Abstract
Several phase II studies have demonstrated that psilocybin-assisted therapy shows therapeutic potential across a spectrum of neuropsychiatric conditions, including major depressive disorder (MDD). However, the mechanisms underlying its often persisting beneficial effects remain unclear. Observational research suggests that improvements in psychological flexibility may mediate therapeutic effects. However, no psychedelic trials to date have substantiated this finding in a clinical sample. In an exploratory placebo-controlled, within-subject, fixed-order study, individuals with moderate to severe MDD were administered placebo (n = 19) followed by psilocybin (0.3 mg/kg) (n = 15) 4 weeks later. Dosing sessions were embedded within a manualized psychotherapy that incorporated principles of Acceptance and Commitment Therapy. Depression severity, psychological flexibility, mindfulness, and values-congruent living were measured over a 16-weeks study period. Psychological flexibility, several facets of mindfulness, and values-congruent living significantly improved following psilocybin and were maintained through week 16. Additionally, improvements in psychological flexibility and experiential acceptance were strongly associated with reductions in depression severity following psilocybin. These findings support the theoretical premise of integrating psilocybin treatment with psychotherapeutic platforms that target psychological flexibility and add to emerging evidence that increasing psychological flexibility may be an important putative mechanism of change in psilocybin-assisted therapy for MDD and potentially, other mental health conditions.
Similar content being viewed by others
Introduction
In recent years, there has been a revitalization of interest in the therapeutic potential of psychedelic substances for a variety of neuropsychiatric and behavioral health conditions1,2. Psilocybin, a naturally occurring alkaloid found in the Psilocybe genus of mushrooms, is categorized as a “classical psychedelic” compound along with lysergic acid diethylamide (LSD), dimethyltryptamine (DMT), and others. These drugs produce a range of acute perceptual and mood alterations in humans presumably through agonism of brain serotonin 5HT-2A receptors3,4.
In the past decade, a number of early phase trials have suggested that psilocybin-assisted therapy (i.e., embedding psilocybin dosing sessions within a framework of psychological support or psychotherapy) may have rapid acting and persisting therapeutic effects across a number of mental health conditions, including depression, anxiety, and substance use disorders5,6,7,8,9,10,11,12,13,14. These beneficial effects have been reported after just one or two doses of psilocybin, and in some cases, may persist up to 1–4.5 years post-administration15,16.
However, the mechanisms by which psilocybin-assisted therapy may produce both rapid and sustained antidepressant effects remain unclear. A number of neurobiological, psychological, cognitive/behavioral and spiritual mechanisms have been proposed to explain psilocybin-assisted therapy’s rapid and sustained antidepressant effects. For instance, certain psilocybin treatment studies have found that positive clinical outcomes were correlated with or partially-mediated by mystical-type subjective experiences12,13,14,17,18 or alterations in neuroplasticity19. Other potential psychological and cognitive/behavioral mechanisms include increased psychological flexibility and experiential acceptance20,21,22, increased connectedness23,24, relaxation and revision of high-level beliefs25,26, and emotional breakthrough27.
Given that multiple potential mechanisms may contribute to the therapeutic effects of psilocybin-assisted therapy, it remains unclear which psychotherapeutic models and approaches are optimal. Some studies have employed non-specific supportive psychotherapeutic models while others have incorporated elements of evidence-based, condition-specific therapies. In developing a therapeutic approach for an exploratory clinical trial of psilocybin-assisted therapy for major depression, our group sought an evidence-based therapy that would be synergistic with the subjective effects of psilocybin and offer a structure for the preparation and integration psychotherapy sessions. After evaluating a range of potential therapies, we selected Acceptance and Commitment Therapy (ACT) given conceptual and phenomenological overlaps between ACT and psilocybin-assisted therapy20.
Within Acceptance and Commitment Therapy, psychological flexibility is conceptualized as the central organizing principle underlying mental well-being and therapeutic change28. Psychological flexibility is a multifaceted construct composed of: (a) openness to experience (experiential acceptance); (b) behavioral awareness (i.e., mindful attention to the present moment); and (c) values-driven action29. In line with this model, global psychological inflexibility and several of its subcomponents (most notably experiential avoidance) have been linked with depression severity (for reviews, see30,31) and improvement in these measures linked with clinical improvement following ACT32,33,34,35.
Psychedelics and psychological flexibility
A growing body of research suggests that psychedelic therapy may increase psychological flexibility and lead to therapeutic benefits via these changes. Several cross-sectional and observational studies have found that use of a classic psychedelic is associated with subsequent increases in psychological flexibility21,36,37,38. Furthermore, following classic psychedelic use, increases in psychological flexibility have been found to be associated with improvements in mental health, including depressive symptoms22,36, anxious/depressive symptoms21, positive and negative affect37, and grief38. These findings suggest that psychological flexibility may be a transdiagnostic mechanism contributing to the positive effects of psychedelics. Importantly, research has not yet examined the effect of psilocybin-assisted therapy on psychological flexibility (or the effect of any psychedelic on psychological flexibility) within a clinical sample. Furthermore, no clinical trials to date have examined the association between increases in psychological flexibility and improvements in depressive symptoms following psilocybin-assisted therapy.
