Abstract
This mediation analysis aimed to investigate the associations among areal bone mineral density, mobility-related brain atrophy, and specific gait patterns. A total of 595 participants from the Taizhou Imaging Study, who underwent both gait and bone mineral density measurements, were included in this cross-sectional analysis. We used a wearable gait tracking device to collect quantitative gait parameters and then summarized them into independent gait domains with factor analysis. Bone mineral density was measured in the lumbar spine, femoral neck, and total hip using dual-energy X-ray absorptiometry. Magnetic resonance images were obtained on a 3.0-Tesla scanner, and the volumes of brain regions related to mobility were computed using FreeSurfer. Lower bone mineral density was found to be associated with higher gait variability, especially at the site of the lumbar spine (β = 0.174, FDR = 0.001). Besides, higher gait variability was correlated with mobility-related brain atrophy, like the primary motor cortex (β = 0.147, FDR = 0.006), sensorimotor cortex (β = 0.153, FDR = 0.006), and entorhinal cortex (β = 0.106, FDR = 0.043). Bidirectional mediation analysis revealed that regional brain atrophy contributed to higher gait variability through the low lumbar spine bone mineral density (for the primary motor cortex, P = 0.018; for the sensorimotor cortex, P = 0.010) and the low lumbar spine bone mineral density contributed to higher gait variability through the primary motor and sensorimotor cortices (P = 0.026 and 0.010, respectively).
Similar content being viewed by others
Introduction
Gait disorder is a common problem among community-dwelling older adults and primarily affects the quality of their lives1,2. The nervous and skeletal muscle systems play crucial roles in gait function3,4, and brain atrophy and osteoporosis are prevalent in old age. Previous research has shown that volume loss in brain regions responsible for mobility-related functions showed discrepancies in associations with poorer gait performances5,6,7. Specific gait performances have been identified as novel markers for detecting individuals with low bone mineral density (BMD)8. Moreover, poor gait performances are related to areal BMD9,10. However, the combined impact of mobility-related brain atrophy and low BMD at specific sites on gait remains unclear. Understanding the underlying mechanisms is crucial for developing interventions to enhance gait performance in the aging population.
Many studies found that brain atrophy and low BMD were not wholly independent, with clinical and molecular evidence suggesting biological similarities and interactions between bone and brain11,12,13. The atrophy of the cerebral cortex in Alzheimer's disease patients has been linked to morphometric changes in the cortical microvascular network, where vascular smooth muscle is composed of collagen I14. Type I collagen, a key component of bone, is closely related to skeletal abnormalities15. Epidemiological evidence indicates a coexistence of brain and bone degeneration in the elderly population. Patients with cognitive impairment, especially those with Alzheimer's disease, are at greater risk for osteoporosis16, and BMD continues to decrease as the severity of cognitive impairment increases17. A recent Mendelian randomization study also demonstrated a causal relationship between atrophy in different brain regions and low bone density in specific areas18. Specifically, the bone–brain axis involves bidirectional communication between the brain and bone tissues. For one thing, neural tissues can produce neurokines that signal down from the brain to bone cells, promoting skeletal homeostasis and regeneration19. Animal experiments have proved that proangiogenic factor SLIT3, a contributor to the positive regulation of bone formation, would influence bone mass20. But brain atrophy may lead to a reduction in neural factor release. Widespread loss of neurotransmitters has been observed in patients with common neurodegenerative disorders21. Such depletion of neural factors may result from the neuronal loss caused by brain atrophy. Meanwhile, osteoporosis, one condition involving inflammation, may affect the survival and activity of osteocytes by inducing the secretion of proinflammatory cytokines and growth factors22. Some bone-derived osteokines can cross the blood–brain barrier to reach the central nervous system and affect nerve cells19. Lipocalin2 (LCN2), osteopontin (OPN), and insulin-like growth factor 1 (IGF-1) were found to be associated with brain atrophy in a region-specific manner23,24,25. We hypothesize that the reciprocal reinforcement between regional brain atrophy and low BMD might be one mechanism causing specific poor gait performances.
In this population-based study, we investigated the associations of gait performances with low BMD at specific sites and mobility-related brain atrophy. Our study aimed to explore whether brain atrophy and low BMD could mediate each other’s effects on gait performances, shedding light on the potential mechanisms through which bone and brain impact gait.
