Abstract
Seizure semiology and electroencephalograph (EEG) are very important for determining seizure type, hemisphere lateralization, or localization. Clinical symptoms of focal seizures, as well as findings at the onset or end of a focal to bilateral tonic–clonic seizure (FBTCS), are highly informative for lateralization. This study aimed to investigate the relationship of asymmetric last clonic jerk in patients with temporal or extratemporal lobe epilepsy with pathologies, localization, lateralization, or other semiological findings detected in neuroimaging or neuro psychometric tests and its positive predictive value for the detection of hemisphere lateralization based on seizure onset ictal EEG activation. 44 patients with asymmetric last clonic jerks (aLCJ) who were followed up in our VEM unit were randomized 1:1 with epilepsy patients without. In patients with ipsilateral automatism and contralateral posture or gustatory and olfactory hallucinations aLCJ was less or absent. In patients with unilateral tonic activity, aLCJ was more common. The positive predictive value of aLCJ for ictal EEG activation lateralization was 86.36%. In conclusion, asymmetric last clonic beat is valuable for lateralization of FBTCS and should be considered. Its presence strongly and reliably lateralizes to the side of seizure onset.
Similar content being viewed by others
Introduction
Seizure semiology and electroencephalograph(EEG) are very important for determining seizure type, hemisphere lateralization, or localization. VEM provides a detailed analysis of the semiological characteristics of seizures correlated with simultaneous EEG activity. Especially in temporal and extratemporal epilepsies, observation of seizures with VEM includes essential information 1,2. Routinely, seizure semiology is analyzed with EEG, neuropsychometric testing (NPT), and neuroimaging. Clinical symptoms in focal seizures, as well as findings at the onset or end of a FBTCS, are highly informative for lateralization 3,4,5. However, it is not possible to examine every patient with VEM, or pathology may not be detected in the recordings. Semiologic findings after the seizure onset are more valuable for these patients than those at the onset, as they can be more clearly seen by both the patient's companions and health professionals.
In temporal or frontal lobe epilepsies, the focal onset and asymmetric termination of the bilateral tonic–clonic phase of secondary generalized tonic–clonic seizures reliably lateralize the side of seizure onset. The asymmetric last clonic jerk occurs ipsilateral to the side of the seizure onset site 6,7. This study aimed to investigate the relationship of asymmetric last clonic jerk in patients with temporal or extratemporal lobe epilepsy with pathologies, localization, lateralization, or other semiological findings detected in neuroimaging or neuro psychometric tests and its positive predictive value for the detection of hemisphere lateralization based on seizure onset ictal EEG activation.
Materials and methods
Patient selection
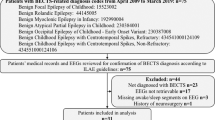
The records of the patients with FBTCS among the patients with focal seizures during hospitalization in the VEM unit of our center between 2005 and 2023 were retrospectively evaluated. Among them, 46 patients with asymmetric last clonic jerks were randomly selected. Two patients were also found to have seizures without electrophysiological correlates (psychogenic non-epileptic seizures) accompanied by last clonic jerks, and 44 patients were included in the study after exclusion (aLCJ). aLCJ patients were randomised in a 1:1 ratio according to age and sex by computer-assisted age and gender with other patients with focal seizures without last clonic jerks (control group; non-aLCJ) from the hospital database. (Fig. 1) (Informed consent was obtained from all subjects and/or their legal guardian(s), and all methods were performed in accordance with the relevant guidelines and regulations.)
