Abstract
Healthcare workers (HCWs) were at high risk of experiencing psychological distress during COVID-19 pandemic. The objective of this study was to evaluate the impact on HCWs’ mental health in a Spanish hospital. Cross-sectional study of HCW, active between May and June 2020. A web-based survey assessed probable current mental disorders (major depressive disorder [PHQ-8 ≥ 10], generalized anxiety disorder [GAD-7 ≥ 10], panic attacks, post-traumatic stress disorder [PTSD; PLC-5 ≥ 7], or substance use disorder [CAGE-AID ≥ 2]). The Sheehan Disability Scale (SDS) was used to assess severe impairment and items taken from the modified self‐report version of the Columbia Suicide Severity Rating Scale (C‐SSRS) assessed suicidal thoughts and behaviors. A total of 870 HCWs completed the survey. Most frequent probable mental disorders were major depressive disorder (33.6%), generalized anxiety disorder (25.5%), panic attacks (26.9%), PTSD (27.2%), and substance use disorder (5.0%). Being female, having aged 18–29 years, being an auxiliary nurse, direct exposure to COVID-19-infected patients, and pre-pandemic lifetime mental disorders were positively associated with mental issues. Hospital HCWs presented a high prevalence of symptoms of mental disorders, especially depression, PTSD, panic attacks, and anxiety. Younger individuals and those with lifetime mental disorders have been more vulnerable to experiencing them.
Similar content being viewed by others
Introduction
In 2020, the COVID-19 outbreak was declared a pandemic by the World Health Organization (WHO), with 618 million and 13.8 million confirmed cases and 6.8 million and 119,618 deaths worldwide and in Spain, respectively as of March 20231,2. Epidemiological studies have shown that past infectious diseases resulted in long-term and persistent psychological consequences among those affected3,4,5. Similarly, the COVID-19 pandemic has threatened global mental health, both indirectly via disruptive societal changes and directly via neuropsychiatric sequelae after SARS-CoV-2 infection6. Indeed, a previous Spanish study analyzing the clinical picture during the first wave by a factor analysis, showed that anosmia/ageusia, cognitive complaints, worry/nervousness, slowing down, and sadness have been the most frequently reported neuropsychological symptoms among hospitalized COVID-19 patients7. Therefore, in addition to its effects on the economy and public health, the COVID-19 pandemic has had a profound impact on the physical health and psychological well-being of healthcare workers (HCWs). HCWs have played a crucial role and are considered a high-risk population for suffering from psychological and mental disorders due to the COVID-19 pandemic8. The absence of data on transmission dynamics and evidence-based recommendations regarding the necessary protective measures made the situation particularly stressful for individuals employed in the healthcare sector. Moreover, HCWs were required to wear personal protective equipment, which can reduce their mobility and slow down their operations, can cause respiratory discomfort and difficulty, further exacerbating the psychological symptoms experienced by HCWs9,10. Several studies have documented that a significant proportion of HCWs experienced persistent psychological issues including anxiety, depression, and insomnia9,11,12,13. Spain ranked first in the world in healthcare infections during the first wave of the pandemic14. A nationwide, cross-sectional, web-based survey determined the mental health impact of the first wave of the COVID-19 pandemic (May–September 2020) on 9138 Spanish HCWs from 18 healthcare centers (MINDCOVID study)15. Authors revealed that approximately one in two HCWs experience an ongoing mental disorder, and 14.5% suffer a disabling one15. Another study by the MINDCOVID group, with data from 5450 HCWs of 10 Spanish hospitals between May and July 2020, reported a prevalence of 30-day suicidal thoughts and behaviors (STB) of 8.4%16.
The objective of the present study was to evaluate the impact of the COVID-19 pandemic on the mental health of HCWs during the first wave in one of the largest front-line tertiary hospitals from Spain and to explore potential factors associated with these probable mental disorders. These data would complement those previously reported in hospitalized COVID-19 patients, thus, providing a more detailed picture of the situation during the first wave of the COVID-19 pandemic in this Spanish hospital.
