Abstract
There is no current consensus on the follow up of kidney function in patients undergoing cardiopulmonary bypass (CPB). The main objectives of this pilot study is to collect preliminary data on kidney function decline encountered on the first postoperative visit of patients who have had CPB and to identify predictors of kidney function decline post hospital discharge. Design: Retrospective chart review. Adult patients undergoing open heart procedures utilizing CPB. Patient demographics, type of procedure, pre-, intra-, and postoperative clinical, hemodynamic echocardiographic, and laboratory data were abstracted from electronic medical records. Acute kidney disease (AKD), and chronic kidney disease (CKD) were diagnosed based on standardized criteria. Interval change in medications, hospital admissions, and exposure to contrast, from hospital discharge till first postoperative visit were collected. AKD, and CKD as defined by standardized criteria on first postoperative visit. 83 patients were available for analysis. AKD occurred in 27 (54%) of 50 patients and CKD developed in 12 (42%) out of 28 patients. Older age was associated with the development of both AKD and CKD. Reduction in right ventricular cardiac output at baseline was associated with AKD (OR: 0.5, 95% CI: 0.3, 0.79, P = 0.01). Prolongation of transmitral early diastolic filling wave deceleration time was associated with CKD (OR: 1.02, 95% CI: 1.01, 1.05, P = 0.03). In-hospital acute kidney injury (AKI) was a predictor of neither AKD nor CKD. AKD and CKD occur after CPB and may not be predicted by in-hospital AKI. Older age, right ventricular dysfunction and diastolic dysfunction are important disease predictors. An adequately powered longitudinal study is underway to study more sensitive predictors of delayed forms of kidney decline after CPB.
Similar content being viewed by others
Introduction
Cardiac surgery requiring cardiopulmonary bypass (CPB) is a common cause of acute kidney injury (AKI). Even milder forms of AKI may progress to chronic kidney disease (CKD) and are associated with increased mortality and morbidity1,2.
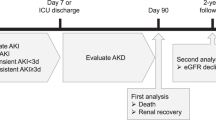
The Kidney Disease Improving Global Outcomes (KDIGO) defines AKI as an abrupt decrease in kidney function that occurs over the course of 7 days or less and CKD as abnormalities in kidney structure that persist over > 90 days. The term acute kidney disease (AKD) has been proposed to define ongoing processes that bridge the progression of AKI to CKD. AKD is defined as acute or subacute damage and/or loss of kidney structure for a duration > 7 days yet < 90 days after an AKI precipitating event3.
Caveats exist in the current KDIGO criteria that may influence the postoperative course and care of patients undergoing CPB. For example, patients may not manifest an AKI during their hospital course yet present with a kidney function decline at the first follow up visit. In such an instance, it is unknown whether these patients manifest a new onset AKI or an AKD from an ongoing injury that has not manifested during hospital discharge. Furthermore, waiting for 90 days to fulfill criteria for CKD may expose these patients to further irreversible kidney damage. The picture becomes more confusing in the absence of a consensus on the follow up of patients who do not manifest in-hospital AKI.
To remedy this gap in the less studied delayed forms of kidney decline post CPB4,5,6, we report our preliminary data on kidney function at the first postoperative visit in a cohort of our patients who have undergone CPB7. Our secondary objective is to assess predictors of kidney function decline at first postoperative visit.
Discussion
In this pilot study we demonstrate a delayed pattern of postoperative kidney dysfunction that is not predicted by baseline kidney function nor by postoperative acute kidney injury and that is not explained by factors known to precipitate a new onset kidney injury. Age is a common predictor of AKD and CKD. Right ventricular (RV) dysfunction is a predictor of AKD. Prolonged deceleration time is a predictor of CKD.