Mindfulness (defined as awareness and acceptance of one’s inner experiences)39 is closely related to several components of psychological flexibility, including behavioral awareness and experiential acceptance29,40. In a sample with MDD, a recent randomized controlled trial found that, relative to escitalopram, psilocybin-assisted therapy led to greater increases in experiential acceptance5. Furthermore, within this trial, increases in experiential acceptance following psilocybin-assisted therapy predicted improvements in depression severity, anxiety, suicidal ideation, and well-being41. Within non-clinical samples, several studies have observed increases in facets of mindfulness (most consistently the facets of experiential acceptance/non-judgmental awareness) following use/administration of classic psychedelics22,42,43,44,45,46,47,48,49, including psilocybin50,51,52 (for a review, see53). Furthermore, in observational studies, increases in non-judgment of inner experience (closely related to experiential acceptance) following psilocybin were associated with reductions in anxiety50. However, no clinical trials have examined the effect of psilocybin-assisted therapy on mindfulness or its association with treatment outcomes.
Several naturalistic studies have found that classic psychedelic use is associated with changes in values. Among individuals that reported decreases in smoking following classic psychedelic use, participants attributed changes in life priorities/values as the primary psychological factor that contributed to this behavior change54. Research has also found that administration of psilocybin alongside support for spiritual practice is associated with increases in valuing of tradition55. However, the effect of classic psychedelics on values has not yet been examined in the context of a psychedelic clinical trial or within a clinical sample.
In sum, psychological flexibility is a promising putative transdiagnostic mechanism underlying psychotherapeutic interventions and potentially, the beneficial effects of psychedelic therapy. However, to date, research has not examined the effect of psilocybin-assisted therapy on (a) psychological flexibility; (b) mindfulness; or (c) values within a clinical trial. Furthermore, clinical research has not yet examined whether psilocybin-assisted therapy leads to improvements in depression severity via its effects on psychological flexibility. Finally, research has not yet evaluated the effect of psilocybin on psychological flexibility when psilocybin is combined with a therapeutic intervention specifically designed to increase psychological flexibility. Therefore, using data from a recent clinical trial of psilocybin-assisted therapy that used ACT as a therapeutic frame (for primary clinical outcomes, see11), we examined (1) the effects of psilocybin-assisted therapy on (a) psychological flexibility/experiential acceptance, (b) mindfulness, and (c) values-congruent living, as well as (2) the association between changes in psychological flexibility/experiential acceptance and reductions in depression severity.
Methods
This study was conducted with approvals from the Institutional Review Boards of the VA Connecticut Healthcare System and Yale University, under a US Food and Drug Administration-approved Investigational New Drug application (D’Souza# IND #124,874), under a schedule 1 license from the US Drug Enforcement Agency (DEA) and was registered on clinicaltrials.gov on 13/06/2018 (NCT03554174). The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Study design
The parent study from which the data presented here was derived utilized a placebo-controlled, within-subject, fixed-order design with enhanced blinding procedures. This study was designed primarily to investigate psilocybin’s effects on an electrophysiological biomarker of neuroplasticity (see19), rather than to demonstrate changes in clinical or behavioral outcomes. The within-subject design was selected to increase the statistical power of the study and maximize feasibility, as each participant serves as their own control. Given that psilocybin can produce strong acute subjective and long-lasting antidepressant effects, the study had a fixed-order design of placebo first, followed by psilocybin, in order to limit functional unblinding and minimize potential carryover effects. The two dosing sessions were conducted approximately four weeks apart and were embedded within an eight-session psychotherapy protocol (see Fig. 1 for study design). Participants were assessed for a total of 16 weeks. For a full discussion of blinding procedures, the psychotherapy protocol, and outcomes related to depression, anxiety and quality of life, see11.
Study participants
Inclusion criteria included: (1) 18–65 years old; (2) Meet DSM-5 criteria for Major Depressive Disorder (MDD) by Structured Clinical Interview for DSM-5 (SCID-5-CT)56; (3) current moderate to severe major depressive episode of at least six weeks duration prior to screening, defined by a score ≥ 17 on the GRID-HAM-D-1757,58; (4) failed at least one adequate antidepressant trial (at least 6 weeks on a therapeutic dose) during the current depressive episode. Since medications commonly used in this population (e.g., serotonergic antidepressants) can interfere with the effects of psilocybin59, participants were required to be off any conventional antidepressant or antipsychotic medications for at least 2 weeks prior to study enrollment (or four weeks for fluoxetine). Exclusion criteria included: (1) primary psychiatric diagnosis other than MDD; (2) active substance use disorders; (3) past personal or family history of psychotic or bipolar disorder; (4) significant or unstable medical or neurological disease; (5) psilocybin exposure within the past year. For detailed inclusion/exclusion criteria see11.
Recruitment and screening procedures
Participants were recruited primarily through online postings, including clinicaltrials.gov, clinician referrals and word of mouth. Interested candidates were prescreened by telephone and if eligible, underwent an in-depth screening process. This included a structured psychiatric assessment (SCID-5-CT), psychiatric history and evaluation, and medical screening. Informed consent was obtained from all study participants. Recruitment began in fall of 2018 and concluded in spring 2021.
Interventions
Drugs
All dosing sessions were conducted at the VA Connecticut Healthcare System, West Haven, CT, USA. At the first dosing session, participants received placebo (microcrystalline cellulose) in an opaque capsule, while during the second session they received an identical capsule containing psilocybin (0.3 mg/kg, maximum dose 35 mg). While lower than the 30 mg/70 kg protocol for which safety has been demonstrated, this dose is sufficient for producing psychedelic effects60. Psilocybin was obtained from the University of Wisconsin and the Usona Institute. For detailed descriptions of drug administration sessions and procedures used to enhance blinding and minimize expectancy effects, see11.
