Abstract
Proximal femoral fractures are a serious life-threatening injury with high morbidity and mortality. Magnetic resonance (MR) imaging has potential to non-invasively assess proximal femoral bone strength in vivo through usage of finite element (FE) modelling (a technique referred to as MR-FE). To precisely assess bone strength, knowledge of measurement error associated with different MR-FE outcomes is needed. The objective of this study was to characterize the short-term in vivo precision errors of MR-FE outcomes (e.g., stress, strain, failure loads) of the proximal femur for fall and stance loading configurations using 13 participants (5 males and 8 females; median age: 27 years, range: 21–68), each scanned 3 times. MR-FE models were generated, and mean von Mises stress and strain as well as principal stress and strain were calculated for 3 regions of interest. Similarly, we calculated the failure loads to cause 5% of contiguous elements to fail according to the von Mises yield, Brittle Coulomb-Mohr, normal principal, and Hoffman stress and strain criteria. Precision (root-mean squared coefficient of variation) of the MR-FE outcomes ranged from 3.3% to 11.8% for stress and strain-based mechanical outcomes, and 5.8% to 9.0% for failure loads. These results provide evidence that MR-FE outcomes are a promising non-invasive technique for monitoring femoral strength in vivo.
Similar content being viewed by others
Introduction
Osteoporosis, through its association with age-related fractures, is one of the most common causes of longstanding pain, functional impairment, disability, and death in elderly populations, and a major contributor to medical care costs worldwide1,2. Hip fracture, in particular, is a serious life-threatening injury, with fracture of the proximal femoral neck, intertrochanteric and/or shaft regions typically occurring from a sideways fall from standing height. Mortality after hip fracture is high (~ 10%) in the immediate post-fracture period, and remains higher than that of the general population1,3,4,5. For these reasons, effective intervention strategies to reduce the risk of hip fracture at both individual and population levels are warranted.
It is well established that exercise training is beneficial for improving bone strength (i.e., bone’s load carrying capacity or failure load), particularly when starting during early adolescence6. With exercise training, bone strength may be maintained (or increased) and hip fracture risk may be reduced in old age. In order to identify specific exercise protocols which reduce hip fracture risk, non-invasive in vivo estimates of proximal femoral strength during adolescence and early adulthood are required.
Dual energy X-ray absorptiometry (DXA) is a two-dimensional (2D) imaging technique offering measures of areal bone mineral density (aBMD) of the proximal femur. The technique is low dose (0.14 µSv7), and thus is suitable for adolescents and young adults8. DXA-based aBMD measures of the proximal femur offer modest-to-strong agreement with experimentally-derived failure load (fall configuration: R2 ranging from 0.41 to 0.929,10,11,12; stance configuration: R2 ranging from 0.42 to 0.7113,14) (for a detailed overview, see summary table in15). DXA though offers representations of complex 3D structures as 2D projection images, and thus cannot distinguish between cortical or trabecular bone geometry or material properties, each of which independently contribute to proximal femoral strength16. Quantitative computed tomography (QCT) is a three-dimensional (3D) imaging technique offering measures of volumetric BMD (BMD) of both cortical and trabecular bone. On its own, QCT measures of proximal femoral geometry and density offers modest predictions of failure load (fall: R2 = 0.199; stance: R2 = 0.6617). However, when combined with computational finite element (FE) modelling (a method referred to as QCT-FE), the approach offers stronger agreement with experimentally-derived failure load (fall: R2 ranging from 0.73 to 0.9012,18,19,20,21; stance: R2 ranging from 0.63 to 0.9517,19,20,21,22). QCT, however, exposes participants to higher levels of ionizing radiation at the radiosensitive pelvic region (e.g., 2900 µSv from Khoo et al.23), which some may argue is ethically unacceptable for growing adolescents and fertile young adults. Accordingly, the QCT-FE technique is typically applied with elderly adult populations. Recently, FE combined with magnetic resonance (MR) imaging (referred to as MR-FE) has seen application for identifying failure regions as well as assessing hip strength of exercise groups engaging in different levels of physical activity (high-impact, odd-impact, repetitive-impact, high-magnitude, non-impact)24,25,26. The key benefits of MR is that it offers multi-planar 3D images and nonionizing radiation of the radiosensitive pelvis (and thus has potential for studying adolescents and young adults). Current research suggests that MR-FE is an accurate tool for estimating mechanical failure loads of the proximal femur with strong agreement with experimentally obtained values (fall: R2 = 0.85)27. To date, there has only been one study which assessed the in vivo precision error of MR-FE; however, this study focused on whole-bone stiffness and elastic modulus for a small region of interest (ROI)28. Currently, the measurement repeatability of MR-FE mechanical outcomes (specifically bone stress and failure load) has not been reported at critical failure regions for fall and stance loading configurations.