VEM protocol
VEM recordings and a continuous video recording were made using scalp electrodes in accordance with the international 10–20 electrode mounting system, with the data using 16–32-channel reference longitudinal and transverse bipolar montages. Spikes, sharp waves, spike and wave complexes temporally intermittent rhythmic delta activity, and continuous focal slow wave activity (theta or delta) were determined. Electrodes with rhythmic theta or delta waves, spike waves or sharp waves before ictal activity were considered as ‘localization of the initial ictal activity’. Anti-seizure medications were reduced or discontinued to facilitate the onset of seizures. After adequate seizure recording, appropriate anti-seizure medication was continued at effective doses. A total of 102 VEM recordings with scalp electrodes (58 patient groups; 5642 h and 44 control group; 3816 h for a total of 9458 h), number of seizures observed, semiologic findings, ictal and interictal EEG findings were retrospectively evaluated. Four hundred twenty-eight seizures (201 and 227, respectively) were analyzed during the recording period.
Other assessments
In addition, all patients underwent NPT during hospitalization. High-resolution 3 Tesla (3 T) Magnetic Resonance Imaging (MRI) was available in all patients. 18F-fluorodeoxyglucose Positron Emission Tomography (FDG PET) results were recorded for patients (56 patients) who underwent 18F-fluorodeoxyglucose Positron Emission Tomography (FDG PET) at the time of hospitalization or within one year before hospitalization, where possible. NPTs were administered by two clinical neuropsychologists experienced in epilepsy. Visual-spatial (occipital regions to anterior pole of temporal lobe, posterior parietal cortex, frontal eye fields, and dorsal visual system), language (classical speech zones, typically in the left dominant hemisphere, including Wernicke's and Broca's areas, and the angular gyrus), attention (ascending reticular activating system, superior colliculus, Five different modalities including thalamus, parietal lobe, anterior cingulate cortex, and the frontal lobe), memory (hippocampal-entorhinal cortex complex, frontal regions, left parietal cortex), and executive functions (frontal-subcortical circuits, including dorsolateral prefrontal, orbital frontal, and anterior) were evaluated in each patient. According to the results, pathological localization and lateralization were categorized as frontal, temporal, right, left, and bilateral.
Reports of all FDG PET scans and MRIs by neuroradiologists, EEG recordings and NPT results were evaluated by a neurologist and two experienced blinded epileptologists, one of whom was a clinical neurophysiologist. After evaluation by more than one expert, the findings were finalized by consensus and analyzed in comparison with clinical characteristics.
Statistical analysis
Descriptive statistics are presented as frequency and percentage for qualitative data. Pearson Chi-square, Fisher-Freeman-Halton, and Fisher's Exact Chi-square tests were used to analyze categorical data. Kappa coefficient and McNemar test were calculated to evaluate the agreement of qualitative data. The significance level was set as α = 0.05. Statistical data analysis was performed using IBM SPSS 28.0 (IBM Corp. Released 2021. IBM SPSS Statistics for Windows, Version 28.0. Armonk, NY: IBM Corp.) statistical package program.
Ethics approval
Ethical permission had been obtained. (Bursa Uludağ University Faculty of Medicine Clinical Research Ethics Committee, Approval no: 2023-24/37).
Results
A total of 44 patients, 19 females, and 25 males, had a median age of 35 (18–53) years during video EEG monitoring. The mean duration of VEM recording was 107.47 ± 47.79 h (patient group 128.22 ± 58.43, control group 86.72 ± 18.09 h). Six patients were on monotherapy, 24 were on dual, and 14 were on three or more anti-seizure medications (12, 19, and 13 in the control group, respectively). Epilepsy syndromes and anti-seizure medications of the patients are given in Table 1. A total of 88 MRIs (44, 44, respectively), 60 FDG PET scans (35 in 31 patients and 25 in 25 patients, respectively), and 82 NPTs (42, 40, respectively (two and four patients did not comply with the tests) were evaluated. The dominant hand (right) was 39 and 41, respectively.
