Abstract
Lung cancer, specifically the histological subtype lung adenocarcinoma (LUAD), has the highest global occurrence and fatality rate. Extensive research has indicated that RNA alterations encompassing m6A, m5C, and m1A contribute actively to tumorigenesis, drug resistance, and immunotherapy responses in LUAD. Nevertheless, the absence of a dependable predictive model based on m6A/m5C/m1A-associated genes hinders accurately predicting the prognosis of patients diagnosed with LUAD. In this study, we collected patient data from The Cancer Genome Atlas (TCGA) and identified genes related to m6A/m5C/m1A modifications using the GeneCards database. The “ConsensusClusterPlus” R package was used to produce molecular subtypes by utilizing genes relevant to m6A/m5C/m1A identified through differential expression and univariate Cox analyses. An independent prognostic factor was identified by constructing a prognostic signature comprising six genes (SNHG12, PABPC1, IGF2BP1, FOXM1, CBFA2T3, and CASC8). Poor overall survival and elevated expression of human leukocyte antigens and immune checkpoints were correlated with higher risk scores. We examined the associations between the sets of genes regulated by m6A/m5C/m1A and the risk model, as well as the immune cell infiltration, using algorithms such as ESTIMATE, CIBERSORT, TIMER, ssGSEA, and exclusion (TIDE). Moreover, we compared tumor stemness indices (TSIs) by considering the molecular subtypes related to m6A/m5C/m1A and risk signatures. Analyses were performed based on the risk signature, including stratification, somatic mutation analysis, nomogram construction, chemotherapeutic response prediction, and small-molecule drug prediction. In summary, we developed a prognostic signature consisting of six genes that have the potential for prognostication in patients with LUAD and the design of personalized treatments that could provide new versions of personalized management for these patients.
Similar content being viewed by others
Introduction
Lung cancer is a fatal malignancy and the leading cause of cancer-related deaths, with an estimated 1.8 million deaths worldwide (almost 18% of all cancers) in 20201,2. Non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC) are the two major histological types of lung cancer3. Lung adenocarcinoma (LUAD), accounting for 40% of all lung cancer cases, is the most prevalent NSCLC subtype4,5. Despite substantial progress in treatments, including targeted therapy, surgical treatment, and early cancer detection, the 5-year survival rate of patients with LUAD is approximately 15–20%, and the treatment effectiveness is poor6,7. Therefore, exploring new potential biomarkers to predict the clinical prognosis and guide individualized treatment is urgently needed.
RNA methylation, the most stable form of epigenetic modification in RNA posttranscriptional regulation, has been linked to several human diseases8. The three major forms of DNA methylation are N6-methyladenosine (m6A), 5-methylcytosine (m5C), and N1-methyladenosine (m1A). Recent studies have found that m6A, m5C, and m1A are involved in tumor regulation by regulating gene expression levels9,10,11,12. For example, m6A-regulated gene methyltransferase 3 (METTL3) recruits YTHDF1/3 and eIF3b to form a translation initiation complex. This complex plays a crucial role in promoting YAP translation, which in turn contributes to the invasion, metastasis, and chemoresistance of lung cancer cells by mediating miR-1914-3p13. m5C methyltransferase NSUN4 is abnormally expressed in LUAD and clear cell renal cell carcinoma and may be utilized to predict prognosis14,15. NSUN5 is significantly upregulated in head and neck squamous cell carcinoma (HNSCC) and promotes colorectal cancer (CRC) by inducing cell cycle arrest16. m1A is found in mitochondrial transcripts, mRNA, rRNA, and tRNA17. m1A demethylase ALKBH3, also known as prostate carcinoma antigen-1 (PCA-1), is not only highly expressed in various human cancers18 but also functions as a tRNA demethylase that promotes protein synthesis in cancer cells19. Presently, no reliable model based on the m6A, m5C, or m1A genes to predict the prognosis of patients with LUAD exists.
In this study, we developed a prognostic signature based on differentially expressed m6A, m5C, and m1A regulatory genes obtained from The Cancer Genome Atlas (TCGA). We also validated the performance of the signature from the Gene Expression Omnibus (GEO) database; survival stratification, somatic mutations, nomogram construction, chemotherapy response prediction, and small-molecule drug prediction based on risk characteristics were analyzed, thereby providing a reliable prognostic signature.
Results
Identification of differentially expressed m6A/m5C/m1A-related gene (DE-MRGs) and biological function analysis
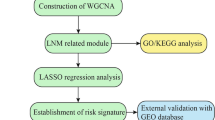
Using the GeneCards database and previous research and literature, 64 genes were obtained using relevance scores ≥ 3 as the screening threshold, and 45 genes associated with LUAD were identified, respectively. The study flow is shown in Supplementary Figure S1. Using differential analysis, 48 upregulated genes and 21 downregulated genes in LUAD and normal colon tissues were screened (Fig. 1A, B). Gene ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway enrichment analyses revealed that these genes were significantly enriched in the cancer, hemopoiesis, transcription regulator complex, and transcription factor binding pathways (Fig. 1C, D). In addition, correlations between the top ten upregulated and top ten downregulated genes are shown Fig. 1E. The protein–protein interaction (PPI) network was established based on the above differentially expressed genes using the Search Tool for the Retrieval of Interacting Genes (STRING) online database, as shown in Fig. 1F. The node degree represented the degree of connectivity between differentially expressed genes. The Maximal Clique Centrality (MCC) algorithm in the CytoHubba plugin was used to calculate the top ten hub genes in terms of node degree: SPI1, TAL1, GFI1B, GATA1, GATA2, LDB2, CD34, CBFA2T3, SOX2, and JUN (Fig. 1G). Module genes of the PPI analysis were identified using Molecular Complex Detection (MCODE), and the two most significant modules were selected (Fig. 1H, I).