Our study is in alignment with other studies that demonstrate a continuum of kidney decline in the cardiac surgical setting8,9,10,11,12,13. Matsuura et al.13 published a study demonstrating an association between AKD and 90-day mortality and 2-year decline in eGFR. Compared to our study, Matsuura et al.’s was a much larger study and studied outcomes over a longer period of observation. Our study, on the other hand, reported AKD and CKD as outcomes and reported predictors on their association Compared with the study by Legouis et al.4, our study did not demonstrate and association of AKD and CKD with postoperative AKI. This contradiction might be attributed to the more patients with advanced stages of AKI in Legouis et al. study compared to ours. Also we measured eGFR as a change from baseline compared to Legouis et al.’s study that defined CKD based on an absolute reduction in eGFR4 below 60 mL/min/1.73 m2. Our study is in line with others that emphasized age as an independent risk factor for AKI postoperatively14,15,16. Whereas age is an important predictor of AKI, its role in more chronic forms of kidney disease is debatable11,17. The ‘natural’ decline of eGFR with aging may overestimate the incidence of CKD or progressive kidney disease occurring in this population. Our study contradicts with other studies that demonstrate age-adjusted eGFR is not associated with progression, or even may be associated with regression of CKD18,19. In contradistinction of these population studies that followed medical volunteers, our study was performed on surgical patients within the realm of an acute insult to the kidneys. We speculate that the non-physiologic state of CPB might have accentuated a steady ongoing nephron loss process occurring in the elderly. As such, an acute insult may overcome the organ reserve of the elderly leading to renal functional deterioration20. Whether this decline in eGFR is a progressive versus a regressive, remains to be proven. This study is in line with a larger study by the same principal investigator that demonstrated an incidence of 20% of postoperative long-term kidney decline in patients without postoperative AKI undergoing endovascular aortic aneurysm repair21. Despite a comparatively higher proportion of patients with postoperative long-term kidney decline who developed postoperative AKI, a 20% is not an insignificant percent. Despite the dissimilarity in the surgical setting, the similarities in the surgical population between cardiac and vascular surgical population warrant the search for more sensitive markers that can differentiate acute from chronic kidney disease. It is important to highlight that we did not stratify eGFR and that we did not follow up these patients to determine the course of disease progression. Equally important, it remains to be determined how elderly patients who are at risk of being impacted by CPB in terms of comorbidities, intraoperative hemodynamics and other factors that affect renal function under CPB22.
The absence of a new insult known to precipitate AKI leads us to speculate a subacute ongoing mechanism of kidney dysfunction commencing with surgery that is unrecognized by insensitive markers of AKI currently in use. The association of kidney disease with a reduction in RV CO and with prolonged deceleration time with the latter being a marker of diastolic dysfunction, proposes a forward hypoperfusion and backward congestive mechanisms to kidney disease, respectively. Important to appreciate that our study was not adequately powered to study predictors of kidney decline. Therefore, these findings remain hypothesis generating at the current stage.
Our study is in line with others that recognize AKD after cardiac surgery13. Yet, we differ than those that demonstrated AKD as an extension of AKI or of baseline CKD.
Small sample size and lack of long-term follow up stand as limitations of our study. The small sample size represents real world circumstances where there is no consensus on following up of renal function post hospital discharge. Furthermore, lack of data on urine output and proteinuria may have altered the results. Yet, this might have resulted in diagnosing more cases with kidney function decline.
In summary, this exploratory study demonstrates that CBP-requiring cardiac surgery is associated with delayed patterns of kidney function decline. As such, these patterns, while may deviate from current standardized definitions, are important potential therapeutic targets. An adequately powered longitudinal study is under way to elucidate more sensitive in-hospital predictors of delayed kidney function decline in patients undergoing CPB.
Results
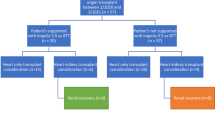
The original cohort consisted of 120 patients who were analyzed for volume responsiveness7. Of these, 36 patients (28%) developed AKI. Of the original 120 patients only 83 patients had postoperative serum creatinine or eGFR value recorded after hospital discharge (Fig. 1). Characteristics of patients who developed and those who did not develop AKD, and CKD are summarized in Table 1. Older age was associated with the development of AKD and CKD. Reduction in eGFR from baseline averaged 4 mL/min/1.73 m2 and 6 mL/min/1.73 m2 in the first 90 days (Fig. 2) and between 91–365 days, respectively (Fig. 3).
