Abstract
The relationship between ammonia and liver-related complications (LRCs) in acute-on-chronic liver failure (ACLF) patients is not clearly established. This study aimed to evaluate the association between ammonia levels and LRCs in patients with ACLF. The study also evaluated the ability of ammonia in predicting mortality and progression of LRCs. The study prospectively recruited ACLF patients based on the APASL definition from the ACLF Research Consortium (AARC) from 2009 to 2019. LRCs were a composite endpoint of bacterial infection, overt hepatic encephalopathy (HE), and ascites. A total of 3871 cases were screened. Of these, 701 ACLF patients were enrolled. Patients with LRCs had significantly higher ammonia levels than those without. Ammonia was significantly higher in patients with overt HE and ascites, but not in those with bacterial infection. Multivariate analysis found that ammonia was associated with LRCs. Additionally, baseline arterial ammonia was an independent predictor of 30-day mortality, but it was not associated with the development of new LRCs within 30 days. In summary, baseline arterial ammonia levels are associated with 30-day mortality and LRCs, mainly overt HE and ascites in ACLF patients.
Similar content being viewed by others
Introduction
Hyperammonemia is a major contributor to hepatic encephalopathy (HE) development1,2,3. The cerebral effect of ammonia is linked to systemic inflammation and bacterial translocation4. In patients with acute liver failure (ALF), hyperammonemia is correlated with brain edema and herniation5. However, this relationship is less well demonstrated in cirrhosis2,6,7. In ACLF patients with HE, intracranial hypertension, cerebral edema, and herniation are uncommon. Key factors associated with the presence and severity of HE are ammonia, abnormal brain oxygen consumption, and systemic inflammation. Improvements in these factors are associated with lower HE grades in ACLF patients8.
Ammonia metabolism is a multiorgan process that involves the liver, brain, kidneys, muscle, and gastrointestinal systems. As a result, hyperammonemia may indicate poor non-cerebral function reserves, ongoing multiorgan impairment, and malnutrition9. Several recent studies have highlighted the association between hyperammonemia and poor outcomes, including liver-related complications (LRCs), hospitalization, progression to ACLF, and mortality in patients with clinically stable advanced chronic liver disease or cirrhosis10,11. Previous studies revealed that ammonia was closely related to ACLF grade, organ failure in the liver, kidney, and brain, and is an independent risk factor for 28-day mortality12,13. These findings provided evidence that ammonia levels not only have clinical usefulness in evaluating HE severity but may also be a potential prognostic biomarker for identifying patients at high risk of poor outcomes. The relationship between plasma ammonia levels and other LRCs, including bacterial infection, ascites, and 30-day mortality in ACLF, is less well defined. Therefore, this study aimed to investigate the association between ammonia levels and LRCs in patients with ACLF and the efficacy of ammonia levels in predicting mortality and the development of new LRCs during the 30 days after hospitalization.
Methods
Study design and participants
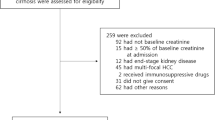
This study prospectively collected data from the Asian Pacific Association for the Study of the Liver (APASL)-ACLF Research Consortium (AARC) database, which included hospitalized ACLF patients from 31 centers between April 2009 and December 2019. Inclusion criteria were hospitalized patients with ACLF. Exclusion criteria were: age < 18 years, death within 24 h after admission, acute liver failure, pregnancy, human immunodeficiency virus infection, hepatocellular carcinoma, extrahepatic malignancy, or subjects missing key parameters such as ammonia levels. Patient characteristics, ACLF grade, organ failure events, and LRCs were recorded at baseline until day 30 or death. The diagnosis of ACLF was based on the APASL criteria, and grading of ACLF was determined by the AARC score14. ACLF grade I, II, and III was determined if the AARC was 5–7, 8–10, and 11–15, respectively14.
LRCs were defined as having at least one decompensating event, including overt hepatic encephalopathy (HE), ascites, and bacterial infection. Overt HE was diagnosed and graded using the West Haven Criteria after excluding other causes of neuropsychological disorders through history taking and neurological examination. Ascites was detected using abdominal imaging or other clinical findings. Bacterial infection was diagnosed according to the criteria as previously published15,16.
The study protocol and patient consent form were approved by the Institutional Review Board, Faculty of Medicine, Chulalongkorn University (IRB No. 330/59). All participants or their legal representatives provided written informed consent to participate in the study. The study protocol adhered to the Helsinki Declaration's ethical standards and the Good Clinical Practice recommendations.
