Abstract
Lupus nephritis (LN) is kidney involvement of systematic lupus erythematous that ranges from mild to severe and occurs in 60% of adult patients. Despite advances in therapy, LN morbidity and mortality remains high. There is a paucity of data regarding adult LN patient's treatment outcome, survival status, and associated factors in developing countries, particularly in Ethiopia. This study aimed to assess the treatment outcome, survival status, and associated factors of adult patients treated for LN in two selected tertiary hospitals [Tikur Anbessa Specialized Hospital (TASH) and St. Paul’s Hospital Millennium Medical College (SPHMMC)] of Addis Ababa, Ethiopia. A hospital-based retrospective cross-sectional multicenter study was conducted from January 1, 2016 to January 1, 2021. Socio-demographic, clinical, and treatment-related data were collected from patient’s medical records by using a structured abstraction checklist. Descriptive statistics were used to summarize the quantitative data as appropriate. The modified Aspreva Lupus Management Study (mALMS) criteria was applied to categorize LN treatment outcomes into complete, partial, and non-response. Multinomial logistic regression analysis was performed to identify predictors of LN treatment outcome. Patients’ survival was estimated by using Kaplan–Meier and Cox proportion regression analysis. P value < 0.05 was considered to declare statistical significance. A total of 200 LN patients were included in the final analysis. Amongst these, the majority of them (91.5%) were females. The median age of the patients was 28 (15–60) years. The mean duration of treatment follow-up was 28 months. The commonly prescribed immunosuppressive drugs during both the induction (49.5%) and maintenance (60%) phases were a combination of mycophenolate mofetil with prednisolone. Complete, partial, and non-responses at the last follow-up visit accounted for 66.5%, 18.0%, and 15.5%, respectively. Patient survival at the last follow-up visit was more than 90% for patients with complete response to the induction therapy. Non-response at the last follow-up visit was significantly associated with severe disease activity index (adjusted odds ratio [AOR] = 6.25, 95% confidence interval [CI] 1.49–26.10), presence of comorbidity (AOR = 0.21, 95% CI 0.05–0.92), baseline leucopenia (AOR = 14.2, 95% CI 1.04–201.3), partial response at the end of induction therapy (AOR = 32.63, 95% CI 1.4–736.0), and duration of induction therapy of greater than 6 months (AOR = 19.47, 95% CI 1.5–258.8). This study unveiled that lower numbers of LN patients were presented with non-response at the last follow-up visit and non-response to induction therapy was associated with lower patients’ survival rates compared with complete or partial response.
Similar content being viewed by others
Introduction
Lupus nephritis (LN) is the most common complication of systemic lupus erythematosus (SLE) which is caused by the complex interaction between genetic predisposition and environmental factors such as excess sunlight exposures, infection, extreme stress, and certain drugs1. It is estimated that lupus nephritis clinically affects around 60% of SLE patients2. The prevalence of LN remained unchanged over the last 45 years, with 50%, 25%, and 20% accounting for class III, IV, and V, respectively2. LN is manifested by an increase in serum creatinine, development of proteinuria (> 0.5 g/day), or active urinary sediment with red blood cells, granular or mixed cast that results in end-stage renal disease (ESRD).
Based on renal biopsy findings, LN was classified into class I (minimal mesangial involvement), class II (mesangial proliferative LN), class III (focal LN involving < 50% of glomeruli), class IV (diffuse segmental LN involving > 50% of glomeruli), class V (lupus membranous nephropathy), and class VI (advanced stage affecting > 90% of glomeruli) as per the International Society of Nephrology (ISN) and the Renal Pathology Society (RPS)3,4.
Treatment of LN is not an easy task. Despite all the studies that have been conducted and the use of various advanced drugs, treating LN poses a significant challenge. Although different protocols were used depending on the histological class of LN, the exact standard treatment regimen for LN patients remains controversial. Class II LN patients often have excellent renal prognosis by prednisolone only. Unless there is an extra-renal manifestation, class I usually does not require specific immunosuppressive therapy5. However, if not treated well, class II LN can transform into class III or IV6,7. For class VI, renal transplantation is preferred over immunosuppressive therapy7,8. Among all the treated patients, 10–15% progress to ESRD. Even with treatment, up to 44% of patients with class III or IV LN develop ESRD within 15 years6,7.
