Abstract
The increasing use of sodium glucose transporter 2 inhibitors (SGLT2i) for treating cardiovascular (CV) diseases and type 2 diabetes (T2D) is accompanied by a rise in euglycemic diabetic ketoacidosis occurrences in cardiac surgery patients. Patients undergoing cardiac surgery, due to their pre-existing CV disease which often requires SGLT2i prescriptions, face an increased risk of postoperative metabolic acidosis (MA) or ketoacidosis (KA) associated with SGLT2i, compounded by fasting and surgical stress. The primary aim of this study is to quantify the incidence of SGLT2i-related postoperative MA or KA and to identify related risk factors. We analyzed data retrospectively of 823 cardiac surgery patients, including 46 treated with SGLT2i from November 2019 to October 2022. Among 46 final cohorts treated preoperatively with SGLT2i, 29 (63%) developed postoperative metabolic complications. Of these 46 patients, stratified into two categories based on postoperative laboratory findings, risk factor analysis were conducted and compared. Analysis indicated a prescription duration over one week significantly elevated the risk of complications (Unadjusted OR, 11.7; p = 0.032*; Adjusted OR, 31.58; p = 0.014*). A subgroup analysis showed that a cardiopulmonary bypass duration of 60 min or less significantly raises the risk of SGLT2i-related postoperative MA in patients with a sufficient prescription duration. We omitted the term "diabetes" in describing complications related to SGLT2i, as these issues are not exclusive to T2D patients. Awareness of SGLT2i-related postoperative MA or KA can help clinicians distinguish between non-life-threatening conditions and severe causes, thereby preventing unnecessary tests and ensuring best practice.
Similar content being viewed by others
Introduction
The U.S. Food and Drug Administration (FDA) granted approval for dapagliflozin, a sodium-glucose transporter 2 inhibitor (SGLT2i), in 2011 for the treatment of type 2 diabetes (T2D). Subsequent research has extensively shown the efficacy of these inhibitors in treating a broader spectrum of cardiovascular (CV) diseases. Two landmark trials—DAPA-HF (Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction)1 and EMPEROR-Reduced (Cardiovascular and Renal Outcomes with Empagliflozin in Heart Failure)2—have explored the effectiveness of SGLT2i in treating heart failure with reduced ejection fraction (HFrEF), irrespective of the presence of T2D. Further studies like EMPEROR-preserved (Empagliflozin in Heart Failure with a Preserved Ejection Fraction)3 and DELIVER (Dapagliflozin in Heart Failure with Mildly Reduced or Preserved Ejection Fraction)4 have broadened their applicability to HF patients with preserved or mildly reduced EF (HFpEF or HFmrEF) irrespective of T2D status. In alignment with these findings, the 2021 European Society of Cardiology guidelines for the treatment of acute and chronic HF recommended dapagliflozin or empagliflozin for patients with HFrEF to reduce the risk of hospitalization for HF (HHF) and death (Class IA)5. Furthermore, the 2022 ACC/AHA/HFSA Guideline for the Management of HF6 advocated for the use of SGLT2i in patients with symptomatic chronic HFrEF to reduce HHF and CV mortality, irrespective of the presence of T2D. More recently, empagliflozin now has FDA approval for reducing HHF or CV death among patients with HFpEF, defined as left ventricular EF being greater than 40%, with or without diabetes7. With the comprehensive management of cardio-renal-metabolism being emphasized, the utilization of SGLT2i is expected to increase over the years, not only in patients with T2D but also in those with CV disease or diabetic kidney disease.
Regarding diabetic ketoacidosis (DKA) related to SGLT2i, these medications have been associated with an elevated risk of DKA8,9. In 2015, the FDA issued a warning about the potential for these drugs to cause ketoacidosis, which generated considerable attention10. Numerous studies have documented instances of 'euglycemic' DKA (EDKA), generally characterized by normoglycemia with a plasma glucose level of less than 200 mg/dL, in T2D patients treated SGLT2i11,12,13,14.