Methods
Study population
This cross-sectional study is based on the Taizhou Imaging Study (TIS), an ongoing community-based cohort study. The inclusion and exclusion criteria for the baseline population have been described in detail in our previous study26. Ethical approval for the TIS was obtained from the Ethics Committee of the School of Life Sciences, Fudan University, and Fudan University Taizhou Institute of Health Sciences (Institutional Review Board approval numbers: 496 and B017, respectively). There are two approval numbers because our subjects were recruited in two phases at baseline. Specifically, in phase I, 562 participants (mean age 59.1 years, 46.0% male) were recruited from two villages (Lubao and Hutou). In phase II, 342 subjects (mean age 60.9 years, 42.1% male) were from Caixiang Village. Among the 904 individuals in TIS, 622 participants had complete magnetic resonance imaging (MRI) data, quantitative gait data, and BMD data. After excluding pre-or perimenopausal women and individuals with a history of fracture and thyroid disease, 595 participants, comprising 266 men and 329 postmenopausal women, were finally included in the current analysis. The inclusion and exclusion process is illustrated in Fig. S1. Written informed consent was obtained from all participants before data and biospecimen collection. All methods included in this study were performed in accordance with the Declaration of Helsinki and its later amendments.
Measurement of gait
A gait tracking device embedded in insoles (Senno gait, Sennotech Co. Ltd., China) was employed to obtain quantitative gait data in multiple dimensions. After placing the insoles comfortably in their shoes, participants were instructed to walk 20 m forth and back in a straight line at their accustomed pace. Vast gait parameters for each stride were recorded and analyzed throughout the procedure, with the gait tracking device automatically excluding the turning strides. The quantitative gait parameters measured included stride time, stance time, swing time, stance time percentage of the gait cycle (%GC) symmetry, swing time (%GC) symmetry, stride time symmetry, stride time coefficient of variation (CV), stance time CV, swing time CV, heel strike angle, stride length, maximum swing velocity, gait velocity, stance time (%GC), and double support time (%GC). Table S1 provides the definitions of each gait parameter and indicates the direction in which a parameter is considered “poorer”. Given that gait velocity is a commonly used measure of overall gait quality, the participants were categorized into two groups based on their gait velocity: the impaired gait group (< 1.0 m/s) and the unimpaired gait group (≥ 1.0 m/s)27.
Measurement of BMD
BMD measurements were conducted at three sites: the lumbar spine, the femoral neck, and the total hip on the left side, using a dual-energy X-ray absorptiometry (Lunar DPX NT-400157; GE Healthcare, Madison, WI, USA). All measurements were assessed by the same experienced operator on the same machine, according to standardized procedures for participant positioning. BMD values were recorded in grams per square centimeter (g/cm2). The lumbar spine BMD included the first, second, third, and fourth lumbar vertebra (L1–L4), and the total hip BMD included the whole hip bone. According to the World Health Organization, participants were divided into the normal BMD (T-score ≥ − 1.0), osteopenia (− 1.0 < T-score < − 2.5), or osteoporosis (T-score ≤ − 2.5) groups28. These diagnoses were defined with the minimum T-score of three measuring positions.
MRI acquisition and measurements
MRI scans were conducted at Taizhou People’s Hospital using a 3.0 T scanner (Magnetom Verio Tim scanner; Siemens, Erlangen, Germany). The detailed protocol and sequence parameters for MRI have been previously reported29. Based on previous studies, we selected specific brain regions associated with mobility as regions of interest5,30. Fifteen mobility-related regions of interest were as follows: motor function (primary motor, sensorimotor), visuospatial attention (inferior posterior parietal lobules, superior posterior parietal lobules), executive control function (dorsolateral prefrontal cortex, anterior cingulate), cognition (hippocampus, entorhinal cortex), motor imagery (precuneus, parahippocampus, posterior cingulated cortex), and balance (pallidum, putamen, caudate, thalamus). FreeSurfer software (v6.0.0) was used to extract these regional volumes from structural T1 images, utilizing the Desikan–Killiany atlas31. All brain region volumes were standardized using z-scores for analysis.
Co-variables
Demographic and lifestyle characteristics data were collected using a questionnaire comprehensively containing age, sex, smoking habits, alcohol and tea consumption, and physical activity. Physical data (height, weight, waist and hip circumferences) were obtained through physical examinations26. Waist-to-Hip Ratio (WHR) was calculated by dividing the waist circumference by the hip circumference. Medical history, including hypertension, diabetes, and hyperlipidemia, was defined as the following criteria. Hypertension was defined as a blood pressure greater than 140/90 mmHg, a self-reported history, or current use of antihypertensive drugs. Diabetes was defined as fasting blood glucose greater than 7.0 mmol/L, a self-reported history, or current use of anti-diabetic drugs. Hyperlipidemia was defined as total cholesterol greater than 5.2 mmol/L, triglyceride greater than 1.7 mmol/L, a self-reported history, or current use of antihyperlipidemic drugs.