Methods
Study design
This is an observational analysis of data from HCWs at the University Hospital 12 de Octubre (Madrid, Spain). Information from HCWs represents a sub-analysis from the MINDCOVID study15. Institutional representatives from the hospital invited (by mail) all healthcare employees to participate in the study. All HCWs from the hospital with an institutional e-mail account were invited to participate, without any additional restriction. All participants accepted the online informed consent before being able to access the interview.
Evaluation of probable mental health disorders
HCWs completed a web-based survey between May and June 2020 that included, among other items, standard screening instruments for measuring probable current mental disorders. Major depressive disorder (MDD) was assessed by the Spanish version of the Patient Health Questionnaire (PHQ-8), with the cut-off point ≥ 10 of the sum score17,18. Panic attacks were evaluated by assessing the number of attacks in the 30 days prior to the interview19,20. For evaluating post-traumatic stress disorder (PTSD), the 4-item version of the PTSD checklist for DSM-5 (PCL-5) was applied20,21. Generalized anxiety disorder (GAD) was evaluated by using the Spanish adaptation of the 7-item GAD scale (GAD-7), with a cut-off point of ≥ 1019,22,23,24. Substance Use Disorder (SUD) was evaluated by using the Spanish version of the CAGE questionnaire adapted to include drugs (CAGE-AID) with a cut-off point of ≥ 225,26. Any of the above probable mental disorders was considered “disabling” if the participant reported severe role impairment (score ≥ 7) during the past 12 months according to an adapted version of the Sheehan Disability Scale27,28,29. Lifetime mental disorders, prior to the COVID-19 pandemic, were assessed by using a checklist based on the Composite International Diagnostic Interview (CIDI) that screens for self-reported lifetime depressive disorder, bipolar disorder, anxiety disorders, panic attacks, alcohol and drug use disorders, and “other” mental disorders. More information from the survey instrument is provided elsewhere15. A modified self‐report version of selected items from the Columbia Suicide Severity Rating Scale (C‐SSRS) was applied to assess suicidial thoughts and behaviors in the past 30 days30, including passive suicidal ideation (“wish you were dead or would go to sleep and never wake up”), active suicidal ideation (“have thoughts of killing yourself”), suicide plans (“think about how you might kill yourself [e.g., taking pills, shooting yourself] or work out a plan of how to kill yourself”), and suicide attempt (“make a suicide attempt [i.e., purposefully hurt yourself with at least some intent to die”).
Statistical analysis
Demographic, clinical, and survey characteristics of HCWs are expressed with the mean and standard deviation (SD), or with absolute and relative frequencies, when appropriate. Post-stratification weights were applied with raking procedure to restore distributions the elegible personnel within the hospital according to age, gender and professional category. Statistical significance was assessed with pooled Chi-square test from multiple imputations after adjustment for multiple comparisons with Benjamin-Hochberg (false discovery rate 0.05). Missing item-level data among respondents were imputed using multiple imputation by chained equations with 12 imputed datasets and 10 iterations per imputation31.
Ethical approval and informed consent
The study complies with the Declaration of Helsinki and the Code of Ethics and was approved by the IRB Parc de Salut Mar (2020/9203/I) and by the corresponding IRBs of all the participating centres. Registered at ClinicalTrials.gov (https://clinicaltrials.gov/ct2/show/NCT04556565). The database was anonymized to preserve sensitive data from patients. Participants signed the written informed consent.
Results
Participants
Of the 7797 eligible professionals, 870 HCWs participated and completed the survey (Sociodemographics are shown in Table 1). The response rate, calculated as the number of participants that completed it divided by the estimated eligible workers, was 11.8%. Survey participation (workers that agreed to participate divided by those who responded to the informed consent) and completion rates (participants that completed the survey divided by those who agreed to participate) were 88.5% and 78.9%, respectively. HCWs of the sample were predominantly females (78.1%), with a mean age of 43.7 (SD: 11.4), and working mainly as nurses (28.1%), physicians (18.3%), and auxiliary nurses (18.3%). Half of them (52.3%) were frontline workers during the COVID-19 pandemic. Most of them were not infected (77.1%) at the time of the study. The most frequent previous lifetime mental disorder was anxiety (41.7% of them), followed by mood disorder (12.8%).
