Abstract
Breathing difficulties and exertional dyspnea are frequently reported in hypermobile Ehlers-Danlos syndrome (hEDS); however, they are not clearly explained. An impaired proprioception or the addition of a cognitive task could influence ventilatory control. How can the perception of lung volume be measured? Is lung volume perception impaired in hEDS patients? Is the breathing control impaired during a cognitive task in hEDS patients? A device was developed to assess the accuracy of lung volume perception in patients with hEDS and matched control subjects. In the second step, ventilation was recorded in both groups with and without a cognitive task. Two groups of 19 subjects were included. The accuracy of lung volume perception was significantly (P < 0.01) lower at 30% of inspired vital capacity in patients with hEDS in comparison to the control group, and they showed erratic ventilation (based on spatial and temporal criteria) when performing a cognitive task. These data support the influence of the proprioceptive deficit on ventilatory control in hEDS patients. These elements may help to understand the respiratory manifestations found in hEDS. Future research should focus on this relationship between lung volume perception and ventilation, and could contribute to our understanding of other pathologies or exercise physiology.
Trial registration number: ClinicalTrials.gov, NCT05000151.
Similar content being viewed by others
Introduction
Ehlers-Danlos syndromes (EDSs) are part of the inherited connective tissue disorders and are mainly characterized by joint hypermobility, skin hyperextensibility, and tissue fragility1. These syndromes are classified into 13 subtypes and present great clinical and genetic heterogeneity1. The most common is the hypermobile Ehlers-Danlos syndrome (hEDS), whose diagnosis remains clinical2. A wide variety of clinical manifestations are present in hEDS such as pain, fatigue, dysautonomia, gastrointestinal disorders, anxiety, and respiratory symptoms3,4,5.
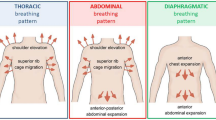
Breathing difficulties and exertional dyspnea are frequently reported3,6,7,8,9, but few studies have been conducted on lung function in patients with hEDS and tend to support normal lung function in hEDS3,9,10,11. The respiratory symptoms of hEDS are still unclear and raise many questions6. However, structural changes in the tissues involved in ventilation, related to the collagen or extracellular matrix abnormalities found in EDS, could lead to changes in ventilatory kinetics. Many hypotheses have been proposed, such as an alteration of diaphragm dynamics due to tissue hyperextensibility5,8, an increase in lung compliance9,12, or involvement of the reduced inspiratory muscle strength11. Another hypothesis is impaired signals from proprioceptive receptors, which could explain some respiratory impairments8. Proprioception is the conscious or unconscious perception of the position and movement of the different parts of the body13. It was demonstrated that patients with hEDS have proprioceptive impairments14,15,16. Breathing involves a large number of structures generating proprioceptive inputs (rib cage joints, respiratory muscles, etc.)17. However, although the control of ventilation is mainly regulated by chemoreceptors, the influence of proprioceptive inputs on this control remains relatively unexplored.
On the one hand we hypothesize that in patients with hEDS, the alteration of the proprioceptive inputs from the musculoskeletal system involved in ventilation could induce an impairment of the perception of lung volume and, thus, of the ventilatory control and could then explain in part some respiratory symptoms. To our knowledge, there is currently no validated tool to assess the accuracy of lung volume perception, which would reflect the proprioceptive sensitivity of the musculoskeletal system involved in ventilation. A simple and non-invasive tool was therefore designed to study differences between hEDS patients and healthy subjects.
On the other hand, it was demonstrated that hEDS patients present greater difficulty than healthy subjects in controlling their balance or walking in dual-task assessments18,19. It is known that cognitive tasks can affect ventilation in healthy people under different conditions20. We can, therefore, hypothesize that in patients with hEDS, cognitive tasks may increase the difficulty of controlling breathing.
This study had three objectives: (1) design a tool for the measure of lung volume perception; (2) investigate whether lung volume perception is impaired in hEDS patients; (3) investigate whether the control of breathing during a cognitive task is impaired in hEDS patients.
Methods
Participants
Participants were enrolled into two groups: a group of patients with hEDS and a group of matched healthy individuals. The inclusion criteria for the hEDS group were understanding the French language, being older than 18 years old, and having been diagnosed with hEDS according to the 2017 criteria1. The exclusion criteria for the hEDS patients were a known ongoing pregnancy, having a respiratory comorbidity independent of those linked to hEDS (other than asthma, hyperventilation, or dyspnea), or having already participated in a rehabilitation program. For each patient, a subject from the control group was matched for sex, age (± 5 years), and body mass index (BMI) (± 2.5 kg.m−2). The participants in the control group were recruited from volunteer employees of the Clinique de la Mitterie (Lomme, France). The exclusion criteria for the control group were a known respiratory or proprioceptive pathology, hypermobility according to the Beighton score (≥ 5 under 50 years old or ≥ 4 over 50 years old), or a known ongoing pregnancy.