To achieve the desired treatment outcome, LN treatment is divided into two phases: induction therapy and maintenance therapy. Induction therapy consists of high-dose immunosuppressant drugs used for six months to decrease disease activity, whereas maintenance therapy consists of less intensive immunosuppressant drugs used to maintain remission and prevent disease relapse in patients who respond to induction therapy9. According to the recent American College of Rheumatology (ACR) guideline, patients with biopsy-proven LN class III or IV should receive induction therapy of either mycophenolate mofetil (MMF) or intravenous cyclophosphamide along with high-dose corticosteroid4. The duration of the maintenance phase is still arguable5,9.
The definition of categorizing LN response into complete response (CR), partial response (PR), and non-response (NR) to drug therapy varies from study to study. The modified Aspreva Lupus Management Study (mALMS) criteria, which classifies LN response into complete, partial, and no response by considering serum creatinine and 24-h urine protein, was widely used in most studies10. The response to therapy in LN patients is affected by numerous factors including patient, clinical and treatment-related factors. In Africa, the response is limited by the availability and cost of drugs, and by the shortage of laboratory facilities and poor drug adherence11,12.
According to internationally accepted guidelines, the last CR is often expected after 24 months of therapy, despite reports of CR at 6 months, 12 months, and 36 months in a few studies13. These realities differ based on ethnicity, baseline clinical characteristics, regimen chosen, and initial Standard Systemic Lupus Erythematous Disease Activity Index (SLEDAI-2 K) score14. When combined with MMF, adjuvant therapy with hydroxychloroquine is used to increase CR15. A nascent study asserted that CR varies among studies and may range from 10 to 85%16.
Although some studies have been conducted in developed countries on the treatment outcome, and survival status of LN, the issue is under-studied in sub-Saharan Africa, particularly Ethiopia. In most of these studies, complete response [CR] and partial response [PR] were merged and considered similar outcomes, despite being clinically distinct. In Ethiopia, there is a knowledge gap about factors associated with non-response to therapy and the survival status of LN patients. So, the current study was designed to fill these gaps of knowledge. This study aimed to assess the treatment outcome, survival status, and associated factors among adult patients treated for LN in TASH and SPHMMC from January 1, 2016 to January 1, 2021.
Methodology
Study area, study setting, and study period
A hospital-based retrospective cross-sectional study was conducted at the adult outpatient renal clinics of TASH and SPHMMC, Addis Ababa, Ethiopia from January 1, 2016-January 1, 2021. Data was collected from July 1-September 1, 2021. TASH is the largest tertiary care, specialized, referral, and teaching hospital in the country that is owned by the government and was established in 1973. It has 51 specialty outpatient clinics, serving 500,000 patients annually17. SPHMMC is a major teaching hospital inaugurated in 1969 by Emperor Haile Selassie with the help of the German Evangelical Church and currently has more than 700 beds, with an annual average of 200,000 patients served in the hospital18. The outpatient renal clinics of both hospitals offer comprehensive clinical and follow-up services in which adult patients with renal diseases including LN were followed. Renal biopsy was provided in both hospitals.
Study participants
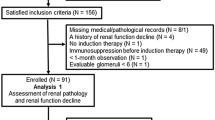
All patients who fulfilled the inclusion criteria were included in the study. All adult patients with LN, who were on follow-up at either TASH or SPHMMC renal clinic between January 2016 and January 2021 were included in the study. Patients were eligible for enrollment in this study if they were at least 15 years of age at diagnosis, diagnosed with LN either by renal biopsy or laboratory results of 24 h urine protein and lupus serology, had SLE based on the 1982 revised ACR criteria, who have had regular follow-up at the adult renal clinic of either TASH or SPHMMC for at least 12 months, had sufficient laboratory data for assessment of renal remission after 6 month, and on standard treatment protocol. Patients with ESRD before starting treatment, had Class I and VI types of LN, with known chronic kidney disease and diabetes prior to LN onset, had double glomerulonephropathy, and with incomplete medical records were excluded.
Sample size determination and sampling technique
All adult LN patients who met the inclusion criteria and had follow-ups in TASH and SPHMMC were included as study participants since a limited number of patients were encountered during the study period. A convenience sampling technique was used to collect the necessary data that fulfils the inclusion criteria. The two health facilities were chosen for convenience because they had a large number of LN patients and were providing renal biopsies for LN patients.
Study variables
Dependent variable
Treatment outcome status (complete response at the last follow-up [CR], partial response at the last follow-up [PR], non-response at the last follow-up [NR]).