Psychotherapeutic support
Participants were assigned a study therapist and psychiatrist for the entire duration of the study. An equivalent number and type of therapy sessions were provided before and after each of the two dosing sessions during the period of primary outcome collection (through week 6): A two-hour long preparatory psychotherapy/psychoeducation session preceded each dosing session, while two one-hour long debriefing/integration psychotherapy sessions were conducted 1 day and 1 week after each dosing session. Following collection of the final primary outcome measures at week 6, participants had two additional integration sessions to help sustain any initial clinical improvements. A delineated therapeutic framework and therapy manual was used to improve consistency in therapeutic approach across participants and between study therapists. This therapy protocol incorporated principles and elements of Acceptance and Commitment Therapy (ACT) (see11 for complete therapy manual). The rationale for including a specific psychotherapy and selecting ACT, the basic structure of the treatment model, and limitations to this approach, are described in detail separately20.
Outcome measures
Psychological flexibility was assessed using the Acceptance and Action Questionnaire-II (AAQ-II)61. Mindfulness was assessed using the Kentucky Inventory of Mindfulness Skills (KIMS)62, which includes the following scales: (a) Observe; (b) Describe; (c) Awareness; and (d) Accept Without Judgment. The degree to which participants are living in accordance with their values (values-congruent living) was measured with the Valued Living Questionnaire (VLQ)63. The AAQ-II, KIMS and VLQ were collected at baseline, week 2 (2 weeks after placebo), week 6 (2 weeks after psilocybin), and week 16 (3 months after psilocybin). Depression symptoms were assessed using the Quick Inventory of Depressive Symptomatology–Self-Report (QIDS-SR-16)64, which was collected throughout the study, from baseline (day before placebo) through week 16. Adverse events were monitored and recorded throughout the trial. Vital signs were monitored throughout each dosing session. For safety data along with other clinical and subjective measures collected, see11.
Statistical analysis
The parent study from which data presented here was derived was powered primarily to investigate an electrophysiological biomarker of neuroplasticity rather than to demonstrate changes in clinical or behavioral outcomes. Data analysis was conducted on participants who completed at least one dosing session (ITT population). Data was analyzed using linear mixed models. Analysis of clinical outcomes through week 16 utilized time as a within-subjects factor. In order to explore the relationship between changes in depressive symptoms (QIDS-SR-16) and both (a) psychological flexibility (AAQ-II) and (b) Accept Without Judgment (KIMS), we conducted Spearman correlations between changes in these variables from before to 2 weeks after each dose. While the parent study also measured depression symptoms using the GRID-HAM-D-17, correlations in this substudy used the QIDS-SR-16 due to more available data points. Given the exploratory nature of the study and small sample size, all statistical tests were conducted using a two-tailed alpha threshold of 0.05, with no adjustments for multiple testing. All tests were performed using SAS, version 9.4 (SAS Institute Inc).
Results
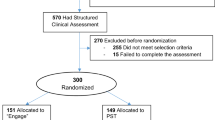
Of 949 individuals assessed for eligibility, 42 (4.4%) were screened in-person, and 22 (2.3%) were ultimately enrolled. 19 participants completed at least one dosing session, of which 15 completed both dosing sessions. Participant demographics and baseline clinical characteristics are presented in Table 1. The primary clinical outcomes related to depression, as well as anxiety and quality of life have been reported separately (see11).
Psychological flexibility
AAQ-II scores decreased over time (i.e., increased psychological flexibility) (F(3,35) = 8.74, p < 0.001) and were significantly lower following psilocybin administration compared to post-placebo (see Fig. 2 and Table 2). The significant reduction in AAQ-II scores was maintained through week 16.
Changes in psychological inflexibility and valued living. (A) Significant reductions in psychological inflexibility 2 weeks post-psilocybin relative to baseline and 2 weeks pre-psilocybin. (B) Significant increases in valued living at 2 weeks and 4 weeks post-psilocybin relative to baseline. Note. Statistical significance relative to baseline = *p < .05, **p < .01, ***p < .001. Statistical significance relative to previous time point = ##p < .01.
Values-congruent living
VLQ scores increased over time (i.e., improvement in values-congruent living) (F(3,36) = 2.99, p = 0.044) and were significantly increased 2 weeks following psilocybin administration compared to baseline but not compared to post-placebo (see Fig. 2 and Table 2). The increases in VLQ scores remained significant through week 16. Scores were not significantly improved following placebo.
Mindfulness
Time analyses were conducted for each of the 4 subscales of the KIMS (see Fig. 3 and Table 2). Significant increases (i.e., improvements) were observed on the Describe (F(3,36) = 2.87, p = 0.05) and Accept Without Judgment subscales (F(3,36) = 3.38, p = 0.029). Describe and Accept Without Judgment were significantly increased 2 weeks following psilocybin administration compared to baseline but not compared to post-placebo. The increased scores remained significant through week 16. Describe and Accept Without Judgment were not significantly improved following placebo. There were no significant changes in the Observe (F(3,36) = 0.72, p = 0.548) or Awareness (F(3,36) = 2.02, p = 0.129) scales.
Changes in mindfulness domains. (A) Significant increases in Acceptance Without Judgment at 2 weeks and 4 weeks post-psilocybin relative to baseline. (B) Significant increases in Awareness at 2 weeks post-psilocybin relative to baseline. (C) No significant changes in Observe. (D) Significant increases in Describe at 2 weeks and 4 weeks post-psilocybin relative to baseline. Note. Statistical significance relative to baseline = *p < .05, **p < .01, ***p < .001. Statistical significance relative to previous time point = ##p < .01.
