormalities during exercise were observed in 4 patients (two with transient ST segment depression, one with numerous premature ventricular complex and one with a short and non-sustained ventricular tachycardia of 8 complex). Arterialized blood gas analysis was performed for 21 patients two minutes after exercise completion and revealed a mean pH of 7.40 ± 0.04 associated with a [lactate]b of 4.9 ± 0.6 mmol L−1. Blood acidosis with pH < 7.35 was observed for only one patient, who presented an end-stage kidney disease (Supplementary Data).
Discussion
In this pilot study, we used an innovative and integrated approach which analyzes simultaneously hemodynamic, cardiac, respiratory, and metabolic parameters during stress test to highlight diastolic cardiac abnormalities linked to premature blood lactate accumulation. To our knowledge, this is the first application of “diastolic stress test” in conjunction with lactate monitoring in SCA patients. Our main findings were: (1) As hypothesized, impaired diastolic adaptation to exercise is independently associated with an early occurrence of BL4, such as low hemoglobin level. (2) Poor physical capacities are observed in all patients, thus reflecting their high vulnerability to exercise. Our protocol of sub-maximal stress test appears safe and feasible despite the severity of SCA patients.
Stress-induced diastolic dysfunction is associated with poor exercise capacity and premature lactate elevation
While baseline echocardiographic data were similar in the two groups (defined according to their %\({\dot{{\text{V}}}{\text{O}}}_{2peakth}\) at BL4), the diastolic stress test unmasked poor diastolic adaptations that was independently associated with an early increase of [lactate]b during a sub-maximal exercise. The evaluation of diastolic function during exercise is a new test, particularly useful to contribute to the challenging diagnosis of heart failure with preserved ejection fraction by identifying elevated LV filling pressures26,27. Yet, diastolic stress test and concomitant evaluation of [lactate]b has not been evaluated in assessing cardiac function and vulnerability to exercise in SCA population. In our study, the increase in cardiac output was similar in both groups, but the increase in e′ velocity at BL4 was lower in the low physical capacity group (< 39% \({\dot{{\text{V}}}{\text{O}}}_{2peakth}\) at BL4), reflecting a subtle impairment in LV compliance. Indeed, a stress-induced increase in cardiac output associated with an altered LV compliance may be responsible for elevated LV filling pressures and alveolar edema. Accordingly, E/e′ ratio, a relevant index of LV filling pressure, increased in the BL4 < 39% group, indicative of a LVFP elevation26, while E/e′ ratio remained stable in the BL4 ≥ 39% group, reflecting a harmonious cardiac adaptation to exercise (Fig. 3). Our data extend previous reports on an independent association between E/e′ at rest and %\({\dot{{\text{V}}}{\text{O}}}_{2peakth}\) or 6-min walk distance in SCA patients, suggestive of existing atrial cardiomyopathy13,18,20. However, we did not find such discriminant abnormalities on resting echocardiography, highlighting the challenge of diagnosing diastolic dysfunction in resting conditions in SCA population15,16. Thus, our results suggest that diastolic stress test during sub-maximal exercise is a valuable and safe tool in the early detection of subtle cardiac impairment in SCA patients.
Oxidative metabolism being directly limited by low oxygen transport capacities, our results also underline the expected role of anemia as a factor associated with the early occurrence of BL432. Furthermore, the degree of anemia is mainly linked to the extent of hemolysis in SCA patients, which also alter peripheral oxygen exchanges through the development of systemic vasculopathy33,34. However, our study did not show any association between hemolysis parameters and BL4 occurrence. This could be explained by the small population size, but also by the lack of specificity of the routinely used hemolysis markers (LDH and bilirubin)35. Since innovative therapies increase (i) hemoglobin level by decreasing HbS sickling and erythrocytes hemolysis, and (ii) oxygen transport and supply, the evaluation of their impact on BL4 occurrence would be of particular interest36,37,38. Such therapeutic strategies could indeed delay the onset of BL4 and decrease complications associated with blood acidosis. In line with the latter hypothesis, sub-maximal exercise testing with early occurrence of BL4 could be the starting point of reinforced therapies.