(A) Volcano plot of 69 DE-MRGs in LUAD. Red dots represent upregulated genes, and blue dots represent downregulated genes. (B) Heatmap of 69 DE-MRGs between normal lung and LUAD tissues. (C) The top ten enriched terms in GO analysis for DE-MRGs. (D) The top ten enriched terms in KEGG analysis. (E) The correlations between the top 10 up-regulated and top 10 down-regulated DE-MRGs. (F) PPI network of the DE-MRGs according to the STRING database. (G) The top ten hub genes are identified in the PPI network using the “CytoHubba” plugin in Cytoscape. The darker the color, the darker the node degree value. (H, I) The two most significant modules are identified from the PPI network using the “MCODE” plugin in Cytoscape. (H, I) The hub genes are obtained from the “CytoHubba” plugin in Cytoscape. LUAD, lung adenocarcinoma; DE-MRGs, differentially expressed m6A/m5C/m1A-related genes; GO, gene ontology; BP, biological process; CC, cell component; MF, molecular function; KEGG, Kyoto Encyclopedia of Genes and Genomes; PPI, protein–protein interaction.
Identifying m6A/m5C/m1A-associated clusters and correlation analysis between clusters and the tumor immune microenvironment and tumorigenesis scores
Using univariate Cox analysis, we identified nine genes that were associated with prognosis, of which TNS1, SNHG12, and CBFA2T3 were protective factors, and the other six genes were risk factors (Fig. 2A, Supplementary Figure S2). The correlation analysis indicated that most genes were correlated with each other (Fig. 2B). Nine prognosis-related genes were used for the cluster analysis. The cluster analysis yielded optimal results when patients with LUAD were divided into two subgroups, and the internal consistency and stability of the subgroups were good (Fig. 2C, E). Survival analysis showed that cluster 1 patients had a better prognosis than cluster 2 patients (Fig. 2F).
(A) Forest plot showing nine prognosis-related DE-MRGs selected by univariate Cox regression analysis. (B) Correlations between the nine genes. (C) Consensus clustering matrix, when k = 2. (D) Consensus clustering CDF with k-values of 2–9. (E) Relative change in the area under the CDF curve for k = 2. (F) KM curve showing the overall survival in patients between clusters 1 and 2. Immune cell infiltration using CIBERSORT (G), the expression of MHC molecules (H), immune and stromal scores using ESTIMATE (I), angiogenic activity, mesenchymal-EMT, tumorigenic cytokines and stemness scores (J), five common immunoinhibitors (K), and TIDE scores (L) between the two clusters. CDF, cumulative distribution function; KM, Kaplan–Meier; EMT, epithelial-mesenchymal-transition; TIDE, Tumor Immune Dysfunction, and Exclusion. *p < 0.05; **p < 0.01.
Subsequently, the CIBERSORT algorithm was used to analyze the differences in immune infiltration between the two clusters. We found differences in the immune cells between the two clusters (Fig. 2G). The ESITIMATE algorithm showed that cluster 1 had a higher immune score, stromal score, and ESITIMATE score and a lower tumor purity (Fig. 2H). We also found that cluster 1 was related to the higher expression of many MHC molecules (Fig. 2I).
In addition, we examined the angiogenic activity, mesenchymal epithelial-to-mesenchymal transition (EMT), tumorigenic cytokines, and stemness scores between the two groups and found that tumorigenic cytokine scores were significantly higher in cluster 1 (Fig. 2J). We also evaluated their correlation with five common immune checkpoints (PD-L1, CD86, HAVCR2, CTLA4, and LAG3). Cluster 1 showed a higher expression of all immune checkpoints (Fig. 2K) and was associated with higher TIDE scores (Fig. 2L).
Construction of a m6A/m5C/m1A-related signature and nomogram based on the signature
To further screen the genes included in the model, we performed a multifactor Cox regression analysis and identified six genes for inclusion in the signature (Fig. 3A). The coefficients for each gene in the signature are shown in Fig. 3B. Figure 3C shows the correlation between the risk score and SNHG12, PABPC1, IGF2BP1, FOXM1, CBFA2T3, and CASC8. Risk scores were calculated as follows:
(A) Forest plot showing six genes selected in the signature through multivariate Cox analysis. (B) Coefficients of the four genes included in the signature. (C) Correlations between the signature and the six genes. KM survival analysis, heatmap, survival status accompanied with the risk score, and ROC analysis in the TCGA cohort (D) and GSE37745 cohort (E). Univariate (F) and multivariate Cox analyses (G) show that signature is an independent risk factor for patients with LUAD in the TCGA cohort. Risk score differences between groups according to clinicopathological features, including the grade (H), stage (I), T stage (J), and N stage (K). (L) Nomogram combining clinicopathological variables and risk scores to predict overall survival at 1, 3, and 5 years of patients with LUAD. (M) The calibration curves of the nomogram for predicting the probability of 1-, 3-, and 5-year survival. ROC, receiver operating characteristic; TCGA, The Cancer Genome Atlas; M, metastasis.