There was no difference for the dominant hand in patients with aLCJ. In patients with ipsilateral automatism and contralateral posture or gustatory and olfactory hallucinations, which are common in temporal lobe epilepsy among other semiologic findings, aLCJ was less or absent. In patients with unilateral tonic activity, aLCJ was more common. (Fig. 2, appendix-1) There was no difference in other semiologic findings. There was no difference in pathologies detected on MRI. (Table 2) aLCJ was slightly more frequent for pathology localization in patients with diffuse/spread or parietal region lesions on MRI. There was no localization difference for PET. For NPT, aLCJ was more frequent in patients with dysfunction in the frontal region than in patients with dysfunction in the temporal region. (Table 3) In the electrophysiological recording, interictal occipital region sharp or spike-wave activation was observed in patients with aLCJ (p = 0.021), while temporal region interictal rhythmic teta or delta wave activation was less frequent (p = 0.017). There was no difference for localization of the initial ictal activity. (Fig. 3, appendix-2) MRI, PET, and NPT ictal EEG were statistically significantly associated with baseline hemispheric activity lateralization. For patients with bilateral or bifocal activation at baseline, the results obtained only in NPT were significant for bilateral involvement. In a total of 40 patients (90.9%) with 18 right and 22 left asymmetric aLCJ, the positive predictive value of aLCJ for ictal EEG activation lateralization was 86.36% (AUC: 0.758, p = 0.002), mostly concurrence (κ = 0.485).
Discussion
The diagnosis of epileptic seizures depends on recognizing the behavioral characteristics of these episodes. The semiology of seizures in epilepsy forms the basis of clinical description. Some semiological features provide essential clues for hemisphere lateralization and lobar localization. However, this alone may not be sufficient; it may be misleading in multifocal epilepsy, or sometimes, it may be a finding of seizure spread rather than seizure onset location. In determining seizure type and localization of onset, EEG and semiology are also very valuable. VEM allows detailed analysis of the semiological features of seizures correlated with simultaneous EEG activity. Especially in temporal and extratemporal epilepsies, observation of seizures with VEM provides essential information for lateralization and localization. However, it is not possible to examine every patient with VEM.
Temporal lobe seizures are the most common site of focal seizures. Usually, aura and psychic symptoms are followed by motor activity. Frontal lobe epilepsies are the most common extratemporal seizures. They usually have sudden onset, short duration, a very short postictal confusion period, and seizures are generally clustered. Different semiologic features are seen according to the onset or location of the seizure. These features may be more frequent or specific in temporal or frontal lobe seizures and have localization or lateralization value. For example, in temporal lobe epilepsy, where auras are more common, elevated epigastric sensation, Fear or joy, déjà, and jamais vu, visceral or auditory illusions, complex auditory or visual hallucinations, and taste or olfactory hallucinations are seen. However, although these auras are usually of localizing value, they do not have lateralizing significance. Findings such as oral or manual automatism, psychic symptoms, ipsilateral automatism and contralateral posture, postictal cough, or ictal speech arrest or preservation during seizures indicate lateralization to the non-dominant hemisphere or localization to the ipsilateral or contralateral temporal lobe. For frontal seizures, tonic–clonic head and eye version, unilateral clonic movements of the face or one of the upper or lower extremities, a slow, involuntary abnormal posture with a rotatory component distal to the upper extremities, unilateral tonic activity, unilateral smile, and four or fencing indicating contralateral lateralization, short-term (2 s) and greater than 30° head version in the first minute of the seizure, unilateral hand automatisms, postictal nose wiping after seizure termination, unilateral blinking at the onset of the seizure, ictal vocalization and asymmetric termination of the clonic phase at the end of the FBTCS evaluated in this article indicate ipsilateral lateralization. (seizure onset hemisphere and long clonic phase are ipsilateral) 7,8,9,10. Since incorrect seizure classification may lead to inappropriate treatment selection or unnecessary investigations, the correct seizure classification should be made first; then, the lateralization value should be interpreted 11.