Poor exercise capacities and high metabolic vulnerability
Our study highlights the low physical capacities of SCA patients in relation to the poor transport, supply, extraction and utilization of oxygen at the muscular level2,39,40,41. It also adds mechanistic information, linking exercise diastolic dysfunction and anemia to the left-shift of [lactate]b vs. work rate curve. The comparison with the control group in our study underlines the low power developed by SCA patients at equivalent metabolic stress levels (BL4). In the same way, healthy non-athlete adult individuals reach about 45% and 65% of their \({\dot{{\text{V}}}{\text{O}}}_{2max}\) at BL2 and BL4, respectively, while in the present study the corresponding values were 29.8 ± 7.9% and 40.5 ± 8.5%42. Furthermore, our results underline a great heterogeneity between patients in their physical capacities at BL4, with values that could vary by a factor of 3, independently of age, sex and body weight. Since BL4 is indicative of the onset of lactate unsteady state and constant accumulation, leading to blood acidosis, the practice of daily life physical activities (e.g. cleaning, shopping, walking the dog) could already be for some patients a too heavy effort at the origin of the deleterious cascade of erythrocyte falciformation, leading potentially to hemolytic and vaso-occlusive complications9. In support with the latter hypothesis, by translating exercise intensity at BL4 into metabolic equivalent of task (MET), 3 (10%) patients displayed MET < 3.0 (light intensity), 24 (83%) were [3.0; 6.0] (moderate intensity) and only 2 (7%) patients had MET ≥ 6.0 (vigorous intensity)43. To go beyond the simple assessment of exercise tolerance, the early occurrence of BL4 in response to low intensity training could be a new indicator of patient’s vulnerability, unmasking a lack of adaptation facing metabolic stress situations. Such findings may be extended to other stress conditions such as fever, dehydration, or altitude. This pilot study paves the way for larger studies with patients’ follow-up to investigate the interest of combined diastolic stress test and [lactate]b monitoring as a tool to identify patients at risk and personalize recommendations in terms of physical activities2.
A safe procedure within our cohort
This protocol of integrative sub-maximal exercise evaluation was feasible with valid measurements in all patients. Although maximal cardiopulmonary exercise appears to be a safe testing procedure in children and adults with SCD44, we, as previously described by our team, ensured the safety of the examination by stopping incremental exercise for each patient as soon as a [lactate]b of 4 mmol L−1 was reached. This sub-maximal exercise prevents patients from being exposed to a metabolic risk situation (acidosis) and potential related complications21,45. Despite an unselected and severe population including patients with frequent organ damage, no patient presented any adverse clinical event during exercise or the recovery phase. In addition, no [lactate]b value exceeding 7 mmol L−1 was observed in early phase of the recovery, a value associated with a risk of acid–base imbalance46. Consistently, exercise-induced blood acidosis was only found in one patient, with an end-stage renal disease.
Strengths and limitations
One key methodological strength of the present study was the extemporaneous monitoring of [lactate]b that allowed to analyze cardiac and ventilatory parameters at homogeneous and comparable levels of metabolic stress between patients (from baseline to 4 mmol L−1). Indeed, the analysis at maximum effort involves many confounding factors such as joint and muscle pain or the willingness of patients that could mislead results. In addition, to evaluate the earliness of BL4, we expressed it in %\({\dot{{\text{V}}}{\text{O}}}_{2peakth}\) in order to automatically adjust for age, sex and BMI and to allow a more relevant comparison between patients47. Our study is limited by its small sample size as well as the heterogeneity of the population, partly counterbalanced by the quality of the phenotyping and the homogenization of the metabolic stress level by blood lactate monitoring. Since pulmonary pressure is strongly associated with patient prognosis in SCD, TRV at BL4 would have been an interesting variable to potentially unmask exercise PH, but it was uninterpretable in more than half of the patients due to the difficulty of obtaining a flow of sufficient quality through examination48,49. Notably, beta-blocker regimen was more often administered to the group with the lowest exercise tolerance. This could reflect more frequent heart disease (such as post-capillary PH), or symptoms justifying the use of beta-blocker by the physician. However, given that the pathophysiology of sickle cell heart disease is rather restrictive added to the anemia and peripheral exchanges alteration, slowing down the heart rate could be deleterious50,51. With regards to the lack of evidence, beta-blockers should be cautiously used in SCA patients.
Conclusion and perspectives
This pilot study provides a new understanding of the mechanisms associated with exercise limitation in SCA patients, adding the role of impaired cardiac diastolic function to anemia. Integrative, sub-maximal, lactate driven exercise evaluation could be safely used to stratify the severity of SCA patients by revealing latent heart impairment or significant metabolic vulnerability and could be the starting point for reinforced therapies and rehabilitation programs.