All participants were volunteers and gave their written informed consent. This study was approved by a national ethics committee (CPP Ouest II, 2021/54) and was registered on ClinicalTrials.gov (NCT05000151). All experiments were performed in accordance with the Declaration of Helsinki.
After giving their informed consent, participants first completed the questionnaire before the investigator proceeded to a measurement of the Beighton score, followed by spirometry measurements, perception of the lung volume, and impact of a cognitive task on ventilation. All measurements were conducted during the same session and by the same operator.
General measurements
Participants completed a questionnaire including anthropometric data, occupation, inclusion and exclusion criteria, smoking status, and some questions on the subject’s feeling of skill in lung volume perception. Patients also completed a section on their diagnosis.
The questions about the subject’s feeling of skill in lung volume perception were: “Do you practice a hobby, physical activity or sport that requires good breathing control?” (Yes/No); “If yes, which one?” (Free answer); “Would you be able to estimate the quantity/volume of air entering your lungs?” (Yes/No) and “Circle the number that best describes your capacity/ability to perceive the quantity/volume of air entering your lungs.” (0–10 scale with 0 = “Not skilled at all. Unable to perceive.” and 10 = “Extremely skillful. Very good perception.”).
Hypermobility was assessed in all participants using the Beighton score21. Hypermobility was defined as a score of ≥ 5 for subjects under 50 years of age and ≥ 4 for subjects over 50 years of age1.
The Marshall’s questionnaire22 was used to look for any differences in physical activity levels between the groups that might influence the results. This questionnaire assesses the number of times the individual performs 20 min of intense physical activity or 30 min of moderate physical activity per week, providing a score from 0 to 8 with a threshold set at 4 (0–3: insufficiently active; 4–8: sufficiently active).
Inspiratory vital capacity (IVC), forced vital capacity (FVC), and forced expiratory volume in one second (FEV1) were measured on a calibrated computerized spirometer (BodyBox 5500, Medisoft, Belgium), according to the current recommendations23.
Lung volume perception
To our knowledge, there is no validated tool to assess lung volume perception, whereas methods exist to assess limb proprioception. As an indicator of articular proprioception, the joint position sense is assessed actively or passively13. The principle is to define a target joint amplitude, get the subject to perceive this amplitude actively or passively, and then ask the subject to reproduce (actively) or recognize (passively) the target amplitude. The difference between the achieved amplitude and the target amplitude is used as the criterion for the accuracy of the joint position sense. By transposition to the assessment of lung volume perception, a target lung volume (inspired air volume) is defined, and the subject is asked to reproduce this volume. The difference between the volume achieved and the target inspiratory volume is used as a criterion for the accuracy of lung volume perception and would reflect the proprioceptive sensitivity of the musculoskeletal system involved in ventilation.
The device for measuring lung volume perception had to display visual feedback in real time in order for the participant to adjust the inspiratory maneuver to reach the target volume in the first phase of the test. This device was composed of a mouthpiece (22M, Intersurgical, France), a single-use electrostatic filter (1420/01 or 1420/03, Medguard, Ireland), a 40.5 cm long and 22 mm diameter connecting tube, a flowmeter (SFM3000, Sensirion, Switzerland), an electronic acquisition card (UNO R3, Elegoo, China) with a 20 Hz sampling frequency, and an LCD screen for visual feedback. This device was calibrated with a 3 L syringe before each test (the same used for spirometer calibration) until an average of 6 measurements between 2985 and 3015 mL was obtained in accordance with the American Thoracic Society’s recommendations23. The program used for measurements was created with the software Arduino IDE Version 1.8.13 (Arduino.cc) and is based on the SFM3000Wedo library available online24. The device was positioned on a height-adjustable table so that the tube connecting the flowmeter to the patient’s mouth was horizontal in a standardized position. Subjects wore a nose clip to prevent nasal breathing and noise-canceling earbuds to cancel noise distraction.