Relationship between changes in depression symptoms and changes in psychological flexibility and accept without judgment
Depression scores (QIDS-SR-16) decreased from 1 day before (mean = 16.79, SE = 0.95) to 2 weeks after (mean = 11.74, SE = 1.49) placebo (Δ mean = 5.05, p = 0.005). There was not a significant correlation between change in depression scores and change in either (a) psychological inflexibility (Spearman's rho = 0.30, p = 0.295) or (b) Accept Without Judgment (Spearman's rho = -0.42, p = 0.140) during this time period.
Depression scores decreased from 2 weeks before (mean = 11.71, SE = 1.49) to 2 weeks after (mean = 6.27, SE = 1.38) psilocybin (Δ mean = 5.47, p = 0.016). Reductions in depression scores were significantly associated with (a) decreases in psychological inflexibility (Spearman's rho = 0.88, p < 0.001) and (b) increases in Accept Without Judgment (Spearman's rho = -0.64, p = 0.014) during this time period (Fig. 4).
Association between post-psilocybin changes in depression severity and psychological inflexibility/Accept Without Judgment. (A) Significant positive association between reductions in psychological inflexibility and depression severity. (B) Significant negative association between increases in Acceptance Without Judgment inflexibility and reductions in depression severity.
Discussion
This placebo-controlled, within-subject, fixed-order trial among participants with long-standing and predominantly treatment-resistant major depression documented significant and durable improvements in measures of psychological flexibility, mindfulness, and valued living following administration of both placebo and a moderate dose of psilocybin in combination with ACT-based psychotherapy. Improvements in psychological flexibility were significantly greater 2 weeks after psilocybin compared to 2 weeks after placebo and were maintained for 3 months after the psilocybin dosing session. Moreover, following psilocybin administration, improvements in measures of psychological flexibility (AAQ-II) and experiential acceptance (KIMS, Accept Without Judgment scale) were significantly correlated with reductions in depression severity.
The significant improvements in psychological flexibility observed post-psilocybin are in line with the aim of the study design to integrate psilocybin dosing sessions within a psychotherapeutic platform that specifically targets psychological flexibility. These results are consistent with previous naturalistic research indicating that classic psychedelic use is associated with improvements in psychological flexibility21,36,65 and are the first to extend this finding to psilocybin or a clinical trial specifically. Given the significant improvement in psychological flexibility post-psilocybin compared to post-placebo, as well as the finding that values-congruent living and mindfulness domains only significantly improved following psilocybin dosing, our data suggests that the psilocybin dosing session had a significant impact on these psychological domains. In other words, the results suggest that improvements in psychological flexibility are likely not attributable exclusively to the ACT-based psychotherapeutic platform or placebo effects. However, carryover effects from the placebo phase of the study are a potential contributing factor given the within subject study design.
Additionally, significant increases were found over time for values-congruent living and in two domains of mindfulness (Acceptance Without Judgment and Describe). While these increases only became significant following psilocybin dosing, they were not significantly greater post-psilocybin compared to post-placebo. These results may be attributable to several factors, including the ACT-based therapeutic intervention itself being the cause of improvements in these domains, minimal power to detect psilocybin specific effects, and issues with the fixed-order design of the study (e.g. carryover effects, gains occurring in the early phase of treatment66). Of note, no significant overall time effect was observed for the mindfulness domains of Observe and Awareness. These findings are in line with previous research that has found significant improvement in experiential acceptance following psilocybin-assisted therapy5 and mindful non-judgment following the administration of psilocybin but no significant changes in other facets of mindfulness following the administration of psilocybin50.
The significant associations between reductions in depression severity and increases in psychological flexibility and experiential acceptance support the notion that changes in psychological flexibility and related concepts of mindfulness and acceptance may be important psychological mechanisms of change in psilocybin-assisted therapy of depression, and perhaps, other disorders. These findings are especially notable given that the parent clinical trial did not find a significant correlation between the strength of mystical-type experience during psilocybin dosing and reductions in depression11. While it is possible that a small sample size and limited variability in MEQ scores during psilocybin dosing contributed to the latter finding, it is also possible that there may be more essential acute experiences (e.g., psychological insight, emotional breakthrough) and post-acute changes (e.g., increases in psychological flexibility and experiential acceptance) that predict psilocybin treatment outcomes. It is important to note that the correlation between reductions in depression severity and increases in psychological flexibility do not necessarily imply causation and it is possible that improvements in depression also lead to greater psychological flexibility. Nonetheless, these findings are consistent with past survey-based, observational, and clinical research linking post-psychedelic increases in psychological flexibility21,36,37,38,65 and experiential acceptance22,41 with improvements in depression severity and a range of mental health outcomes.
Limitations and future directions
An important limitation of this within-subject study is the inability to fully disambiguate the relative contribution of each therapeutic intervention (placebo dosing, psilocybin dosing, and ACT-based psychotherapy) to the results observed. Because of this, as well as the possibility of carryover effects from the placebo phase, the persisting psychological changes observed following psilocybin dosing cannot be definitively attributed specifically to psilocybin. Moreover, given that we did not compare ACT-based therapy to another therapeutic approach, it is unclear if similar results would have been observed if the therapists had used a non-ACT-based model (e.g. psychological support) to guide preparation and integration. Future studies may attempt to compare the relative efficacy of different therapeutic modalities or the amount of psychotherapeutic support provided.