Abbreviations
- %\({\dot{\text{V}}\text{O}}_{2peakth}\) :
-
Percentage of theoretical peak oxygen uptake
- %\({\dot{{\text{W}}}}_{maxth}\) :
-
Percentage of predicted power output
- A:
-
Peak late diastolic velocity
- ACS:
-
Acute chest syndrom
- AV-O2Δ:
-
Arteriovenous oxygen difference
- BL4:
-
4 Mmol L−1 blood lactate concentration
- CO:
-
Cardiac output
- CI:
-
Cardiac index
- CKD:
-
Chronic kidney disease
- CPET:
-
Cardiopulmonary exercise test
- DT:
-
E Waves deceleration time
- E:
-
Peak early diastolic velocity
- e′:
-
Early diastolic velocity at the lateral site of the mitral annulus
- ECG:
-
Electrocardiogram
- EV:
-
Expired volume
- FEV1:
-
Forced expiratory volume in 1 s
- FVC:
-
Forced vital capacity
- HbS:
-
Hemoglobin S
- HF:
-
Heart failure
- HR:
-
Heart rate
- LAVind :
-
Left atrium volume indexed to body surface area
- LDH:
-
Lactate dehydrogenase
- LT1:
-
First lactate threshold
- LV:
-
Left ventricle
- LVEDVnd :
-
Left ventricular end-diastolic volume indexed to body surface area
- LVEF:
-
Left ventricular ejection fraction
- LVMind :
-
Left ventricular mass indexed to body surface area
- MAP:
-
Mean arterial pressure
- MET:
-
Metabolic equivalent of task
- PH:
-
Pulmonary hypertension
- RHC:
-
Right heart catheterization
- SCA:
-
Sickle cell anemia
- SCD:
-
Sickle cell disease
- SEV:
-
Systolic ejection volume
- TAPSE:
-
Tricuspid annular plane systolic anterior excursion
- TTE:
-
Transthoracic echocardiography
- TRV:
-
Tricuspid regurgitation velocity
- \(\dot{{\text{V}}}{\text{E}}\) :
-
Minute ventilation
- \({\dot{{\text{V}}}{\text{CO}}}_{2}\) :
-
Carbon dioxide output
- \({\dot{{\text{V}}}{\text{O}}}_{2}\) :
-
Oxygen uptake
- W:
-
Power output
References
GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet (London, England). 388(10053), 1545–1602 (2016).
Gellen, B. et al. Moderate-intensity endurance-exercise training in patients with sickle-cell disease without severe chronic complications (EXDRE): An open-label randomised controlled trial. Lancet Haematol. 5(11), e554–e562 (2018).
Halphen, I. et al. Severe nocturnal and postexercise hypoxia in children and adolescents with sickle cell disease. PLoS ONE 9(5), e97462 (2014).
Moheeb, H., Wali, Y. A. & El-Sayed, M. S. Physical fitness indices and anthropometrics profiles in schoolchildren with sickle cell trait/disease. Am. J. Hematol. 82(2), 91–97 (2007).
Messonnier, L. A. et al. Preventive measures for the critical postexercise period in sickle cell trait and disease. J. Appl. Physiol 130(2), 485–490 (2021).
Messonnier, L. A. et al. How to implement endurance exercise training in sickle cell disease. Haematologica. 106(5), 1476–1479 (2021).
Messonnier, L. A. et al. Lower muscle and blood lactate accumulation in sickle cell trait carriers in response to short high-intensity exercise. Nutrients. 14(3), 501 (2022).
Stewart, P. A. Modern quantitative acid–base chemistry. Can. J. Physiol. Pharmacol. 61(12), 1444–1461 (1983).
Chatel, B., Messonnier, L. A. & Bendahan, D. Do we have to consider acidosis induced by exercise as deleterious in sickle cell disease?. Exp. Physiol. 103(9), 1213–1220 (2018).
Parent, F. et al. A hemodynamic study of pulmonary hypertension in sickle cell disease. N. Engl. J. Med. 365(1), 44–53 (2011).
Savale, L. et al. Clinical phenotypes and outcomes of precapillary pulmonary hypertension of sickle cell disease. Eur. Respir. J. 54(6), 1900585 (2019).
Gladwin, M. T. Cardiovascular complications and risk of death in sickle-cell disease. Lancet. 387(10037), 2565–2574 (2016).