First, an inspiratory vital capacity was measured with the device described above (IVC with flowmeter; IVCfm). Then, three target inspiratory volumes (IV) were defined according to IVCfm. An initial familiarization IV at 40% of IVCfm (IV40) allowed the patient to become familiar with the procedure, followed by two IVs at 30% (IV30) and 50% (IV50) of the IVCfm used to measure accuracy at different levels of structural stretch. The applied order (IV40, then IV30, then IV50) remained the same for all subjects. A break of one to two minutes was taken between each IV. The instruction for the participants was, after emptying their lungs, to inhale a volume as close as possible to these IVs. Participants were asked to empty their lungs before inhaling. The current IV was written on a board visible to the subject. The subject had three training sessions per IV, during which the volume was displayed in real time on an LCD screen. During training sessions, the subject was asked to reproduce the target volume and to focus on the perceived feelings in order to reproduce it afterward without a screen. The subject then performed three trials without visual feedback. The achieved volume was verbally indicated after each blind trial. Verbal instructions to the subjects were standardized.
The absolute difference between each trial and the IV (ΔIV) was calculated in milliliters and as a percentage of the IV. These values were used to calculate the average ΔIV for IV30 and IV50. A schematic representation of this design is presented in Fig. 1.
Schematic representation of the lung volume perception test design. On the left side is the overall process with the three target inspiratory volumes; on the right side is the process for each target inspiratory volume with the training session (visual feedback) and the measurements (no visual feedback). ΔIV absolute difference between the measure and the IV, IVC inspired ventilatory capacity; and IV target inspiratory volume.
Ventilatory response to cognitive task
The objective of this last measurement was to assess the influence of a cognitive task on the ventilatory control in hEDS patients versus healthy subjects. Wearing earbuds and nose clips, subjects first breathed freely through the same device one minute before, immediately afterward, and for one minute, during a cognitive task. The cognitive task was the Trail making test part B25, consisting of connecting, as quickly and accurately as possible, in ascending order circles containing numbers and letters, alternating one number and one letter each time. This test was used as a simple, standardized, non-verbal cognitive task requiring little movement. As recommended, an example was shown to the subject before the start of the two periods. As the first experimental condition was in a resting condition (subjects sitting on a chair), there was no randomization of the order of conditions between subjects. The verbal instructions given to the participants were standardized.
In order to analyze the variability of ventilation, each inspiratory peak was identified. Only respiratory cycles longer than 0.1 s and larger than 100 mL were taken into account26. This made it possible to calculate the time intervals between two inspiratory peaks (PP) and the tidal volume (VT).
Temporal variations were measured by breathing frequency (fB), standard deviation of PP (PPSD), or root mean square of PP (RMSSD). Spatial variations were measured by the mean VT and the standard deviation of this volume (VT,SD). Minute ventilation (V̇E) was used as a mixed index (temporal and spatial). The ventilatory coefficients of variability for both temporal (CoefVar_t) and spatial domains (CoefVar_V) were calculated as follows:
Statistical analysis
Data are described with mean and standard deviation (mean ± SD). Statistical analysis was performed on SigmaStat Version 3.5 (Systat Software Inc., San Jose, USA). Before each test, the normality of the data distribution and equality of variances were tested. Differences between the two groups were tested with a paired t-test or a Wilcoxon signed-rank test. Differences were considered as significant for a P value < 0.05.
Results
Participants characteristics
Twenty patients were recruited in the hEDS group. One could not be matched due to a high BMI (42 kg.m−2), for which we could not find a matching control subject. This participant was therefore excluded from the analysis, and 19 control subjects were included. Each group consisted of 18 women and one man. Anthropometric data, Marshall and Beighton scores, and general information are presented in Table 1. There was no significant difference between the two groups for age, height, weight, BMI, and Marshall score, contrary to the Beighton score (P < 0.001). Four patients reported asthma, one of whom also reported hyperventilation.
Concerning the subjects’ feeling of skill in lung volume perception, 10 participants in the hEDS group reported “doing an activity requiring good breathing control” compared to 9 in the control group. The activities were mostly physical. For patients, they were yoga, cycling, swimming, walking, horse riding, and dancing, and for control subjects, running, bodybuilding, judo, pilates, gymnastics, and cycling. Only one control subject cited sophrology as a non-physical activity requiring good ventilatory control. Only three participants (two hEDS, one control) answered “Yes” to the question “Would you be able to estimate the quantity/volume of air entering your lungs?” and when participants rated their ability to perceive on a numeric scale, the mean score obtained was 3.1 ± 2.5 for the hEDS group and 3.4 ± 2.5 for the control group, with no significant difference between the two groups.