In our study, the association of aLCJ with ipsilateral automatism and contralateral posture, smell or taste aura, which are more common in temporal lobe epilepsy, and unilateral tonic activity, which is more common in frontal lobe epilepsy, was significant. There was no significant association of aLCJ with other semiologic features. The mechanisms leading to aLCJ need to be clarified and speculative. In focal seizures, it is thought that earlier active inhibition in the hemisphere of seizure onset or earlier depletion in the retained hemisphere may cause this phenomenon 12,13. In our study, there was a significant association of aLCJ with ipsilateral automatism and contralateral posturing or gustatory and olfactory hallucinations, which are common in temporal lobe epilepsies, especially in mesial temporal lobe epilepsy (most commonly sclerosis). This association may be related to abnormally organized neuronal network structures based on the sclerosis of mesial temporal structures over a long period. On the other hand, the significant association we found with unilateral tonic posture, which is more common in frontal lobe epilepsies, may be related to the proximity to the ictal onset localization. However, since there is no difference in the frequency of association with many other semiologic findings, the pathogenesis remains to be elucidated.
Literature studies evaluating the relationship between semiological features and organic pathologies are limited. Our study did not find a significant difference between aLCJ and the MRI pathologies detected in our cohort. However, diffuse/spread or parietal localization on MRI was mildly associated with aLCJ, although we did not find significance for localization on FDG PET. This suggests that diffuse/spread lesions may lead to more depletion in the previously involved hemisphere or that lesions in the parietal region, which are located right next to the seizure onset localization in patients with frontal lobe epilepsy, may be associated with aLCJ by undergoing earlier inhibition.
Notably, interictal temporal slow wave activation is less common in those with aLCJ, and the difference between temporal and frontal localizations for interictal or ictal activation is reduced in favor of frontal. This suggests that aLCJ may be more frequent in frontal lobe epilepsy. The higher frequency of aLCJ in patients with initial activation in the occipital region may be related to the faster spread of occipital lobe epilepsies compared to temporal lobe epilepsies and earlier hemispheric exhaustion 14. However, the small number of patients makes confirmation difficult.
Although advanced invasive examinations and imaging studies have improved considerably, VEM, ictal semiologic findings, and analysis of ictal discharges are still important in epileptic focus detection 15. Asymmetric motor signs in the semiology of FBTCS, such as forced head version, fencing, and aLCJ, have remarkable accuracy for seizure origin lateralization. aLCJ occurs ipsilaterally next to the seizure onset site, and FBTCS of frontal or temporal origin have a high positive predictive value for lateralization 6,7,12. On the other hand, it should be kept in mind that aLCJ can be seen not only in focal onset seizures but also in primary generalized tonic–clonic seizures and even in psychogenic non-epileptic seizures (PNES) (aLCJ was detected in two patients with PNES who were excluded from our study).16 However, epilepsy surgery are currently the gold standard for the confirmation of lateralisation findings. In our cohort, the number of patients with aLCJ who underwent epilepsy surgery during follow-up was too small to be included in the statistical evaluation (n = 8). Therefore, unfortunately, we could not perform this analysis in this study. Nevertheless, the positive predictive value of asymmetric last clonic jerks for ipsilateral lateralisation was 86.36% when evaluated with ictal EEG activation. This result confirms that it is a robust semiological finding for ipsilateral lateralisation. In our study, the positive predictive value of the asymmetric last clonic jerk for ipsilateral lateralization was 86.36%. This result confirms that it is a robust semiological finding for ipsilateral lateralization.
Conclusion
In patients with refractory epilepsy, seizure semiology is very important in combination with neuroimaging and neuropsychometric tests for accurate seizure classification, appropriate anti-seizure medication or appropriate treatment modality. VEM may not be suitable for evaluating all patients, or data may not be obtained during hospitalization. In this context, the asymmetric last clonic beat is precious for lateralization of FBTCS and should be considered. Its presence strongly lateralizes to the side of seizure onset.
