Abstract
Obesity can lead to cardiovascular dysfunctions and cause electrocardiographic disruptions. Bariatric surgery plays a significant role in weight loss. To assess its benefits, this study investigated electrocardiographic changes before and after bariatric surgery. The present article describes a retrospective cohort study with a 6-month follow-up period. Electrocardiograms were interpreted and compared before and six months after surgery. The relationships between weight loss, type of surgery, and electrocardiographic alterations were analyzed. A total of 200 patients participated in the study, with 34 (17%) men and 166 (83%) women. The mean age of the participants was 44.6 ± 8.6, and their mean body mass index was 43.8 ± 5.5 kg/m2. The mean of QTc decreased after the surgery, while the Sokolow-Lyon scores increased. The statistical analysis showed that QTc dispersion (> 40) (P < 0.001), right ventricular hypertrophy (P < 0.001), abnormal R wave progression (P < 0.001), QTc (P < 0.001) and Sokolow-Lyon criteria (P < 0.001) significantly changed postoperatively. In conclusion, bariatric surgery can reduce QTc, correct poor R wave progression, and resolve right ventricular hypertrophy (RVH) in patients with morbid obesity.
Similar content being viewed by others
Introduction
Obesity, the souvenir of modern lifestyle, has become a major universal concern in recent years. The prevalence of obesity has surpassed one billion worldwide. According to the World Health Organization (WHO), it is estimated that more than 167 million people worldwide will struggle with health issues due to obesity by 20251,2. Obesity is defined as a body mass index (BMI) > 30 kg/m2 and can cause a greater risk of diabetes, hypertension, and hyperlipidemia, which results in more cardiovascular events3. A recent study reported that almost three million people die from obesity-induced cardiovascular diseases annually4. Furthermore, studies have shown that obesity affects cardiac electrophysiology directly by changing the heart’s structure3,5,6. Excess visceral adipocytes trigger the secretion of “adipokines”, which can lead to myocardial hypertrophy3. Hypertension secondary to obesity can also promote left ventricle hypertrophy (LVH); however, LVH is also observed in normotensive severely obese patients7,8. Cardiac morphologic changes can result in electrocardiographic alterations such as QTc dispersion, P-wave, and QTc prolongation3. The QT interval or corrected QT (QTc), an indicator of ventricular repolarization, has been reported to be prolonged in patients with obesity9,10. Studies have shown that long QTc is associated with fatal arrhythmias and sudden cardiac death11,12.
Moreover, changes in heart structure can lead to serious heart problems, such as atrial fibrillation (AF). Weight loss can significantly improve diabetes, dyslipidemia, and cardiovascular complications13. However, studies have shown that primary weight loss methods such as lifestyle modifications and dietary vigilance are ineffective in the long term. Some studies have shown that these techniques have limited long-term utility in maintaining weight loss and have no significant impact on the incidence of cardiovascular events. Therefore, surgical strategies for overcoming the medical and habitual methods are needed to address obesity-related complications3,5,14,15. Studies revealed that patients struggling with obesity succeeded in losing up to 60% of their extra body weight16. Several bariatric surgeries, such as sleeve gastrectomy and classic bypass, are commonly performed. These surgeries can lead to significant improvements in heart failure, coronary artery disease, and cardiac rhythm abnormalities17,18,19.
Our study aimed to evaluate the impact of bariatric surgeries on electrocardiography and to determine whether surgical weight loss methods are beneficial for correcting obesity-related problems.
Results
Demographics
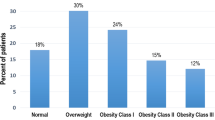
The study included 200 patients, 166 (83%) of whom were female. The mean age of the population was 44.6 ± 8.6 years. Most participants were between 25 and 60 years of age; no one was younger than 25 years, and only two patients were above this range. The majority of the patients were severely obese (BMI > 40 kg/m2), and the mean BMI among the patients was 43.8 ± 5.5 kg/m2. Table 1 provides a detailed overview of the demographic and baseline characteristics of the participants.