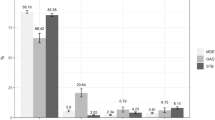
Probable mental disorders
The most frequent probable mental disorders identified in HCWs were MDD (33.6% of them), GAD (25.5%), panic attacks (26.9%), PTSD (27.2%), and SUD (5.0%) (Fig. 1). In total, 51.2% of the HCWs had a probable current mental disorder, and 16.3% presented a disabling mental disorder. The prevalence of any suicidal thought and behavior (STB) was 7.9% (Fig. 1).
Table 2 shows the prevalence of all mental disorders and STBs according to sociodemographic variables and by proximal and distal risk factors. Significant differences (higher prevalence) of mental disorders were found regarding gender (females, for current MDD, GAD, panic attacks, PTSD, and any mental and any disabling mental disorder); age (18–29 years, for current MDD, GAD, panic attacks, PTSD, any mental disorder, and any STB); job position (auxiliary nurse, for current MDD, GAD, panic attacks, PTSD, and any previous mental and disabling mental disorder); direct exposure to infected patients (for current MDD, GAD, panic attacks, PTSD, and any mental disorder); and lifetime disorders (mood, anxiety, other mental disorder) (Table 2).
Discussion
The emergence of the COVID-19 pandemic has led to a worldwide public health emergency, causing significant psychological challenges in the global healthcare system, particularly during the initial stages of the outbreak32. The results obtained from the present study show a high prevalence of current probable mental disorders and suicidal ideation in a large sample of HCWs from Hospital 12 de Octubre (Spain) during the first wave of the COVID-19 pandemic. Symptoms of MDD were the most frequently reported, followed by GAD, panic attacks, and PTSD. Furthermore, we observed that HCWs with lifetime mental disorders had a notably higher occurrence of adverse mental health. Other specific variables such as gender, age, job position, and direct exposure to infected patients were found to pose a greater risk in the onset of mental disorders.
During the COVID-19 pandemic, HCWs have been confronted with an unprecedented situation that has taken a toll on their mental and physical health33. Their essential duties required them to make difficult decisions under extreme pressure, thereby placing them at a higher risk of developing mental health disorders34,35. Previous studies evidencing the impact of the COVID-19 crisis on the mental health of HCWs are in agreement with the findings presented herein15,16,36,37,38,39. A survey carried out in May 2020 by the British Medical Association showed that 45% of UK physicians were experiencing anxiety, depression, stress, or other mental issues due to the COVID-19 pandemic36. In Spain, another survey performed during the first COVID-19 wave (between May 2020 and September 2020), reported that 43.7% of the 2929 primary care professionals (95% confidence interval [CI] = 41.9–45.4) screened positive for a probable mental disorder37. In general, published studies evaluating the psychological toll on HCWs report symptoms of anxiety, depression, insomnia, or distress38. The prevalence of depressive symptoms and anxiety ranges from 8.9 to 50.4% and between 14.5 and 44.6%, respectively. A systematic review and meta-analysis, involving data from 70 studies and 101,017 HCWs, have revealed a pooled prevalence of 30.0% for anxiety, 31.1% for depression and depressive symptoms, 56.5% for acute stress, 20.2% for post-traumatic stress, 44.0% for sleep disorders39. Another systematic review and meta-analysis, including 12 studies related to the psychological impact of the COVID-19 outbreak on HCWs in Asian countries, reported an overall prevalence rate of anxiety, depression, and stress of 34.8%, 32.4% and 54.1%, respectively40.