In the perioperative setting, diagnosing SGLT2i-related EDKA becomes more complicated due to the specific postoperative status of patients. Several studies have already highlighted the issue of unrecognized diagnosis of SGLT2i-related EDKA in this context. Thiruvenkatarajan. et al. reported a 89% prevalence of postoperative SGLT2i-related EDKA in systematic review15, while Blau. et al. found a 71% incidence in their research using FDA data16. Among cardiac surgery patients, Murugesan, K.B. observed a 70.8% incidence of SGLT2i-related ketoacidosis (KA)17. Given these findings, it is imperative to differentiate SGLT2i-induced KA in cardiac surgery patients for the following reasons:
-
1.
Due to shared patient population with HF, cardiac surgery patients show a higher incidence of SGLT2i usage than other surgical patients.
-
2.
While the surgical stress is a known risk factor for SGLT2i-induced EDKA, cardiac surgery is unique in the implementation of cardiopulmonary bypass (CPB), setting it apart from other surgical procedures.
-
3.
The laboratory presentations of SGLT2i-induced KA may mimic those of other severe postoperative complications in cardiac surgery patients, leading to potential diagnostic delays and additional expenditures.
Moreover, the clinical application of SGLT2i expands in CV patients, six cases of postoperative SGLT2i-related KA following cardiac surgery were identified in our center. Given the subtle presentation of SGLT2i-related KA, we hypothesized that it might be underdiagnosed, prompting a retrospective analysis of cardiac surgery patients who were preoperatively administered SGLT2i. Due to the retrospective nature of the study, confirmation of ketone body presence could not be conducted for all patients except the six identified; hence, their condition was termed as SGLT2i-related metabolic acidosis (MA).
The primary aim of this study is to quantify the incidence of postoperative SGLT2i related KA or MA and to identify related risk factors. Such insights could assist clinicians in differentiating SGLT2i-associated postoperative KA or MA, which is typically non-life-threatening18, from cardiac or other severe causes of MA, thus preventing unnecessary tests and prolonged intensive care unit (ICU) stays. Furthermore, this study assessed the impact of CPB, which induces a reduction in plasma protein concentration during bypass, on SGLT2i-related KA or MA19.
Materials and methods
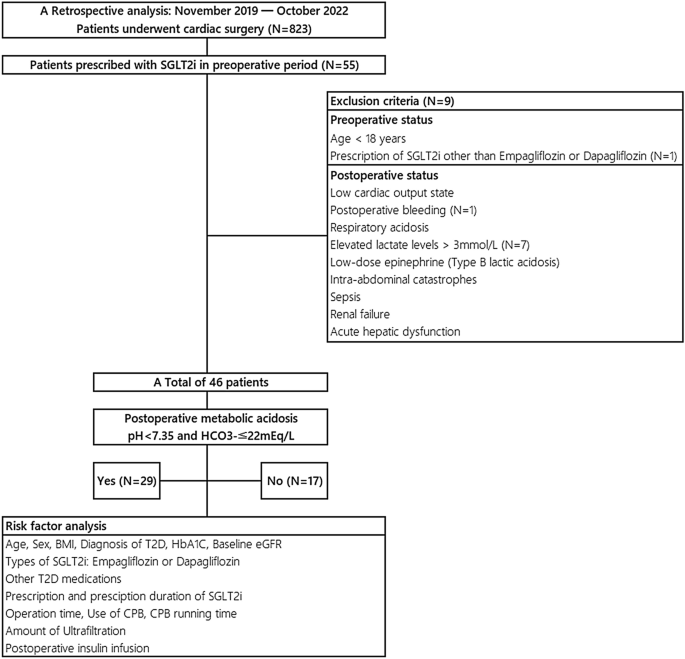
This study is a retrospective analysis of 823 patients who underwent cardiac surgery at Incheon Sejong Hospital from November 2019 to October 2022. Of the initial cohort, 55 were preoperatively prescribed SGLT2i. Exclusion criteria were set for conditions likely to induce postoperative acidosis20, including low cardiac output, postoperative bleeding, respiratory acidosis, elevated lactate levels (> 3 mmol/L), low-dose epinephrine (Type B lactic acidosis), intra-abdominal catastrophes, sepsis, renal failure, and acute hepatic dysfunction. An additional patient prescribed an SGLT2i other than Empagliflozin or Dapagliflozin was excluded for study consistency. Subsequently, the refined cohort consisted of 46 patients, stratified into two categories based on postoperative laboratory findings: the MA group (pH < 7.35 and HCO3- ≤ 22 mEq/L, n = 27) and the non-MA group (pH ≥ 7.35 or HCO3- > 22 mEq/L, n = 19). [Fig. 1] In both groups, we collected data on preoperative baseline characteristics, intraoperative factors, and immediate postoperative factors to identify risk factors associated with SGLT2i-related KA or MA.