Electrocardiographic alterations
Table 2 shows the ECG changes observed before and after surgery. The table shows that bariatric procedures significantly improved R wave progression (60 versus 27, P < 0.001), corrected RVH (63 versus 18, P < 0.001), reduced QTc dispersion (139 versus 35, P < 0.001), shortened the QTc interval (443.9 versus 409.7, P < 0.001), and increased the Sokolow-Lyon score (15 versus 17.17, P < 0.001).
Correlations and regression analysis
We examined whether the demographic and anthropometric factors and the type of bariatric surgery impacted postoperative changes. We conducted a multiple regression analysis for QTc and the Sokolow-Lyon score. However, none of the dependent variables significantly affected either of these parameters. We used binary logistic regression to analyze the relationships between dichotomous variables such as QTc dispersion, RVH, and abnormal R wave progression. Only the type of bariatric procedure significantly predicted abnormal R wave progression (OR: 0.434, P = 0.025). Tables 3 and 4 demonstrate the results of the regression analysis in detail.
Discussion
Obesity is a well-known risk factor for various cardiac complications. Therefore, weight is an essential intervention in managing these conditions. Studies have shown that while any weight loss method can improve cardiac function and lower the risk of cardiovascular events13, surgical methods provide the best short-term and long-term benefits compared to pharmacological treatments and lifestyle modifications3.
In the current study, we aimed to evaluate the effects of bariatric surgery on ECG alterations during a 6-month follow-up period. The most common preoperative abnormality was QTc dispersion in 69.5% of participants, followed by RVH and abnormal R wave progression in 31.5% and 30% of the participants, respectively. However, all three abnormalities were significantly improved after bariatric surgery (P < 0.001). The mean QTc duration was 443.9 ± 23.4 ms, which markedly decreased to 409.7 ± 20.5 ms after the 6-month follow-up (P < 0.001). Our findings suggest that weight loss achieved through bariatric surgery significantly shortened the QTc duration, improved QTc dispersion and RVH and corrected R wave progression (Table 2). The Sokolow-Lyon criteria indicate LVH if the score exceeds 35. Our findings revealed that the score significantly increased after the surgery. This could be explained by the fact that after surgery, patients experienced weight loss, leading to less subcutaneous fat, better positioning of the heart in the thorax, and lower afterload pressure in the left ventricle, which can result in improved left ventricle function. However, although the Sokolow-Lyon score increased, none of the participants developed LVH within the 6-month follow-up period.
A regression analysis was conducted to predict ECG improvements based on sex, age, BMI, and type of surgery, as presented in Table 3. None of these variables had any statistically significant impact on the ECG. However, a statistically meaningful relationship was found between the type of surgery and abnormal R wave progression. Regression analysis revealed that sleeve gastrectomy was less effective than classic bypass in correcting abnormal R wave progression (OR:0.434, P = 0.025). The binomial logistic regression model was statistically significant (χ2(4):10.619; P = 0.031). The model explained 8.5% (Nagelkerke R2) of the variance in abnormal R wave progression and correctly classified 78.8% of the cases. The reason for these improvements lies in the hormonal and autonomic consequences of bariatric surgeries. Previous studies have shown that insulin resistance (IR) is one of the leading causes of prolonged QTc and QT dispersion6,20,21,22,23,24,25. Insulin has been found to hyperpolarize both excitable and nonexcitable cells, and can directly prolong the QT interval26. Excess insulin can indirectly cause QTc prolongation by inducing a hyperkalemic state, which is a known cause of this abnormality27. Moreover, higher doses and prolonged periods of hyperinsulinemia can result in increased release of catecholamines, leading to increased blood pressure. Over time, hypertension caused by elevated catecholamine release can cause left ventricle hypertrophy. Studies have suggested that an increased left ventricle mass is one of the most important causes of rhythm abnormalities, particularly QT prolongation28,29. Significant weight loss is the second most important cause of ECG changes after bariatric surgery. One study showed that individuals lose approximately 25%-30% of their initial weight or achieve 50%-70% excess weight loss after a successful surgery30. This substantial weight loss results in various cardiovascular changes31. These include a decrease in BMI, which can lead to lower blood pressure, reduced preload, and a decrease in ventricle mass in the long-term. Recent studies have shown that a prolonged QT interval is related to obstructive sleep apnea and sympathetic nervous system activation5,7,14,32. Losing weight by any means is expected to improve obstructive sleep apnea and reduce sympathetic activation, resulting in a normalized QT interval.
