Abstract
Darier disease (DD) is a rare monogenetic skin disorder with limited data on its potential association with neurological disorders. This study aimed to investigate the association between DD and neurological disorders, specifically Parkinson's disease, dementias, and epilepsy. Using Swedish national registers in a period spanning between 1977 and 2013, 935 individuals with DD were compared with up to 100 comparison individuals each, randomly selected from the general population based on birth year, sex, and county of residence at the time of the first diagnosis of DD. Individuals with DD had increased risks of being diagnosed with Parkinson's disease (RR 2.1, CI 1.1; 4.4), vascular dementia (RR 2.1, CI 1.0; 4.2), and epilepsy, (RR 2.5, CI 1.8; 3.5). No association of DD with other dementias were detected. This study demonstrates a new association between DD and neurodegenerative disorders and epilepsy, underlining the need for increased awareness, interdisciplinary collaboration, and further research to understand the underlying mechanisms. Early identification and management of neurological complications in DD patients could improve treatment strategies and patient outcomes. The findings also highlight the role of SERCA2 in the pathophysiology of neurological disorders, offering new targets for future research and potentials for novel treatments.
Similar content being viewed by others
Introduction
Darier disease (DD) is an autosomal dominant genodermatosis characterized by keratotic papules and plaques, malodorous skin, nail abnormalities, and mucosal changes1. DD is caused by mutations in the ATP2A2 gene, which encodes the sarco/endoplasmic reticulum Ca2+-ATPase isoform 2 (SERCA2) pump2. SERCA2 is ubiquitously expressed and important for maintaining Ca2+ homeostasis in the endoplasmic reticulum3,4. Dysfunction of SERCA2 leads to abnormal intracellular Ca2+ levels and impaired cell adhesion, ultimately resulting in the characteristic skin manifestations of DD. Being a rare disorder, the estimated prevalence of DD is 1 in 30,000–100,000 individuals5.
Although DD is traditionally considered to be a skin disorder, several studies have suggested potential links between DD and psychiatric disorders6,7. In a descriptive study of 163 DD patients, a larger occurrence of epilepsy than the population baseline has been seen1. The evidence for an association with neurological disorders is, however, lacking. The ATP2A2 gene is expressed in various regions of the brain, and the role of SERCA2 dysfunction in the neurobiology and pathophysiology of several neurological disorders is well documented3. Given these findings, this study aimed to investigate the plausible association between DD and common neurological disorders such as Parkinson's disease (PD), vascular dementia, Alzheimer’s disease (AD), other dementias, and epilepsy.
Results
Individuals with DD had an increased risk of being diagnosed with PD (RR 2.1, CI 1.1; 4.4) and vascular dementia (RR 2.1, CI. 1.0; 4.2), whereas no association with other dementias could be confirmed (RR 1.1, CI 0.7; 2.0). Due to insufficient statistical power, the association of DD with AD could not be assessed. Finally, there was an increased risk of epilepsy in individuals with DD (RR 2.5, CI 1.8; 3.5). Risk ratios adjusted for common and impactful vascular risk factors did not more than marginally differ from unadjusted risk ratios regarding PD and epilepsy, whereas the adjusted risk ratio for vascular dementia turned insignificant (RR 1.5, CI 0.8; 4.9). All results are presented in Table 1.
Discussion
Our findings revealed for the first time that individuals with DD had an increased risk of PD, vascular dementia, and epilepsy. This suggests a potential connection between DD and these neurological disorders and constitutes direct human evidence for the role of SERCA2 in neurological disease. Although the underlying mechanisms remain unclear, several hypotheses can be proposed. For instance, the ATP2A2 gene, which is causal in DD, is also involved in Ca2+ signaling in neurons8. Dysregulation of Ca2+ signaling has been implicated in the pathophysiology of various neurological disorders, including PD and epilepsy9. No association between DD and AD was seen due to low insufficient statistical power. Considering that AD is the most prevalent neurodegenerative disorder, a reasonable conclusion is that there might indeed be no association. Further, the association with vascular dementia lost significance when adjusting for a large array of vascular risk factors, tempering this association.
SERCA2 is a ubiquitously expressed protein, meaning that the ATP2A2 mutations give rise to lower functioning levels of SERCA2 in all tissues, not just the skin4. Given the important role of SERCA2 in the brain, it is reasonable that individuals with DD also display increased risks of neurological disorders, as shown in this investigation. Several recent studies have given evidence of DD being a disorder with significant comorbidities including heart failure, diabetes, and cognitive dysfunction10,11,12. This further implies the ubiquitous nature of SERCA2 dysfunction in DD and broadens the understanding of DD as a multisystem condition.