Knowledge of the measurement error is important to establish the repeatability of the technique. Specifically, an understanding of the precision error is critical as it identifies parameters which may be best suited for future research related to MR-FE. Relatedly, knowledge of precision error can be used to determine the least significant change (LSC). The International Society of Clinical Densitometry recommends estimating the LSC to determine if observed skeletal differences are true and greater, with 95% confidence, than the measurement error29. LSC is estimated using the root-mean squared coefficient of variation (RMS-CV%) multiplied by an adjusting z-score (2.77 × RMS-CV% for 95% confidence) and is an important quantitative metric to ensure changes are sufficiently larger than the precision error30,31. LSC is suitably important for clinical studies and comparing bone strength differences. To date, LSCs have not been reported for MR-FE derived mechanical outcomes.
The objective of this study was to characterize the in vivo measurement precision of MR-FE mechanical outcomes of the proximal femur (bone stress and failure load, specifically) for configurations simulating fall and stance loading.
Methods
Participants
Thirteen healthy participants (5 males and 8 females) with ages ranging from 21 to 68 years (median age: 27 years), and weights ranging from 54 to 105 kg (median: 70 kg), were recruited as part of a previous study at the University of Saskatchewan32. Participant information is presented in Table 1. Study approval was obtained from the University of Saskatchewan Biomedical Research Ethics Board. All study procedures were conducted in accordance with the guidelines approved by the Biomedical Research Ethics Board and the Declaration of Helsinki. Informed consent was obtained from all study participants.
MRI scan parameters
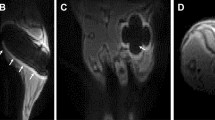
MRI scans of the left proximal femur were obtained from a previous research study32. Axial images (relative to the orientation of the participant) of the hip were obtained using a clinical 1.5 T scanner (Magnetom Avanto, Siemens, Germany) with a 6-channel body array coil positioned over the hip region. Each participant was positioned supine with their left leg extended and externally rotated 15˚. Scanned image volumes included ~ 2 cm superior to the femoral head and concluded ~ 5 cm inferior to the lesser trochanter. A T1-weighted turbo spin echo sequence was used with the following parameters: TR 616 ms, TE 12 ms, 2 excitations, 180˚ flip angle, 0.45 × 0.45 mm in plan pixel size, 4 mm slice thickness, ~ 4.5 min scan time, ~ 40 images. Each participant was scanned three times with repositioning done following a short walk between repeat scans.
Image analysis
Intensity shading inhomogeneity, commonly known as “bias field”, was present in the original MRI scans33. An open-source software platform for medical imaging (3D Slicer) was used in conjunction with a non-parametric, non-uniform intensity normalization module (N4ITK) to interactively correct the image inhomogeneity34,35. Each original scan of the proximal femur was individually loaded and processed using the correction module. Images were then qualitatively checked for shading improvement.
Using commercial software (Analyze 12.0: Mayo Foundation, Rochester, MN, USA), MRI scans were semi-automatically segmented to delineate the proximal femur from surrounding soft tissue. Each image slice was segmented in the transverse plane followed by manual correction. Subject-specific thresholds (defined via the half-maximum height, HMH) method approach were used to define the periosteal boundary and separate it from the soft tissue36,37. The thresholds were defined at a site approximately 2 cm below the lesser trochanter on the femoral shaft32. All segmentations were performed by a single researcher (K.B.M.). The original discrete MRI scans and segmentations were reformatted via cubic interpolation to create isotropic cubic arrays (from 0.45 × 0.45 × 4 mm to 0.45 × 0.45 × 0.45 mm). Following interpolation, binary masks were adjusted in the coronal plane to reduce delineation precision errors caused by participant repositioning between scans.
Image volumes (scans and masks) were aligned into fall and stance loading orientations using custom coding (Matlab 2018a; MathWorks, Natick, MA, USA), as per previous proximal femoral FE studies26,38. Using mask data, this process involved identifying the center of the femoral head by fitting a sphere to the surface of the head via a variant of the iterative closest point algorithm39. The long axis of the femur (aka shaft axis) was defined by identifying the line-of-best-fit through centroids of axial slices distal to the greater trochanter. A plane was then fit to the shaft axis and the center of the femoral head. A vector corresponding with the neck was also defined by identifying the line-of-best-fit through centroids of slices in an axial-oblique orientation. This vector was then projected to the plane containing the shaft axis and center of the femoral head. The neck axis was defined as the projected vector passing through the femoral head and intersecting with the shaft axis. This configuration was used to define the common 0° orientation with the shaft axis aligned vertically and the neck axis aligned with 0° internal/external rotation (Fig. 1). From here the images were rotated to the stance configuration (shaft long axis rotated 20° from vertical38) and fall configuration (shaft long axis tilted 10° with respect the ground with the neck axis internally rotated 15°26) (Fig. 2).