Study limitation
In this study, we did not perform a retrospective evaluation for poor/good surgical outcomes because the proportion of patients with asymmetric last clonic jerk who underwent epilepsy surgery was small. The main limitations of the study are the small number of patients, the fact that the findings were obtained from EEG examinations with superficial electrodes and were not confirmed by surgery, which has recently been the gold standard. Especially in patients with rapid generalization, muscle artifacts may be confusing as they may obscure the onset and propagation pattern. However, despite this, the PPV was found to be high, indicating that the result is robust.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Chee, M. W. et al. Lateralizing signs in intractable partial epilepsy: Blinded multiple-observer analysis. Neurology 43(12), 2519–2525 (1993).
Marks, W. J. & Laxer, K. D. Semiology of temporal lobe seizures: Value in lateralizing the seizure focus. Epilepsia 39(7), 721–726 (1998).
Janszky, J. et al. Lateralizing value of unilateral motor and somatosensory manifestations in frontal lobe seizures. Epilepsy Res. 43(2), 125–133 (2001).
Bonelli, S. B. & Baumgartner, C. Frontal lobe epilepsy–clinical seizure seminology. Wien Klin. Wochenschr. 114(8–9), 334–340 (2002).
Kotagal, P. et al. Lateralizing value of asymmetric tonic limb posturing observed in secondarily generalized tonic-clonic seizures. Epilepsia 41(4), 457–462 (2000).
Trinka, E. et al. Asymmetric termination of secondarily generalized tonic-clonic seizures in temporal lobe epilepsy. Neurology 59(8), 1254–1256 (2002).
Bonelli, S. B. et al. Clinical seizure lateralization in frontal lobe epilepsy. Epilepsia 48(3), 517–523 (2007).
Blair, R. D. Temporal lobe epilepsy semiology. Epilepsy Res. Treat. 2012, 751510 (2012).
Chowdhury, F. A. et al. Localisation in focal epilepsy: A practical guide. Pract. Neurol. 21(6), 481–491 (2021).
Christie, H. et al. Can semiology differentiate between bilateral tonic-clonic seizures of focal-onset and generalized-onset? A systematic review. Epilepsy Behav. 116, 107769 (2021).
Chin, P. S. & Miller, J. W. Ictal head version in generalized epilepsy. Neurology 63(2), 370–372 (2004).
Jobst, B. C. et al. Secondarily generalized seizures in mesial temporal epilepsy: Clinical characteristics, lateralizing signs, and association with sleep-wake cycle. Epilepsia 42(10), 1279–1287 (2001).
Leutmezer, F., Lurger, S. & Baumgartner, C. Focal features in patients with idiopathic generalized epilepsy. Epilepsy Res. 50(3), 293–300 (2002).
Blume, W. T., Wiebe, S. & Tapsell, L. M. Occipital epilepsy: Lateral versus mesial. Brain 128(Pt 5), 1209–1225 (2005).
Dupont, S. et al. Lateralizing value of semiology in medial temporal lobe epilepsy. Acta Neurol. Scand. 132(6), 401–409 (2015).
KoÇ, G. et al. Comparison of semiologic characteristics of psychogenic nonepileptic seizures and frontal and temporal lobe seizures. Neurol. Sci. Neurophysiol. (Online) 39(3), 126–131 (2022).
Acknowledgements
We would like to thank our technicians Sefer Sert and Nursen Satik for their contributions during the data collection phase of the study and Prof. Guven Ozkaya for statistical analysis consultancy.
Author information
Authors and Affiliations
Contributions
Author Contribution: Concepts: F.S; Design: F.S., Y.D. ; Supervision: A.B.D; Resources: A.B.D., I.B.; Materials: G.M., F.S. ; Data Collection and Processing: G.M., F.S. ; Analysis and interpretation: F.S. ; Literature Research: F.S., Y.D. ; Writing Manuscript: F.S. ; Critical Review: A.B.D., I.B.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Saridas, F., Mesut, G., Dinc, Y. et al. Lateralizing value and clinicoradiological features of asymmetric last clonic jerks in temporal and extratemporal epilepsy. Sci Rep 14, 11578 (2024). https://doi.org/10.1038/s41598-024-61401-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-61401-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.