Moreover, the genetic background of DD may predispose individuals to a higher risk of developing neurological disorders due to shared genetic factors or pleiotropic effects13. It is currently unknown whether pleiotropic effects or interactions of ATP2A2 mutations with other specific constellations of genes can explain the associations seen. Furthermore, the common embryological origin of both skin and nervous tissue from the ectoderm might imply a shared pathophysiological role. Future research should focus on identifying potential genetic modifiers or interactions that could contribute to the observed associations. An alternative speculative explanation could be that individuals with DD may experience increased exposure to risk factors for developing neurological disorders throughout their lives.
Strengths and limitations
The main strengths of this study are the rigorous methodology with a longitudinal design and incidence density sampling scheme with a 1:100 matching ratio, allowing for a robust estimation of the association between DD and neurological disorders. The sample size of 935 individuals with DD is uniquely large given the rarity of DD, further increasing statistical power and the reliability of the findings. Lastly, Swedish nationwide registers are comprehensive and of very high quality.
The lack of association between DD and other dementias may be due to the limited sample size and the need for further research to explore this relationship. It is also important to note that the study was unable to provide an estimation of the association with Alzheimer's disease due to insufficient power since only two individuals with DD in our cohort had such a diagnosis. One limitation of this study is the reliance on register-based data, which may be subject to diagnostic misclassification. However, a validation study has shown that diagnoses of chronic somatic diseases in the NPR, such as DD, are generally valid14, and assigned by specialist physicians in their respective fields.
Conclusions
This study provides evidence for an association between DD and certain neurological disorders, including PD, vascular dementia, and epilepsy. Clinicians treating patients with DD should be aware of the potentially increased risk of neurological disorders in this population. Early identification of neurological complications in individuals with DD may enable improved management and treatment strategies, ultimately enhancing patient outcomes. The observed associations underscore the importance of interdisciplinary collaboration in the care of patients with DD and co-occurring neurological disorders. These findings also highlight the need for further research to better understand the underlying mechanisms linking DD and neurological disorders. Lastly, further light is shed on the role of SERCA2 in brain pathophysiology, providing new targets for future research and highlighting the potential for therapeutic interventions.
Methods
Ethics
This study was approved by the Swedish Ethical Review Authority. All methods were carried out in accordance with relevant guidelines and regulations.
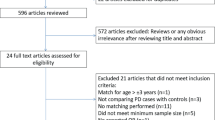
Study population
We identified a total of 935 individuals with DD and matched them with up to 100 comparison individuals each, all derived and randomly selected from the general population. Matching was done for birth year, sex, and county of residence at the time of the first DD diagnosis of the index person, i.e., an incidence density sampling scheme. The study period spanned between 1977 and 2013.
Data sources
We performed a longitudinal cohort study based on the Swedish Total Population Register, which holds demographic information on all individuals registered as Swedish inhabitants since 1968, including immigrants and The National Patient Register (NPR), which includes discharge diagnoses for inpatient care since 1973 and for outpatient care since 200115. All diagnoses were assigned by the treating medical doctor according to International Classification of Diseases, Ninth and Tenth Revision (ICD-9/10). The linkage between registers was made possible by the unique personal identification number, which is assigned to all individuals born in Sweden since 1932, and to immigrants at their arrival to Sweden.
Study variables
DD was the exposure in the study and defined as a diagnosis of Q82.8E (ICD-10) or 757D (ICD-9) in the NPR. PD, vascular dementia, AD, other dementias, and epilepsy were the outcomes of the study and defined as (1) G20 (ICD-10) or 332A (ICD-9) for PD, (2) F01 (ICD-10) or 290E (ICD-9) for vascular dementias, (3) F00 and G30 (ICD-10) or 290A-B and 331A (ICD-9) for AD, (4) F02, F03, F051, G311 and G318A (ICD-10) or 290W, 290X, 294B, 331B, 331C and 331X (ICD-9) for other dementias, and (5) G40-41 (ICD-10) or 345 (ICD-9) for epilepsy. Vascular risk factors in the adjusted analysis were defined as I63 (ICD-10) or 433, 434, and 436 (ICD-9) for stroke, I21 (ICD-10) or 410 (ICD-9) for myocardial infarction, I50 (ICD-10) or 428 (ICD-9) for heart failure, I10.9 (ICD-10) or 401 (ICD-9) for essential hypertension, I15.9 (ICD-10) or 405 (ICD-9) for secondary hypertension, E10 (ICD-10) or 250 (ICD-9) for diabetes type 1, E11 (ICD-10) or 250 (ICD-9) for diabetes type 2, and E78.0, 1, 2, 5 (ICD-10) or 272A, B, C, E (ICD-9) for hyperlipidemias.
Statistical analysis
Conditional logistic regression analysis was performed to assess the associations between exposure and outcomes, with results expressed as odds ratios and corresponding 95% confidence intervals. SAS 9.3 software (SAS Institute, Cary, NC) was used for all analyses. As a result of the incidence density sampling, all odds ratios can be interpreted as risk ratios (RR).