MRI scans were aligned into a common 0° orientation (shown) and then rotated into fall and stance configurations prior to FE model generation. Using the segmented mask data, the long axis of the femur (aka shaft axis) (a) was defined by identifying the line-of-best-fit through centroids of axial slices distal to the greater trochanter. The center of the femoral head (b) was identified by fitting a sphere to the surface of the head via a variant of the iterative closest point algorithm. A vector corresponding with the neck was also defined by identifying the line-of-best-fit through centroids of slices in an axial-oblique orientation. This vector was then projected to a plane containing the shaft axis and center of the femoral head. The neck axis (c) was defined as the projected vector passing through the femoral head and intersecting with the shaft axis. This configuration was used to define the common 0° orientation with the shaft axis aligned vertically and the neck axis aligned with 0° internal/external rotation.
Stance and fall loading configurations of the FE models. The shaft long axis was rotated 20° from the vertical and an initial distributed load applied over the femoral head for the stance models (a). For the fall configuration, the femoral shaft was tilted 10° with respect to the ground (b) and the neck axis was internally rotated 15° (c). The distal shaft was constrained with a hinge-type boundary condition (prohibiting displacements but allowing rotations), and the greater trochanter nodes were restrained in the direction of the distributed load.
FE modelling
FE models representative of stance and sideways fall loading configurations were generated from the realigned MRI volumes and segmentations. Using custom algorithms (Matlab), we converted each voxel into an 8-noded hexahedral element with dimensions corresponding to the 0.45 mm voxel size. Bone material properties were assumed to be linearly elastic and isotropic, with the elastic moduli of each voxel computed from the image intensity. Voxel-specific bone volume fraction’s (BVF) were computed from the image intensity via BVF = 1 − (Intvoxel/Intmax), as per40. A custom MRI phantom was used to verify that a linear relationship exists between image intensity and BVF (R2 > 0.99) (Supplementary Material). Imaged BVF was converted to elastic moduli (E) via the equation E = 12.9[1.08(1-Intvoxel/Intmax)]2, where Intvoxel is the intensity of each voxel and Intmax is the maximum fat intensity in the scan. This equation was based upon Öhman et al.41 density-modulus equation for the proximal femur, combined with conversion equations linking BVF, apparent density and ash density42,43. A Poisson’s ratio of 0.3 was assumed for all elements44.
Nodal connectivity and material properties of the proximal femur were imported into Abaqus (version 6.13, Providence, RI, USA) for loading and analysis (Fig. 2). For the loading configurations, we applied a distributed load over the femoral head. The distal shaft was fully constrained for the stance models as in previous studies20,21,38. For the sideways fall, a hinge-type boundary condition was applied on the distal shaft, and the most lateral nodes of the greater trochanter were fully constrained in the direction of the force21,26,45. For both the stance and sideways fall configurations, an arbitrary load of 1 body weight was applied (arbitrary in that the linearity of the models allowed for the results to be scaled).
FE outcomes
The FE outcomes were analyzed at 4.5 mm thick anatomical regions of interest (Fig. 3) at the neck, intertrochanteric, and shaft. The regions were selected based on common critical failure regions and automatically defined using anatomical landmarks and custom coding (Matlab)38,45. For each region and orientation, the mean von Mises stress, von Mises strain, principal stresses, and principal strains were calculated. The principal stresses and strains were used to derive failure loads from four different failure criteria, including the von Mises yield, brittle Coulomb-Mohr (BCM), normal principal, and Hoffman criteria stress and strain analogs19,20,46,47,48. Failure theories were assessed at the three regions of interest for each configuration. The applied force was linearly scaled to determine the failure load which would cause 5% of contiguous elements to fail.
Strain and equivalent stress limits were used for cortical and trabecular bone. We assigned bone a tensile strain limit of 7000 μstrain49,50 and a compressive strain limit of 10,000 μstrain41. The equivalent stress limits were assigned by multiplying the strain limits by the respective element’s elastic modulus46. The tensile and compressive strain limits (εyt, εyc), and stress limits (σyt, σyc) were related using the ratios εyt/εyc and σyt/σyc, being equal to 0.720,51.