Our research findings support previously published articles on the effects of bariatric surgery on patients with obesity. Pontiroli et al.33 conducted a study on 116 patients with obesity who underwent bariatric surgery. They found that LVH and QT prolongation were common prior to surgery. However, one year after the surgery, the QTc decreased in all patients (P < 0.05), and LVH was resolved in the majority of the participants (P = 0.0025). In a similar study, Al-Salameh et al.34 assessed 28 patients who underwent sleeve gastrectomy and compared QTc changes three months after the operation. They discovered an average decrease of 28.46 ± 15.61 ms in the QTc within the first three months after the surgery (P < 0.0001). Notably, no statistically significant correlation was found between weight loss and decreased QTc34.
In a study conducted by Bezante et al.31 85 individuals with severe obesity were examined in a case–control setting. Of these, 55 people underwent biliopancreatic diversion, while the remaining 30 were in the control group. The researchers found a significant reduction in QTc and QT dispersion after the operation (P < 0.0001). However, they discovered no correlation between weight loss percentage and QTc changes. They concluded that normalizing ventricular rhythm abnormalities is much more responsive to serum glucose and insulin levels than to absolute weight loss31.
We must acknowledge that our study had a few limitations to consider. First, we did not measure weight loss or postoperative BMI percentage in our study group. These measurements are crucial for understanding the correlation between the amount of weight loss and the QTc in the short term. Second, we need laboratory data such as glucose, insulin, and lipid profiles to make our study more comprehensive. By comparing these values, we could identify further correlations and insights.
Finally, we conclude that bariatric surgeries can correct abnormal R wave progression and resolve QT dispersion in morbidly obese patients. The QTc interval significantly decreased within six months postoperatively. Given the positive impact on the cardiovascular system, bariatric surgery can be a practical and beneficial choice for morbidly obese patients who are struggling with cardiac complications.
Methods
Ethics statement
The study was carried out in accordance with the principles of the Declaration of Helsinki. All authors confirm that all methods were performed in accordance with the relevant guidelines and regulations. The study started after approval from the Shiraz University of Medical Sciences Ethics Committee (approval ID: IR.SUMS.MED.REC.1401.056, approval date: 2022.05.01). The patients undergoing bariatric surgery had to provide written informed consent that informed them of the potential risks during and after the surgery. Patients agreed to participate in a long-term follow-up after the surgery.
Population and study design
In the current cohort, we included 200 patients who underwent bariatric surgery at Mother and Child Hospital in Shiraz, Iran, from April 2020 to March 2021. We used the census method to determine the study population size and enrolled 500 patients admitted for bariatric operations. Ultimately, 200 patients met the inclusion criteria: were candidates for bariatric surgery, had complete medical records, and provided informed consent. Patients who did not consent to participate or had incomplete medical records were excluded from the survey. The patient selection, exclusions, and inclusions are shown in Fig. 1.
We collected demographic information, past medical histories, and intraoperative and postoperative data from the patients' medical records using a prepared checklist. The criteria for bariatric surgeries include the following:
-
1.
BMI > 40 kg/m2,
-
2.
BMI > 35 kg/m2 accompanied by a significant risk factor, e.g., diabetes and hypertension,
-
3.
Poor response to primary weight loss methods, such as exercise, diet, and medical approaches.
Exclusion criteria were considered to remove variables that may bias the results and hamper a clear safety assessment for both patients and researchers. The following exclusion criteria were then applied (Fig. 1):
-
1.
Aged under 18 and over 65,
-
2.
Prior to bariatric procedures,
-
3.
Loss to follow-ups,
-
4.
Contraindicating medical conditions such as advanced heart disease, unmanaged mental health disorders, or end-stage organ diseases,
-
5.
Individuals who reported medical interference, who were taking medications that could significantly influence weight or interact with surgical procedures or who experienced postoperative recovery were excluded.
The patients were then divided into two groups based on the type of bariatric surgery they received: sleeve gastrectomy and classic bypass. An electrocardiogram was obtained before the surgery and six months postoperatively. An expert cardiologist blindly interpreted and compared the ECGs before and after surgery.