Statistical analysis
Description analysis
Continuous variables were reported as mean (standard deviation, SD), and categorical variables were presented as frequencies (%). The normality of continuous variables was assessed using the Shapiro–Wilk test, and Levene's test evaluated the homogeneity of variance. Logarithmic transformation was applied to the symmetry gait variables (Fig. S2), whereas square root transformation was applied to the variability gait variables (Fig. S3). Group differences in gait velocity were examined using the following tests: the two-sample t-test or Wilcoxon rank sum test for continuous variables and Pearson's chi-squared test or Fisher's exact test for categorical variables.
Factor analysis of quantitative gait parameters
The original variables in the rhythm, symmetry, variability, and phase domains were inverted, representing poorer gait performances with lower values. To extract independent factors with an eigenvalue > 1, fifteen quantitative gait parameters were orthogonally rotated using the “Varimax” rotation method. Gait parameters were then categorized into independent domains based on correlation loadings and the extracted factors. These factors were standardized and expressed as z-scores for further analysis.
Association analysis
General linear models were employed to investigate the associations among BMD, mobility-related brain regions, and gait performances. The regression analysis, which evaluated the associations of gait performances with BMD and brain volumes, was fitted in two models: Model 1 was adjusted for age, sex, height, and standardized total intracranial volume (included in the analysis of brain volumes); Model 2 was further adjusted for WHR, hypertension, diabetes, hyperlipidemia, tea consumption, smoking, alcohol consumption, and physical activity. A linear trend test was conducted to assess the association between BMD groups and gait domains by scoring the BMD groups from 0 (normal) to 2 (osteoporosis) and entering the score as a continuous term in the regression model. Multiple testing problem was corrected by the false discovery rate (FDR) method.
Mediation analysis
Two mediation models were fitted with gait performances as the dependent variables for both. In the first set of models, brain atrophy was inserted as the independent variable, with BMD as the candidate mediator. Conversely, in the second set of models, BMD was inserted as the independent variable, while brain atrophy served as the candidate mediator. The mediation analysis was conducted utilizing the R package (mediation) with 1,000 repetitions. Additionally, a sensitivity analysis of mediation was conducted using the R package “medsens” to explore the potential influence of unmeasured confounders on the assumption and assess the robustness of the results, represented as ρ. The threshold of statistical significance was set at adjusted two-tailed P < 0.05. Statistical analyses were performed using R software (Version 4.2.2).
Ethical approval
The studies involving human participants were reviewed and approved by the Ethics Committee of the School of Life Sciences, Fudan University, and Fudan University Taizhou Institute of Health Sciences (institutional review board Approval Number: 496 and B017, respectively). The patients/participants provided their written informed consent to participate in this study.
Results
Characteristics of the study population
Table 1 presents the demographic, cardiovascular risk factors, neuroimaging, gait, and BMD characteristics of our participants. The impaired gait group and unimpaired gait group comprised 23.2% and 76.8% of the sample. The two groups differed in sex, age, height, and tea consumption (P < 0.05). In addition, participants with impaired gait velocity exhibited smaller gray matter volumes and poorer gait performance, such as maximum swing velocity, heel strike angle, and double support time.
Associations between gait domains and different BMD groups
Quantitative gait parameters were summarized into five independent domains with factor analysis, which accounted for 84.70% of the total variance (Table S2). Referring to previous studies32,33,34, we categorized them as rhythm domain (stride time, stance time, swing time), phase domain (double support time percentage of the gait cycle, stance time percentage of the gait cycle), symmetry domain (stance time percentage of the gait cycle symmetry, swing time percentage of the gait cycle symmetry, stride time symmetry), variability domain (stance time coefficient of variation, swing time coefficient of variation, stride time coefficient of variation), and pace domain (stride length, maximum swing velocity, heel strike angle, gait velocity).
The associations between gait domains and BMD groups were examined (Table S3). Figure 1 shows mean standardized z-scores for gait variability in different groups. After full adjustment (Model 2), we observed a trend (P = 0.004) in gait variability across different groups, indicating that participants with lower BMD may exhibit higher variability when walking. However, no statistically significant association was observed in other gait domains, such as rhythm, symmetry, pace, and phase.