Regarding spirometry, there was no significant difference between the two groups. IVC and IVCfm measurements were strongly correlated (r = 0.96; P < 0.001).
Lung volume perception
Regarding the IV30, there were significant differences between the hEDS and the control groups for the mean ΔIV in mL (P = 0.002) and in percentage (P = 0.001). There was no significant difference in the IV50 between the two groups (Table 2).
Ventilatory response to cognitive task
In the free condition (breathing without instruction), there was a significant difference between the hEDS and the control groups for fB (P = 0.032). There was no other significant difference between the two groups in this condition (Table 3).
When performing the cognitive task, there were significant differences between the hEDS and the control groups for VT,SD (P = 0.023), CoefVar_V (P = 0.004), PPSD (P = 0.011) and CoefVar_t (P = 0.003).
Figure 2 illustrates, among hEDS patients, an erratic respiratory pattern (apnea, volume variations, and flow variations) during the cognitive task.
Examples of curves obtained during measurements of the effect of a cognitive task on ventilation. The left part of the curve corresponds to one minute of breathing without instruction; the right part corresponds to one minute of breathing performing the cognitive task. The curves are grouped by matched participants’ pairs (A–D). hEDS hypermobile Ehlers-Danlos syndrome.
Discussion
The objectives of this study were: (1) design a tool for the measure of lung volume perception; (2) investigate whether lung volume perception is impaired in hEDS patients; (3) investigate whether the control of breathing during a cognitive task is impaired in hEDS patients.
The tool designed to measure lung volume perception seems reliable, as indicated by the significant correlation (r = 0.96; P < 0.001) with the spirometer measurements. The results showed that the accuracy of lung volume perception was significantly reduced at 30% of IVCfm in patients with hEDS and that they showed erratic ventilation when performing a cognitive task.
To our knowledge, this study is the first to explore the impact of a proprioceptive deficit on ventilation in hEDS. There was a significant difference between the two groups for IV30, with an average error of 22.3% in hEDS compared with 13.1% in healthy subjects, and similar results when expressed in mL. These results indicate that subjects with hEDS are less precise in perceiving their lung volume at moderate volumes. Impairment of this information could lead to abnormalities in ventilation regulation and potentially explain some of the dyspnea described in hEDS.
On the other hand, there is no significant difference for IV50, which suggests that both groups are more accurate at IV50. One hypothesis is that there would be more sensory information at IV50 than at IV30 due to an increased stretch of the different structures involved. One of the hypotheses to explain the proprioceptive deficit in hEDS subjects is that the structures containing the proprioceptive receptors would be more flexible in these subjects. Therefore, greater stretching might be necessary to trigger the nerve signal16. This is consistent with our results, since some signals would only occur at larger lung volumes in hEDS subjects. There is a need to further investigate the methodology of this measurement technique, such as looking for differences in healthy subjects at several lung volumes.
More generally, and to our knowledge, this is the first study to use a protocol inspired by joint proprioception to measure the accuracy of lung volume perception. Although this protocol seemed to be particularly adapted in the case of patients with hEDS, it would be interesting for future studies to establish standards and to investigate this lung volume perception in other respiratory pathologies such as chronic obstructive pulmonary disease or hyperventilation, but also in different physical activities. This tool could also be used to work on the perception of lung volume or to evaluate certain management techniques focused on ventilatory work.
Regarding the results of the ventilatory response to a cognitive task, an increase in temporal and spatial variability was observed in both groups during the cognitive task. However, this increase was more important in the hEDS group, which is responsible for the significant differences between the groups observed during the cognitive task but not during the free condition. This is seen in the visual analysis of the ventilatory curves (Fig. 2).
The increased variability of ventilatory spatial and temporal parameters during the addition of a cognitive task in the hEDS group could represent erratic ventilation during daily activities, such as difficulties in walking and balance when adding a cognitive task, as already mentioned in the literature18,19. However, this is the first time such difficulties in relation to ventilation are described.
As suggested in the first part of this study, a reduction in proprioceptive inputs from the musculoskeletal system involved in ventilation could cause abnormalities in ventilatory control. If we consider that the central nervous system also integrates these proprioceptive inputs to regulate ventilation, absent or erroneous information could lead to central dysregulation of ventilation. The addition of a cognitive task, which should normally produce minor changes in ventilation, would, therefore, result in the genesis of erratic ventilation due to dysregulation of ventilation control by anomalies in proprioceptive inputs from the musculoskeletal system involved in ventilation.