Patient selection, exclusion criteria and risk factor analysis. From November 2019 to October 2022, we conducted a retrospective analysis on 823 cardiac surgery patients at our center, 46 of whom were preoperatively treated with SGLT2i, specifically dapagliflozin or empagliflozin. Based on postoperative arterial blood gas analysis, patients were categorized into two groups: those with postoperative metabolic acidosis and those without. SGLT2i sodium-glucose transporter 2 inhibitors, BMI body mass index, T2D type 2 diabetes, HbA1c Hemoglobin A1C, eGFR estimated glomerular filtration rate, CPB cardiopulmonary bypass.
To clarify, the postoperative period generally refers to the time starting immediately after surgery, typically beginning with the patient's admission to the ICU. At our institution, preoperative glycemic control in T2D patients is managed with a glucose-insulin mix or glucose-insulin-potassium (GIK) solution, following endocrinologist consultation. Postoperatively, we follow ICU protocol to maintain blood glucose between 110 and 150 mg/dL using insulin infusion20. Both preoperative and postoperative insulin infusions are administered as mentioned earlier.
Statistical analysis
The IBM SPSS software, version 21.0, was utilized for data analysis. Continuous variables were expressed as mean ± standard deviation (SD) or as median (25th and 75th percentiles), while categorical variables were presented as frequency counts and percentages (n%). Independent t-tests and χ2 tests were employed, as appropriate, to compare variables such as types of SGLT2i, arterial blood gas analyses (ABGA), duration of mechanical ventilator (MV) support, and length of ICU stay between the postoperative MA group and the non-MA group. The Mann–Whitney U test was used to compare the number of inotropes administered between the two groups. Univariate logistic regression analysis was conducted to identify potential associated risk factors in preoperative, intraoperative and postoperative period. The covariables for the multivariable logistic regression model were selected based on clinical judgement and a comprehensive review of existing literature. The variables evaluated in this model include Body Mass Index (BMI), the status of preoperative insulin usage, duration of SGLT2i prescription and cessation, operating time, CPB duration, and postoperative insulin utilization. Also, CPB running time was divided into before and after 60 min to indicate a short CPB running time. While there is no basis for specifically choosing 60 min, but generally, one shot of cardioplegia lasts between 60 to 90 min, depending on the type of cardioplegia used. We set 60 min as the criterion for short CPB time, which is also related to the reduction of plasma protein concentration and the duration or amount of ultrafiltration. The impact CPB duration on postoperative MA or KA associated with SGLT2i was examined in a subgroup analysis of patients with sufficient prescription duration. The odds ratio (OR) or hazard ratio (HR) are presented with a 95% confidence interval(CI) for inferential statistics, and a two-sided P-value of less than 0.05 was statistically significant.
Ethics approval and consent to participate
Given the retrospective design of this study and the fact that there was no harm to participants, the Institutional Review Board of Incheon Sejong Hospital approved a waiver for the requirement of informed consent. (IRB approval no. 2022-09-001). All personal and clinical data, including laboratory results and patient outcomes, were obtained from the patients' medical records. All the methods were carried out in accordance with relevant guidelines and regulations.