Patients with high-risk scores had a poorer prognosis than those with low-risk scores, and the area under the curve (AUC) of the signature was 0.733 at one year (Fig. 3D). The GEO dataset was used to validate the efficiency of the signature, which showed good efficiency (Fig. 3E). Stratified analysis revealed that this signature could effectively differentiate the patient prognosis across various clinical subgroups. Specifically, patients classified in the high-risk group exhibited a notably poorer prognosis (Supplementary Figure S3). In addition, univariate and multivariate Cox regression analyses indicated that the risk signature was an independent risk factor for LUAD (Fig. 3F, G). We also analyzed the differences in risk scores between subgroups based on different clinicopathological parameters. The results indicated that patients with grade III–IV, stage III–IV, T3–4, and N3 disease had higher risk scores. This implied that the tumors became more advanced as the risk score increased (Figs. 3H–K).
To enhance the ability to predict the prognosis of patients with LUAD, we constructed a nomogram incorporating clinicopathological variables and risk scores to predict the prognosis of patients with ccRCC at 1, 3, and 5 years (Fig. 3L). The calibration curve showed excellent agreement between the actual overall survival (OS) and the predicted survival at 1, 3, and 5 years (Fig. 3M).
Estimation of tumor immune cell infiltration and immune checkpoint inhibitors according to the signature
Considering the varying prognoses of patients in the high- and low-risk groups, we performed gene set enrichment analysis (GSEA). The intestinal immune network for immunoglobulin A production and pathways for primary immunodeficiency were significantly enriched in the high-risk group (Table S1), suggesting that a high risk is closely associated with an immune response. Therefore, we further investigated the relationship between this signature and the tumor immune microenvironment. The single-sample Gene Set Enrichment Analysis (ssGSEA) algorithm revealed that the high-risk group exhibited a greater degree of immune cell infiltration and a higher number of immune-related functions or pathways than the low-risk group (Fig. 4A, B). Using the ESTIMATE algorithm, patients in the high-risk group had higher immune, stromal, and estimation scores and lower tumor purity (Fig. 4C). Immune cells that predominantly infiltrated the high-risk group included memory CD4 + T cells, regulatory T cells, monocytes, and resting dendritic cells (Fig. 4D). Memory B cells, CD8 + T cells, and resting mast cells were also higher in the high-risk group (Fig. 4E). Additionally, we detected the expression of MHC molecules and found that the low-risk group exhibited significantly lower expression levels (Fig. 4F). We also evaluated their correlation with five common immune checkpoints (PD-L1, CD86, HAVCR2, CTLA4, and LAG3). In the high-risk group, immune checkpoints PD-L1, CTLA4, and LAG3 showed higher expression (Fig. 4G).
(A) Infiltration levels of 16 immune cells in the high- and low-risk groups using the ssGSEA algorithm. (B) Correlation of predictive signature with 13 immune-related functions or pathways. Immune and stromal scores (C), immune cell infiltration using TIMER (D) and CIBERSORT (E), MHC molecule expression levels (F), and five common immunoinhibitors (G) between the high- and low-risk groups. (*p < 0.05; **p < 0.01; ***p < 0.001; ns, not significant).
Correlation of angiogenic activity, mesenchymal EMT, tumorigenic cytokines, stemness scores and TSIs with the signature
Previous studies identified clusters linked to angiogenic activity, mesenchymal EMT, tumorigenic cytokines, and stemness scores. Therefore, our objective was to investigate whether these four tumor-associated functions play a role in the underlying mechanisms of the signature. We calculated the angiogenic activity, mesenchymal EMT, tumorigenic cytokines, and stemness scores in patients with LUAD. The high-risk group showed higher angiogenic activity and mesenchymal EMT (Fig. 5A). Correlation analysis revealed that the risk score was significantly and positively associated with angiogenic activity (R = 0.44, p = 2.2e-16) (Fig. 5B). In addition, the low-risk group exhibited lower levels of TSIs, including mRNAsi, EREG-mRNAsi, mDNAsi, EREG-mDNAsi, and ENHsi (Fig. 5C).
(A) Differences in angiogenic activity, mesenchymal EMT, tumorigenic cytokines, and stemness scores between the high- and low-risk groups. (B) Correlation of the risk score and the angiogenic activity, mesenchymal EMT, tumorigenic cytokines, and stemness scores. (C) Differences in TSIs between the two groups. TSIs, tumor stemness indices. (*p < 0.05; **p < 0.01; ***p < 0.001; ns, not significant).
Comparison of somatic mutation and tumor mutation burden (TMB) in the signature
To investigate genomic mutations between the high- and low-risk groups, we obtained simple nucleotide variation data from the TCGA. In the high-risk group, the five genes with the highest mutation frequencies were TTN (56%), TP53 (49%), MUC16 (45%), CSMD3 (44%), and RYR2 (41%). In the low-risk group, the five genes with the lowest mutation frequencies were TP53 (42%), TTN (33%), MUC16 (34%), CSMD3 (31%), and RYR2 (31%) (Fig. 6A, B). In addition, we identified somatic mutation interactions and observed gene mutation co-occurrence among most genes. Notably, the high-risk group showed mutually exclusive TP53-KRAS mutations (Fig. 6C). Although gene mutation co-occurrence was common in low-risk groups, mutually exclusive mutations existed among a significant number of genes (Fig. 6D). Further correlation analysis suggested that the TMB of patients with LUAD in the high-risk group was significantly higher than that of patients in the low-risk group (Fig. 6E). There was no difference in survival between the patients with high and low TMB (Fig. 6F). By combining the TMB with the risk model, we found that patients in the low-risk and high-TMB group had the best prognosis, whereas those in the high-risk and low-TMB group had the worst (Fig. 6G). Finally, we detected the mutation rates of six genes in the signature and found that they were low (Fig. 6H).