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Burge, S. M. & Wilkinson, J. D. Darier-White disease: A review of the clinical features in 163 patients. J. Am. Acad. Dermatol. 27(1), 40–50 (1992).
Sakuntabhai, A. et al. Mutations in ATP2A2, encoding a Ca2+ pump, cause Darier disease. Nat. Genet. 21(3), 271–277. https://doi.org/10.1038/6784 (1999).
Britzolaki, A., Saurine, J., Klocke, B. & Pitychoutis, P. M. A role for SERCA pumps in the neurobiology of neuropsychiatric and neurodegenerative disorders. Adv. Exp. Med. Biol. 1131, 131–161. https://doi.org/10.1007/978-3-030-12457-1_6 (2020).
Vandecaetsbeek, I. et al. Structural basis for the high Ca2+ affinity of the ubiquitous SERCA2b Ca2+ pump. Proc. Natl. Acad. Sci. USA. 106(44), 18533–18538. https://doi.org/10.1073/pnas.0906797106 (2009).
Cooper, S. M. & Burge, S. M. Darier’s disease: Epidemiology, pathophysiology, and management. Am. J. Clin. Dermatol. 4(2), 97–105 (2003).
Cederlof, M. et al. The association between Darier disease, bipolar disorder, and schizophrenia revisited: A population-based family study. Bipolar Disord. 17(3), 340–344. https://doi.org/10.1111/bdi.12257 (2015).
Craddock, N. et al. Familial cosegregation of major affective disorder and Darier’s disease (keratosis follicularis). Br. J. Psychiatry. 164(3), 355–358. https://doi.org/10.1192/bjp.164.3.355 (1994).
Britzolaki, A., Saurine, J., Flaherty, E., Thelen, C. & Pitychoutis, P. M. The SERCA2: A gatekeeper of neuronal calcium homeostasis in the brain. Cell Mol. Neurobiol. 38(5), 981–994. https://doi.org/10.1007/s10571-018-0583-8 (2018).
Brini, M., Calì, T., Ottolini, D. & Carafoli, E. Intracellular calcium homeostasis and signaling. Met. Ions Life Sci. 12, 119–168. https://doi.org/10.1007/978-94-007-5561-1_5 (2013).
Bachar-Wikstrom, E. et al. Darier disease is associated with heart failure: a cross-sectional case-control and population based study. Sci. Rep. 10(1), 6886. https://doi.org/10.1038/s41598-020-63832-9 (2020).
Cederlöf, M. et al. Darier disease is associated with type 1 diabetes: Findings from a population-based cohort study. J. Am. Acad. Dermatol. 81(6), 1425–1426. https://doi.org/10.1016/j.jaad.2019.05.087 (2019).
Curman, P. et al. Patients with darier disease exhibit cognitive impairment while patients with hailey-hailey disease do not: an experimental, matched case-control study. Acta Derm. Venereol. 101(6), 476. https://doi.org/10.2340/00015555-3818 (2021).
Zuk, O., Hechter, E., Sunyaev, S. R. & Lander, E. S. The mystery of missing heritability: Genetic interactions create phantom heritability. Proc. Natl. Acad. Sci. USA. 109(4), 1193–1198. https://doi.org/10.1073/pnas.1119675109 (2012).
Ludvigsson, J. F. et al. External review and validation of the Swedish national inpatient register. BMC Public Health. 11, 450. https://doi.org/10.1186/1471-2458-11-450 (2011).
Ludvigsson, J. F. et al. Registers of the Swedish total population and their use in medical research. Eur. J. Epidemiol. 31(2), 125–136. https://doi.org/10.1007/s10654-016-0117-y (2016).
Funding
Open access funding provided by Karolinska Institute. This article was funded by Hudfonden, Swedish Science Council, Svenska Sällskapet för Medicinsk Forskning, Leo foundation, ALF medicin Stockholm, Jeanssons stiftelse, Marcus och Amalia Wallenbergs minnesfond and Tore Nilssons Stiftelse.
Author information
Authors and Affiliations
Contributions
All authors contributed to conceptualizing the project and design the experiments. PC and MC performed analysis. All authors contributed to the manuscript writing that was led by PC and JDW. JDW led the study.
Corresponding author
Ethics declarations
Competing interests
Henrik Larsson reports receiving grants from Shire Pharmaceuticals; personal fees from and serving as a speaker for Medice, Shire/Takeda Pharmaceuticals and Evolan Pharma AB; and sponsorship for a conference on attention-deficit/hyperactivity disorder from Shire/Takeda Pharmaceuticals and Evolan Pharma AB, all outside the submitted work. Henrik Larsson is editor-in-chief of JCPP Advances. The other authors have no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Curman, P., Jebril, W., Larsson, H. et al. Darier disease is associated with neurodegenerative disorders and epilepsy. Sci Rep 14, 7109 (2024). https://doi.org/10.1038/s41598-024-57779-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-57779-4
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.