Results
Demographic and postoperative profile of the study cohort
In a retrospective study of 46 patients undergoing cardiac surgeries, 26 (56.5%) were prescribed dapagliflozin, and 29 (63%) developed postoperative SGLT2i-related MA. Clinical and demographic characteristics of the study population are shown in [Table 1]. The average of age was 62.2 ± 11.14 year and BMI was 24.78 ± 3.3 kg/\({m}^{2}\). Of the 46 patients, 33 (71.3%) were men, and 42 (91.3%) had a past medical history of T2D. Blood glucose levels in both groups were investigated, and no statistical difference was found (117.7 ± 61.2 vs. 191.4 ± 35.3; p = 0.373). Furthermore, no statistically significant difference was noted between the two groups regarding the duration of MV support or the length of ICU stay. When evaluating the quantity of inotropes administered, instances of postoperative MA associated with SGLT2i exhibited a greater proportion of patients with a high inotropic demand (more than 2 agents); however, this variance was not statistically significant. (5 (17.2%) vs. 0 (0%); p = 0.140).
Clinical variables and incidence of SGLT2i -related postoperative MA
The potential risk factors, preoperative, intraoperative and postoperative variables, associated with SGLT2i-related postoperative MA were examined in univariate and multivariable regression analyses [Table 2]. We included factors with a p-value of less than 0.2 in the univariate analysis as significant variables in the multivariable logistic regression test. Additionally, we incorporated the presence of insulin-dependent T2D, a previously known precipitating factor for DKA, and the cessation time of more than 72 h for SGLT2i, as specified in the guidelines for the prevention of EDKA, into the analysis.
Preoperative factors
In the unadjusted analysis, several factors—including age, sex, BMI, premedical history of T2D, hemoglobin A1C (HbA1c) levels, preoperative glucose-insulin mixed infusion, use of other T2D medications, duration of SGLT2i cessation, and baseline estimated glomerular filtration rate (eGFR)—did not exhibit statistically significant differences between the postoperative MA group and the non-MA group. However, a prescription duration of SGLT2i of more than one week was associated with SGLT2i-related postoperative MA (OR, 11.7; 95% CI 1.65–237; p = 0.032*). In the multivariable analysis, this association remained significant (adjusted OR, 31.58; 95% CI 1.97–505.23; p = 0.014*).
Intraoperative factors
Regarding intraoperative factors, we assessed the types of operations conducted, the duration of these operations, the utilization of CPB, the duration of CPB running time, instances where CPB exceeded 60 min (referred as CPB 60), and the volume of ultrafiltration. In the univariate analysis, no statistically significant differences in intraoperative factors between the two groups were observed. In the adjusted model, which examined potential risk factors associated with postoperative MA or KA related to SGLT2i—including operation time and CPB 60—no statistical significance was found.
Postoperative factors
In both the univariate and multivariable models, the immediate postoperative administration of insulin infusion did not show any statistically significant differences between the group with postoperative MA related to SGLT2i and the non-MA group. (Unadjusted OR: 0.44; 95% CI 0.12–1.49; p = 0.197; Adjusted OR: 0.40; 95% CI 0.07–2.22; p = 0.298).
Subgroup analysis: impact of CPB running time on SGLT2i-related postoperative MA in patients with sufficient prescription duration
A subgroup analysis was conducted to assess the impact of CPB duration in patients with a sufficient SGLT2i prescription duration over 7 days (N = 40). Table 3 shows that a CPB duration ≤ 60 min is associated with a significantly higher risk of SGLT2i-related postoperative MA (HR 2.94; 95% CI 0.50–5.38, p = 0.018*).
Discussion
For individuals with T2D, the prevalence of DKA or EDKA following the introduction of SGLT2i remains uncertain. In predominantly non-operative settings, in clinical trials involving SGLT2i for T2D treatment, the incidence of DKA ranged from 0.2 to 0.8 cases per 1000 patient-years21,22. The DKA incidence in T2D patients on SGLT2i might not be higher than in the wider diabetic population; however, clinical trials may not fully reflect real-world incidences. In a meta-analysis of 36 trials that evaluated T2D drug therapies, SGLT2i were the only class of drugs associated with an increased risk of DKA compared to other therapies23. A large-scale study from Canada and the United Kingdom, involving over 350,000 patients and 500 DKA cases, noted an increased risk with SGLT2i (dapagliflozin, empagliflozin, canagliflozin) compared to dipeptidyl peptidase-4 inhibitors, with respective incidence rates of 2.03 and 0.75 per 1,000 patient-years, and heightened DKA risks associated with dapagliflozin (HR: 1.86) and empagliflozin (HR: 2.52)24.