Statistical analysis
We assessed short-term in vivo precision errors of each outcome using RMS-CV% (short-term refers to the case where measurements are acquired over a time period of less than 1 month, as per Bonnick et al.31)52. With 13 participants scanned 3 times, this provided 26 degrees-of-freedom (DOF = # participants * (# scans–1)), which met recommendations by Glüer et al.52. With this DOF, we established a precision error with an upper 90% confidence limit less than ~ 30%. We report mean values for each outcome. Short-term precision was also assessed in absolute terms using the root mean square standard deviation (RMS-SD) of the 3 repeat measures.
Results
Regional means
For the fall configuration, RMS-CV% precision errors of the regional unadjusted stress and strain measures averaged 7.9% and ranged from 5.3% to 11.7% (Table 2). For the stance configuration, RMS-CV% precision errors of the regional stress and strain measures averaged 7.8% and ranged from 3.3% to 11.8%. RMS-CV% for the strain measures ranged from 7.0% to 11.8%, and 3.3% to 7.9% for the stress measures. Regional stress/strain precision errors appeared similar between the femoral neck, intertrochanteric, and shaft regions.
Failure loads
RMS-CV% precision errors for failure loads in the fall configuration averaged 7.5% and ranged from 5.8% to 9.0% (Table 3). RMS-CV% precision errors of failure loads for the stance configuration averaged 7.3% and ranged from 6.4% to 8.1%. Failure load precision errors were < 8.2% at the femoral neck, < 9.0% at intertrochanteric region, and < 8.3% at the shaft (Table 3).
Discussion
This study characterized short-term in vivo precision errors of MR-FE outcomes of the proximal femur for two loading configurations and three regions. To our knowledge, this is the first study to report FE precision errors at the neck, intertrochanteric, and shaft regions using MR-FE. This study complements existing studies which focused on evaluating differences in MR-FE outcomes between groups and provides indication of measurement error.
Generally, the von Mises stress, principal stresses, principal strains, and failure loads had similar precision errors (RMS-CV% < 8.3%), except for the von Mises strain criterion which was higher (RMS-CV% < 11.8%). The high measurement error of the von Mises strain outcomes may be attributed to the small strain values, whereby a small variation resulted in a large precision error. Our FE-based in vivo precision error results are similar (though slightly higher) to previous QCT-FE findings at the knee, which had an average RMS-CV% of < 6%53. Additionally, MR-FE precision errors for the two configurations are comparable with no substantial differences. In comparison to an MR precision study of bone morphology (e.g., cortical thickness)32, which used the same scan data evaluated here, reported precision errors were smaller (< 7.1%) than the errors reported here. Though, our study considered FE outcomes of 3D volumetric ROI’s whereas Johnston et al.32 reported metrics based on single 2D image slices.
To sufficiently recommend a best-suited failure criterion for future MR-FE studies, various parameters including precision error (RMS-CV%), explained variance (R2), and ability to capture changes or differences are needed for consideration. With regards to the presented precision errors, the four failure theories assessed in this study were similar and provided measurement errors ≤ 9.0%. Though, a large range of estimated failure loads may indicate a more sensitive criterion for identifying differences in bone strength for MR-FE. In this case, BCM (stress and strain) generally had the largest failure load ranges. In line with this finding, and comparable measurement error with other failure criteria, BCM may best characterize hip strength. Future research is needed to evaluate experimentally-derived failure loads against MR-FE derived estimates acquired via various failure theories to identify the best-suited criterion.
Numerical failure load results from this study are similar to those published in previous research25. The estimated failure loads from our study, focused on a young adult population, ranged from 3.0 to 16.4 kN at the neck in the fall configuration. Previous experimental studies found failure loads ranging from 5.2 kN to 8.5 kN for the same site and configurations45,54,55; though, these findings were specific to elderly adult (> 70 years of age) cadaveric femurs. As adult femurs are approximately twice as strong as elderly adult femurs54, our results may be comparable. Our failure load findings though are specific to the applied criteria (e.g., 5% of elements failing). A lower percentage of failed elements would lead to lower failure loads approaching experimental findings. Accordingly, further validation research is needed identifying specific modelling approaches (e.g., failure criterion, percentage of failed elements) best-suited for predicting failure of the proximal femur. Of note, stress and strain outcomes presented in this paper are presented for measurement repeatability only. The applied force magnitude of 1 body weight was arbitrary and lower than estimated failure loads. The lower applied load can explain lower stress values (Table 2, Fig. 4) in comparison to other MR-FE research (e.g., Abe et al.26 used an impact force ~ 8 × body weight).