Independent variables
(1) Sociodemographic characteristics include age, sex, and place of residence. (2) Clinical characteristics include SLE duration before LN onset, class of LN, SLE disease activity, presence of comorbidity, leucopenia, thrombocytopenia or anemia, baseline serum creatinine, and 24 h urine protein, and baseline ANA and anti-DsDNA. (3) Treatment-related characteristics include treatment regimen selected, pulse steroid therapy, response to induction therapy, time to remission, treatment duration, total follow up period, admission during follow up, and cotrimoxazole infection prophylaxis.
Data collection instrument and procedure
Data was collected by using a structured checklist. The checklist was developed after reviewing different literature published on the subject area. It contained necessary variables that could be obtained from the patient’s medical profile, like patient-related data (age, sex, diagnosis, disease duration, baseline clinical information, laboratory data, and disease severity score by SLEDAI-2K, medication-related data (regimen selected, dose, and duration) and outcome status (CR, PR, and NR). The SLEDAI-2K score was used to assess the SLE disease severity index19. Data were retrospectively collected from the patient’s medical record by strictly following criteria needed to confirm LN like renal biopsy. In the absence of renal biopsy, the presence of two consecutive 24-h proteinuria readings > 0.5 g/day, and an additional feature supporting active lupus, such as positive serology or active urinary sediment was considered to diagnose LN20. A pre-test was done on 5% of the sample population to assure clarity and content uniformity. The checklist was amended based on the pretest finding. Two days training was given by the principal investigators for two clinical pharmacists (data collectors) about the aim of the study, the checklist, and data collection procedures. Initially, SLE patients with LN were counted from the patient registration logbook. Then, by using patient’s identification card number, patient’s medical chart, and I-care profile, data were retrieved from the card room and I-care respectively. However, as this study was retrospective, adverse drug events were not collected unless recorded by the physicians.
Data analysis
The data were entered into and cleaned in Epi Info version 4.6.0.2 and were exported into and analyzed in Statistical Package for the Social Sciences (SPSS) version 26. Initially, normality and multicollinearity were checked. A normality test was done by using Shapiro–Wilk’s and Kolmogorov-Simonov (K-S) tests for numerical independent variables. To declare the absence of normality, a level of significance greater than 0.05 was used. Multicollinearity was checked to test the correlation among predictor variables using the variance inflation factor (VIF). A VIF < 8 was considered a cut point for excluding collinearity. Frequencies and percentages were used for categorical variables, while mean ± standard deviation and/or median (IQR) for continuous variables.
A multinomial logistic regression analysis was carried out to analyze the association between independent variables and treatment outcomes. The maximum likelihood of parameter estimators for variables composing the model was used to obtain crude odds ratio (COR) and adjusted odds ratio (AOR) with a 95% confidence interval. The validity of the model was tested by likelihood ratio test. During multinomial analysis, the LN treatment outcome category labeled as NR was considered as the reference category against which all other outcomes were compared. Different reference categories were used when comparing variables categorized within the same variable. All variables associated with LN treatment outcome at p-value ≤ 0.25 in the bivariate analysis were picked and entered into the multivariate analysis to control confounders.
Survival analysis (Kaplan–Meier method) was used to calculate the survival rate by total follow-up time between variables. The overall survival curves were derived by Kaplan–Meier methods and the difference between the survival curves were compared by using a log-rank test. The Cox regression model assumption of proportional hazards was checked by testing the interaction of covariates with time before running the Cox proportional hazard regression analysis using Cox with time-dependent covariates. Multivariate Cox proportional hazard regression analysis was performed to identify independent factors associated with non-response (NR). For measuring the strength of association, the hazard ratio (HR) was used. The level of statistical significance was declared at p-value < 0.05 and results were reported at a 95% confidence interval.