Laboratory measurement
Baseline laboratory parameters, arterial lactate, and ammonia levels were evaluated. Arterial ammonia samples were obtained at admission. Samples were collected in a heparinized syringe and quickly transported on ice to the central laboratory for measurement.
Management protocol
All patients were managed in accordance with local protocols. Broad-spectrum antibiotics were given to treat infection in accordance with each hospital’s guidelines, following blood collection and a septic workup. Patients with hepatitis B virus infection were immediately treated with anti-viral therapy. Patients using hepatotoxic medications or alcohol consumption were required to discontinue. Intravenous crystalloids, as well as human albumin were administered for fluid resuscitation and terlipressin, if treating hepatorenal syndrome. Patients with HE were treated with lactulose and rifaximin. Organ support was administered as needed with renal replacement therapy for renal failure, intubation and mechanical ventilation for respiratory failure, and vasopressors for circulatory failure.
Statistical analysis
Categorical variables were presented as numbers and percentages and compared between groups using the Pearson Chi-square or Fisher's exact test. Continuous variables were analyzed for normality using the Shapiro–Wilk test. Normally distributed data were expressed as mean (standard deviation) with group means comparisons using the independent t-test, while non-normally distributed data were expressed as median (interquartile range) with group comparison testing using the Mann–Whitney U test. Multivariate logistic regression was done to assess the association with LRCs at baseline. Cox regression analyses identified potential factors associated with 30-day mortality. The Kaplan–Meier graph and survival predictions were compared using the Log-rank test. Area under the receiver operating characteristics (AUROC), and Youden’s index were analyzed to identify the optimal ammonia cutoffs for 30-day mortality. Comparison of AUROC was done by the Medcalc Software (Belgium) using Delong’s technique. Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) software, Version 23 (IBM Corporation, Armonk, NY, USA). Two-sided p-values less than 0.05 were considered statistically significant.
Results
Patient baseline characteristics
A total of 3871 patients with ACLF were screened. Of these, 701 patients with ACLF were enrolled. The most common reason for exclusion was a lack of ammonia presence. Baseline characteristics of patients who were included and excluded were shown in the Supplementary Table 1. Patients who were excluded had higher rates of LRCs and alanine aminotransferase (ALT), but a lower proportion of ACLF grade II-III, total bilirubin (TB), INR, creatinine, and lactate levels than those who were included. In patients who were enrolled, most of the patients were male (85.6%, n = 600), with a median age of 43 (IQR: 37–52) years. The most common cause of chronic liver disease or cirrhosis was alcohol-related liver disease (84.2%, n = 590), followed by hepatitis B virus infection (15.8%, n = 111). The median Model for End-Stage Liver Disease (MELD), Sequential Organ Failure Assessment (SOFA), and AARC scores were 29.0 (IQR: 24.3–35.0), 8 (IQR: 6–10) and 9 (IQR: 8–11), respectively. At baseline, 127 patients (18.1%) had ACLF grade I, 364 (51.9%) had ACLF grade II, and 210 (30.0%) had ACLF grade III. In addition, 427 patients (60.9%) had at least one LRC, 346 (49.4%) had ascites, 276 (39.4%) had overt HE, and 245 (35.0%) had bacterial infections at admission. Baseline patient characteristics according to each LRC, overt HE, ascites, and bacterial infection were analyzed and shown in the Supplementary Table 2. ACLF with overt HE, ascites, or bacterial infection were sicker, as evidenced by higher MELD score than those without these complications.
Ammonia level, severity of ACLF, and liver-related complications at admission
Ammonia levels increased with the severity of ACLF with mean values of 117.2 ± 91.6, 131.4 ± 74.2, and 161.5 ± 113.2 µmol/L (p < 0.001) in ACLF grades I, II, and III, respectively. Baseline demographics and characteristics of LRC presence are shown in Table 1. Patients with LRCs had a larger proportion of ACLF grade III as well as higher white blood cell counts (WBC), ALT, INR, serum lactate, MELD, and AARC scores. Ammonia levels were significantly higher in patients who had at least one LRCs than those without LRCs [133 (IQR: 98.0–194.7) vs. 69 (IQR: 36.1–141.0) µmol/L, p < 0.001]. Baseline ammonia levels were significantly higher in ACLF patients with ascites [122 (IQR: 71.2–198.8) vs. 107 (IQR: 67–160.5) µmol/L, p < 0.001] and overt HE [136.1 (IQR: 71.2–198.8) vs. 111 (IQR: 67–160.5) µmol/L, p = 0.02] than those without these complications. Patients with bacterial infections showed a non-significant difference compared to those without bacterial infections [125 (IQR: 75.6–180.1) vs. 114 (IQR: 64–171) µmol/L, p = 0.09].