As known, several factors are recognized to precipitate DKA in the context of SGLT2i use. Patient characteristics such as insulin deficiency, commonly seen in latent autoimmune diabetes in adults, type 1 diabetes, or some individuals with long-standing T2D, have been noted25. Metabolic stressors like surgical interventions, vigorous exercise, myocardial infarctions, strokes, severe infections, and prolonged fasting have also been identified as significant contributors25,26. Other risk variables that could potentially predispose an individual to KA include pancreatic insulin deficiency, reductions in prescribed insulin dosage, caloric restriction, alcohol misuse and acute febrile illness.
Regarding perioperative patients with SGLT2i-related KA or MA, Thiruvenkatarajan et al. reported a prevalence of 89% for postoperative SGLT2i-related EDKA in their systematic review15. Blau. et al. using FDA data, found a comparable incidence rate of 71% (29 out of 51)16 and Murugesan, K.B. observed a 70.8% (17 out of 24) for SGLT2i-associated EDKA in cardiac surgery patients17. Each study has different criteria, making comparison somewhat nonsensical; however, our study identified a 63% incidence (29 out of 46) of SGLT2i-related KA or MA, which aligns with previous studies and shows no significant statistical difference, as evidenced by p-values of 0.598 and 0.278, respectively.
Patients undergoing cardiac surgery represent a unique demographic at an intersection of heightened risk for postoperative MA or KA associated with SGLT2i, primarily because they have pre-existing CV disease, which often necessitates the prescription of SGLT2i. Moreover, these patients typically undergo fasting and experience the surgical stress. Despite these compounded risk factors, the risk-to-benefit ratio overwhelmingly supports the continued use of SGLT2i for managing CV disease or T2D, and current guidelines uphold this stance.
With the rising use of SGLT2i for treating CV disease, we observed six patients who developed postoperative KA associated with these medications. Table 4 details these patients with confirmed ketone bodies who suffered from SGLT2i-related postoperative KA. Notably, there was no consistent pattern regarding the hours of onset of ketoacidosis among these patients. For our first patient (case #1) was involved in extended diagnostic process such as bedside transthoracic echocardiography and cardiac angiography and resulting in a 24-h diagnostic delay. This initial experience facilitated more straightforward diagnoses in subsequent cases, highlighting the importance of considering SGLT2i related EDKA in the care of post-cardiac surgery patients to prevent diagnostic delays. Interestingly, one patient (case #6) without a prior medical history of T2D also exhibited postoperative KA. This implies that these incidents may not be limited only to patients with diabetes, but might also include those using SGLT2i. Therefore, we referred to this condition not as SGLT2i related EDKA, but as postoperative MA or KA related to SGLT2i, omitting the term 'diabetic’. A mechanism associated with SGLT2 inhibition appears to induce an early transition to fat metabolism, leading to an accumulation of ketones and resulting in KA or MA27.
We conducted a retrospective review to assess the incidence and risk factors of postoperative MA or KA related to SGLT2i in 46 cardiac surgery patients; 63% (29 patients) developed postoperative MA associated with SGLT2i [Fig. 1]. Although the threshold for MA might differ across clinical laboratories, we characterized SGLT2i-related postoperative MA based on the criteria of a pH < 7.35 and an HCO3- ≤ 22 mEq/L28. While our chosen threshold could be relatively liberal, we believe it is crucial to initially rule out benign but potentially concerning laboratory anomalies in post-cardiac surgery patients.
Cessation duration, according to the prescribing information29,30, dictates that SGLT2i should be discontinued 72 h prior to surgery.. In the univariate analysis, a cessation duration of more than 72 h in the preoperative period did not result in a significant decrease in the occurrence of SGLT2i-related postoperative MA or KA (unadjusted OR, 0.58; 95% CI 0.16–2.20; p = 0.42) [Table 2]. This lack of significance might suggest that the advised cessation period is shorter than actually needed.