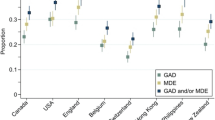
In Spain, MINDCOVID studies were multicenter observational trials that aimed to evaluate the impact of COVID-19 on the mental well-being of HCWs during the first wave15,16. In line with our findings, almost half of the surveyed workers (45.7%) presented any current mental disorder and 14.5% tested positive for a disabling mental disorder15. The most frequent probable mental disorders reported were current MDD (28.1%), GAD (22.5%), panic attacks (24.0%), PTSD (22.2%), SUD (6.2%), and any STB (8.4%). Other prevalence rates reported were passive ideation (4.9%), active ideation without plan or attempt (0.8%), and active ideation with plan or attempt (2.7%)15,16. When comparing our present results (unicenter) with those from the multicenter, nationwide MINDCOVID study15, prevalence rates of any probable mental disorder, MDD and PTSD are higher (Supplementary Fig. 1). The observed differences may respond to the different casuistry of Spanish hospitals during the first wave. Indeed, the pandemic carried out potentially traumatic moral and ethical challenges (e.g., choosing whom to indicate a ventilator in a situation where there was not for everyone) that exposed HCWs to the risk of developing moral injury41,42. Although moral injury is not considered a mental disorder yet, it is thought to be associated with PTSD by symptomatology and etiology, since both could be two different responses to trauma41,42. Thus, the higher prevalence of this PTSD could be attributed to the exposure of HCWs to these moral stressors41,42.
Regarding potential factors associated with probable mental disorders, our study pointed out a higher vulnerability of young individuals (aged between 18 and 29 years), female gender, and those with lifetime mental disorders (p < 0.05). Sociodemographic factors, such as gender and age have been previously related to a higher risk38. Female sex has been associated with a increased risk of mental disorders in several studies analyzing the impact of the COVID-19 pandemic on the mental health of HCWs43,44,45,46,47. A recent meta-analysis conducted by Lee and colleagues including 401 studies, has reported higher odds of probable mental health disorders in women, in particular depression, anxiety, PTSD and insomnia48. Multiple explanations or mechanisms have been proposed to explain these differences, including potential response bias (e.g., males may experience greater difficulty in recognizing and expressing psychological distress) as well as various biological, social, and demographic factors49,50. Therefore, although age and gender appear to be risk factors, this should be considered with caution. Moreover, the existence of a previous mental disorder has been identified as a predictor of other mental issues, such as depression and anxiety, during COVID-1951. Also, some studies have indicated that the COVID-19 pandemic could have a negative impact on current mental disorders52. Given that all HCWs were exposed to a high risk of developing or aggravating psychiatric symptoms, those with prior or current mental disorders would have been more vulnerable during the COVID-19 pandemic.
The limited availability of personal protective equipment, the continuous exposure to infected patients, the rate of deaths, the absence of specific treatments, overwhelming workload are other factors contributing to the development of these mental issues53. Additionally, HCWs' rising anxiety about the spread of COVID-19 may be linked to the misinformation that circulated during the initial wave of the pandemic and the concern that they may be a possible risk of contagion to their partner and family43,54. Furthermore, herein it was observed that some job positions, specifically auxiliary nurses, have a higher risk of mental disorders (p < 0.05). Maunder et al.55 studied the trend of burnout and psychological distress among HCWs from the fall of 2020 to the summer of 2021 and also found that nurses mostly reported the highest rates of burnout. Similarly, Fattori et al.56 observed that nurses and health assistants had higher risks of scoring above cut-offs than physicians (OR = 4.72 and 6.76 respectively). Differences between public and private healthcare sectors has been also analyze previously. According to a recent study by Pabón-Carrasco, HCWs employed in publicly healthcare institutions reported a lower perceived risk of COVID-19 transmission compared to their counterparts in private institutions during the first wave43. However, anxiety levels were higher in public employed HCWs compared to those reported by those privately employed (more than 25% and ~ 20%, respectively). Both groups had high levels of anxiety, despite private sector was not considered first-line43.
Some limitations of our study should be considered. First, its cross-sectional design, without similar information collected before the pandemic, does not allow us to infer the causality of the impact of the COVID-19 pandemic on the mental health of HCWs, nor to estimate the true magnitude of change in the prevalence of probable mental disorders. Furthermore, it is worth mentioning that during the first wave of the pandemic, psychological support was offered on demand to those professionals who requested it voluntarily at the hospital. Additionally, group interventions were conducted to alleviate symptoms at the onset. It would have been interesting to assess the impact of these interventions as a protective factor; however, we lack this data, which constitutes an additional limitation and possible bias.