Results from the univariate analysis revealed that total WBC, TB, INR, and ammonia levels were associated with LRCs. Multivariate analysis showed that ammonia levels (OR = 1.011, 95%CI 1.009–1.014, p < 0.001) was independently associated with LRCs (Table 2).
Factor associated with 30-day mortality
Overall, the 30-day mortality rate was 49.9% (n = 350). ACLF patients who died within 30 days after hospitalization were older and had a proportional higher incidence of alcohol-related liver disease, baseline LRCs, and ACLF grade III. Higher baseline MELD, SOFA, and AARC scores were also reported compared to patients who survived the 30-day period. Baseline ammonia (p < 0.001) and lactate (p < 0.001) was significantly lower in survivors compared to non-survivors (Supplementary Table 3).
Results from the univariate Cox regression analysis found that older age, baseline hemoglobin, WBC, TB, ALT, INR, creatinine, ammonia levels, MELD, and AARC score were associated with 30-day mortality. In multivariate analysis, model 1 revealed that older age (HR = 1.022, 95% CI 1.013–1.032, p < 0.001), lower hemoglobin (HR = 0.941, 95% CI 0.894–0.989, p = 0.02), high INR (HR = 1.219, 95% CI 1.126–1.320, p < 0.001), serum creatinine (HR = 1.154, 95% CI 1.089–1.224, p < 0.001), arterial ammonia (HR = 1.002, 95% CI 1.001–1.003, p < 0.001) and ALT (HR = 1.000, 95%CI 1.000–1.001, p < 0.001) were independent predictors of 30-day mortality in ACLF patients (Table3). Ammonia levels were independent predictors of 30-day mortality when adjusting for MELD score (Model 2) and AARC score (Model 3). Baseline ammonia levels predicted 30-day mortality with an AUROC of 0.58 (95% CI 0.53–0.62, p = 0.001). However, the accuracy of ammonia was less than baseline AARC score (p < 0.001) in predicting 30-day mortality (AUROC = 0.68, 95%CI 0.64–0.72).
By maximizing Youden’s index, the optimal cutoff of baseline ammonia to predict 30-day mortality was ≥ 150 µmol/L with 40.3% sensitivity, 72.4% specificity, 59.2% positive predictive value, 54.9% negative predictive value, and an AUROC of 0.56 (95%CI 0.52–0.61, p = 0.004). The Kaplan–Meier survival analysis stratified by ammonia level is shown in Fig. 1. Patients with baseline ammonia < 150 µmol/L had a higher 30-day survival rate than those with ammonia ≥ 150 µmol/L (log-rank test; p = 0.002). However, ammonia ≥ 150 µmol/L was not an independent predictor for 30-day mortality after adjusting with MELD score (adjusted HR = 1.106, 95%CI 0.888–1.378, p = 0.37).
Ammonia as a predictor of liver-related complications development
At the time of admission, 274 out of 701 patients (39.1%) did not have any LRCs. During the 30-day follow-up, 63 patients (23%) developed at least one LRC, 23 (8.4%) developed ascites, 13 (4.7%) had bacterial infections, and 21 got overt HE (7.7%). Patients who developed LRCs exhibited higher arterial ammonia than those without LRC development (124.6 ± 108.7 vs. 83.4 ± 64.5 µmol/L, p = 0.04). Ammonia levels were also significantly higher in those with ascites or overt HE compared to those without these complications, while ammonia levels were not statistically different in patients with or without the development of bacterial infection over 30 days. Univariate analysis revealed that only baseline ammonia (OR = 1.006, 95% CI 1.003–1.010, p < 0.001) predicted the development of LRCs during the 30-day follow-up period. (Supplementary Table 4). Patients with LRCs development during 30 days had a higher 30-day mortality rate than those without LRCs development (42.7% vs. 28.6%, p = 0.04).