Operational definition
Complete response (CR) at the last follow-up—is reducing serum creatinine to ≤ 1.4 mg/dl and 24-h urine protein to ≤ 0.5 g/day. Partial response (PR) at the last follow-up—is occurrence of either serum creatinine to ≤ 1.4 mg/dl or 24-h urine protein ≤ 0.5 g/day. Non-response (NR) at the last follow-up—is failure to achieve complete [CR] or partial response [PR]), death, development of ESRD, and relapse. Relapse—is nephrotic range proteinuria (> 3 g/24 h), active urinary sediment, and an increase in serum creatinine by 30% after achieving complete or partial remission. End-stage renal disease (ESRD)-serum creatinine > 6 mg/dl at the last follow-up visit, on renal dialysis for at least 3 months, and waiting for renal transplantation. Comorbidity—is the presence of cardiovascular disease, neurologic disease, dyslipidemia, cancer, infection, hypothyroidism, psychosis, and drug-induced complications. Baseline clinical characteristics—it is the patient clinical characteristics and laboratory data at the first diagnosis of lupus nephritis as registered on the patient's medical card. Baseline WBC—is the reading of WBC at the initial diagnosis of lupus nephritis before starting treatment of lupus nephritis as registered on the patient’s medical record. Mild disease activity—Lupus nephritis patients with SLEDAI-2 K score between 1 and 3 inclusive. Moderate disease activity—Lupus nephritis patients with SLEDAI-2 K score between 4 and 12 inclusive. Severe disease activity—Lupus nephritis patients with SLEDAI-2 K score above 12.
Ethical consideration
The study was approved by the Ethical Review Board (ERB) of Addis Ababa University, College of Health Sciences (25/03/2021; ERB No. 252/13/2021), and the Institutional Review Board of SPHMMC (Reference number; Pm23/384). The study protocol was performed in accordance with the Declaration of Helsinki. All methods were performed in accordance with the relevant guidelines and regulations. informed consent was obtained from all subjects. To collect the necessary data, official letters were written to each hospital and permission to conduct the study was obtained from responsible directorates of each hospital. Confidentiality, neutrality, anonymity, accountability, and academic honesty were maintained throughout the study.
Results
Socio-demographic and clinical characteristics of lupus nephritis patients
A total of 216 LN patients were enrolled from TASH and SPHMMC. Of these, 16 patients were lost from follow-up, and thus only 200 patients were included in the final analysis. Out of the total studied participants, 183 (91.5%) were females. The median (IQR) age of patients was 28 (33–23) years. The median duration of SLE before clinical diagnosis of LN onset was 9.5 month and 98% of the patients were considered early-onset LN. The mean duration of observation in LN patients included in our study during the study periods was 28 months. Renal involvement of LN was verified by renal biopsy in only 73.5% of patients, possibly due to the patient's financial constraints in the study setting. Mean baseline serum creatinine and 24-h urine protein were 2.04 ± 1.75 mg/dl, and 2.4 ± 0.52 g/day, respectively. About 79(39.5%) of patients had a baseline serum creatinine of ≤ 1.4 mg/dl and 80(40%) of patients had a baseline 24-h urine protein of > 3 g/day. Approximately 38.5% of patients had a variety of comorbidities (Table 1).
Treatment outcomes and causes of admission of lupus nephritis patients
About 36.5% of LN patients had a history of admission to a hospital during their follow-up time. The most common causes of admissions were acute kidney injury (11.5%), and pneumonia (9%). Overall remission (complete plus partial response) was achieved in 84.5% of patients and non-response to drug therapy occurred in 15.5% of patients at their last follow-up visit (Table 2).
Types of comorbidities of lupus nephritis patients
Hypertension was the most prevalent comorbid condition manifested in LN patients, constituting 22.5% of all comorbidities. Amlodipine (9.5%) and Enalapril (9.5%) were the most frequent drugs used to manage comorbidities. The most common immunosuppressant drugs that cause comorbidity were prednisolone and chloroquine, as recorded by physicians (Table 3).
Treatment-related characteristics of lupus nephritis patients
The most common drugs during the induction phase were mycophenolate mofetil (MMF) with prednisolone 99 (49.5%) and cyclophosphamide (CYC) with prednisolone 62 (31%). Regarding maintenance therapy, the most frequently prescribed drugs were MMF with prednisolone 120 (60%), and prednisolone alone 42 (21%). Only 24.5% of patients received three days of pulse steroid therapy which is comprised of either methylprednisolone or prednisolone. The dose of prednisolone used in pulse steroid therapy in this study is in the range of 80–110 mg per day. The total daily dose of prednisolone was divided into morning and evening doses for three days when used for pulse steroid therapy. The drug most widely used for pulse steroid therapy in lupus nephritis patients is methylprednisolone; however, given its easy availability and cost, high-dose prednisolone has been often used in Ethiopia for pulse steroid to decrease the severity of diseases. Patients with an overall complete plus partial response to immunosuppressive therapy during the induction therapy were 185 (92.5%). From this, LN patients who achieved partial response (57%) were higher than those who achieved complete response (35.5%). The median duration of induction and maintenance therapy was 6 (6–8) months and 20 (18–25) months, respectively. Prophylactic cotrimoxazole was used in approximately half of the patients. In this study, regimen changes in both induction and maintenance therapy for LN were observed in 17 and 18 LN patients, respectively. The most common reason for the regimen change was non-responsiveness to immunosuppressive therapy, with only two patients on metformin due to medication error (Table 4).