Waterfall plot of somatic mutation features in the high-risk group (A) and low-risk group (B). Heatmap of co-occurrence and mutually exclusive mutations of the differently mutated genes in the high-risk group (C) and the low-risk group (D). (E) Comparison of the difference in TMB between high- and low-risk groups. (F) The difference in overall survival between high- and low-TMB groups. (G) The difference in overall survival is based on the TMB and risk score. (H) Mutation rates of six genes (SNHG12, PABPC1, IGF2BP1, FOXM1, CBFA2T3, and CASC8) in patients with LUAD from the cBioPortal database.
Small-molecule drug screening
To further explore individualized treatment regimens, we calculated the half-maximal inhibitory concentration (IC50) of 95 chemotherapy drugs in the high- and low-risk groups based on LUAD data from the TCGA. BIBW2992, bicalutamide, doxorubicin, embelin, gemcitabine, midostaurin, parthenolide, pazopanib, rapamycin, salubrinal, sunitinib, and tipifarnib were candidate drugs for treating high-risk patients (Fig. 7A). We identified 15 upregulated and 51 downregulated genes by comparing the low- and high-risk groups, respectively (Fig. 7B). Subsequently, we used the cMap database to screen for small-molecule drugs. The eight most relevant drugs were screened as prospective candidates for treating patients with LUAD based on the differentially expressed genes. The 3D structures of albendazole, androstenedione, evodiamine, fenbendazole, fenoterol, prostaglandin PKCβ-inhibitor, and vinburnine are shown in the PubChem database (Fig. 7C).
Discussion
According to recent studies, LUAD has emerged as the predominant form of NSCLC, surpassing lung squamous cell carcinoma20. The 5-year survival rate for this type of cancer is only 15%21. In recent years, an increasing number of studies have focused on the effects of RNA methylation on the occurrence, development, and prognosis of LUAD.
In the present study, we identified 109 DE-MRGs between tumor and normal tissues based on LUAD data from the TCGA. We conducted a systematic analysis of relevant biological pathways and constructed co-expression and PPI networks. Moreover, we performed several statistical analyses to determine the predictive capabilities of a signature comprising the six DE-MRGs in patients with LUAD. These analyses included univariate Cox regression, survival, multiple stepwise Cox regression, and receiver operating characteristic (ROC) analyses. Our results showed that a signature consisting of SNHG12, PABPC1, IGF2BP1, FOXM1, CBFA2T3, and CASC8 could accurately predict clinical outcomes and treatment responses in patients with LUAD.
SNHG12 is a small nucleolar RNA host gene (SNHG) implicated in cancer progression22. Ruan et al. demonstrated that SNHG12 plays a role in cell proliferation and migration23. Previous studies have reported SNHG12 overexpression in CRC and breast cancer24,25. IGF2BP1, a member of the IGF2BP family, is an m6A-binding protein that recognizes GG(m6A)C sequences within targeted mRNA, thereby participating in the transcription, stability, splicing, and translation of various RNA molecules26. Previous studies demonstrated that IGF2BP1 interacts with LIN28B-AS1 to enhance the stability and translation of mRNA in a manner influenced by m6A modification, which ultimately leads to increased proliferation and invasion of cancer cells27,28,29. Previous studies have shown that FOXM1 is important for regulating various processes involved in lung cancer tumorigenesis, including cell cycle progression, cancer therapy resistance, and metastasis30,31,32. For example, FOXM1 plays a role in regulating the radiosensitivity of lung cancer cells, partially through the upregulation of KIF20A33, and FOXM1 activation leads to the progression of lung adenomas into invasive mucinous adenocarcinomas by activating AGR234. CBFA2T3, a chromatin repressor localized in the nucleolus, functions as a suppressor of breast tumorigenesis35. CBFA2T3 is also a tumor suppressor in lung cancer and can serve as an independent prognostic marker for LUAD36. Given the positive correlation between CBFA2T3 expression and higher antigen-presenting cell infiltration, CBFA2T3 holds promise as a potential tumor antigen for future mRNA vaccines37. Studies have shown that cancer susceptibility candidate 8 (CASC8) is a tumor susceptibility gene38,39. Interestingly, CASC8 regulates EMT genes via FOXM1. Moreover, CASC8 suppression substantially decreases the proliferation, migration, and invasion of NSCLC cells38.
Further analyses showed the high predictive accuracy and robustness of the m6A/m5C/m1A-related gene signature in this study. Moreover, the patients in the high-risk group had poorer outcomes in the training and validation cohorts. The 3-year survival AUC was 0.733 in the TCGA cohort and 0.631 in the GSE37745 cohort. Univariate and multivariate Cox regression analyses identified the risk score as an independent prognostic factor. Subsequently, we developed a quantitative and objective nomogram based on multivariate analysis. Therefore, our nomogram is suitable for clinical practice.