(A) A box-and-whisker plots conveys the distribution of 90-day eGFR changes (defined as the difference between the lowest eGFR measurement within 90 days of discharge and the baseline eGFR). The average change is − 4.09 mL/min/1.73 m2. The median change is − 6.40 mL/min/1.73 m2. (B) A box-and-whisker plots conveys the distribution of 90-day creatinine changes (defined as the difference between the lowest creatinine measurement within 90 days of discharge and the baseline creatinine). The average change is − 0.07 mg/dL. The median change is 0.10 mg/dL.
(A) A box-and-whisker plots conveys the distribution of 91-to-365-day eGFR changes (defined as the difference between the lowest eGFR measurement between 91 and 365 days of discharge and the baseline eGFR). The average change is − 5.94 mL/min/1.73 m2. The median change is 0 mL/min/1.73 m2. (B) A box-and-whisker plots conveys the distribution of 91-to-365-day creatinine changes (defined as the difference between the lowest creatinine measurement between 91 and 365 days of discharge and the baseline creatinine). The average change is − 0.06 mg/dL. The median change is 0 mg/dL.
No significant differences existed between those who developed and those who did not develop either of AKD and CKD in terms of preoperative eGFR, exposure to medications known to affect perioperative kidney function, the distribution of comorbidities, or average severity scores during hospital stay, average serum lactate for their hospital stay, cross clamp time and duration on CPB. Coronary artery bypass grafting was the most frequent procedure with no difference between those who developed and those who did not develop AKD and CKD (data not shown). There were no significant differences between those who developed and those who did not develop each of AKD and CKD in the incidence of postoperative AKI (Supplementary Tables 1, 2).
Multi-stage logistic regression demonstrated age and increased right ventricular cardiac output prior to institution of CPB to independently predict AKD. On the other hand, age and prolonged deceleration time were independently associated with CKD (Tables 2 and 3). Deceleration time refers to the time taken form the peak velocity of the early filling waveform (E wave) to baseline as measure by spectral Doppler23.
Methods
This is a retrospective chart review. The study is an extension of our published retrospective study reporting on the association of end of procedure volume responsiveness and AKI7. The original study focused on patients who developed AKI during their hospital stay. Comparatively, the current study focuses on patients after their hospital discharge and on more delayed forms of kidney function decline after CPB-requiring procedures. The study was approved by the Institutional Review Board (IRB#150508005) of The University of Alabama At Birmingham (UAB) and adhered to the Declaration of Helsinki Informed written consent was obtained from all patients participating in this study in accordance with regulatory standards. Adult patients undergoing open heart procedures utilizing CPB were enrolled in the study. Patients < 19 years old, those with estimated glomerular filtration rate (eGFR) < 30 mL/kg/min2, transplanted patients, patients with preoperative ejection fraction < 30%, and patients undergoing mechanical assist device placement, off pump coronary artery bypass grafting or percutaneous valve interventions were excluded from the study. The authors complied with STROBE Guidelines on reporting cohort studies. A study flow chart is shown in Fig. 1.
Data collection
Patient demographics, type of procedure, pre-, intra-, and postoperative clinical, hemodynamic echocardiographic, and laboratory data were routinely collected and abstracted from electronic medical records (EMR) for up to 7 days of hospital stay and at the first post discharge clinic visit. Acute kidney injury, and chronic kidney disease (CKD) were diagnosed based on KDIGO standardized criteria for serum creatinine and eGFR, respectively24. Intraoperative transesophageal echocardiography was performed pre- immediately post- CPB and at chest closure. Kidney function was assessed on the first postoperative visit up to 1 year and was stratified as within the first 90 days (acute kidney disease, AKD) versus 91–365 days post hospital discharge (chronic kidney disease, CKD). Interval change in medications, hospital admissions, and exposure to contrast, from hospital discharge till first postoperative visit were collected from EMR. Patients who were exposed to any of the aforementioned insults were excluded from the analysis.