Second, the response rate was lower than expected. It is possible that those experiencing mental health issues were more willing to participate or stressed workers did not have time to respond. However, weighting data has attempted to counteract this limitation. Third, this study’s assessments are based on self-reports from HCWs and not clinically diagnosed mental disorders. It is for this reason that we describe them as probable mental disorders.
Importantly, our approach has been used in most epidemiological studies, allowing for comparisons of results21,23,57. A more detailed analysis of proximal factors would have been interesting for linking the probable mental disorders with pandemic-related stressors.
Despite the above-mentioned limitations, we are confident to conclude that, during the first wave of the COVID-19 pandemic, HCWs of this large Spanish university hospital have presented a high prevalence of probable mental disorders, especially depression, PTSD, panic attack and anxiety. Younger individuals and those with lifetime mental disorders have been more vulnerable to experiencing them.
Based on our results, it appears to be expected that there is a significant demand for mental healthcare services among healthcare professionals in this Hospital that needs to be addressed. Our results, like others, highlight the significance of closely monitoring the psychological well-being of HCWs and facilitating their access to psychological assistance.
Understanding this data can also be relevant when selecting profiles of professionals who should be especially protected in high-stress situations, in order to care for their emotional well-being, such as those workers with a history of mental health issues or other vulnerability factors.
Future studies are needed to determine the evolution of the psychological impact of the COVID-19 pandemic over time in HCWs to implement appropriate therapeutic interventions.
Data availability
The de‐identified participant data as well as the study protocol and statistical analysis plan used for this study are available upon reasonable request from the corresponding author as long as the main objective of the data sharing request is replicating the analysis and findings as reported in this paper.
References
World Health Organization (WHO). Coronavirus (COVID-19). Available from: https://covid19.who.int/
Número de casos confirmados de coronavirus en España a fecha de 10 de marzo de 2023, por comunidad autónoma. Available from: https://es.statista.com/estadisticas/1100641/regiones-afectadas-por-el-covid-19-segun-los-casos-confirmados-espana
Diseases, G. B. D. & Injuries, C. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 396(10258), 1204–1222. https://doi.org/10.1016/S0140-6736(20)30925-9 (2020).
Penninx, B. W., Pine, D. S., Holmes, E. A. & Reif, A. Anxiety disorders. Lancet 397(10277), 914–927. https://doi.org/10.1016/S0140-6736(21)00359-7 (2021).
Herrman, H. et al. Time for united action on depression: A lancet-world psychiatric association commission. Lancet 399(10328), 957–1022. https://doi.org/10.1016/S0140-6736(21)02141-3 (2022).
Penninx, B., Benros, M. E., Klein, R. S. & Vinkers, C. H. How COVID-19 shaped mental health: From infection to pandemic effects. Nat. Med. 28(10), 2027–2037. https://doi.org/10.1038/s41591-022-02028-2 (2022).
Molina, J. D. et al. Neuropsychological symptom identification and classification in the hospitalized COVID-19 patients during the first wave of the pandemic in a Front-Line Spanish Tertiary Hospital. Front. Psychiatry 13, 838239. https://doi.org/10.3389/fpsyt.2022.838239 (2022).
Alzueta, E. et al. How the COVID-19 pandemic has changed our lives: A study of psychological correlates across 59 countries. J. Clin. Psychol. 77(3), 556–570. https://doi.org/10.1002/jclp.23082 (2021).
Chen, Q. et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry 7(4), e15–e16. https://doi.org/10.1016/S2215-0366(20)30078-X (2020).
Giusti, E. M. et al. The psychological impact of the COVID-19 outbreak on health professionals: A cross-sectional study. Front. Psychol. 11, 1684. https://doi.org/10.3389/fpsyg.2020.01684 (2020).
Chen, X. et al. Belief in a COVID-19 conspiracy theory as a predictor of mental health and well-being of health care workers in ecuador: Cross-sectional survey study. JMIR Public Health Surveill 6(3), e20737. https://doi.org/10.2196/20737 (2020).
Cheng, F. F. et al. Anxiety in Chinese pediatric medical staff during the outbreak of Coronavirus Disease 2019: A cross-sectional study. Transl. Pediatr. 9(3), 231–236. https://doi.org/10.21037/tp.2020.04.02 (2020).