The tumor microenvironment has garnered considerable attention because of its substantial influence on cancer progression, including tumor growth, invasion, and metastasis40,41. In this study, the m6A/m5C/m1A-related signature was significantly associated with immune cell infiltration. For example, the high-risk group was infiltrated by a higher proportion of memory B cells, CD8 + T cells, resting memory CD4 + T cells, regulatory T cells, monocytes, resting dendritic cells, and resting mast cells. CD8 + T cells are essential for establishing antitumor immunity within the tumor microenvironment of LUAD. These cells play a significant role in antitumor immunity, and CD4 + T cells contribute to this antitumor effect by secreting various cytokines and assisting in activating CD8 + T and other immune cells.
Immune checkpoints are molecules expressed by immune cells sensitive to the regulation of immune activation42. We investigated the expression of five immune checkpoint genes in the two risk subtypes in this study. These findings revealed increased expression of the three immune checkpoint genes in high-risk patients. This suggests that patients in the high-risk group may benefit from immunotherapies that inhibit immune checkpoints.
Resistance to chemotherapy is a significant challenge encountered during LUAD treatment that contributes to the high mortality rate associated with cancer. Identifying a chemosensitive population may enhance the antitumor effects in patients with LUAD who can benefit from standard chemotherapeutic regimens.
Patients in the high-risk group were sensitive to ABT.888, AICAR, MS.275, sunitinib, AZD.2281, and GDC.0449. AT.888 has been used to treat a wide variety of tumors. Patients in the high-risk group were sensitive to BIBW2992, bicalutamide, doxorubicin, embelin, gemcitabine, midostaurin, parthenolide, pazopanib, rapamycin, salubrinal, sunitinib, and tipifarnib, which can be used to treat a wide range of tumors. Bicalutamide, a second-generation oral nonsteroidal antiandrogen, is widely used to treat prostate cancer and triple-negative breast cancer43,44. Sunitinib is a tyrosine kinase inhibitor with antiangiogenic properties that plays a crucial role in the treatment of metastatic renal cell carcinoma45. We also used the cMap database to screen eight small-molecule drugs for LUAD treatment. Therefore, the results of this study can be used to provide personalized and precise drug treatment for high-risk patients.
Our study had several limitations. First, we conducted a retrospective analysis of the signature using data from the GEO database. However, to further assess its clinical value, it is imperative to conduct more prospective studies. Second, further in vivo and in vitro investigations are necessary to explore the involvement of the six selected genes in the development of LUAD. Third, this study analyzed the correlation between risk models and various aspects of the immune system, including immune cells, immune function, MHC molecules, immune checkpoints, and immunotherapy. However, sufficient samples to assess the efficacy of this model in conjunction with immunotherapy were not collected. Furthermore, a more thorough evaluation of the model by incorporating additional metrics, such as the variation statistics, unbiased concordance statistic K, and the Royston-Sauerbrei D statistic46, would be valuable.
In conclusion, we developed a novel m6A/m5C/m1A-related gene signature that can effectively predict the prognosis of patients with LUAD. This study establishes a foundation and highlights the potential predictive significance of the mechanisms connecting m6A/m5C/m1A-related genes to LUAD. Our findings may contribute to the development of novel clinical interventions for this disease.
Materials and methods
Data source
The fragments per kilobase of transcript per million mapped reads (FPKM)-normalized transcript RNA-sequencing data, relevant clinical information, and simple nucleotide variation data were downloaded from the TCGA database (https://portal.gdc.cancer.gov). The GSE37745 dataset was downloaded from the GEO database to validate the signature. The list of m6A/m5C/m1A-related genes was obtained from the GeneCards database (https://www.genecards.org), previous studies, and literature10,47,48,49.
Analysis of DE-MRGs
m6A/m5C/m1A-related genes were obtained by comparing 59 normal and 541 LUAD tissues in the TCGA using the following criteria: |log fold change (FC)|> 1 and a false discovery rate (FDR) < 0.05. The genes were analyzed using Metascape (https://metascape.org)50 for GO and KEGG analyses and visualized using ggplot2.
Hub DE-MRGs selection and analyses
The online STRING database (https://string-db.org/) was used to analyze the interactive relationships among the DE-ERGs. Parameter settings were as follows: network scoring, degree cutoff = 2 and cluster finding, node score cutoff = 0.2, k-core = 2, and maximum depth = 100. Cytoscape software (version 3.7.0) was used to create PPI networks. The top ten DE-MRGs with higher node degree scores were identified as hub ERGs using the Cytoscape plug-in CytoHubba. Hub modules were analyzed using MCODE plug-ins in Cytoscape.
Cluster analysis
Prognosis-related DE-MRGs were screened using univariate Cox regression analysis. The “ConsensusClusterPlus” package was used to perform cluster analysis to identify m6A/m5C/m1A-related molecule subtypes51. Survival analysis was performed to compare the prognosis between the two clusters. A heatmap was used to display the correlation between clusters and clinical parameters, which were analyzed using the chi-square test.