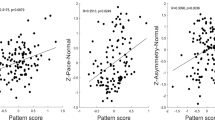
Associations between gait domains and areal BMD
Considering that different anatomical parts of bones have distinct physiological effects during walking, we further studied the influence of BMD of different anatomical parts on gait variability. Figure 2 shows the associations of various gait domains with areal BMDs (the lumbar spine BMD, the femoral neck BMD, and the total hip BMD) as the independent variables. Lower lumbar spine BMD exhibited a significant association with higher gait variability, a relationship that remained statistically significant even after full adjustment (FDR = 0.001). The negative associations of the phase domain with the femoral neck BMD and the total hip BMD were also significant after correction (both FDR < 0.05).
Associations between gait domains and mobility-related brain regions
After full adjustment, higher gait variability was significantly associated with smaller volumes in the primary motor (β = 0.147, FDR = 0.006), sensorimotor (β = 0.153, FDR = 0.006), and entorhinal cortex (β = 0.106, FDR = 0.043) (Table 2). Additionally, the pace domain exhibited significant associations with the primary motor (β = 0.263, FDR < 0.001), sensorimotor (β = 0.210, FDR < 0.001), visuospatial attention (β = 0.170, FDR < 0.001), executive control function (β = 0.146, FDR = 0.005), entorhinal cortex (β = 0.155, FDR < 0.001), motor imagery (β = 0.262, FDR < 0.001), and basal ganglia (β = 0.166, FDR = 0.006) regions. Moreover, we also found the associations of the rhythm domain with the primary motor (β = 0.109, FDR = 0.047) and sensorimotor (β = 0.103, FDR = 0.047) cortex were borderline significant after full adjustment (Table S4). However, no statistically significant association was observed between mobility-related brain regions and the symmetry and phase domains (Table S4).
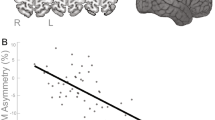
Mediation analysis
Bidirectional mediation analysis was conducted to assess the combined impact of lumbar spine BMD and mobility-related brain atrophy on gait variability. The findings indicated that the atrophy of mobility-related brain regions, such as the primary motor cortex and sensorimotor cortex, may contribute to higher gait variability by decreasing the lumbar spine BMD (Fig. 3a). Specifically, the lumbar spine BMD explained 11.8% of the total effect of the primary motor cortex on gait variability (Pmediation = 0.018) and 10.6% of the total effect of the sensorimotor cortex on gait variability (Pmediation = 0.010). Furthermore, the reverse mediation analyses revealed that the lumbar spine BMD could also influence the gait variability through the two brain regions (Fig. 3b). The mediating effect of the primary motor cortex represented 8.2% (Pmediation = 0.026), while that of the sensorimotor cortex accounted for 8.3% (Pmediation = 0.010). Additional detailed information was provided in Tables S5 and S6.
Sensitivity analysis
We conducted sensitivity analyses to assess the potential impact of unmeasured confounding. The results in Tables S7 and S8 indicated that the estimated indirect effects were relatively robust to unmeasured confounders, as indicated by the sensitivity parameter (ρ).
Discussion
This study found evidence for a bidirectional relationship between BMD and brain atrophy concerning gait variability. Specifically, we found that the lumbar spine BMD partially mediated the effects of the primary motor cortex and sensorimotor cortex on gait variability, and the primary motor cortex and the sensorimotor cortex partially mediated the effect of the lumbar spine BMD on gait variability. Although our results showed a small-to-medium range of effect sizes, we consider it reasonable because the role of a single anatomical site of the brain and bone is limited.
Previous studies have indicated a link between brain atrophy and gait variability. Specifically, a meta-analysis of 25 studies found a strong association between high gait variability and neurodegeneration35. Compared to other gait domains, variability can help to differentiate Alzheimer's disease dementia, a common neurodegenerative disorder, which can be observed atrophy in specific brain regions36. Notably, higher step length variability is associated with the atrophy of the hippocampus, superior parietal lobe, and anterior cingulate gyrus, regions responsible for cognition and executive control that matter in mobility7. Similarly, our research has corroborated these findings, showing that brain atrophy affecting motor function and cognition, including areas like the primary motor cortex, sensorimotor cortex, and entorhinal cortex, is associated with higher gait variability. However, to our knowledge, no existing studies have investigated the potential impact of brain atrophy on gait performance through BMD. The following evidence supports our finding that the lumbar spine BMD can explain the effect of mobility-related brain atrophy on gait variability. First, higher gait variability seems to be a shared gait performance between individuals with brain atrophy and those with lower BMD. Besides, based on the bone–brain axis, brain atrophy may directly affect central control of bone remodeling, thus resulting in low BMD37. A recent Mendelian randomization study has further supported these relationships by establishing causal links between the atrophy of specific brain regions and BMD at distinct sites18. Our results provided evidence of the mediating effect of BMD on the association between brain atrophy and gait.