This research has strengths requiring consideration. First, with MR-FE, each voxel of the proximal femur was modeled as a hexahedral element, allowing us to preserve the cortical detail from the scans. Conversely, using tetrahedral elements requires intensive surface smoothing and careful strategies to map elastic moduli to elements. The surface smoothing process inherently incorporates voxels inside and/or outside the original image mask, which may lead to loss of femoral detail. Secondly, we applied a custom algorithm to automatically align MR scans into the fall and stance loading configurations, which reduced variation between repeat scans, leading to a lower precision error. Third, we report precision errors at three clinically relevant regions56,57 for the two commonly studied loading configurations in the literature. The inclusion of different regions and loading configurations provides information of regional precision. Fourth, we have used a conservative sample size (13 participants, 39 scans, 26 DOF) to establish precision errors with an upper 90% confidence interval limit of ~ 30%, as proposed by Glüer et al.52. Although our study did not exactly meet the DOF recommendations (28 DOF), the upper 90% confidence limit with our DOF (31%) is comparable to recommendations (30%).
With regards to limitations, first, due to the large slice thickness (4 mm), the true 3D geometry of the femur was difficult to capture and resulted in a jagged structure. The large slice thickness may have resulted in under/over estimation of bone strength as critical bone features may not have been captured in the original scans. To more accurately characterize the shape of the proximal femur, our original scans consisting of 37 slices were interpolated to 329 slices. This approach led to a more correct shape, but small variations in material properties were not truly captured. Second, due to the poor signal-to-noise ratios on some scans, it was difficult to identify the periosteal surface within the intertrochanteric region. To segment, we defined the boundary using semi-automatic region growing and subject-specific thresholds (HMH)37, followed by manual segmentation where needed. Operator judgment had an influence on femoral segmentations and may have induced error. Third, presented MR-FE models of the proximal femur were not validated against mechanical testing, unlike previous QCT-FE studies12,17,18,19,20,21,22. To address this, we adopted similar boundary and loading conditions as previous studies and compared our numerical results25,26,38. However, it would be beneficial to validate MR-FE derived estimates of bone failure load, along with corresponding failure criteria, reported here. Fourth, our study assessed the short-term precision errors of relatively young adults (median age: 27 years), making it difficult to generalize our results beyond the studied age group. Still, our study provides insight into MR-FE measurement precision and supports the application of MR-FE for monitoring bone strength differences. Fifth, in this study we applied short-term precision errors to estimate LSC. Glüer et al.30 though advises to use long-term precision errors (i.e., measures taken over at least 1 year) in the LSC calculation to account for factors such as scanner calibration, drift and differences in operator technique. Unfortunately (and in line with Bonnick et al.31), we found that the logistical difficulties in performing a long-term precision study, compounded with the need to apply linear regression to account for biological changes due to growth and development, made the approach unfeasible. Accordingly, it is important to be cognizant that the LSC presented here may be underestimated.
In conclusion, this study found that short-term precision errors were less than 11.8% for the two loading configurations. Precision errors ranged from 3.3% to 11.8% for regional stress and strain mean outcomes, and 5.8% to 9.0% for failure loads. This is the first study to assess the short-term in vivo precision error of MR-FE outcomes for fall and stance loading configurations at the proximal femur. Results from this study demonstrate that MR-FE outcomes are a promising non-invasive technique for monitoring femoral strength in vivo and may guide future studies in their assessment of femoral strength.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Cummings, S. R. & Melton, L. J. Epidemiology and outcomes of osteoporotic fractures. Lancet 359, 1761–1767 (2002).
U.S. Dept. of Health and Human Services, P. H. S. Bone health and osteoporosis: a report of the Surgeon General. (2003).
Kannus, P. Preventing osteoporosis, falls, and fractures among elderly people. Promotion of lifelong physical activity is essential. BMJ 318, 205–206 (1999).
Seeman, E. Pathogenesis of bone fragility in women and men. Lancet 359, 1841–1850 (2002).
Jarvinen, T. L., Sievanen, H., Khan, K. M., Heinonen, A. & Kannus, P. Shifting the focus in fracture prevention from osteoporosis to falls. BMJ 336, 124–126 (2008).
Kannus, P. et al. Effect of starting age of physical activity on bone mass in the dominant arm of tennis and squash players. Ann. Intern. Med. 123, 27–31. https://doi.org/10.7326/0003-4819-123-1-199507010-00003 (1995).