Sun, P. et al. The psychological impact of COVID-19 pandemic on health care workers: A systematic review and meta-analysis. Front. Psychol. 12, 626547. https://doi.org/10.3389/fpsyg.2021.626547 (2021).
The Lancet Public Health. COVID-19 in Spain: A predictable storm?. Lancet Public Health 5(11), e568. https://doi.org/10.1016/S2468-2667(20)30239-5 (2020).
Alonso, J. et al. Mental health impact of the first wave of COVID-19 pandemic on Spanish healthcare workers: A large cross-sectional survey. Rev Psiquiatr Salud Ment (Engl Ed) 14(2), 90–105. https://doi.org/10.1016/j.rpsm.2020.12.001 (2021).
Mortier, P. et al. Thirty-day suicidal thoughts and behaviors among hospital workers during the first wave of the Spain COVID-19 outbreak. Depress Anxiety 38(5), 528–544. https://doi.org/10.1002/da.23129 (2021).
Wu, Y. et al. Equivalency of the diagnostic accuracy of the PHQ-8 and PHQ-9: A systematic review and individual participant data meta-analysis. Psychol. Med. 50(8), 1368–1380. https://doi.org/10.1017/S0033291719001314 (2020).
Diez-Quevedo, C., Rangil, T., Sanchez-Planell, L., Kroenke, K. & Spitzer, R. L. Validation and utility of the patient health questionnaire in diagnosing mental disorders in 1003 general hospital Spanish inpatients. Psychosom. Med. 63(4), 679–686. https://doi.org/10.1097/00006842-200107000-00021 (2001).
Kessler, R. C. et al. Clinical reappraisal of the composite international diagnostic interview screening scales (CIDI-SC) in the army study to assess risk and resilience in servicemembers (Army STARRS). Int. J. Methods Psychiatr. Res. 22(4), 303–321. https://doi.org/10.1002/mpr.1398 (2013).
Blasco, M. J. et al. Predictive models for suicidal thoughts and behaviors among Spanish University students: Rationale and methods of the UNIVERSAL (University and mental health) project. BMC Psychiatry 16, 122. https://doi.org/10.1186/s12888-016-0820-y (2016).
Zuromski, K. L. et al. Developing an optimal short-form of the PTSD checklist for DSM-5 (PCL-5). Depress Anxiety 36(9), 790–800. https://doi.org/10.1002/da.22942 (2019).
Garcia-Campayo, J. et al. Cultural adaptation into Spanish of the generalized anxiety disorder-7 (GAD-7) scale as a screening tool. Health Qual Life Outcomes 8, 8. https://doi.org/10.1186/1477-7525-8-8 (2010).
Newman, M. G. et al. Preliminary reliability and validity of the generalized anxiety disorder questionnaire-IV: A revised self-report diagnostic measure of generalized anxiety disorder. Behavior Therapy 33(2), 215–233. https://doi.org/10.1016/S0005-7894(02)80026-0 (2002).
Kroenke, K., Spitzer, R. L., Williams, J. B. & Lowe, B. The patient health questionnaire somatic, anxiety, and depressive symptom scales: A systematic review. Gen. Hosp. Psychiatry 32(4), 345–359. https://doi.org/10.1016/j.genhosppsych.2010.03.006 (2010).
Diez Martinez, S. et al. Brief questionnaires for the early detection of alcoholism in primary health care. Aten Primaria 8(5), 367–70 (1991) (Cuestionarios breves para la deteccion precoz de alcoholismo en atencion primaria).
Mdege, N. D. & Lang, J. Screening instruments for detecting illicit drug use/abuse that could be useful in general hospital wards: A systematic review. Addict. Behav. 36(12), 1111–1119. https://doi.org/10.1016/j.addbeh.2011.07.007 (2011).
Leon, A. C., Olfson, M., Portera, L., Farber, L. & Sheehan, D. V. Assessing psychiatric impairment in primary care with the Sheehan Disability Scale. Int. J. Psychiatry Med. 27(2), 93–105. https://doi.org/10.2190/T8EM-C8YH-373N-1UWD (1997).