Likewise, the potential mediating role of brain atrophy between BMD and gait performance has not been studied. Previous studies have indicated an association between low BMD and mobility impairment, such as balance, variability, and symmetry38,39,40. This may be attributed to less propulsion and stability caused by abnormal changes in kinematics and kinetics parameters of the trunk or extremities41. Such associations between specific physical performances and areal BMD were informed before10,42. Similarly, we found a significant association between low lumbar spine BMD and higher gait variability and the mediating role of mobility-related brain atrophy. Although there are no direct comparisons available for our specific findings, existing evidence indirectly supports our findings. First, some elderly-based studies have observed that individuals with osteoporosis tend to exhibit greater parenchymal atrophy and significant ventricular enlargement and that BMD loss was correlated with regional gray matter volume decline43,44. Second, patients with osteoporotic vertebral compression fractures were found to have smaller volumes of brain parenchyma45, which emphasizes the association of the lumbar spine BMD with brain atrophy. Finally, insights from the bone–brain axis suggest that osteokines, like IGF-1, could help improve behavioral phenotypes in mouse models46 and have also been associated with gait speed in older adults47.
Lumbar BMD was observed to have a more substantial impact on gait variability compared to femoral neck and total hip BMD. This is likely attributed to several factors. Firstly, potential vertebral compression fractures could be a contributing factor. Patients suffering from vertebral compression fractures may experience varying degrees of lower back pain, resulting in reduced lumbar extensor function and increased gait variability48. Lumbar acceleration was also identified as being more indicative of gait stability. In terms of biomechanics, the stability of the human body during walking primarily depends on the ability to regulate the movement of the center of mass (COM)49, typically situated at the junction of the waist and pelvis of the human body50.
Our study contributes to the existing literature by examining and providing evidence for the bidirectional relationship between areal BMD, regional brain atrophy, and their combined effects on gait variability in elderly adults. To enhance the sensitivity of gait assessments, we employed a quantitative approach using an insole-style wearable gait tracking device, addressing limitations of commonly used qualitative or semi-quantitative methods. The gait parameters collected were categorized into distinct domains representing specific gait patterns in our study. Gait variability assessment can serve as a valuable tool for potentially identifying elderly individuals with low lumbar BMD or reduced motor cortex volume. By detecting these conditions early, interventions targeting bone and brain degeneration processes can be initiated, ultimately delaying their progression and promoting increased years of healthy living. Moreover, gait variability assessment can also play a role in evaluating the efficacy of bone and brain health care for patients, offering valuable insights to guide treatment strategies and rehabilitation efforts to enhance physical function.
However, our results should be interpreted in light of several limitations. First, causal conclusions cannot be drawn in this cross-sectional study. Further investigation using longitudinal designs of TIS would be valuable to help rectify this limitation. Second, our sample is a Chinese rural population around 60 years old, potentially limiting the generalizability of our findings to other population groups. Future research could involve individuals in our expanded cohort to enhance external validity. Third, potential back pain resulting from vertebral compression fractures was not taken into account51,52. In the future, we will consider adding a measurement of vertebral compression fractures and related pain severity when conducting the DXA examination. Finally, muscular factors were not considered in the present study. Including these factors in future studies would provide a more comprehensive understanding of gait.
Conclusion
The present study indicates that brain atrophy, especially mobility-related brain regions, and low BMD in the lumbar spine are associated with higher gait variability. Importantly, bidirectional mediation analysis conducted for the first time identifies the interrelationship between mobility-related brain atrophy and low lumbar spine BMD in gait variability. However, additional extensive population studies and longitudinal investigations are required to validate our findings and provide a more comprehensive understanding of the effects of brain and bone on gait changes in more detail.
Data availability
The datasets used and/or analyzed in this study are available from the corresponding author on reasonable request.
References
Mahlknecht, P. et al. Prevalence and burden of gait disorders in elderly men and women aged 60–97 years: A population-based study. PLoS ONE 8, e69627. https://doi.org/10.1371/journal.pone.0069627 (2013).
Pieruccini-Faria, F. & Montero-Odasso, M. Obstacle negotiation, gait variability, and risk of falling: Results from the “Gait and Brain Study”. J. Gerontol. A Biol. Sci. Med. Sci. 74, 1422–1428. https://doi.org/10.1093/gerona/gly254 (2019).
Pirker, W. & Katzenschlager, R. Gait disorders in adults and the elderly : A clinical guide. Wien Klin Wochenschr 129, 81–95. https://doi.org/10.1007/s00508-016-1096-4 (2017).