Discussion
The current study investigated the association between arterial ammonia levels and LRCs in patients with ACLF. We also assessed the potential role of arterial ammonia in predicting mortality and development of LRCs during the 30 days after hospitalization. Our main finding showed that baseline ammonia levels are associated with LRC, particularly overt HE, and ascites. In addition, arterial ammonia is a potential predictor of 30-day mortality and LRC development. The study findings have highlighted the additional role of ammonia in detecting and predicting poor clinical outcomes other than HE in ACLF patients.
Hyperammonemia is traditionally described as the central contributor of HE development. It is also associated with non-neurological organ injury. Ammonia exerts multiorgan dysfunction by promoting hepatocyte death, activation of hepatic stellate cells, and producing neutrophil phagocytic impairment, resulting in liver inflammation, fibrosis, portal hypertension, and increased risk for infection17,18,19. Tranah et al. demonstrated that ammonia independently predicts 1-year mortality and LRCs such as bacterial infection, variceal bleeding, ascites, and overt HE in clinically stable outpatients with cirrhosis11. In addition, ammonia outperforms Child–Pugh and MELD scores in predicting complications. Balcar et al. recently showed that ammonia is linked to liver-related death, liver dysfunction, and portal hypertension severity in clinically stable outpatients with advanced chronic liver disease10. In sicker patients, such as those with ACLF, ammonia is associated with mortality8,12,20,21, severity of ACLF12, and an increased risk of organ failure12,21. Consistent with the current study’s findings, ammonia is independently associated with the severity of ACLF and 30-day mortality. To our knowledge, the study presents new evidence that ammonia is also independently related to the presence of LRCs, not only overt HE but also ascites in patients with ACLF. Although the study did not demonstrate the association between bacterial infection and high ammonia levels. This finding should be considered in the context that seventy percent (n = 172/245) of patients with bacterial infection had more than one liver-related complication. This could potentially impact the relationship between this complication and ammonia level. Further analysis in ACLF without baseline LRCs found that ammonia level predicts the new onset of LRC development within 30 days after admission. These findings support the additional prognostic role of ammonia in detecting and predicting complications in ACLF patients. However, the current study found that baseline ammonia levels ≥ 150 µmol/L was associated with 30-day mortality, but the AUROC was fair and had low sensitivity.
There is an unmet need for a universal definition of ACLF. Three main definitions from different consortiums around the world have been proposed from the APASL AARC, European Association for the Study of the Liver-Chronic Liver Failure (EASL-CLIF) consortium22, and the North American Consortium for the Study of End-Stage Liver Disease (NACSELD)23. Organ failure is one of the key differences among the three guidelines. APASL AARC requires hepatic failures, EASL-CLIF requires a combination of hepatic and extrahepatic organ failure, and NACSELD needs at least two extrahepatic organ failures. ACLF is characterized by acute hepatic insult presenting as jaundice and coagulopathy, followed by ascites and/or encephalopathy within 4 weeks in patients with prior chronic liver disease or cirrhosis by APASL guidelines14. The feature of acute decompensation indicates significant hepatic deterioration, supporting the importance of hepatic failure in these criteria. ACLF precipitated by hepatic insults is distinct from that caused by extrahepatic insults24. The presence of LRC in ACLF may indicate prominent portal hypertension. Development of LRCs is associated with high 6-week mortality and poor outcomes in patients with ACLF25. In addition, hepatic decompensation indicates poor reversibility of ACLF syndrome26. According to this study's findings, ammonia may guide physicians in managing these complications.
There are some limitations in this study. First, there could be discrepancies in technical concerns with ammonia testing among centers, even though investigators checked the test’s reliability before entering data. Strict sample handling and processing requirements were the possible explanations for the differences in ammonia levels among testing sites27. Ammonia level is affected by various factors such as the centrifugation process, blood drawing tourniquet technique, transportation, and hemolysis. Second, the study only enrolled participants with alcohol-related liver disease and hepatitis B virus, since these are two common causes of chronic liver disease in the Asia–Pacific region. Third, variceal bleeding was not included in the list of liver-related complications due to the inaccessibility of this data in the majority of the hospitals. Fourth, there were a small number of patients without baseline LRCs who developed LRCs during the 30 days of follow-up, which might affect the result’s validity. In addition, the management of ACLF relied on the decision-making of physicians in each hospital, which could impact the outcome of patients. If the patients were discharged earlier than day 30, they were re-evaluated clinical information at the outpatient clinic on the 30th day after enrollment. Ascites was assessed using abdominal imaging or clinical findings according to the attending physician's decision at each hospital. Therefore, patients with grade 1 ascites might be overlooked if they were not evaluated by ultrasound.