Furthermore, findings from the present study cannot firmly establish a causal effect of psilocybin therapy on psychological flexibility (for further discussion, see67). Additional research remains necessary to elucidate the potential mechanistic role of psychological flexibility within psilocybin therapy. For instance, intensive longitudinal designs (e.g., the use of ecological momentary assessment) may help to further elucidate the temporal relationship between changes in psychological flexibility and depressive symptoms. Similarly, dose–response studies with variable dosages of psilocybin and amounts of psychotherapy may also help to establish the gradient of the relationship between psychological flexibility and depressive symptoms within psilocybin therapy. Future research examining the effects of psilocybin-assisted therapy on psychological flexibility (and its subdomains) should also include alternative measures of psychological flexibility (e.g., the Multidimensional Psychological Flexibility Inventory68), given significant concerns regarding the validity of the AAQ-II as a measure of psychological flexibility69,70, including its overlap with measures of distress and its single factor measurement of psychological flexibility.
Finally, findings from the present study should be interpreted in light of difficulties with blinding and the likely contribution of expectancy effects (for in depth discussion, see11,71). This issue remains ubiquitous across psychedelic research72 and is likely a problem more broadly within psychiatry (e.g., see73).
Conclusion
In conclusion, this placebo-controlled, within-subject, fixed-order trial of psilocybin-assisted therapy for MDD demonstrated significant improvements in psychological flexibility, several facets of mindfulness (accept without judgment and describe, but not observe and awareness) and values-congruent living. Improvements in psychological flexibility (but not mindfulness or values-congruent living) were greater post-psilocybin compared to post-placebo. Additionally, improvements in psychological flexibility and experiential acceptance were strongly associated with reductions in depression severity. These findings support the theoretical premise of integrating psilocybin dosing sessions with psychotherapeutic platforms that target psychological flexibility and add to the emerging evidence that psychological flexibility may be an important putative mechanism of change in psilocybin-assisted therapy for MDD and potentially, other mental health conditions.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Johnson, M. W., Hendricks, P. S., Barrett, F. S. & Griffiths, R. R. Classic psychedelics: An integrative review of epidemiology, therapeutics, mystical experience, and brain network function. Pharmacol. Ther. 197, 83–102. https://doi.org/10.1016/j.pharmthera.2018.11.010 (2019).
Schimmers, N. et al. Psychedelics for the treatment of depression, anxiety, and existential distress in patients with a terminal illness: a systematic review. Psychopharmacology 239, 15–33. https://doi.org/10.1007/s00213-021-06027-y (2022).
Vollenweider, F. X., Vollenweider-Scherpenhuyzen, M. F., Babler, A., Vogel, H. & Hell, D. Psilocybin induces schizophrenia-like psychosis in humans via a serotonin-2 agonist action. Neuroreport 9, 3897–3902 (1998).
Madsen, M. K. et al. Psychedelic effects of psilocybin correlate with serotonin 2A receptor occupancy and plasma psilocin levels. Neuropsychopharmacology 44, 1328–1334. https://doi.org/10.1038/s41386-019-0324-9 (2019).
Carhart-Harris, R. et al. Trial of psilocybin versus escitalopram for depression. New Engl. J. Med. 384, 1402–1411. https://doi.org/10.1056/nejmoa2032994 (2021).
von Rotz, R. et al. Single-dose psilocybin-assisted therapy in major depressive disorder: A placebo-controlled, double-blind, randomised clinical trial. EClinicalMedicine 56, 101809. https://doi.org/10.1016/j.eclinm.2022.101809 (2023).
Goodwin, G. M. et al. Single-dose psilocybin for a treatment-resistant episode of major depression. N. Engl. J. Med. 387, 1637–1648. https://doi.org/10.1056/NEJMoa2206443 (2022).
Bogenschutz, M. P. et al. Percentage of heavy drinking days following psilocybin-assisted psychotherapy vs placebo in the treatment of adult patients with alcohol use disorder: A randomized clinical trial. JAMA Psychiatry 79, 953–962. https://doi.org/10.1001/jamapsychiatry.2022.2096 (2022).
Davis, A. K. et al. Effects of psilocybin-assisted therapy on major depressive disorder. JAMA Psychiatry 78, 481–489. https://doi.org/10.1001/jamapsychiatry.2020.3285 (2021).
D’Souza, D. C. et al. Exploratory study of the dose-related safety, tolerability, and efficacy of dimethyltryptamine (DMT) in healthy volunteers and major depressive disorder. Neuropsychopharmacology 47, 1854–1862. https://doi.org/10.1038/s41386-022-01344-y (2022).
Sloshower, J. et al. Psilocybin-assisted therapy for major depressive disorder: An exploratory placebo-controlled, fixed-order trial. J. Psychopharmacol. 37, 698–706. https://doi.org/10.1177/02698811231154852 (2023).
Griffiths, R. R. et al. Psilocybin produces substantial and sustained decreases in depression and anxiety in patients with life-threatening cancer: A randomized double-blind trial. J. Psychopharmacol. 30, 1181–1197. https://doi.org/10.1177/0269881116675513 (2016).
Ross, S. et al. Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: A randomized controlled trial. J. Psychopharmacol. 30, 1165–1180. https://doi.org/10.1177/0269881116675512 (2016).
Carhart-Harris, R. L. et al. Psilocybin with psychological support for treatment-resistant depression: an open-label feasibility study. Lancet Psychiatry https://doi.org/10.1016/s2215-0366(16)30065-7 (2016).