Snijders, A. H., van de Warrenburg, B. P., Giladi, N. & Bloem, B. R. Neurological gait disorders in elderly people: Clinical approach and classification. Lancet Neurol. 6, 63–74. https://doi.org/10.1016/s1474-4422(06)70678-0 (2007).
DiSalvio, N. L. et al. Gray matter regions associated with functional mobility in community-dwelling older adults. J. Am. Geriatr. Soc. 68, 1023–1028. https://doi.org/10.1111/jgs.16309 (2020).
Rosano, C., Aizenstein, H. J., Studenski, S. & Newman, A. B. A regions-of-interest volumetric analysis of mobility limitations in community-dwelling older adults. The journals of gerontology. Ser. A Biol. Sci. Med. Sci. 62, 1048–1055. https://doi.org/10.1093/gerona/62.9.1048 (2007).
Rosso, A. L. et al. Higher step length variability indicates lower gray matter integrity of selected regions in older adults. Gait Posture 40, 225–230. https://doi.org/10.1016/j.gaitpost.2014.03.192 (2014).
Kim, J. K., Bae, M. N., Lee, K., Kim, J. C. & Hong, S. G. Explainable artificial intelligence and wearable sensor-based gait analysis to identify patients with osteopenia and sarcopenia in daily life. Biosensors (Basel) 12, 167. https://doi.org/10.3390/bios12030167 (2022).
Hauger, A. V. et al. Physical capability, physical activity, and their association with femoral bone mineral density in adults aged 40 years and older: The Tromsø study 2015–2016. Osteoporos. Int. 32, 2083–2094. https://doi.org/10.1007/s00198-021-05949-9 (2021).
Taaffe, D. R. et al. Lower extremity physical performance and hip bone mineral density in elderly black and white men and women: cross-sectional associations in the Health ABC study. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 58, M934-942. https://doi.org/10.1093/gerona/58.10.m934 (2003).
Saboori, P. & Sadegh, A. Histology and morphology of the brain subarachnoid trabeculae. Anat. Res. Int. 2015, 279814. https://doi.org/10.1155/2015/279814 (2015).
Idelevich, A. & Baron, R. Brain to bone: What is the contribution of the brain to skeletal homeostasis?. Bone 115, 31–42. https://doi.org/10.1016/j.bone.2018.05.018 (2018).
Obri, A., Khrimian, L., Karsenty, G. & Oury, F. Osteocalcin in the brain: From embryonic development to age-related decline in cognition. Nat. Rev. Endocrinol. 14, 174–182. https://doi.org/10.1038/nrendo.2017.181 (2018).
Richard, E. et al. Morphometric changes in the cortical microvascular network in Alzheimer’s disease. J. Alzheimer’s Dis. JAD 22, 811–818. https://doi.org/10.3233/jad-2010-100849 (2010).
Marini, J. C. et al. Osteogenesis imperfecta. Nat. Rev. Dis. Primers 3, 17052. https://doi.org/10.1038/nrdp.2017.52 (2017).
Xie, C., Wang, C. & Luo, H. Increased risk of osteoporosis in patients with cognitive impairment: A systematic review and meta-analysis. BMC Geriatr. 23, 797. https://doi.org/10.1186/s12877-023-04548-z (2023).
Lin, S. F., Fan, Y. C., Pan, W. H. & Bai, C. H. Bone and lean mass loss and cognitive impairment for healthy elder adults: Analysis of the nutrition and health survey in Taiwan 2013–2016 and a validation study with structural equation modeling. Front. Nutr. 8, 747877. https://doi.org/10.3389/fnut.2021.747877 (2021).
Guo, B. et al. Causal associations of brain structure with bone mineral density: A large-scale genetic correlation study. Bone Res. 11, 37. https://doi.org/10.1038/s41413-023-00270-z (2023).
Schurman, C. A. et al. Molecular and cellular crosstalk between bone and brain: Accessing bidirectional neural and musculoskeletal signaling during aging and disease. J. Bone metab. 30, 1–29. https://doi.org/10.11005/jbm.2023.30.1.1 (2023).
Xu, R. et al. Targeting skeletal endothelium to ameliorate bone loss. Nat. Med. 24, 823–833. https://doi.org/10.1038/s41591-018-0020-z (2018).
Alisky, J. M. Neurotransmitter depletion may be a cause of dementia pathology rather than an effect. Med. Hypotheses 67, 556–560. https://doi.org/10.1016/j.mehy.2006.02.043 (2006).
Kitaura, H. et al. Osteocyte-related cytokines regulate osteoclast formation and bone resorption. Int. J. Mol. Sci. 21, 5169. https://doi.org/10.3390/ijms21145169 (2020).