In conclusion, baseline arterial ammonia levels demonstrated an association with 30-day mortality and LRCs, encompassing not only overt HE but also ascites in patients with ACLF.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Wright, G., Sharifi, Y., Jover-Cobos, M. & Jalan, R. The brain in acute on chronic liver failure. Metab. Brain Dis. 29, 965–973. https://doi.org/10.1007/s11011-014-9553-0 (2014).
Ong, J. P. et al. Correlation between ammonia levels and the severity of hepatic encephalopathy. Am. J. Med. 114, 188–193. https://doi.org/10.1016/s0002-9343(02)01477-8 (2003).
Vierling, J. M. et al. Fasting blood ammonia predicts risk and frequency of hepatic encephalopathy episodes in patients with cirrhosis. Clin. Gastroenterol. Hepatol. 14, 903-906.e901. https://doi.org/10.1016/j.cgh.2015.11.018 (2016).
Thanapirom, K. et al. Bacterial DNA translocation-induced systemic inflammation is associated with overt hepatic encephalopathy and predicts mortality in patients with cirrhosis. J. Hepatol. 78, S217 (2023).
Clemmesen, J. O., Larsen, F. S., Kondrup, J., Hansen, B. A. & Ott, P. Cerebral herniation in patients with acute liver failure is correlated with arterial ammonia concentration. Hepatology 29, 648–653. https://doi.org/10.1002/hep.510290309 (1999).
Haj, M. & Rockey, D. C. Ammonia levels do not guide clinical management of patients with hepatic encephalopathy caused by cirrhosis. Am. J. Gastroenterol. 115, 723–728. https://doi.org/10.14309/ajg.0000000000000343 (2020).
Shawcross, D. L. et al. Infection and systemic inflammation, not ammonia, are associated with Grade 3/4 hepatic encephalopathy, but not mortality in cirrhosis. J. Hepatol. 54, 640–649. https://doi.org/10.1016/j.jhep.2010.07.045 (2011).
Chiriac, S. et al. Role of ammonia in predicting the outcome of patients with acute-on-chronic liver failure. World J. Clin. Cases 9, 552–564. https://doi.org/10.12998/wjcc.v9.i3.552 (2021).
Tapper, E. B., Jiang, Z. G. & Patwardhan, V. R. Refining the ammonia hypothesis: A physiology-driven approach to the treatment of hepatic encephalopathy. Mayo Clin. Proc. 90, 646–658. https://doi.org/10.1016/j.mayocp.2015.03.003 (2015).
Balcar, L. et al. Impact of ammonia levels on outcome in clinically stable outpatients with advanced chronic liver disease. JHEP Rep. 5, 100682. https://doi.org/10.1016/j.jhepr.2023.100682 (2023).
Tranah, T. H. et al. Plasma ammonia levels predict hospitalisation with liver-related complications and mortality in clinically stable outpatients with cirrhosis. J. Hepatol. 77, 1554–1563. https://doi.org/10.1016/j.jhep.2022.07.014 (2022).
Hu, C. et al. Serum ammonia is a strong prognostic factor for patients with acute-on-chronic liver failure. Sci. Rep. 10, 16970. https://doi.org/10.1038/s41598-020-73603-1 (2020).
Shalimar, et al. Prognostic role of ammonia in patients with cirrhosis. Hepatology 70, 982–994. https://doi.org/10.1002/hep.30534 (2019).
Sarin, S. K. et al. Acute-on-chronic liver failure: consensus recommendations of the Asian Pacific association for the study of the liver (APASL): An update. Hepatol. Int. 13, 353–390. https://doi.org/10.1007/s12072-019-09946-3 (2019).
Piano, S. et al. Epidemiology and effects of bacterial infections in patients with cirrhosis worldwide. Gastroenterology 156, 1368-1380.e1310. https://doi.org/10.1053/j.gastro.2018.12.005 (2019).
Bajaj, J. S. et al. Second infections independently increase mortality in hospitalized patients with cirrhosis: The North American consortium for the study of end-stage liver disease (NACSELD) experience. Hepatology 56, 2328–2335. https://doi.org/10.1002/hep.25947 (2012).