Sachdev, V. et al. Diastolic dysfunction is an independent risk factor for death in patients with sickle cell disease. J. Am. Coll. Cardiol. 49(4), 472–479 (2007).
d’Humières, T. et al. Determinants of ventricular arrhythmias in sickle cell anemia: Towards a better prevention of sudden cardiac death. Blood. 142, 409–420 (2023).
d’Humières, T. et al. Cardiovascular phenotypes predict clinical outcomes in sickle cell disease: An echocardiography-based cluster analysis. Am. J. Hematol. 96(9), 1166–1175 (2021).
Hammoudi, N., Lionnet, F., Redheuil, A. & Montalescot, G. Cardiovascular manifestations of sickle cell disease. Eur. Heart J. 41(13), 1365–1373 (2020).
Damy, T. et al. Haematological determinants of cardiac involvement in adults with sickle cell disease. Eur. Heart J. 37(14), 1158–1167 (2016).
Hammoudi, N. et al. Altered cardiac reserve is a determinant of exercise intolerance in sickle cell anaemia patients. Eur. J. Clin. Investig. 52, e13664 (2021).
Alsaied, T. et al. Left atrial dysfunction in sickle cell anemia is associated with diffuse myocardial fibrosis, increased right ventricular pressure and reduced exercise capacity. Sci. Rep. 10(1), 1767–1767 (2020).
Alsaied, T. et al. Diastolic dysfunction is associated with exercise impairment in patients with sickle cell anemia. Pediatr. Blood Cancer. 65(8), e27113–e27113 (2018).
Messonnier, L. A., Gellen, B., Lacroix, R., Peyrot, S., Rupp, T., Mira, J., et al. Physiological evaluation for endurance exercise prescription in sickle cell disease. Med. Sci. Sports Exerc. 51(9) (2019). https://journals.lww.com/acsm-msse/Fulltext/2019/09000/Physiological_Evaluation_for_Endurance_Exercise.1.aspx.
Myers, J. et al. A Reference equation for normal standards for VO2 max: Analysis from the fitness registry and the importance of exercise national database (FRIEND Registry). Progr. Cardiovasc. Dis. 60(1), 21–29 (2017).
Haykowsky, M. J. et al. Effect of endurance training on the determinants of peak exercise oxygen consumption in elderly patients with stable compensated heart failure and preserved ejection fraction. J. Am. Coll. Cardiol. 60(2), 120–128 (2012).
Nagueh, S. F. et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 29(4), 277–314 (2016).
Mitchell, C. et al. Guidelines for performing a comprehensive transthoracic echocardiographic examination in adults: Recommendations from the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 32(1), 1–64 (2019).
Burgess, M. I., Jenkins, C., Sharman, J. E. & Marwick, T. H. Diastolic stress echocardiography: Hemodynamic validation and clinical significance of estimation of ventricular filling pressure with exercise. J. Am. Coll. Cardiol. 47(9), 1891–1900 (2006).
Obokata, M. et al. Role of diastolic stress testing in the evaluation for heart failure with preserved ejection fraction. Circulation. 135(9), 825–838 (2017).
Nishi, T. et al. Incremental value of diastolic stress test in identifying subclinical heart failure in patients with diabetes mellitus. Eur. Heart J. Cardiovasc. Imaging. 21(8), 876–884 (2020).
Tan, Y. T. et al. The pathophysiology of heart failure with normal ejection fraction: Exercise echocardiography reveals complex abnormalities of both systolic and diastolic ventricular function involving torsion, untwist, and longitudinal motion. J. Am. Coll. Cardiol. 54(1), 36–46 (2009).
Sullivan, G. M. & Feinn, R. Using effect size—or why the P value is not enough. J. Grad. Med. Educ. 4(3), 279–282 (2012).
Conroy, R. The RCSI Sample Size Handbook. (2018).
Johnson, S. et al. Exercise-induced changes of vital signs in adults with sickle cell disease. Am. J. Hematol. 96(12), 1630–1638 (2021).
Sundd, P., Gladwin, M. & Novelli, E. Pathophysiology of sickle cell disease. Annu. Rev. Pathol. Mech. Dis. 14, 263–292 (2019).
Kato, G. J., Steinberg, M. H. & Gladwin, M. T. Intravascular hemolysis and the pathophysiology of sickle cell disease. J. Clin. Investig. 127(3), 750–760 (2017).