On visual analysis of the curves, some apnea intervals can be observed (Fig. 2, panel B, hEDS subject). It would be relevant to explore the link between these and the respiratory blockages described in hEDS by some authors8,27.
The fB was found to be higher in the free condition in the hEDS group than in the control group. This is consistent with our clinical observations of a tendency for hyperventilation in patients with hEDS. The question of the energetic cost of faster ventilation may also arise, especially in a pathology frequently associated with chronic fatigue28.
Considering that physical activity requires more conscious joint control in subjects with hEDS due to increased laxity, this control could be viewed as a cognitive task and lead to ventilatory difficulties during physical activity. Erratic ventilation during physical activity could be a factor in exercise intolerance, and the altered lung volume perception could be one explanation for the dynamic hyperinflation described in these patients in a previous study29. These data open up new therapeutic perspectives in the management of respiratory disorders in hEDS.
One limitation of the study is the moderate number of subjects included. A larger study would be required to confirm these results. Although the hypothesis that has been proposed was oriented towards an influence of sensory inputs coming from the musculoskeletal system of the thoracic cage it is not possible to exclude a sensory influence from upper airway. The relative influence of each other could be the subject of a future study.
Conclusions
This study demonstrates an impaired perception of lung volume at lower percentages of IVC and an increased difficulty in regulating ventilation during a cognitive task in patients with hEDS compared to healthy subjects. These elements may help to understand the respiratory manifestations found in hEDS.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- ΔIV:
-
Absolute difference between the trial and the IV
- CoefVar_t:
-
Temporal coefficients of variability
- CoefVar_V:
-
Spatial coefficients of variability
- EDS:
-
Ehlers-Danlos syndrome
- fB :
-
Breathing frequency
- FEV1 :
-
Forced expiratory volume in one second
- FVC:
-
Forced vital capacity
- hEDS:
-
Hypermobile Ehlers-Danlos syndrome
- IVx :
-
Inspiratory volume at x% of IVCfm
- IVC:
-
Inspiratory vital capacity (spirometer)
- IVCfm :
-
Inspiratory vital capacity with flowmeter
- PP:
-
Time interval between two inspiratory peaks
- RMSSD:
-
Root mean square of PP
- V̇E :
-
Minute ventilation
- VT :
-
Tidal volume
References
Malfait, F. et al. The 2017 international classification of the Ehlers-Danlos syndromes. Am. J. Med. Genet. C Semin. Med. Genet. 175, 8–26 (2017).
Sulli, A. et al. Ehlers-Danlos syndromes: State of the art on clinical practice guidelines. RMD Open 4, e000790 (2018).
Castori, M. et al. Natural history and manifestations of the hypermobility type Ehlers-Danlos syndrome: A pilot study on 21 patients. Am. J. Med. Genet. A. 152A, 556–564 (2010).
De Wandele, I. et al. Clinical heterogeneity in patients with the hypermobility type of Ehlers-Danlos Syndrome. Res. Dev. Disabil. 34, 873–881 (2013).
Tinkle, B. et al. Hypermobile Ehlers-Danlos syndrome (a.k.a. Ehlers-Danlos syndrome type III and Ehlers-Danlos syndrome hypermobility type): Clinical description and natural history. Am. J. Med. Genet. C Semin. Med. Genet. 175, 48–69 (2017).
Bascom, R., Dhingra, R. & Francomano, C. A. Respiratory manifestations in the Ehlers-Danlos syndromes. Am. J. Med. Genet. C Semin. Med. Genet. https://doi.org/10.1002/ajmg.c.31953 (2021).
Chohan, K. et al. A review of respiratory manifestations and their management in Ehlers-Danlos syndromes and hypermobility spectrum disorders. Chronic Respir. Dis. 18, 147997312110253 (2021).
Hamonet, C. et al. Manifestations respiratoires dans le syndrome d’Ehlers-Danlos (SED) Nouveaux apports thérapeutiques. J. Réadapt. Médicale Prat Form. Médecine Phys. Réadapt. 36, 56–61 (2016).
Morgan, A. W., Pearson, S. B., Davies, S., Gooi, H. C. & Bird, H. A. Asthma and airways collapse in two heritable disorders of connective tissue. Ann. Rheum. Dis. 66, 1369–1373 (2007).
Ayres, J. G., Pope, F. M., Reidy, J. F. & Clark, T. J. Abnormalities of the lungs and thoracic cage in the Ehlers-Danlos syndrome. Thorax 40, 300–305 (1985).