Gukasyan, N. et al. Efficacy and safety of psilocybin-assisted treatment for major depressive disorder: Prospective 12-month follow-up. J. Psychopharmacol. 36, 151–158. https://doi.org/10.1177/02698811211073759 (2022).
Agin-Liebes, G. I. et al. Long-term follow-up of psilocybin-assisted psychotherapy for psychiatric and existential distress in patients with life-threatening cancer. J. Psychopharmacol. 34, 155–166. https://doi.org/10.1177/0269881119897615 (2020).
Garcia-Romeu, A., Griffiths, R. R. & Johnson, M. W. Psilocybin-occasioned mystical experiences in the treatment of tobacco addiction. Curr. Drug Abuse Rev. 7, 157–164 (2014).
Bogenschutz, M. P. et al. Psilocybin-assisted treatment for alcohol dependence: A proof-of-concept study. J. Psychopharmacol. 29, 289–299. https://doi.org/10.1177/0269881114565144 (2015).
Skosnik, P. D. et al. Sub-acute effects of psilocybin on EEG correlates of neural plasticity in major depression: Relationship to symptoms. J. Psychopharmacol. 37, 687–697. https://doi.org/10.1177/02698811231179800 (2023).
Sloshower, J. et al. Psilocybin-assisted therapy of major depressive disorder using acceptance and commitment therapy as a therapeutic frame. J. Context. Behav. Sci. 15, 12–19. https://doi.org/10.1016/j.jcbs.2019.11.002 (2020).
Davis, A. K., Barrett, F. S. & Griffiths, R. R. Psychological flexibility mediates the relations between acute psychedelic effects and subjective decreases in depression and anxiety. J. Context. Behav. Sci. 15, 39–45. https://doi.org/10.1016/j.jcbs.2019.11.004 (2020).
Zeifman, R. J. et al. Post-psychedelic reductions in experiential avoidance are associated with decreases in depression severity and suicidal ideation. Front. Psychiatry 11, 782. https://doi.org/10.3389/fpsyt.2020.00782 (2020).
Carhart-Harris, R. L., Erritzoe, D., Haijen, E., Kaelen, M. & Watts, R. Psychedelics and connectedness. Psychopharmacology 235, 547–550. https://doi.org/10.1007/s00213-017-4701-y (2018).
Watts, R. et al. The watts connectedness scale: A new scale for measuring a sense of connectedness to self, others, and world. Psychopharmacology 239, 3461–3483. https://doi.org/10.1007/s00213-022-06187-5 (2022).
Carhart-Harris, R. L. & Friston, K. J. REBUS and the Anarchic Brain: Toward a unified model of the brain action of psychedelics. Pharmacol. Rev. 71, 316–344. https://doi.org/10.1124/pr.118.017160 (2019).
Zeifman, R. J. et al. From relaxed beliefs under psychedelics (rebus) to revised beliefs after psychedelics (rebas): Preliminary development of the relaxed beliefs questionnaire (reb-q). (2022).
Roseman, L. et al. Emotional breakthrough and psychedelics: Validation of the Emotional Breakthrough Inventory. J. Psychopharmacol. 33, 1076–1087. https://doi.org/10.1177/0269881119855974 (2019).
Hayes, S. C., Pistorello, J. & Levin, M. E. Acceptance and commitment therapy as a unified model of behavior change. Counsel. Psychol. 40, 976–1002 (2012).
Francis, A. W., Dawson, D. L. & Golijani-Moghaddam, N. The development and validation of the Comprehensive assessment of Acceptance and Commitment Therapy processes (CompACT). J. Context. Behav. Sci. 5, 134–145 (2016).
Stange, J. P., Alloy, L. B. & Fresco, D. M. Inflexibility as a vulnerability to depression: A systematic qualitative review. Clin. Psychol. Sci. Pract. 24, 245 (2017).
Akbari, M., Seydavi, M., Hosseini, Z. S., Krafft, J. & Levin, M. E. Experiential avoidance in depression, anxiety, obsessive-compulsive related, and posttraumatic stress disorders: A comprehensive systematic review and meta-analysis. J. Context. Behav. Sci. 24, 65–78 (2022).
Forman, E. M., Herbert, J. D., Moitra, E., Yeomans, P. D. & Geller, P. A. A randomized controlled effectiveness trial of acceptance and commitment therapy and cognitive therapy for anxiety and depression. Behav. Modif. 31, 772–799. https://doi.org/10.1177/0145445507302202 (2007).
Ostergaard, T., Lundgren, T., Zettle, R. D., Landro, N. I. & Haaland, V. O. Psychological flexibility in depression relapse prevention: Processes of change and positive mental health in group-based act for residual symptoms. Front. Psychol. 11, 528. https://doi.org/10.3389/fpsyg.2020.00528 (2020).
Stockton, D. et al. Identifying the underlying mechanisms of change during acceptance and commitment therapy (ACT): A systematic review of contemporary mediation studies. Behav. Cogn. Psychother 47, 332–362. https://doi.org/10.1017/S1352465818000553 (2019).
Walser, R. D. et al. Effectiveness of acceptance and commitment therapy in treating depression and suicidal ideation in Veterans. Behav. Res. Ther. 74, 25–31. https://doi.org/10.1016/j.brat.2015.08.012 (2015).
Close, J. B., Hajien, E. C., Watts, R., Roseman, L. & Carhart-Harris, R. L. Psychedelics and psychological flexibility–Results of a prospective web-survey using the Acceptance and Action Questionnaire II. J. Context. Behav. Sci. 16, 37–44 (2020).