Construction and validation of the prognostic signature
Multivariate Cox regression analysis was used to identify DE-MRGs that provided a prognostic signature. ROC and KM analysis were used to evaluate the prognostic value of the signature52,53. The GSE37745 dataset was used to validate the prognostic signatures. Univariate and multivariate Cox regression analyses were performed to determine whether the signature was an independent risk factor. We combined risk scores with clinicopathological characteristics to construct a nomogram that predicted survival at 1, 3, and 5 years in patients with LUAD. Calibration curves were used to determine whether the predicted survival rates were consistent with actual survival rates.
GSEA
Patients with LUAD were divided into high- and low-risk groups based on the median risk scores. To explore the potential underlying mechanisms, we used GSEA v4.1.0 (http://www.broad.mit.edu/gsea) to investigate the enriched pathways in the high-risk group, with p < 0.05 and FDR < 0.25 as thresholds for statistical significance54.
Immune landscape analysis
The infiltration scores of 16 immune cells and the activities of 13 immune-related pathways were calculated using the GSVA software package employing the ssGSEA method55. Marker genes of various immune cells were obtained from previous studies56 and are listed in Table S2. The ESTIMATE algorithm was used to calculate the immune score, stromal score, estimated score, and tumor purity of all patients with LUAD. Immune cell infiltration was analyzed using the CIBERSORT algorithm and TIMER database. We also compared the expression of MHC molecules using cluster and signature analyses.
We compared five commonly studied immunoinhibitors (PD-L1, CD86, HAVCR2, CTLA4, and LAG3) based on clusters and risks for the immune checkpoints.
Tumor-related scores and tumor stemness indices (TSIs) analysis
The ssGSEA algorithm was utilized to calculate the scores of angiogenic activity, mesenchymal-EMT, tumorigenic cytokines, and stemness for each tumor sample, and relevant marker genes are listed in Table S3. TSIs were closely linked to active biological processes in stem cells and correlated with a higher degree of tumor dedifferentiation. We obtained TSIs from the TCGA in a previous study57.
Gene mutation analysis
Somatic mutation expression data were obtained from the TCGA and analyzed using the R package “maftools.” We calculated the TMB for each patient and compared it between the high- and low-risk groups. Additionally, we conducted a survival analysis based on the TMB scores. The cBioPortal database was used to display somatic mutations in selected genes in the signature58.
Chemotherapy response and small-molecule drugs
To investigate the predictive role of the signature concerning the clinical response to treatment, we utilized the 'pRRophetic' package to calculate the IC50 values of commonly used chemotherapeutic agents for the clinical treatment of LUAD. The Wilcoxon signed-rank test was used to compare the IC50 values of the chemotherapeutic drugs between the high- and low-risk groups.
Statistical analysis
DE-MRGs were screened using the Wilcoxon test. Univariate Cox regression analysis was used to analyze the relationship between m6A/m5C/m1A-associated genes and overall survival (OS). Multifactorial Cox regression analysis was used to screen for genes associated with m6A/m5C/m1A and construct a predictive signature. Kaplan–Meier survival analysis and log-rank tests were used to analyze the differences in OS between the different risk score groups. The "timeROC" package was utilized to generate ROC curves and calculate the AUC. All statistical analyses were performed using R software v4.1.3 and its appropriate websites59.
Data availability
Some or all data, models, or code generated or used during the study are available from the corresponding author by request.
References
Sung, H. et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249 (2021).
Konert, T. et al. Introducing FDG PET/CT-guided chemoradiotherapy for stage III NSCLC in low- and middle-income countries: Preliminary results from the IAEA PERTAIN trial. Eur. J. Nucl. Med. Mol. Imaging 46, 2235–2243 (2019).
Chen, J. et al. LINC00173v.1 promotes angiogenesis and progression of lung squamous cell carcinoma by sponging miR-511-5p to regulate VEGFA expression. Mol. Cancer 19, 98 (2020).
Jin, X., Zhang, B., Zhang, H. & Yu, H. Smoking-associated upregulation of CBX3 suppresses ARHGAP24 expression to activate Rac1 signaling and promote tumor progression in lung adenocarcinoma. Oncogene 41, 538–549 (2022).
Liang, R., Li, X., Li, W., Zhu, X. & Li, C. DNA methylation in lung cancer patients: Opening a “window of life” under precision medicine. Biomed. Pharmacother. 144, 112202 (2021).
Liu, Y. et al. Potentiated lung adenocarcinoma (LUAD) cell growth, migration and invasion by lncRNA DARS-AS1 via miR-188-5p/ KLF12 axis. Aging (Albany NY). 13, 23376–23392 (2021).
Miller, K. D. et al. Cancer treatment and survivorship statistics, 2016. CA Cancer J. Clin. 66, 271–289 (2016).
Chen, S. et al. Targeting the Histone methyltransferase disruptor of telomeric silencing 1-Like restricts avian leukosis virus subgroup j replication by restoring the innate immune response in chicken macrophages. Front. Microbiol. 11, 603131 (2020).
An, Y. & Duan, H. The role of m6A RNA methylation in cancer metabolism. Mol. Cancer 21, 14 (2022).
Wang, T., Kong, S., Tao, M. & Ju, S. The potential role of RNA N6-methyladenosine in cancer progression. Mol. Cancer 19, 88 (2020).
Wang, Y. et al. Aberrant m5C hypermethylation mediates intrinsic resistance to gefitinib through NSUN2/YBX1/QSOX1 axis in EGFR-mutant non-small-cell lung cancer. Mol. Cancer 22, 81 (2023).