Statistical analysis
Continuous variables are reported as the mean ± SD, while quantitative values are reported as the frequency. To check normality, we used Shapiro–Wilk and Kolmogorov–Smirnov tests and related histograms. We used a paired t-test to compare the means for normally distributed variables, while nonparametric tests were performed for nonnormally distributed values. To analyze categorical data, we conducted a chi-square test. We also ran multiple and binary logistic regression analyses to predict possible correlations between variables. We considered p-values less than 0.05 to indicate statistical significance. The data were analyzed using SPSS version 23.
Data availability
The ethnical appendix, statistical code, and dataset are available based on requests sent to the corresponding author.
References
Organization, W.H. World Obesity Day 2022: Accelerating Action to Stop Obesity. https://www.who.int/news/item/04-03-2022-world-obesity-day-2022-accelerating-action-to-stopobesity#:~:text=More%20than%201%20billion%20people,adolescents%20and%2039%20million%20children (2022).
Papaioannou, A. et al. Effects of weight loss on QT interval in morbidly obese patients. Obes. Surg. 13, 869–873 (2003).
Vest, A. R., Heneghan, H. M., Agarwal, S., Schauer, P. R. & Young, J. B. Bariatric surgery and cardiovascular outcomes: A systematic review. Heart 98, 1763–1777 (2012).
Ford, E. S., Giles, W. H. & Dietz, W. H. Prevalence of the metabolic syndrome among US adults: Findings from the third National Health and Nutrition Examination Survey. Jama 287(3), 356–359 (2002).
Lascaris, B. et al. Cardiac structure and function before and after bariatric surgery: A clinical overview. Clin. Obes. 8, 434–443 (2018).
Lavie, C. J. et al. Obesity and prevalence of cardiovascular diseases and prognosis—the obesity paradox updated. Prog. Cardiovasc. Dis. 58, 537–547 (2016).
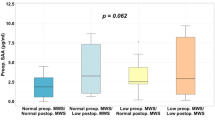
Alpert, M. A. et al. Effect of weight loss on ventricular repolarization in normotensive severely obese patients with and without heart failure. Am. J. Med. Sci. 349, 17–23 (2015).
Gulizia, M. M. et al. ANMCO/AIIC/SIT Consensus Information Document: Definition, precision, and suitability of electrocardiographic signals of electrocardiographs, ergometry, Holter electrocardiogram, telemetry, and bedside monitoring systems. Eur. Heart J. Suppl. 19, D190–D211 (2017).
Russo, V. et al. Effect of weight loss following bariatric surgery on myocardial dispersion of repolarization in morbidly obese patients. Obes. Surg. 17, 857–865 (2007).
Arslan, E., Yığıner, Ö., Yavaşoğlu, İ, Kardeşoğlu, E. & Nalbant, S. Effect of uncomplicated obesity on QT interval in young men. Polis. Arch. Intern. Med. 120, 209–213 (2010).
Steinberg, J. S. et al. 2017 ISHNE-HRS expert consensus statement on ambulatory ECG and external cardiac monitoring/telemetry. Heart Rhythm 14, e55–e96 (2017).
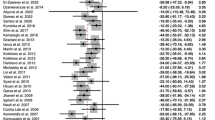
Sanches, E. E. et al. Effects of bariatric surgery on heart rhythm disorders: A systematic review and meta-analysis. Obes. Surg. 31, 2278–2290 (2021).
Sjöström, L. et al. Bariatric surgery and long-term cardiovascular events. Jama 307, 56–65 (2012).
Pouwels, S. et al. Interaction of obesity and atrial fibrillation: An overview of pathophysiology and clinical management. Expert Rev. Cardiovasc. Ther. 17, 209–223 (2019).
Omran, J., Firwana, B., Koerber, S., Bostick, B. & Alpert, M. Effect of obesity and weight loss on ventricular repolarization: A systematic review and meta-analysis. Obes. Rev. 17, 520–530 (2016).
Delville, M. et al. Prevalence and predictors of early cardiovascular events after kidney transplantation: Evaluation of pre-transplant cardiovascular work-up. PLoS ONE 10, e0131237 (2015).
Persson, C. E. et al. Risk of heart failure in obese patients with and without bariatric surgery in Sweden: A registry-based study. J. Cardiac Failure 23, 530–537 (2017).