Reychler, G., Liistro, G., Piérard, G. E., Hermanns-Lê, T. & Manicourt, D. Inspiratory muscle strength training improves lung function in patients with the hypermobile Ehlers-Danlos syndrome: A randomized controlled trial. Am. J. Med. Genet. A 179, 356–364 (2019).
Sharman, T. Acute respiratory failure secondary to persistent lobar atelectasis in Ehlers-Danlos syndrome patient and the role of connective tissue disease in altering the mechanical properties of the lungs. Am. J. Med. Case Rep. 7, 284–288 (2019).
Hillier, S., Immink, M. & Thewlis, D. Assessing proprioception: A systematic review of possibilities. Neurorehabil. Neural Repair 29, 933–949 (2015).
Clayton, H. A., Jones, S. A. H. & Henriques, D. Y. P. Proprioceptive precision is impaired in Ehlers-Danlos syndrome. SpringerPlus 4, 1–8 (2015).
Rombaut, L., De Paepe, A., Malfait, F., Cools, A. & Calders, P. Joint position sense and vibratory perception sense in patients with Ehlers-Danlos syndrome type III (hypermobility type). Clin. Rheumatol. 29, 289–295 (2010).
Scheper, M. et al. The association between muscle strength and activity limitations in patients with the hypermobility type of Ehlers-Danlos syndrome: The impact of proprioception. Disabil. Rehabil. 39, 1391–1397 (2017).
Road, J. D. Chest wall afferent output. Chest 97, 40S-43S (1990).
Dupuy, E. G. & Decker, L. M. Modification des stratégies de régulation posturale dans le syndrome d’Ehlers-Danlos de type hypermobile (SEDh). Neurophysiol. Clin. 48, 327 (2018).
Rombaut, L. et al. Balance, gait, falls, and fear of falling in women with the hypermobility type of Ehlers-Danlos syndrome. Arthritis Care Res. 63, 1432–1439 (2011).
Grassmann, M., Vlemincx, E., von Leupoldt, A., Mittelstädt, J. M. & Van den Bergh, O. Respiratory changes in response to cognitive load: A systematic review. Neural Plast. 2016, 1–16 (2016).
Beighton, P., Solomon, L. & Soskolne, C. L. Articular mobility in an African population. Ann. Rheum. Dis. 32, 413–418 (1973).
Marshall, A. L., Smith, B. J., Bauman, A. E. & Kaur, S. Reliability and validity of a brief physical activity assessment for use by family doctors. Br. J. Sports Med. 39, 294–297 (2005).
Graham, B. L. et al. Standardization of spirometry 2019 update. An official American thoracic society and european respiratory society technical statement. Am. J. Respir. Crit. Care Med. 200, e70–e88 (2019).
dwerne. dwerne/Sensirion_SFM3000_arduino (2022).
Bowie, C. R. & Harvey, P. D. Administration and interpretation of the trail making test. Nat. Protoc. 1, 2277–2281 (2006).
Beda, A., Jandre, F. C., Phillips, D. I. W., Giannella-Neto, A. & Simpson, D. M. Heart-rate and blood-pressure variability during psychophysiological tasks involving speech: Influence of respiration. Psychophysiology 44, 767–778 (2007).
Celletti, C. & Camerota, F. The multifaceted and complex hypermobility syndrome (aka Ehlers-Danlos Syndrome Hypermobility Type): Evaluation and management through a rehabilitative approach. Clin. Ter. https://doi.org/10.7417/CT.2013.1597 (2013).
Hakim, A., De Wandele, I., O’Callaghan, C., Pocinki, A. & Rowe, P. Chronic fatigue in Ehlers-Danlos syndrome-hypermobile type. Am. J. Med. Genet. C Semin. Med. Genet. 175, 175–180 (2017).
Hakimi, A., Bergoin, C. & Mucci, P. Evidence of ventilatory constraints during exercise in hypermobile Ehlers-Danlos syndrome. Eur. J. Appl. Physiol. https://doi.org/10.1007/s00421-022-05017-y (2022).
Acknowledgements
The authors would like to thank all the participants in this study, the entire staff of the Clinique de la Mitterie and the patient association SED1+.
Author information
Authors and Affiliations
Contributions
All the authors contributed substantially to the study design, data analysis and interpretation, and the writing of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hakimi, A., Bergoin, C., De Jesus, A. et al. Impairment of lung volume perception and breathing control in hypermobile Ehlers-Danlos syndrome. Sci Rep 14, 8119 (2024). https://doi.org/10.1038/s41598-024-58890-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-58890-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.