Li, J., Zhang, H. & Wang, H. N(1)-methyladenosine modification in cancer biology: Current status and future perspectives. Comput. Struct. Biotechnol. J. 20, 6578–6585 (2022).
Bai, R. et al. Genetic diversity and drug susceptibility patterns of the Mycobacterium tuberculosis complex in Yunnan, China. Biosci. Rep. 39, BSR20181746 (2019).
Wang, G., Qu, F., Liu, S., Zhou, J. & Wang, Y. Nucleolar protein NOP2 could serve as a potential prognostic predictor for clear cell renal cell carcinoma. Bioengineered 12, 4841–4855 (2021).
Pan, J., Huang, Z. & Xu, Y. m5C RNA methylation regulators predict prognosis and regulate the immune microenvironment in lung squamous cell carcinoma. Front. Oncol. 11, 657466 (2021).
Li, M. et al. 5-methylcytosine RNA methyltransferases and their potential roles in cancer. J. Transl. Med. 20, 214 (2022).
Rong, D. et al. Epigenetics: Roles and therapeutic implications of non-coding RNA modifications in human cancers. Mol. Ther. Nucl. Acids. 25, 67–82 (2021).
Yamato, I. et al. PCA-1/ALKBH3 contributes to pancreatic cancer by supporting apoptotic resistance and angiogenesis. Cancer Res. 72, 4829–4839 (2012).
Ueda, Y. et al. AlkB homolog 3-mediated tRNA demethylation promotes protein synthesis in cancer cells. Sci. Rep. 7, 42271 (2017).
Lu, T. et al. Trends in the incidence, treatment, and survival of patients with lung cancer in the last four decades. Cancer Manag. Res. 11, 943–953 (2019).
Chen, W. et al. Cancer statistics in China, 2015. CA Cancer J. Clin. 66, 115–132 (2016).
Zhu, T. G., Xiao, X., Wei, Q., Yue, M. & Zhang, L. X. Revealing potential long non-coding RNA biomarkers in lung adenocarcinoma using long non-coding RNA-mediated competitive endogenous RNA network. Braz. J. Med. Biol. Res. 50, e6297 (2017).
Ruan, W., Wang, P., Feng, S., Xue, Y. & Li, Y. Long non-coding RNA small nucleolar RNA host gene 12 (SNHG12) promotes cell proliferation and migration by upregulating angiomotin gene expression in human osteosarcoma cells. Tumour Biol. 37, 4065–4073 (2016).
Wang, J. Z., Xu, C. L., Wu, H. & Shen, S. J. LncRNA SNHG12 promotes cell growth and inhibits cell apoptosis in colorectal cancer cells. Braz. J. Med. Biol. Res. 50, e6079 (2017).
Wang, O. et al. C-MYC-induced upregulation of lncRNA SNHG12 regulates cell proliferation, apoptosis and migration in triple-negative breast cancer. Am. J. Transl. Res. 9, 533–545 (2017).
Jiang, F., Hu, Y., Liu, X., Wang, M. & Wu, C. Methylation pattern mediated by m(6)A regulator and tumor microenvironment invasion in lung adenocarcinoma. Oxid. Med. Cell Longev. 2022, 2930310 (2022).
Zhang, J. et al. LIN28B-AS1-IGF2BP1 binding promotes hepatocellular carcinoma cell progression. Cell Death Dis. 11, 741 (2020).
Huang, H. et al. Recognition of RNA N(6)-methyladenosine by IGF2BP proteins enhances mRNA stability and translation. Nat. Cell Biol. 20, 285–295 (2018).
Bell, J. L. et al. Insulin-like growth factor 2 mRNA-binding proteins (IGF2BPs): Post-transcriptional drivers of cancer progression?. Cell Mol. Life Sci. 70, 2657–2675 (2013).
Costa, R. H. FoxM1 dances with mitosis. Nat. Cell Biol. 7, 108–110 (2005).
Xu, N. et al. FoxM1 is associated with poor prognosis of non-small cell lung cancer patients through promoting tumor metastasis. PLoS One 8, e59412 (2013).
Madhi, H. et al. FOXM1 inhibition enhances the therapeutic outcome of lung cancer immunotherapy by modulating PD-L1 expression and cell proliferation. Adv. Sci. (Weinh). 9, e2202702 (2022).
Xiu, G., Sui, X., Wang, Y. & Zhang, Z. FOXM1 regulates radiosensitivity of lung cancer cell partly by upregulating KIF20A. Eur. J. Pharmacol. 833, 79–85 (2018).
Milewski, D. et al. FOXM1 activates AGR2 and causes progression of lung adenomas into invasive mucinous adenocarcinomas. PLoS Genet. 13, e1007097 (2017).
Rossetti, S., Hoogeveen, A. T., Esposito, J. & Sacchi, N. Loss of MTG16a (CBFA2T3), a novel rDNA repressor, leads to increased ribogenesis and disruption of breast acinar morphogenesis. J. Cell. Mol. Med. 14, 1358–1370 (2010).
Zhang, D. L. et al. Genome-wide identification of transcription factors that are critical to non-small cell lung cancer. Cancer Lett. 434, 132–143 (2018).
Xu, R. et al. Identification of tumor antigens and immune subtypes in lung adenocarcinoma for mRNA vaccine development. Front. Cell Dev. Biol. 10, 815596 (2022).