Unno, K. et al. Theanine, the main amino acid in tea, prevents stress-induced brain atrophy by modifying early stress responses. Nutrients 12, 174. https://doi.org/10.3390/nu12010174 (2020).
Chai, Y. L. et al. Plasma osteopontin as a biomarker of Alzheimer’s disease and vascular cognitive impairment. Sci. Rep. 11, 4010. https://doi.org/10.1038/s41598-021-83601-6 (2021).
Westwood, A. J. et al. Insulin-like growth factor-1 and risk of Alzheimer dementia and brain atrophy. Neurology 82, 1613–1619. https://doi.org/10.1212/wnl.0000000000000382 (2014).
Jiang, Y. et al. Lifestyle, multi-omics features, and preclinical dementia among Chinese: The Taizhou Imaging Study. Alzheimer’s Dementia J. Alzheimer’s Assoc. 17, 18–28. https://doi.org/10.1002/alz.12171 (2021).
Cesari, M. et al. Prognostic value of usual gait speed in well-functioning older people–results from the health, aging and body composition study. J. Am. Geriatr. Soc. 53, 1675–1680. https://doi.org/10.1111/j.1532-5415.2005.53501.x (2005).
Kanis, J. A. et al. A reference standard for the description of osteoporosis. Bone 42, 467–475. https://doi.org/10.1016/j.bone.2007.11.001 (2008).
Wang, Y. et al. Deep/mixed cerebral microbleeds are associated with cognitive dysfunction through thalamocortical connectivity disruption: The Taizhou Imaging Study. Neuroimage Clin. 22, 101749. https://doi.org/10.1016/j.nicl.2019.101749 (2019).
Rosano, C. et al. Patterns of focal gray matter atrophy are associated with bradykinesia and gait disturbances in older adults. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 67, 957–962. https://doi.org/10.1093/gerona/glr262 (2012).
Wang, Y. et al. Cross-sectional associations between cortical thickness and independent gait domains in older adults. J. Am. Geriatr. Soc. 70, 2610–2620. https://doi.org/10.1111/jgs.17840 (2022).
Darweesh, S. K. L. et al. Quantitative gait, cognitive decline, and incident dementia: The Rotterdam study. Alzheimer’s Dementia J. Alzheimer’s Assoc. 15, 1264–1273. https://doi.org/10.1016/j.jalz.2019.03.013 (2019).
Verlinden, V. J. et al. Gait patterns in a community-dwelling population aged 50 years and older. Gait Posture 37, 500–505. https://doi.org/10.1016/j.gaitpost.2012.09.005 (2013).
Hollman, J. H., McDade, E. M. & Petersen, R. C. Normative spatiotemporal gait parameters in older adults. Gait Posture 34, 111–118. https://doi.org/10.1016/j.gaitpost.2011.03.024 (2011).
Moon, Y., Sung, J., An, R., Hernandez, M. E. & Sosnoff, J. J. Gait variability in people with neurological disorders: A systematic review and meta-analysis. Hum. Mov. Sci. 47, 197–208. https://doi.org/10.1016/j.humov.2016.03.010 (2016).
Pieruccini-Faria, F. et al. Gait variability across neurodegenerative and cognitive disorders: Results from the Canadian Consortium of Neurodegeneration in Aging (CCNA) and the gait and brain study. Alzheimer’s Dementia J. Alzheimer’s Assoc. 17, 1317–1328. https://doi.org/10.1002/alz.12298 (2021).
Zaidi, M. Skeletal remodeling in health and disease. Nat. Med. 13, 791–801. https://doi.org/10.1038/nm1593 (2007).
Mendy, A. et al. Low bone mineral density is associated with balance and hearing impairments. Ann. Epidemiol. 24, 58–62. https://doi.org/10.1016/j.annepidem.2013.10.012 (2014).
Palombaro, K. M. et al. Gait variability detects women in early postmenopause with low bone mineral density. Phys. Ther. 89, 1315–1326. https://doi.org/10.2522/ptj.20080401 (2009).
Takano, Y. et al. Assessment of gait symmetry in Elderly women with low bone mineral density using a portable trunk accelerometer: A pilot study. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 25, 6669–6674. https://doi.org/10.12659/msm.916763 (2019).
Eldeeb, A. M. & Khodair, A. S. Three-dimensional analysis of gait in postmenopausal women with low bone mineral density. J. Neuroeng. Rehabilit. 11, 55. https://doi.org/10.1186/1743-0003-11-55 (2014).