Dubert, M. et al. Degree of anemia, indirect markers of hemolysis, and vascular complications of sickle cell disease in Africa. Blood. 130(20), 2215–2223 (2017).
Vichinsky, E. et al. A phase 3 randomized trial of voxelotor in sickle cell disease. N. Engl. J. Med. 381(6), 509–519 (2019).
Rab, M. A. E. et al. Decreased activity and stability of pyruvate kinase in sickle cell disease: A novel target for mitapivat therapy. Blood. 137(21), 2997–3001 (2021).
Tshilolo, L. et al. Hydroxyurea for children with sickle cell anemia in Sub-Saharan Africa. N. Engl. J. Med. 380(2), 121–131 (2019).
Quinn, C. T. & Ahmad, N. Clinical correlates of steady-state oxyhaemoglobin desaturation in children who have sickle cell disease. Br. J. Haematol. 131(1), 129–134 (2005).
Ravelojaona, M. et al. Evidence for a profound remodeling of skeletal muscle and its microvasculature in sickle cell anemia. Am. J. Pathol. 185(5), 1448–1456 (2015).
Callahan, L. A. et al. Cardiopulmonary responses to exercise in women with sickle cell anemia. Am. J. Respir. Crit. Care Med. 165(9), 1309–1316 (2002).
Binder, R. K. et al. Methodological approach to the first and second lactate threshold in incremental cardiopulmonary exercise testing. Eur. J. Cardiovasc. Prev. Rehabil. 15(6), 726–734 (2008).
Ainsworth, B. E., Haskell, W. L., Herrmann, S. D., Meckes, N., Bassett, D. R. J. R., Tudor-Locke, C., et al. 2011 compendium of physical activities: A second update of codes and MET values. Med. Sci. Sports Exerc. 43(8) (2011). https://journals.lww.com/acsm-msse/Fulltext/2011/08000/2011_Compendium_of_Physical_Activities__A_Second.25.aspx.
Smith, K. N. et al. Safety of maximal cardiopulmonary exercise testing in individuals with sickle cell disease: A systematic review. Br. J. Sports Med. 56, 764–769 (2021).
Liem, R. I. Balancing exercise risk and benefits: lessons learned from sickle cell trait and sickle cell anemia. Hematol. Am. Soc. Hematol. Educ. Program. 2018(1), 418–425 (2018).
Osnes, J. B. & Hermansen, L. Acid-base balance after maximal exercise of short duration. J. Appl. Physiol. 32(1), 59–63 (1972).
Arena, R. et al. Determining the preferred percent-predicted equation for peak oxygen consumption in patients with heart failure. Circ. Heart Fail. 2(2), 113–120 (2009).
Gladwin, M. T. et al. Pulmonary hypertension as a risk factor for death in patients with sickle cell disease. N. Engl. J. Med. 350(9), 886–895 (2004).
de Lima-Filho, N. N. et al. Exercise-induced abnormal increase of systolic pulmonary artery pressure in adult patients with sickle cell anemia: An exercise stress echocardiography study. Echocardiography. 33(12), 1880–1890 (2016).
Niss, O. et al. Cardiomyopathy with restrictive physiology in sickle cell disease. JACC Cardiovasc. Imaging. 9(3), 243–252 (2016).
Muchtar, E., Blauwet, L. A. & Gertz, M. A. Restrictive cardiomyopathy. Circ. Res. 121(7), 819–837 (2017).
Acknowledgements
The sponsor was Assistance Publique—Hôpitaux de Paris (Direction de la Recherche Clinique et de l'Innovation)
Funding
FHU-SENEC, allocation RSE20003DDA.
Author information
Authors and Affiliations
Contributions
P.B. received grants from ADDMEDICA, Fabre Foundation, NOVARTIS and Bluebird in the past 36 months—consulting fees for ADDMEDICA, NOVARTIS, ROCHE, GBT, Bluebird, EMMAUS, HEMANEXT, AGIOS and honoraria for lectures from NOVARTIS, ADDMEDICA, JAZZPHARMA. P.B. is a membre of NOVARTIS steering committee and Cofounder of INNOVHEM. L.A.M. received consulting fees from Abbott Diabetes Care in the past 36 months.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
d’Humières, T., Bouvarel, A., Boyer, L. et al. Cardiac diastolic maladaptation is associated with the severity of exercise intolerance in sickle cell anemia patients. Sci Rep 14, 11095 (2024). https://doi.org/10.1038/s41598-024-61689-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-61689-w
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.