Jiang, X. et al. Silencing of CASC8 inhibits non-small cell lung cancer cells function and promotes sensitivity to osimertinib via FOXM1. J. Cancer. 12, 387–396 (2021).
Cui, Z., Gao, M., Yin, Z., Yan, L. & Cui, L. Association between lncRNA CASC8 polymorphisms and the risk of cancer: A meta-analysis. Cancer Manag. Res. 10, 3141–3148 (2018).
Saito, K. et al. PODXL1 promotes metastasis of the pancreatic ductal adenocarcinoma by activating the C5aR/C5a axis from the tumor microenvironment. Neoplasia 21, 1121–1132 (2019).
Tang, X. et al. A mechanically-induced colon cancer cell population shows increased metastatic potential. Mol. Cancer 13, 131 (2014).
Xu, C., Li, F., Liu, Z., Yan, C. & Xiao, J. A novel cell senescence-related IncRNA survival model associated with the tumor immune environment in colorectal cancer. Front. Immunol. 13, 1019764 (2022).
Gerratana, L. et al. Androgen receptor in triple negative breast cancer: A potential target for the targetless subtype. Cancer Treat. Rev. 68, 102–110 (2018).
Harris, A. E. et al. Exploring anti-androgen therapies in hormone dependent prostate cancer and new therapeutic routes for castration resistant prostate cancer. Front. Endocrinol. (Lausanne) 13, 1006101 (2022).
Nassif, E. et al. Sunitinib in kidney cancer: 10 years of experience and development. Expert Rev. Anticancer Ther. 17, 129–142 (2017).
Patrick, R. & Douglas, G. External validation of a Cox prognostic model: Principles and methods. BMC Med. Res. Methodol. 13, 13 (2013).
Zhang, Q. et al. The role of RNA m(5)C modification in cancer metastasis. Int. J. Biol. Sci. 17, 3369–3380 (2021).
Li, X. et al. Transcriptome-wide mapping reveals reversible and dynamic N(1)-methyladenosine methylome. Nat. Chem. Biol. 12, 311–316 (2016).
Bohnsack, K. E., Höbartner, C. & Bohnsack, M. T. Eukaryotic 5-methylcytosine (m5C) RNA methyltransferases: Mechanisms, cellular functions, and links to disease. Genes (Basel). 10, 102 (2019).
Zhou, Y. et al. Metascape provides a biologist-oriented resource for the analysis of systems-level datasets. Nat. Commun. 10, 1523 (2019).
Wang, W. et al. The cuproptosis-related signature associated with the tumor environment and prognosis of patients with glioma. Front. Immunol. 13, 998236 (2022).
Wu, M., Li, X., Zhang, T., Liu, Z. & Zhao, Y. Identification of a nine-gene signature and establishment of a prognostic nomogram predicting overall survival of pancreatic cancer. Front. Oncol. 9, 996 (2019).
Zhang, Y. et al. A novel oxidative-stress related lncRNA signature predicts the prognosis of clear cell renal cell carcinoma. Sci. Rep. 13, 5740 (2023).
Qiu, C. et al. Identification of molecular subtypes and a prognostic signature based on inflammation-related genes in colon adenocarcinoma. Front. Immunol. 12, 769685 (2021).
Li, Z. et al. Construction of a novel signature and prediction of the immune landscape in gastric cancer based on necroptosis-related genes. Sci. Rep. 12, 13290 (2022).
Bindea, G. et al. Spatiotemporal dynamics of intratumoral immune cells reveal the immune landscape in human cancer. Immunity 39, 782–795 (2013).
Malta, T. M. et al. Machine learning identifies stemness features associated with oncogenic dedifferentiation. Cell 173, 338-354.e315 (2018).
Wei, Y. et al. Robust analysis of a novel PANoptosis-related prognostic gene signature model for hepatocellular carcinoma immune infiltration and therapeutic response. Sci. Rep. 13, 14519 (2023).
Song, D. et al. Identification and validation of prognosis-associated DNA repair gene signatures in colorectal cancer. Sci. Rep. 12, 6946 (2022).
Funding
This work was supported by the Regional Fund Project of the National Natural Science Foundation of China (82360523), the Regional Fund Project of the National Natural Science Foundation of China (82060423), Xingdian Talent Plan “Famous Doctor Special Project” (RLMY20220018), Science and Technology Innovation Team for Precision Pathological Diagnosis of Lung Malignant Tumours at Kunming Medical University (CXTD202210) and Scientific Research Fund Project of Education Department of Yunnan Province (2024Y221).
Author information
Authors and Affiliations
Contributions
YZ and LB initiated the project and were responsible for protocol design. YZ, QYJ, FFL, XL, ZYW, XFW and LB download and collate data. YZ, QYJ, FFL, YHW, YLZ, MYL, XL and LB interpreted the data and constructed the signature. YZ, QYJ, FFL and LB wrote the initial draft of the manuscript. All authors were responsible for critical revision of the manuscript and provided important intellectual content. All authors approved the final version of the manuscript submitted for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, Y., Jia, Q., Li, F. et al. Identification of molecular subtypes and a prognostic signature based on m6A/m5C/m1A-related genes in lung adenocarcinoma. Sci Rep 14, 7543 (2024). https://doi.org/10.1038/s41598-024-57910-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-57910-5
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.