Agin-Liebes, G. et al. Prospective examination of the therapeutic role of psychological flexibility and cognitive reappraisal in the ceremonial use of ayahuasca. J. Psychopharmacol. 36, 295–308. https://doi.org/10.1177/02698811221080165 (2022).
González, D. et al. Therapeutic potential of ayahuasca in grief: A prospective, observational study. Psychopharmacology 41, 205–212. https://doi.org/10.1007/s00213-019-05446-2 (2020).
Cardaciotto, L., Herbert, J. D., Forman, E. M., Moitra, E. & Farrow, V. The assessment of present-moment awareness and acceptance: The Philadelphia Mindfulness Scale. Assessment 15, 204–223. https://doi.org/10.1177/1073191107311467 (2008).
Fletcher, L. & Hayes, S. C. Relational frame theory, acceptance and commitment therapy, and a functional analytic definition of mindfulness. J. Rational-Emot. Cognit. Behav. Therapy 23, 315–336 (2005).
Zeifman, R. J., Wagner, A. C., Monson, C. M. & Carhart-Harris, R. L. How does psilocybin therapy work? An exploration of experiential avoidance as a putative mechanism of change. J. Affect. Disord. 334, 100–112. https://doi.org/10.1016/j.jad.2023.04.105 (2023).
Dominguez-Clave, E. et al. Ayahuasca improves emotion dysregulation in a community sample and in individuals with borderline-like traits. Psychopharmacology 236, 573–580. https://doi.org/10.1007/s00213-018-5085-3 (2019).
Murphy-Beiner, A. & Soar, K. Ayahuasca’s “afterglow”: Improved mindfulness and cognitive flexibility in ayahuasca drinkers. Psychopharmacology 237, 1161–1169. https://doi.org/10.1007/s00213-019-05445-3 (2020).
Sampedro, F. et al. Assessing the psychedelic “after-glow” in Ayahuasca users: Post-acute neurometabolic and functional connectivity changes are associated with enhanced mindfulness capacities. Int. J. Neuropsychopharmacol. 20, 698–711. https://doi.org/10.1093/ijnp/pyx036 (2017).
Soler, J. et al. Exploring the therapeutic potential of Ayahuasca: Acute intake increases mindfulness-related capacities. Psychopharmacology 233, 823–829. https://doi.org/10.1007/s00213-015-4162-0 (2016).
Soler, J. et al. Four weekly ayahuasca sessions lead to increases in “acceptance” capacities: A comparison study with a standard 8-week mindfulness training program. Front. Pharmacol. 9, 224. https://doi.org/10.3389/fphar.2018.00224 (2018).
Uthaug, M. V. et al. Prospective examination of synthetic 5-methoxy-N, N-dimethyltryptamine inhalation: effects on salivary IL-6, cortisol levels, affect, and non-judgment. Psychopharmacology 237, 773–785. https://doi.org/10.1007/s00213-019-05414-w (2020).
Uthaug, M. V. et al. A single inhalation of vapor from dried toad secretion containing 5-methoxy-N, N-dimethyltryptamine (5-MeO-DMT) in a naturalistic setting is related to sustained enhancement of satisfaction with life, mindfulness-related capacities, and a decrement of psychopathological symptoms. Psychopharmacology 236, 2653–2666. https://doi.org/10.1007/s00213-019-05236-w (2019).
Uthaug, M. V. et al. Sub-acute and long-term effects of ayahuasca on affect and cognitive thinking style and their association with ego dissolution. Psychopharmacology 235, 2979–2989. https://doi.org/10.1007/s00213-018-4988-3 (2018).
Kiraga, M. K., Kuypers, K. P., Uthaug, M. V., Ramaekers, J. G. & Mason, N. L. Decreases in state and trait anxiety post-psilocybin: A naturalistic, observational study among retreat attendees. Front. Psychiatry 13, 883869 (2022).
Madsen, M. K. et al. A single psilocybin dose is associated with long-term increased mindfulness, preceded by a proportional change in neocortical 5-HT2A receptor binding. Eur. Neuropsychopharmacol. 33, 71–80 (2020).
Smigielski, L. et al. Characterization and prediction of acute and sustained response to psychedelic psilocybin in a mindfulness group retreat. Sci. Rep. 9, 14914. https://doi.org/10.1038/s41598-019-50612-3 (2019).
Radakovic, C., Radakovic, R., Peryer, G. & Geere, J.-A. Psychedelics and mindfulness: A systematic review and meta-analysis. J. Psychedelic Stud. 6, 137–153 (2022).
Johnson, M. W., Garcia-Romeu, A., Johnson, P. S. & Griffiths, R. R. An online survey of tobacco smoking cessation associated with naturalistic psychedelic use. J. Psychopharmacol. 131, 026988111668433–026988111668410. https://doi.org/10.1177/0269881116684335 (2017).
Griffiths, R. R. et al. Psilocybin-occasioned mystical-type experience in combination with meditation and other spiritual practices produces enduring positive changes in psychological functioning and in trait measures of prosocial attitudes and behaviors. J. Psychopharmacol. 32, 49–69. https://doi.org/10.1177/0269881117731279 (2018).
First, M., Williams, J., Karg, R. & Spitzer, R. Structured Clinical Interview for DSM-5 Disorders, Clinical Trials Version (SCID-5-CT). (American Psychiatric Association, 2015).
Hamilton, M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 23, 56–62. https://doi.org/10.1136/jnnp.23.1.56 (1960).