Ormel, J. et al. Disability and treatment of specific mental and physical disorders across the world. Br. J. Psychiatry 192(5), 368–375. https://doi.org/10.1192/bjp.bp.107.039107 (2008).
Luciano, J. V. et al. Factor structure, internal consistency and construct validity of the Sheehan Disability Scale in a Spanish primary care sample. J. Eval. Clin. Pract. 16(5), 895–901. https://doi.org/10.1111/j.1365-2753.2009.01211.x (2010).
Posner, K. et al. The columbia-suicide severity rating scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am. J. Psychiatry 168(12), 1266–1277. https://doi.org/10.1176/appi.ajp.2011.10111704 (2011).
Van Buuren, S. Flexible Imputation of Missing Data 2nd edn. (CRC Press, Boca Raton, 2018).
Holmes, E. A. et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry 7(6), 547–560. https://doi.org/10.1016/S2215-0366(20)30168-1 (2020).
Al-Falasi, R. J. & Khan, M. A. The impact of COVID-19 on Abu Dhabi and its primary care response. Aust. J. Gen. Pract. https://doi.org/10.31128/AJGP-COVID-35 (2020).
Greenberg, N. Mental health of health-care workers in the COVID-19 era. Nat. Rev. Nephrol. 16(8), 425–426. https://doi.org/10.1038/s41581-020-0314-5 (2020).
Greenberg, N., Docherty, M., Gnanapragasam, S. & Wessely, S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ 368, m1211. https://doi.org/10.1136/bmj.m1211 (2020).
British Medical Association. The mental health and wellbeing of the medical workforce – now and beyond COVID-19. Available from: https://www.bma.org.uk/media/2475/bma-covid-19-and-nhs-staff-mental-health-wellbeing-report-may-2020.pdf
Aragones, E. et al. Psychological impact of the COVID-19 pandemic on primary care workers: A cross-sectional study. Br. J. Gen. Pract. 72(720), e501–e510. https://doi.org/10.3399/BJGP.2021.0691 (2022).
De Kock, J. H. et al. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: Implications for supporting psychological well-being. BMC Public Health 21(1), 104. https://doi.org/10.1186/s12889-020-10070-3 (2021).
Marvaldi, M., Mallet, J., Dubertret, C., Moro, M. R. & Guessoum, S. B. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 126, 252–264. https://doi.org/10.1016/j.neubiorev.2021.03.024 (2021).
Cheung, T. et al. Psychological impact on healthcare workers, general population and affected individuals of SARS and COVID-19: A systematic review and meta-analysis. Front. Public Health 10, 1004558. https://doi.org/10.3389/fpubh.2022.1004558 (2022).
D’Alessandro, A. M. et al. Healthcare workers and COVID-19-related moral injury: An interpersonally-focused approach informed by PTSD. Front. Psychiatry 12, 784523. https://doi.org/10.3389/fpsyt.2021.784523 (2021).
Riedel, P. L., Kreh, A., Kulcar, V., Lieber, A. & Juen, B. A scoping review of moral stressors, moral distress and moral injury in healthcare workers during COVID-19. Int. J. Environ. Res. Public Health 19(3), 1666. https://doi.org/10.3390/ijerph19031666 (2022).
Pabon-Carrasco, M. et al. Comparison of the psychological impact of COVID-19 on self-employed private healthcare workers with respect to employed public healthcare workers: Three-wave study during the COVID-19 pandemic in Spain. Healthc. Basel 11(1), 134. https://doi.org/10.3390/healthcare11010134 (2022).
Liu, S. et al. Gender differences in mental health problems of healthcare workers during the coronavirus disease 2019 outbreak. J. Psychiatr. Res. 137, 393–400. https://doi.org/10.1016/j.jpsychires.2021.03.014 (2021).
Di Tella, M., Romeo, A., Benfante, A. & Castelli, L. Mental health of healthcare workers during the COVID-19 pandemic in Italy. J. Eval. Clin. Pract. 26(6), 1583–1587. https://doi.org/10.1111/jep.13444 (2020).