Outcomes
The primary outcome was development of AKD and CKD as defined by KDIGO standardized criteria for serum creatinine and eGFR on first postoperative visit3.
Statistical analysis
Given the exploratory nature of the study, no power calculation was performed. For binary variables, Chi-squared test was used to investigate the association between each covariate and kidney disease. The Student’s t-test and the Wilcoxon rank sum test were used to compare independent continuous variables between a patient with and without kidney disease for normally and non- normally distributed variables, respectively. Univariable logistic regression models were used to investigate the association between each covariate and kidney disease. Any covariate that was significant at P < 0.05 was then entered into a multivariable model. Variables with high Variance Inflation Factor (VIF > 4) were removed to avoid collinearity. Additionally, variables with more than 25% missingness were excluded from the multivariate model. Logistic regressions, t-tests, and Pearson's Chi-squared tests with Yates’ continuity correction were conducted in R version 4.0.2.
Institutional review board statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of UNIVERSITY OF ALABAMA (protocol code #150508005, 9/25/2017).”
Informed consent
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from all participating patients to publish this paper.
Data availability
Data used and/or analyzed in this study will be available upon a reasonable request from the first author according to institutional guidelines for data sharing.
Abbreviations
- CS-KD:
-
Cardiac surgery related kidney dysfunction
- CPB:
-
Cardiopulmonary bypass
- IRB:
-
Institutional Review Board
- UAB:
-
University of Alabama
- EMR:
-
Electronic medical records
- AKD:
-
Acute kidney disease
- CKD:
-
Chronic kidney disease
- AKI:
-
Acute kidney injury
- KDIGO:
-
Kidney Disease Improving Global Outcomes
- VIF:
-
Variance inflation factor
References
Li, P. K., Burdmann, E. A., Mehta, R. L., World Kidney Day Steering Committee. Acute kidney injury: Global health alert. Curr. Opin. Nephrol. Hypertens. 22(3), 253–258 (2013).
Coca, S. G., Singanamala, S. & Parikh, C. R. Chronic kidney disease after acute kidney injury: A systematic review and meta-analysis. Kidney Int. 81(5), 442–448 (2012).
Chawla, L. S. et al. Acute kidney disease and renal recovery: Consensus report of the Acute Disease Quality Initiative (ADQI) 16 Workgroup. Nat. Rev. Nephrol. 13(4), 241–257 (2017).
Legouis, D. et al. Development of a practical prediction score for chronic kidney disease after cardiac surgery. Br. J. Anaesth. 121(5), 1025–1033 (2018).
Echouffo-Tcheugui, J. B. & Kengne, A. P. Risk models to predict chronic kidney disease and its progression: A systematic review. PLoS Med. 9(11), e1001344 (2012).
Choe, S. H. et al. Severity and duration of acute kidney injury and chronic kidney disease after cardiac surgery. J. Clin. Med. 10(8), 1556 (2021).
Zaky, A. et al. End-of-procedure volume responsiveness defined by the passive leg raise test is not associated with acute kidney injury after cardiopulmonary bypass. J. Cardiothorac. Vasc. Anesth. 35(5), 1299–1306 (2021).
Ishani, A. et al. The magnitude of acute serum creatinine increase after cardiac surgery and the risk of chronic kidney disease, progression of kidney disease, and death. Arch. Intern. Med. 171(3), 226–233 (2011).
Coca, S. G., Yusuf, B., Shlipak, M. G., Garg, A. X. & Parikh, C. R. Long-term risk of mortality and other adverse outcomes after acute kidney injury: A systematic review and meta-analysis. Am. J. Kidney Dis. 53(6), 961–973 (2009).