Lindsey, C., Brownbill, R. A., Bohannon, R. A. & Ilich, J. Z. Association of physical performance measures with bone mineral density in postmenopausal women. Arch. Phys. Med. Rehabilit. 86, 1102–1107. https://doi.org/10.1016/j.apmr.2004.09.028 (2005).
Bae, I. S., Kim, J. M., Cheong, J. H., Ryu, J. I. & Han, M. H. Association between bone mineral density and brain parenchymal atrophy and ventricular enlargement in healthy individuals. Aging 11, 8217–8238. https://doi.org/10.18632/aging.102316 (2019).
Takano, Y. et al. Voxel-based morphometry reveals a correlation between bone mineral density loss and reduced cortical gray matter volume in Alzheimer’s disease. Front. Aging Neurosci. 12, 178. https://doi.org/10.3389/fnagi.2020.00178 (2020).
Bae, I. S., Kim, J. M., Cheong, J. H., Han, M. H. & Ryu, J. I. Association between cerebral atrophy and osteoporotic vertebral compression fractures. PLoS One 14, e0224439. https://doi.org/10.1371/journal.pone.0224439 (2019).
Eleftheriadou, I. et al. αCAR IGF-1 vector targeting of motor neurons ameliorates disease progression in ALS mice. Ann. Clin. Transl. Neurol. 3, 752–768. https://doi.org/10.1002/acn3.335 (2016).
Waters, D. L., Vlietstra, L., Qualls, C., Morley, J. E. & Vellas, B. Sex-specific muscle and metabolic biomarkers associated with gait speed and cognitive transitions in older adults: A 9-year follow-up. Geroscience 42, 585–593. https://doi.org/10.1007/s11357-020-00163-7 (2020).
Steele, J., Bruce-Low, S., Smith, D., Jessop, D. & Osborne, N. Lumbar kinematic variability during gait in chronic low back pain and associations with pain, disability and isolated lumbar extension strength. Clin. Biomech. 29, 1131–1138. https://doi.org/10.1016/j.clinbiomech.2014.09.013 (2014).
Kurz, M. J., Arpin, D. J. & Corr, B. Differences in the dynamic gait stability of children with cerebral palsy and typically developing children. Gait Posture 36, 600–604. https://doi.org/10.1016/j.gaitpost.2012.05.029 (2012).
Biondi, G., Mauro, S., Mohtar, T., Pastorelli, S. & Sorli, M. in 2015 IEEE Metrology for Aerospace (MetroAeroSpace). 265–270.
Nishi, Y., Shigetoh, H., Fujii, R., Osumi, M. & Morioka, S. Changes in trunk variability and stability of gait in patients with chronic low back pain: Impact of laboratory versus daily-living environments. J. Pain Res. 14, 1675–1686. https://doi.org/10.2147/jpr.S310775 (2021).
Urrutia, J., Besa, P. & Piza, C. Incidental identification of vertebral compression fractures in patients over 60 years old using computed tomography scans showing the entire thoraco-lumbar spine. Arch. Orthop. Trauma Surg. 139, 1497–1503. https://doi.org/10.1007/s00402-019-03177-9 (2019).
Acknowledgements
We appreciate all the participants, staff, and graduate students of TIS for their crucial contributions.
Funding
This work was supported by the Science and Technology Innovation 2030 Major Projects (Grant Number 2022ZD0211600); National Key Research and Development program of China (Grant Number 2021YFC2500100); the Natural Science Foundation of Shanghai, China (Grant Numbers 23ZR1414000, 22ZR1405300); the Shanghai Rising-Star Program (Grant Number 22QA1404000); the National Natural Science Foundation of China (Grant Number 82304239); and Fudan School of Public Health-Jiading CDC key disciplines for the high-quality development of public health (Grant Number GWGZLXK-2023-02).
Author information
Authors and Affiliations
Contributions
X.Z.: Conceptualization, formal analysis, visualization, writing—original draft. H.L.: Investigation. M.F.: Project administration, supervision. W.T.: Project administration, supervision. Y.W.: Formal analysis. M.C.: Project administration, supervision. Y.J.: Funding acquisition, Project administration, supervision. C.S.: Project administration, supervision. T.Z.: Project administration, supervision. L.J.: Project administration, supervision. K.X.: Conceptualization, funding acquisition, project administration, supervision, writing—review & editing. X.C.: Funding acquisition, Project administration, supervision. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, X., Lu, H., Fan, M. et al. Bidirectional mediation of bone mineral density and brain atrophy on their associations with gait variability. Sci Rep 14, 8483 (2024). https://doi.org/10.1038/s41598-024-59220-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-59220-2
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.