A significant proportion of the cohort, 12 out of 46 (26%), were prescribed SGLT2i at the time of their CV diagnosis, within 1 month before their cardiac surgery. The univariate analysis indicated that a prescription duration exceeding 7 days significantly increased the incidence of SGLT2i-related postoperative MA (unadjusted OR, 11.7; 95% CI 1.65–237; p = 0.032*). This significance persisted in the multivariable analysis (adjusted OR, 31.58; 95% CI 1.97–505.23; p = 0.014*) [Table 2]. Our assumption is that the shift to fat metabolism induced by SGLT2 inhibition takes at least a few days, and patients who were prescribed for less than 7 days actually took SGLT2i for 3–5 days, considering the preoperative cessation period.
Furthermore, a subgroup analysis was performed to assess the impact of CPB running time on the occurrence of SGLT2i-related postoperative MA or KA. [Table 3] While ultrafiltration is employed to concentrate blood during CPB operations, reductions in both plasma colloid osmotic pressure and total protein concentration were noted following CPB use19. Following a decrease in protein levels, including drug-binding proteins, we hypothesized that the utilization of CPB might reduce the incidence of postoperative MA or KA associated with SGLT2i. Among patients prescribed SGLT2i for a sufficient duration (> 7 days, N = 40), those undergoing cardiac surgery with a short CPB running time (≤ 60 min) exhibited a higher risk of postoperative SGLT2i-related MA(OR, 2.94; 95% CI 0.50–5.38; p = 0.018*).
Rapid resolution of metabolic abnormalities induced by SGLT2i was observed after initiating insulin and dextrose infusions, as stated by Aaron Lau et al. in their case series31. Our findings were consistent with this; resolution of postoperative KA related to SGLT2i was easily achieved in our cases as well [Table 4]. Given that the ICU hyperglycemic management protocol for cardiac surgery patients targets a postoperative blood sugar range of 110 to 150 mg/dL and initiates a corrective protocol for levels above 150 mg/dL20, it was hypothesized that this protocol could incidentally manage undiagnosed cases of postoperative MA or KA related to SGLT2i. Despite this assumption, our analysis found that postoperative insulin infusion did not significantly affect the incidence of MA associated with SGLT2i (unadjusted OR, 0.44; 95% CI 0.12–1.49; p = 0.197; adjusted OR, 0.40; 95% CI 0.07–2.22; p = 0.298). [Table 2].
For our strategy in managing post-cardiac surgery patients without kidney disease, we utilized a GIK solution to treat KA associated with SGLT2i. Electrolyte imbalances in post-cardiac surgery patients can provoke arrhythmias, making the restoration of potassium levels especially crucial in this patient population.
Based on our findings, we advocate for the verification of ketone bodies using urine or serum ketone tests in post-cardiac surgery patients who present with high anion-gap MA, a condition solely attributable to the preoperative use of SGLT2i. As a time and cost-effective approach, we assess urine ketone levels through routine urinalysis, which provides results within 30 min in these patients. When patients present with a urine ketone level exceeding 2 +, we subsequently conduct a serum ketone test, which often requires 2–3 days for results, and initiate GIK solution administration concomitantly.
Limitations
Given the nature of a retrospective observational study, ketone body tests were not routinely included in postoperative laboratory tests, so ketone body confirmations could not be conducted for all patients. Regarding ICU management, there was a lack of uniformity among physicians, and unnecessary injections of sodium bicarbonate affected anion gap and pH levels. Furthermore, this issue spoiled anion gap, which is crucial for differentiating postoperative hyperchloremic metabolic acidosis, thereby preventing the establishment of an accurate exclusion criteria. As a single-center study, there were deviations in operation entities, with a scarcity of aortic surgeries.
Conclusion
The CV benefits of SGLT2i in patients with CV disease are undeniably profound. Not every case of KA is necessarily harmful, but the FDA-issued warnings about these risks have not been sufficiently integrated into perioperative care protocols. The lack of awareness complicates diagnosis and treatment of postoperative metabolic issues related to SGLT2i. However, our research shows that timely diagnosis and proper treatment can ease the patient's transition from ICU support to general wards.