Lafrance, J. P. & Miller, D. R. Acute kidney injury associates with increased long-term mortality. J. Am. Soc. Nephrol. 21(2), 345–352 (2010).
Xu, J. et al. Preoperative hidden renal dysfunction add an age dependent risk of progressive chronic kidney disease after cardiac surgery. J. Cardiothorac. Surg. 14(1), 151 (2019).
Sickeler, R. et al. The risk of acute kidney injury with co-occurrence of anemia and hypotension during cardiopulmonary bypass relative to anemia alone. Ann. Thorac. Surg. 97(3), 865–871 (2014).
Matsuura, R. et al. The clinical course of acute kidney disease after cardiac surgery: A retrospective observational study. Sci. Rep. 10(1), 6490 (2020).
Huen, S. C. & Parikh, C. R. Predicting acute kidney injury after cardiac surgery: A systematic review. Ann. Thorac. Surg. 93(1), 337–347 (2012).
Husain-Syed, F. et al. Clinical and operative determinants of acute kidney injury after cardiac surgery. Cardiorenal Med. 10(5), 340–352 (2020).
Guan, C. et al. Risk factors of cardiac surgery-associated acute kidney injury: Development and validation of a perioperative predictive nomogram. J. Nephrol. 32(6), 937–945 (2019).
Hallan, S. I. et al. Age and association of kidney measures with mortality and end-stage renal disease. JAMA 308(22), 2349–2360 (2012).
Liu, P. et al. Accounting for age in the definition of chronic kidney disease. JAMA Intern. Med. 181(10), 1359–1366 (2021).
Liu, P. et al. Progression and regression of chronic kidney disease by age among adults in a population-based cohort in Alberta, Canada. JAMA Netw. Open 4(6), e2112828 (2021).
Glassock, R. J. & Rule, A. D. Aging and the kidneys: Anatomy, physiology and consequences for defining chronic kidney disease. Nephron 134(1), 25–29 (2016).
Novak, Z. et al. Incidence and predictors of early and delayed renal function decline after aortic aneurysm repair in the Vascular Quality Initiative database. J. Vasc. Surg. 74(5), 1537–1547 (2021).
Hsu, C. Y. et al. Post-acute kidney injury proteinuria and subsequent kidney disease progression: The Assessment, Serial Evaluation, and Subsequent Sequelae in Acute Kidney Injury (ASSESS-AKI) Study. JAMA Intern. Med. 180(3), 402–410 (2020).
Henein, M. Y. & Lindqvist, P. Assessment of left ventricular diastolic function by Doppler echocardiography. Card. Fail. Rev. 1(2), 87–89 (2015).
Ad-hoc Working Group of ERBP et al. A European Renal Best Practice (ERBP) position statement on the Kidney Disease Improving Global Outcomes (KDIGO) clinical practice guidelines on acute kidney injury: Part 1: Definitions, conservative management and contrast-induced nephropathy. Nephrol. Dial. Transplant. 27(12), 4263–4272 (2012).
Acknowledgements
The Anesthesiology Informatics group, a resource supported by the UAB Department of Anesthesiology and Perioperative Medicine, provided Informatics services for this project.
Funding
The University of Alabama School of Medicine Faculty Development Grant 2015.
Author information
Authors and Affiliations
Contributions
AZ: developed the concept, study design and collected and analyzed data, and wrote the manuscript draft. DSY, DWM, JD: edited the manuscript. ATW, MM: participating in the concept and design of the manuscript. Participated in editing the manuscript. BK, BJM: participated in data collection and analysis and editing of the manuscript. RLM, DB: participated in data collection and statistical analysis. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zaky, A., Younan, D.S., Meers, B. et al. A pilot study to explore patterns and predictors of delayed kidney decline after cardiopulmonary bypass. Sci Rep 14, 6739 (2024). https://doi.org/10.1038/s41598-024-57079-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-57079-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.