Jalan, R. et al. Ammonia produces pathological changes in human hepatic stellate cells and is a target for therapy of portal hypertension. J. Hepatol. 64, 823–833. https://doi.org/10.1016/j.jhep.2015.11.019 (2016).
Jia, B. et al. Hyperammonaemia induces hepatic injury with alteration of gene expression profiles. Liver Int. 34, 748–758. https://doi.org/10.1111/liv.12365 (2014).
Shawcross, D. L. et al. Ammonia impairs neutrophil phagocytic function in liver disease. Hepatology 48, 1202–1212. https://doi.org/10.1002/hep.22474 (2008).
Verma, N. et al. Dynamic assessments of hepatic encephalopathy and ammonia levels predict mortality in acute-on-chronic liver failure. Hepatol. Int. 15, 970–982. https://doi.org/10.1007/s12072-021-10221-7 (2021).
Shalimar, et al. Persistent or incident hyperammonemia is associated with poor outcomes in acute decompensation and acute-on-chronic liver failure. JGH Open 4, 843–850. https://doi.org/10.1002/jgh3.12314 (2020).
Jalan, R. et al. Development and validation of a prognostic score to predict mortality in patients with acute-on-chronic liver failure. J. Hepatol. 61, 1038–1047. https://doi.org/10.1016/j.jhep.2014.06.012 (2014).
Bajaj, J. S. et al. Survival in infection-related acute-on-chronic liver failure is defined by extrahepatic organ failures. Hepatology 60, 250–256. https://doi.org/10.1002/hep.27077 (2014).
Shi, Y. et al. Acute-on-chronic liver failure precipitated by hepatic injury is distinct from that precipitated by extrahepatic insults. Hepatology 62, 232–242. https://doi.org/10.1002/hep.27795 (2015).
Sharma, S. et al. Acute variceal bleeding portends poor outcomes in patients with acute-on-chronic liver failure: A propensity score matched study from the APASL ACLF Research Consortium (AARC). Hepatol. Int. 16, 1234–1243. https://doi.org/10.1007/s12072-022-10372-1 (2022).
Wang, H. et al. Reversibility of acute-on-chronic liver failure syndrome in hepatitis B virus-infected patients with and without prior decompensation. J. Viral Hepat. 29, 890–898. https://doi.org/10.1111/jvh.13732 (2022).
Bajaj, J. S. et al. Variability and lability of ammonia levels in healthy volunteers and patients with cirrhosis: Implications for trial design and clinical practice. Am. J. Gastroenterol. 115, 783–785. https://doi.org/10.14309/ajg.0000000000000384 (2020).
Acknowledgements
We would like to thank all the staff of the Division of Gastroenterology and Hepatology, Chulalongkorn University, and King Chulalongkorn Memorial Hospital, Thai Red Cross Society, for their technical assistance and clinical support.
Funding
This study was supported by Ratchadaphiseksomphot Endowment Fund of Center of Excellence in Hepatic Fibrosis and Cirrhosis, Chulalongkorn University: GCE 3300170037 (Dr. Kessarin Thanapirom), the Liver Research Unit, and the Fatty Liver Unit, Division of Gastroenterology of the Faculty of Medicine, Chulalongkorn University (Prof. Sombat Treeprasertsuk).
Author information
Authors and Affiliations
Contributions
Conceptualization: K.T., S.T., SK. Sarin; methodology: K.T., S.T., SK. Sarin; formal analysis and investigation: K.T., S.T.; writing—original draft preparation: K.T.; writing—review and editing: S.T., A.C., SK. Sarin; funding acquisition: S.T.; resources: K.T., S.T., A.C., N.V., RK. Dhiman, MA. Mahtab, H.D., A.S, SS. Hamid, SS. Tan, GH. Lee , H. G., A.S., DJ. Kim, CE. Eapen, H.T., N.Y., AK. Dokmeci, M.S., A.A., A. K., R. K., VGM. Prasad, A. S., J. S., DA. Payawal, G. L., SK. Sarin; Supervision: S.T., SK. Sarin. All authors have reviewed and agreed to the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Thanapirom, K., Treeprasertsuk, S., Choudhury, A. et al. Ammonia is associated with liver-related complications and predicts mortality in acute-on-chronic liver failure patients. Sci Rep 14, 5796 (2024). https://doi.org/10.1038/s41598-024-56401-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-56401-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.