In describing the postoperative metabolic issues observed in our study, we chose not to use the term 'diabetes' to highlight the possibility that these conditions might extend beyond patients with T2D. Further research is needed concerning the optimal duration for preoperative cessation of SGLT2i. Additionally, it is imperative to study the effects of CPB institution on SGLT2i-related postoperative KA in patients, including the assessment of SGLT2i-induced KA among nondiabetic individuals.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- FDA:
-
Food and Drug administration
- SGLT2i:
-
Sodium-glucose transporter 2 inhibitors
- T2D:
-
Type 2 diabetes
- CV:
-
Cardiovascular
- HFrEF:
-
Heart failure with reduced ejection fraction
- HFpEF:
-
Heart failure with preserved ejection fraction
- HFmrEF:
-
Heart failure with mildly reduced ejection fraction
- HHF:
-
Hospitalization for heart failure
- DKA:
-
Diabetic ketoacidosis
- EDKA:
-
Euglycemic diabetic ketoacidosis
- KA:
-
Ketoacidosis
- CPB:
-
Cardiopulmonary bypass
- MA:
-
Metabolic acidosis
- ICU:
-
Intensive care unit
- GIK solution:
-
Glucose-insulin-potassium solution
- SD:
-
Standard deviation
- ABGA:
-
Arterial blood gas analyses
- MV:
-
Mechanical ventilator
- BMI:
-
Body mass index
- OR:
-
Odds ratio
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- HbA1c:
-
Hemoglobin A1C
- eGFR:
-
Estimated glomerular filtration rate
References
McMurray, J. V. et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N. Engl. J. Med. 381(21), 1995–2008 (2019).
Packer, M. et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. N. Engl. J. Med. 383(15), 1413–1424 (2020).
Anker, S. D. et al. Empagliflozin in heart failure with a preserved ejection fraction. N. Engl. J. Med. 385(16), 1451–1461 (2021).
Solomon, S. D. et al. Dapagliflozin in heart failure with mildly reduced or preserved ejection fraction. N. Engl. J. Med. 387(12), 1089–1098 (2022).
McDonagh, T. A. et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 42(36), 3599–3726 (2021).
Paul, A. H. et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure. J. Card. Fail. 28(5), e1–e167 (2022).
Larkin, H. D. FDA expands empagliflozin heart failure indication. JAMA 327(13), 1219–1219. https://doi.org/10.1001/jama.2022.3970 (2022).
Marilly, E. et al. SGLT2 inhibitors in type 2 diabetes: A systematic review and meta-analysis of cardiovascular outcome trials balancing their risks and benefits. Diabetologia 65(12), 2000 (2022).
Liu, J. et al. Sodium-glucose co-transporter-2 inhibitors and the risk of diabetic ketoacidosis in patients with type 2 diabetes: A systematic review and meta-analysis of randomized controlled trials. Diabetes Obes. Metab. 22(9), 1619 (2020).
FDA Drug Safety Communication: FDA revises labels of SGLT2 inhibitors for diabetes to include warnings about too much acid in the blood and serious urinary tract infections. Food and Drug Administration. http://www.fda.gov/Drugs/DrugSafety/ucm475463.htm (2021).
Heidi, G. & David, W. L. Endocrine emergencies. In Diabetic Emergencies: Ketoacidosis, Hyperglycemic Hyperosmolar State, and Hypoglycemia 5th edn (eds Heidi, G. & David, W. L.) 167–182 (Elsevier, 2020).
Peters, A. L. et al. Euglycemic diabetic ketoacidosis: A potential complication of treatment with sodium-glucose cotransporter 2 inhibition. Diabetes Care 38(9), 1687 (2015).
Fralick, M., Chneeweiss, S. & Patorno, E. Risk of diabetic ketoacidosis after initiation of an SGLT2 inhibitor. N. Engl. J. Med. 376(23), 2300 (2017).
Ueda, P. et al. Sodium glucose cotransporter 2 inhibitors and risk of serious adverse events: Nationwide register based cohort study. BMJ 363, k4365 (2018).
Thiruvenkatarajan, V. et al. Perioperative diabetic ketoacidosis associated with sodium-glucose co-transporter-2 inhibitors: A systematic review. Br. J. Anaesth. 123, 27–36 (2019).