Bezakova, E., Collins, P. J. & Beddoe, A. H. Absorbed dose measurements in dual energy X-ray absorptiometry (DXA). Br. J. Radiol. 70, 172–179. https://doi.org/10.1259/bjr.70.830.9135444 (1997).
Weber, D. R. et al. The utility of DXA assessment at the forearm, proximal femur, and lateral distal femur, and vertebral fracture assessment in the pediatric population: 2019 ISCD official position. J. Clin. Densitom. 22, 567–589. https://doi.org/10.1016/j.jocd.2019.07.002 (2019).
Lochmuller, E. M., Muller, R., Kuhn, V., Lill, C. A. & Eckstein, F. Can novel clinical densitometric techniques replace or improve DXA in predicting bone strength in osteoporosis at the hip and other skeletal sites?. J. Bone Miner. Res. 18, 906–912 (2003).
Bouxsein, M. L., Coan, B. S. & Lee, S. C. Prediction of the strength of the elderly proximal femur by bone mineral density and quantitative ultrasound measurements of the heel and tibia. Bone 25, 49–54. https://doi.org/10.1016/s8756-3282(99)00093-9 (1999).
Courtney, A. C., Wachtel, E. F., Myers, E. R. & Hayes, W. C. Age-related reductions in the strength of the femur tested in a fall-loading configuration. J. Bone Joint Surg. Am. 77, 387–395. https://doi.org/10.2106/00004623-199503000-00008 (1995).
Koivumaki, J. E. et al. Cortical bone finite element models in the estimation of experimentally measured failure loads in the proximal femur. Bone 51, 737–740. https://doi.org/10.1016/j.bone.2012.06.026 (2012).
Holzer, G., von Skrbensky, G., Holzer, L. A. & Pichl, W. Hip fractures and the contribution of cortical versus trabecular bone to femoral neck strength. J. Bone Miner. Res. 24, 468–474. https://doi.org/10.1359/jbmr.081108 (2009).
Bousson, V. et al. Volumetric quantitative computed tomography of the proximal femur: Relationships linking geometric and densitometric variables to bone strength. Role for compact bone. Osteoporos. Int. 17, 855–864. https://doi.org/10.1007/s00198-006-0074-5 (2006).
Dall’Ara, E. et al. DXA predictions of human femoral mechanical properties depend on the load configuration. Med. Eng. Phys. 35, 1564–1572. https://doi.org/10.1016/j.medengphy.2013.04.008 (2013) (discussion 1564).
Manske, S. L. et al. Cortical and trabecular bone in the femoral neck both contribute to proximal femur failure load prediction. Osteoporos. Int. 20, 445–453 (2009).
Cody, D. D. et al. Femoral strength is better predicted by finite element models than QCT and DXA. J. Biomech. 32, 1013–1020. https://doi.org/10.1016/s0021-9290(99)00099-8 (1999).
Koivumaki, J. E. et al. Ct-based finite element models can be used to estimate experimentally measured failure loads in the proximal femur. Bone 50, 824–829. https://doi.org/10.1016/j.bone.2012.01.012 (2012).
Keyak, J. H., Rossi, S. A., Jones, K. A. & Skinner, H. B. Prediction of femoral fracture load using automated finite element modeling. J. Biomech. 31, 125–133. https://doi.org/10.1016/S0021-9290(97)00123-1 (1997).
Keyak, J. H. & Rossi, S. A. Prediction of femoral fracture load using finite element models: an examination of stress- and strain-based failure theories. J. Biomech. 33, 209–214. https://doi.org/10.1016/s0021-9290(99)00152-9 (2000).
Schileo, E., Balistreri, L., Grassi, L., Cristofolini, L. & Taddei, F. To what extent can linear finite element models of human femora predict failure under stance and fall loading configurations?. J. Biomech. 47, 3531–3538. https://doi.org/10.1016/j.jbiomech.2014.08.024 (2014).
Bessho, M. et al. Prediction of strength and strain of the proximal femur by a CT-based finite element method. J. Biomech. 40, 1745–1753. https://doi.org/10.1016/j.jbiomech.2006.08.003 (2007).
Khoo, B. C. et al. Comparison of QCT-derived and DXA-derived areal bone mineral density and T scores. Osteoporos. Int. 20, 1539–1545. https://doi.org/10.1007/s00198-008-0820-y (2009).
Abe, S. et al. Effect of fall direction on the lower hip fracture risk in athletes with different loading histories: A finite element modeling study in multiple sideways fall configurations. Bone 158, 116351. https://doi.org/10.1016/j.bone.2022.116351 (2022).