Benotti, P. N. et al. Gastric bypass surgery produces a durable reduction in cardiovascular disease risk factors and reduces the long-term risks of congestive heart failure. J. Am. Heart Assoc. 6, e005126 (2017).
Douglas, I. J., Bhaskaran, K., Batterham, R. L. & Smeeth, L. Bariatric surgery in the United Kingdom: A cohort study of weight loss and clinical outcomes in routine clinical care. PLoS Med. 12, e1001925 (2015).
Dekker, J. M., Schouten, E. G., Klootwijk, P., Pool, J. & Kromhout, D. Association between QT interval and coronary heart disease in middle-aged and elderly men. The Zutphen Study. Circulation 90, 779–785 (1994).
Gryglewska, B., Grodzicki, T., Czarnecka, D., Kaweoicka-Jaszcz, K. & Kocemba, J. QT dispersion and hypertensive heart disease in the elderly. J. Hypertens. 18, 461–464 (2000).
Clarkson, P. B. et al. QT dispersion in essential hypertension. QJM 88, 327–332 (1995).
Bastien, M., Poirier, P., Lemieux, I. & Després, J.-P. Overview of epidemiology and contribution of obesity to cardiovascular disease. Prog. Cardiovasc. Dis. 56, 369–381 (2014).
Cavallini, B., Perri, V. & Sali, M. Dispersion of QT interval in arterial hypertension with left ventricular hypertrophy. Minerva Cardioangiol. 44, 45–48 (1996).
Salles, G., Cardoso, C. & Deccache, W. Multivariate associates of QT interval parameters in diabetic patients with arterial hypertension: Importance of left ventricular mass and geometric patterns. J. Hum. Hypertens. 17, 561–567 (2003).
Ferrannini, E. et al. Insulin: New roles for an ancient hormone. Eur. J. Clin. Investig. 29, 842–852 (1999).
Li, S.-H. et al. Impaired atrial synchronicity in patients with metabolic syndrome associated with insulin resistance and independent of hypertension. Hypertens. Res. 32, 791–796 (2009).
Kanoupakis, E. et al. Left ventricular function and cardiopulmonary performance following surgical treatment of morbid obesity. Obes. Surg. 11, 552–558 (2001).
Mukerji, R. et al. Effect of weight loss after bariatric surgery on left ventricular mass and ventricular repolarization in normotensive morbidly obese patients. Am. J. Cardiol. 110, 415–419 (2012).
Alfadda, A. A. et al. Long-term weight outcomes after bariatric surgery: A single Center Saudi Arabian cohort experience. J. Clin. Med. 10, 4922 (2021).
Bezante, G. P. et al. Biliopancreatic diversion reduces QT interval and dispersion in severely obese patients. Obesity 15, 1448–1454 (2007).
Gillis, A. M., Stoohs, R. & Guilleminault, C. Changes in the QT interval during obstructive sleep apnea. Sleep 14, 346–350 (1991).
Pontiroli, A. et al. Left ventricular hypertrophy and QT interval in obesity and in hypertension: Effects of weight loss and of normalisation of blood pressure. Int. J. Obes. 28, 1118–1123 (2004).
Al-Salameh, A., Allain, J., Jacques, A., Verhaeghe, P. & Desailloud, R. Shortening of the QT interval is observed soon after sleeve gastrectomy in morbidly obese patients. Obes. Surg. 24, 167–170 (2014).
Acknowledgements
We appreciate the help of participants and hospital staff in this study. Figure 1. was created by Soroush Nematollahi using Microsoft PowerPoint.
Author information
Authors and Affiliations
Contributions
H.BD. developed the idea and designed the study; M.B., N.N., and A.F. gathered the data; H.B. and N.M. checked the data and prepared them for analysis; S.N. and M.KHA. analyzed the data; S.N. wrote the manuscript and prepared it for submission. M.K., S.N., M.B. revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bazrafshan, M., Nematollahi, S., Kamali, M. et al. Bariatric surgery mitigated electrocardiographic abnormalities in patients with morbid obesity. Sci Rep 14, 6710 (2024). https://doi.org/10.1038/s41598-024-57155-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-57155-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.