Factors associated with treatment outcome of lupus nephritis patients
According to the multinomial logistic regression model; LN patients with moderate SLE disease activity index (AOR = 6.25, 95% CI 1.49–26.10), took pulse steroid (AOR = 5.68, 95% CI 0.99–32.3), started induction therapy with prednisolone only (AOR = 85.79, 95% CI 1.16–635.0) or CYC with prednisolone (AOR = 85.79, 95% CI 1.16–635.0), completed induction therapy at 6 months (AOR = 16.35, 95% CI 1.50–180.75), achieved complete response (AOR = 200.8, 95% CI 16.5–2437.6) or partial response (AOR = 20.26, 95% CI 1.96–209.4) after 6 months of induction therapy, placed on maintenance therapy of MMF with prednisolone (AOR = 69.15, 95% CI 2.818–1442.0), or AZA with prednisolone (AOR = 72.1, 95% CI 1.16–447.0), received cotrimoxazole prophylaxis (AOR = 7.48, 95% CI 1.76–31.87), and had baseline leucopenia (AOR = 14.2, 95% CI 1.04–201.3) were more likely to achieve a complete response at their last follow-up visit as compared to the non-responders (Table 5).
On the other hand, patients who started MMF with prednisolone induction therapy (AOR = 17.55, 95% CI 1.76–174.0), completed induction therapy at 6 months (AOR = 19.47, 95% CI 1.46–258.8), and achieved partial response after 6 months of induction therapy (AOR = 32.63, 95% CI 1.45–736.0) were more likely to attain a partial response at their last follow-up as compared to the non-responders. Conversely, patients with comorbid conditions (AOR = 0.21, 95% CI 0.05–0.92) were less likely to achieve partial response as compared to the non-responders (Table 5).
Factors associated with lupus nephritis patients' survival
During bivariate Cox regression analysis, baseline serum creatinine ≥ 1.4 mg/dl (P = 0.034) and increased white blood cell (P = 0.016) were associated with an increased risk of non-response in LN patients on follow-up, whereas complete response (P = 0.000) and partial response (P = 0.000) to induction therapy were associated with decreased risk of non-response.
However, during multivariate Cox regression analysis, only response to induction therapy was significantly associated with a reduction in non-response. Accordingly, patients with complete responses at initial treatment were found to have an approximately 93.1% decreased risk of non-response as compared with patients with non-response at initial therapy. Similarly, patients with a partial response at initial treatment were found to have nearly 75.1% decreased risk of non-response as compared with patients with non-response at initial therapy (Table 6).
To support the Cox regression analysis finding, Kaplan–Meier survival analysis was performed by considering the period from treatment initiation to end of follow-up or death as the time frame. Based on Kaplan–Meier analysis, complete and partial responses to initial therapy were independent factors associated with decreased risk of non-response. The survival of LN patients with a complete response to initial therapy was greater than the survival of patients with a non-response to initial therapy (P = 0.000 by log-rank test). Similarly, the survival of LN patients with partial response during initial therapy was greater than the survival of those patients with non-response at initial therapy (P = 0.000 by log-rank test) (Fig. 1).
The 24-month survival rate for LN patients who achieved CR after induction therapy and those who achieved PR were 94.02% and 87.86%, respectively while non-responders had a survival rate of 54.17% at 24 months. Patient survivals at the end of follow-up were 91.67%, 58.93%, and 7.9% for patients with complete, partial, and non-response to initial therapy, respectively. The overall median survival time for LN patients with partial response and non-response at initial therapy was 56 months and 25 months, respectively (Fig. 1).
Discussion
This study is one of the few that assesses the treatment outcome, survival status, and associated factors of LN patients in the sub-Saharan Africa (SSA) contexts, particularly in Ethiopia. It is also the pioneer study to profoundly examine multiple factors associated with LN treatment outcome, and survival status by using a dual-center setting containing a relatively larger sample.