Abe, S. et al. Impact loading history modulates hip fracture load and location: A finite element simulation study of the proximal femur in female athletes. J. Biomech. 76, 136–143. https://doi.org/10.1016/j.jbiomech.2018.05.037 (2018).
Abe, S. et al. Exercise loading history and femoral neck strength in a sideways fall: A three-dimensional finite element modeling study. Bone 92, 9–17. https://doi.org/10.1016/j.bone.2016.07.021 (2016).
Rajapakse, C. S. et al. MRI-based assessment of proximal femur strength compared to mechanical testing. Bone 133, 115227. https://doi.org/10.1016/j.bone.2020.115227 (2020).
Chang, G. et al. Measurement reproducibility of magnetic resonance imaging-based finite element analysis of proximal femur microarchitecture for in vivo assessment of bone strength. MAGMA 28, 407–412. https://doi.org/10.1007/s10334-014-0475-y (2015).
Engelke, K. et al. Clinical use of quantitative computed tomography and peripheral quantitative computed tomography in the management of osteoporosis in adults: The 2007 ISCD Official Positions. J. Clin. Densitom. 11, 123–162. https://doi.org/10.1016/j.jocd.2007.12.010 (2008).
Gluer, C. C. Monitoring skeletal changes by radiological techniques. J. Bone Miner. Res. 14, 1952–1962. https://doi.org/10.1359/jbmr.1999.14.11.1952 (1999).
Bonnick, S. L. et al. Importance of precision in bone density measurements. J. Clin. Densitom. 4, 105–110. https://doi.org/10.1385/jcd:4:2:105 (2001).
Johnston, J. D., Liao, L., Dolovich, A. T., Leswick, D. A. & Kontulainen, S. A. Magnetic resonance imaging of bone and muscle traits at the hip: An in vivo precision study. J. Musculoskelet. Neuronal Interact. 14, 104–110 (2014).
Snehashis, R., Aaron, C., Pierre-Louis, B. & Jerry, L. P. in Proc.SPIE. 79621F.
Fedorov, A. et al. 3D Slicer as an image computing platform for the quantitative imaging network. Magn. Reson. Imaging 30, 1323–1341. https://doi.org/10.1016/j.mri.2012.05.001 (2012).
Tustison, N. J. et al. N4ITK: Improved N3 bias correction. IEEE Trans. Med. Imaging 29, 1310–1320. https://doi.org/10.1109/TMI.2010.2046908 (2010).
Fajardo, R. J., Ryan, T. M. & Kappelman, J. Assessing the accuracy of high-resolution X-ray computed tomography of primate trabecular bone by comparisons with histological sections. Am. J. Phys. Anthropol. 118, 1–10. https://doi.org/10.1002/ajpa.10086 (2002).
Spoor, C. F., Zonneveld, F. W. & Macho, G. A. Linear measurements of cortical bone and dental enamel by computed tomography: Applications and problems. Am. J. Phys. Anthropol. 91, 469–484 (1993).
Keyak, J. H., Rossi, S. A., Jones, K. A., Les, C. M. & Skinner, H. B. Prediction of fracture location in the proximal femur using finite element models. Med. Eng. Phys. 23, 657–664. https://doi.org/10.1016/s1350-4533(01)00094-7 (2001).
Besl, P. J. & McKay, N. D. A method for registration of 3-D shapes. Pattern Anal. Mach. Intell. 14, 239–256 (1992).
Hwang, S. N. & Wehrli, F. W. Estimating voxel volume fractions of trabecular bone on the basis of magnetic resonance images acquired in vivo. Int. J. Imaging Syst. Technol. 10, 186–198. https://doi.org/10.1002/(SICI)1098-1098(1999)10:2%3c186::AID-IMA9%3e3.0.CO;2-7 (1999).
Ohman, C. et al. Compressive behaviour of child and adult cortical bone. Bone 49, 769–776. https://doi.org/10.1016/j.bone.2011.06.035 (2011).
Gibson, L. J. The mechanical behaviour of cancellous bone. J. Biomech. 18, 317–328. https://doi.org/10.1016/0021-9290(85)90287-8 (1985).
Schileo, E. et al. An accurate estimation of bone density improves the accuracy of subject-specific finite element models. J. Biomech. 41, 2483–2491. https://doi.org/10.1016/j.jbiomech.2008.05.017 (2008).