International Society for CNS Drug Development. GRID-HAMD-17 Structured Interview Guide. (ISCDD, 2003).
Malcolm, B. & Thomas, K. Serotonin toxicity of serotonergic psychedelics. Psychopharmacology https://doi.org/10.1007/s00213-021-05876-x (2021).
Griffiths, R. R., Richards, W. A., McCann, U. & Jesse, R. Psilocybin can occasion mystical-type experiences having substantial and sustained personal meaning and spiritual significance. Psychopharmacology 187, 268–283 (2006).
Bond, F. W. et al. Preliminary psychometric properties of the acceptance and action questionnaire–II: A revised measure of psychological inflexibility and experiential avoidance. Behav. Therapy 42, 676–688 (2011).
Baer, R. A., Smith, G. T. & Allen, K. B. Assessment of mindfulness by self-report: The Kentucky Inventory of Mindfulness Skills. Assessment 11, 191–206 (2004).
Wilson, K. G., Sandoz, E. K., Kitchens, J. & Roberts, M. The Valued Living Questionnaire: Defining and measuring valued action within a behavioral framework. Psychol. Record 60, 249 (2010).
Rush, A. J. et al. The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): A psychometric evaluation in patients with chronic major depression. Biol. Psychiatry 54, 573–583 (2003).
Davis, A. K., Xin, Y., Sepeda, N. D., Garcia-Romeu, A. & Williams, M. T. Increases in psychological flexibility mediate relationship between acute psychedelic effects and decreases in racial trauma symptoms among people of color. Chronic Stress 5, 24705470211035610 (2021).
Shalom, J. G. & Aderka, I. M. A meta-analysis of sudden gains in psychotherapy: Outcome and moderators. Clin. Psychol. Rev. 76, 101827. https://doi.org/10.1016/j.cpr.2020.101827 (2020).
Kangaslampi, S. Uncovering psychological mechanisms mediating the effects of drugs: Some issues and comments using the example of psychedelic drugs. Psychopharmacology 237, 3799–3802. https://doi.org/10.1007/s00213-020-05703-9 (2020).
Rolffs, J. L., Rogge, R. D. & Wilson, K. G. Disentangling components of flexibility via the Hexaflex model: Development and validation of the multidimensional psychological flexibility inventory (MPFI). Assessment 25, 458–482. https://doi.org/10.1177/1073191116645905 (2018).
Tyndall, I. et al. The acceptance and action questionnaire-II (AAQ-II) as a measure of experiential avoidance: Concerns over discriminant validity. J. Context. Behav. Sci. 12, 278–284 (2019).
Doorley, J. D., Goodman, F. R., Kelso, K. C. & Kashdan, T. B. Psychological flexibility: What we know, what we do not know, and what we think we know. Social Personal. Psychol. Compass 14, 1–11 (2020).
Muthukumaraswamy, S., Forsyth, A. & Lumley, T. Blinding and expectancy confounds in psychedelic randomised controlled trials. Expert Rev. Clin. Phar. https://doi.org/10.1080/17512433.2021.1933434 (2021).
Wen, A. et al. A systematic review of study design and placebo controls in psychedelic research. Psychedel. Med. https://doi.org/10.1089/psymed.2023.0028 (2023).
Scott, A. J., Sharpe, L. & Colagiuri, B. A systematic review and meta-analysis of the success of blinding in antidepressant RCTs. Psychiatry Res. 307, 114297. https://doi.org/10.1016/j.psychres.2021.114297 (2022).
Acknowledgements
We are grateful to: the Heffter Research Institute who advised on study design and funded the study with the aid of Carey and Claudia Turnbull; Nicholas Cozzi and the Usona Institute for providing psilocybin; Angelina Genovese, Elizabeth O’Donnell, Margaret Dion-Marovitz (Research Nurses) of the Neurobiological Studies Unit, VA Connecticut Healthcare System; the Research Pharmacy, VA Connecticut Healthcare System; Christina Luddy and all research assistants who contributed effort to the study; Ryan Wallace for assistance writing the study protocol; and Anne Dutton, Stephanie Kilpatrick, Robert Krause, John Cline, and Gabrielle Agin-Liebes for serving as study therapists.
Funding
This work was supported by the Heffter Research Institute.
Author information
Authors and Affiliations
Contributions
J.S. and D.C.D. oversaw the overall design and conduct of the study. J.S. and R.J.Z. wrote the main manuscript text and prepared the figures and tables. R.K. and J.G. assisted with study design and development of the psychotherapy protocol. S.P. and H.S.A. were responsible for data collection. B.P. and R.J.Z. analyzed the study data. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
DCD receives research funding administered through Yale University from the US National Institute of Health, US Dept. of Veteran Affairs, Takeda, Biogen, Boehringer Ingelheim, Ceruvia, Heffter Institute and Wallace Foundation. DCD has served as a paid consultant to Jazz Pharmaceuticals, Biohaven and Abide. JS serves has served as a paid consultant to the Usona Institute and Cybin. RJZ is a postdoctoral fellow in the NYU Langone Psychedelic Medicine Research Training program funded by MindMed. No other potential conflicts of interest relevant to this article were reported.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sloshower, J., Zeifman, R.J., Guss, J. et al. Psychological flexibility as a mechanism of change in psilocybin-assisted therapy for major depression: results from an exploratory placebo-controlled trial. Sci Rep 14, 8833 (2024). https://doi.org/10.1038/s41598-024-58318-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-58318-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.