Lopez-Atanes, M. et al. Gender-based analysis of the psychological impact of the COVID-19 pandemic on healthcare workers in Spain. Front. Psychiatry 12, 692215. https://doi.org/10.3389/fpsyt.2021.692215 (2021).
Elsayed, M. E. G. et al. Mental health, risk perception, and coping strategies among healthcare workers in Egypt during the COVID-19 pandemic. PLoS One 18(2), e0282264. https://doi.org/10.1371/journal.pone.0282264 (2023).
Lee, B. E. C., Ling, M., Boyd, L., Olsson, C. & Sheen, J. The prevalence of probable mental health disorders among hospital healthcare workers during COVID-19: A systematic review and meta-analysis. J. Affect. Disord. 330, 329–345. https://doi.org/10.1016/j.jad.2023.03.012 (2023).
Klose, M. & Jacobi, F. Can gender differences in the prevalence of mental disorders be explained by sociodemographic factors?. Arch. Womens Ment. Health 7(2), 133–148. https://doi.org/10.1007/s00737-004-0047-7 (2004).
Kuehner, C. Why is depression more common among women than among men?. Lancet Psychiatry 4(2), 146–158. https://doi.org/10.1016/S2215-0366(16)30263-2 (2017).
Ozdin, S. & Bayrak, O. S. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. Int. J. Soc. Psychiatry 66(5), 504–511. https://doi.org/10.1177/0020764020927051 (2020).
Vindegaard, N. & Benros, M. E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 89, 531–542. https://doi.org/10.1016/j.bbi.2020.05.048 (2020).
Vizheh, M. et al. The mental health of healthcare workers in the COVID-19 pandemic: A systematic review. J. Diabetes Metab. Disord. 19(2), 1967–1978. https://doi.org/10.1007/s40200-020-00643-9 (2020).
Vilar Palomo, S. et al. Assessment of the anxiety level of andalusian podiatrists during the COVID-19 pandemic: The increase phase. Healthc. Basel 8(4), 432. https://doi.org/10.3390/healthcare8040432 (2020).
Maunder, R. G. et al. Trends in burnout and psychological distress in hospital staff over 12 months of the COVID-19 pandemic: A prospective longitudinal survey. J. Occup. Med. Toxicol. 17(1), 11. https://doi.org/10.1186/s12995-022-00352-4 (2022).
Fattori, A. et al. Long-term trajectory and risk factors of healthcare workers’ mental health during COVID-19 pandemic: A 24 month longitudinal cohort study. Int. J. Environ. Res. Public Health 20(5), 4586. https://doi.org/10.3390/ijerph20054586 (2023).
Kroenke, K., Spitzer, R. L. & Williams, J. B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern Med. 16(9), 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x (2001).
Acknowledgements
The authors would like to sincerely thank all healthcareworkers that participated in the study in extremely busytimes, and MINDCOVID working group for supporting this reseach.
Funding
The study has received funding by Instituto de Salud Carlos III/Ministerio de Ciencia e Innovación/FEDER (Jordi Alonso, Grant number COV20/00711); ISCIII-FEDER (Jordi Alonso, Grant number PI17/00521); ISCIII-FSE, Sara Borrell and Miguel Servet (Philippe Mortier, Grant number CD18/00049 and CP21/00078), Generalitat de Catalunya (AGAUR 2021 SGR 00624).
Author information
Authors and Affiliations
Contributions
Contributors J.D.M., J.A., F.F.A., G.V. and P.M. reviewed the literature. J.A., G.V., P.M., conceived and designed the study. J.D.M., C.M.R., I.R.H., A.J.G., C.C.R. acquired the data. G.V., F.F.A. and P.M. cleaned and analyzed the data. J.D.M., J.A., F.F.A. and G.R. drafted the initial version of the manuscript. All authors reviewed the initial draft and made critical contribution to the interpretation of the data and approved the manuscript. The corresponding author attest that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Molina, J.D., Amigo, F., Vilagut, G. et al. Impact of COVID-19 first wave on the mental health of healthcare workers in a Front-Line Spanish Tertiary Hospital: lessons learned. Sci Rep 14, 8149 (2024). https://doi.org/10.1038/s41598-024-58884-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-58884-0
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.