Blau, J. E., Tella, S. H., Taylor, S. I. & Rother, K. I. Ketoacidosis associated with SGLT2 inhibitor treatment: Analysis of FAERS data. Diabetes Metab. Res. Rev. https://doi.org/10.1002/dmrr.2924 (2017).
Murugesan, K. B., Balakrishnan, S., Arul, A., Ramalingam, S. & Srinivasan, M. A retrospective analysis of the incidence, outcome and factors associated with the occurrence of euglycemic ketoacidosis in diabetic patients on sodium glucose co-transporter—2 inhibitors undergoing cardiac surgery. Ann. Card. Anaesth. 25(4), 460–465 (2022).
Plewa, M. C., Bryant, M. & King-Thiele, R. Euglycemic Diabetic Ketoacidosis (StatPearls Publishing, 2022).
English, T. A. H., Stan, D. & Kirklin, J. W. Changes in colloid osmotic pressure during and shortly after open intracardiac operation. J. Thorac. Cardiovasc. Surg. 61(3), 338–341 (1971).
Bojar, R. M. Manual of Perioperative Care in Adult Cardiac Surgery 6th edn. (Wiley, 2020).
Ngozi, E., Mehul, D., Kirk, W. & Gary, M. Diabetic ketoacidosis and related events in the Canagliflozin type 2 diabetes clinical program. Diabetes Care 38, 1680–1686 (2015).
Zinman, B., Wanner, C. & Lachin, J. M. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N. Engl. J. Med. 373(22), 2117–2128 (2015).
Shi, Q. et al. Benefits and harms of drug treatment for type 2 diabetes: Systematic review and network meta-analysis of randomized controlled trials. BMJ 381, e074068 (2023).
Douros, A. et al. Sodium-glucose cotransporter-2 inhibitors and the risk for diabetic ketoacidosis: A multicenter cohort study. Ann. Intern. Med. 173(6), 417–425 (2020).
Handelsman, Y. et al. American association of clinical endocrinologists and American college of endocrinology position statement on the association of SGLT-2 inhibitors and diabetic ketoacidosis. Endocr. Pract. 22(6), 753–762 (2016).
Fitchett, D. A safety update on sodium glucose co-transporter 2 inhibitors. Diabetes Obes. Metab. 21(Suppl 2), 34–42 (2019).
Ogawa, W. & Sakaguchi, K. Euglycemic diabetic ketoacidosis induced by SGLT2 inhibitors: Possible mechanism and contributing factors. J. Diabetes Investig. 7(2), 135–138 (2016).
Fenves, A. Z. & Emmett, M. Approach to patients with high anion gap metabolic acidosis: Core curriculum 2021. Am. J. Kidney Dis. 78(4), 590–600 (2021).
Wilmington, D. E. Farxiga (Dapagliflozin) [Prescribing Information] (AstraZeneca Pharmaceuticals LP, 2023).
Ridgefield, C. T. Jardiance (Empagliflozin) [Prescribing Information] (Boehringer Ingelheim Pharmaceuticals Inc, 2023).
Lau, A. et al. Perioperative implications of sodium-glucose cotransporter-2 inhibitors: A case series of euglycemic diabetic ketoacidosis in three patients after cardiac surgery. Can. J. Anaesth. 65(2), 188–193 (2018).
Author information
Authors and Affiliations
Contributions
Conceptualization and design: HA Kim, JY Kim. Analysis and interpretation: HA Kim. Data collection: HA Kim, JY Kim. Writing original draft, Fig. 1 and Tables 1, 2, 3, 4: HA Kim. Review and editing: All authors. Statistical analysis: HA Kim. Funding: N/A. The requirement for informed consent was waived due to the retrospective nature of the study. All personal and clinical data, including laboratory results and patient outcomes, were obtained from the patients' medical records.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, H.A., Kim, J.Y., Kim, Y.H. et al. Missed postoperative metabolic acidosis associated with sodium-glucose transporter 2 inhibitors in cardiac surgery patients: a retrospective analysis. Sci Rep 14, 8087 (2024). https://doi.org/10.1038/s41598-024-58853-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-58853-7
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.