Zysset, P. K., Guo, X. E., Hoffler, C. E., Moore, K. E. & Goldstein, S. A. Elastic modulus and hardness of cortical and trabecular bone lamellae measured by nanoindentation in the human femur. J. Biomech. 32, 1005–1012. https://doi.org/10.1016/s0021-9290(99)00111-6 (1999).
de Bakker, P. M. et al. During sideways falls proximal femur fractures initiate in the superolateral cortex: Evidence from high-speed video of simulated fractures. J. Biomech. 42, 1917–1925. https://doi.org/10.1016/j.jbiomech.2009.05.001 (2009).
Edwards, W. B. & Troy, K. L. Finite element prediction of surface strain and fracture strength at the distal radius. Med. Eng. Phys. 34, 290–298. https://doi.org/10.1016/j.medengphy.2011.07.016 (2012).
Hoffman, O. The brittle strength of orthotropic materials. J. Composite Mater. 1, 200–206. https://doi.org/10.1177/002199836700100210 (1967).
Kheirollahi, H. & Luo, Y. Assessment of hip fracture risk using cross-section strain energy determined by QCT-based finite element modeling. Biomed. Res. Int. 2015, 413839. https://doi.org/10.1155/2015/413839 (2015).
Evans, F. G. & Vincentelli, R. Relations of the compressive properties of human cortical bone to histological structure and calcification. J. Biomech. 7, 1–10. https://doi.org/10.1016/0021-9290(74)90064-5 (1974).
Morgan, E. F. & Keaveny, T. M. Dependence of yield strain of human trabecular bone on anatomic site. J. Biomech. 34, 569–577. https://doi.org/10.1016/s0021-9290(01)00011-2 (2001).
Zani, L., Erani, P., Grassi, L., Taddei, F. & Cristofolini, L. Strain distribution in the proximal Human femur during in vitro simulated sideways fall. J. Biomech. 48, 2130–2143. https://doi.org/10.1016/j.jbiomech.2015.02.022 (2015).
Gluer, C. C. et al. Accurate assessment of precision errors: How to measure the reproducibility of bone densitometry techniques. Osteoporos. Int. 5, 262–270 (1995).
Arjmand, H. et al. Mechanical metrics of the proximal tibia are precise and differentiate osteoarthritic and normal knees: A finite element study. Sci. Rep. 8, 11478. https://doi.org/10.1038/s41598-018-29880-y (2018).
Courtney, A. C., Wachtel, E. F., Myers, E. R. & Hayes, W. C. Effects of loading rate on strength of the proximal femur. Calcif. Tissue Int. 55, 53–58. https://doi.org/10.1007/BF00310169 (1994).
Pinilla, T. P., Boardman, K. C., Bouxsein, M. L., Myers, E. R. & Hayes, W. C. Impact direction from a fall influences the failure load of the proximal femur as much as age-related bone loss. Calcif. Tissue Int. 58, 231–235. https://doi.org/10.1007/BF02508641 (1996).
Russell, G. V. Jr., Kregor, P. J., Jarrett, C. A. & Zlowodzki, M. Complicated femoral shaft fractures. Orthop. Clin. North Am. 33, 127–142. https://doi.org/10.1016/s0030-5898(03)00076-2 (2002).
Sheehan, S. E., Shyu, J. Y., Weaver, M. J., Sodickson, A. D. & Khurana, B. Proximal femoral fractures: What the orthopedic surgeon wants to know. RadioGraphics 35, 1563–1584. https://doi.org/10.1148/rg.2015140301 (2015).
Acknowledgements
Financial support to conduct the study was provided by the Canadian Institute of Health Research (CIHR) (Grant MOP98002; SAK) as well as the Natural Sciences and Engineering Research Council (NSERC) (Discovery Grant RGPIN-2016-05301 (SAK) and RGPIN-2015-06420 (JDJ)). We thank study participants.
Funding
Canadian Institutes of Health Research (CIHR); Natural Sciences and Engineering Research Council (NSERC).
Author information
Authors and Affiliations
Contributions
K.B.M. was jointly responsible for performing the image analyses, finite element analysis, data analysis, statistical analyses, data interpretation, and drafted the manuscript. S.A.K. assisted with statistical analyses and was jointly responsible for the original ideas and was a key editor. D.A.L. was involved in the original study design and assisted in the image analysis. A.T.D. assisted with the precision analyses and was a key editor. J.D.J. was jointly responsible for the original ideas, image analysis, data analysis, and was a key editor. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Majcher, K.B., Kontulainen, S.A., Leswick, D.A. et al. Magnetic resonance imaging based finite element modelling of the proximal femur: a short-term in vivo precision study. Sci Rep 14, 7029 (2024). https://doi.org/10.1038/s41598-024-57768-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-57768-7
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.