In this study, remission rate to treatment (complete plus partial response) is around 92.5% at the end of induction therapy with immunosuppressant drugs. This finding is in line with a study done in China in which nearly 90% of patients achieved remission after induction therapy consisting of prednisolone with either MMF or CYC21. However, it was relatively higher than the studies done in Ibn Sina University Hospital of Morocco, and Aristide Le Dante University Hospital of Senegal, in which 66% and 57.14% of patients achieved remission, respectively22,23. The discrepancy could be attributed to the differences in the selection of treatment regimen (MMF with prednisolone vs CYC alone or AZA alone), male-to-female sex ratio (0.09 vs 0.23 and 0.09 vs 0.128), and sample size (200 vs 114 and 200 vs 93). For instance, CYC alone was utilized in almost all cases of LN from Morocco due to low cost, whereas MMF was mainly utilized in our study by combining with prednisolone. Moreover, the current finding was relatively lower than a study done in India24, which reported 94.1% of remission (complete plus partial). The variation could also be attributed to differences in the inclusion criteria (age; 15–60 years vs < 18 years), minimum follow-up time (1 year vs 5 years), genetic difference, and definition of response.
At the last visit of follow-up, about 84.5% LN patients achieved remission (complete plus partial response). Out of these, 66.5% of them had a complete response [CR] while 18% had a partial response [PR]. A similar observation was noted in a study done in Italy in which 82.8% of LN patients achieved remission at the last follow-up25. However, this finding was relatively higher than the finding of a study done in Libya which reported a complete, partial, and non-response in 64.5%, 13.3%, and 22.3%, respectively26. This incongruity might be ascribed to the variation in the definition of response, magnitude of comorbidity like hypertension (38.5% vs 89.5%), choice of treatment protocol followed (ACR vs EULAR), sample size (200 vs 76), and use of adjuvant chloroquine (100% vs 0%)27. The current finding was relatively lower compared to a previous study done in Russia28, where overall remission (CR plus PR) was reported to be around 95.7%. Likewise, this is mostly due to differences in length of follow-up (5 years vs 23 years), genetics, socioeconomic status, and type of regimen selected for maintenance therapy.
Among the baseline laboratory tests, lupus serology (positive ANA and anti-dsDNA), serum creatinine, and 24-h urine protein were not significantly associated with either CR or PR in this study. These findings were consistent with a study done in Turkey8. In this study, the male gender had no statistically significant contribution to non-response, even though several studies29,30,31 identified it as a risk factor. This could be due to the small number of male participants (N = 17) in our study, and genetic or hormonal differences. Similar to a study done in Senegal, the presence of leucopenia at baseline was significantly associated with non-response23. However, this finding is not consistent with many previous studies22,26,32,33. This could be partly due to variations in laboratory test control, sample size, and the presence of infection.
In the present study, LN patients who had a severe SLE disease activity index were less likely to achieve a CR than NR as compared with patients with a moderate disease activity index. This real-world finding conforms with studies conducted in Taiwan tertiary referral center, West China Hospital of Sichuan University, and India33,34,35 but is incongruent with a study conducted in Egypt36. The incongruity might be ascribed to the higher proportion of patients receiving three days high dose pulse steroid therapy (24.5% vs 100%) and the smaller sample size (85 vs 200).
Our study differs from other studies23,26 concerning the impact of pulse steroid therapy on treatment outcomes. In our study, the use of pulse steroid therapy was significantly associated with CR though only a few patients (24.5%) received it. This finding is in agreement with studies conducted in Japan and Senegal37,38. In contrast, a study conducted in Pakistan found that pulse steroids had no statistically significant effect on LN treatment outcomes. This dispute is likely due to nearly 90% of patients receiving only oral corticosteroids after pulse steroid therapy in Pakistan while either CYC or MMF was initiated in our case39.
Our findings revealed that the presence of comorbidity is significantly associated with LN non-response. This finding was supported by a prospective study done in Egypt36, in which 81.1% of non-responders had comorbidity at the initial. Conversely, patients with comorbidity were not significantly associated with a reduction in PR in two previous studies23,33. This discrepancy could be attributed to the merging of complete and partial responses.
In this study, partial response is more likely to occur in patients taking MMF with prednisolone than in patients taking CYC with prednisolone during induction therapy. This finding was similar to a study done in the United States of America in which most patients were black African40. This is because MMF is more effective than CYC in black African patients. Prolonged duration of induction therapy (more than 6 months) favors NR when compared with 6-month therapy, possibly because of non-adherence, drug toxicity, and medication error. Using either MMF or AZA as maintenance therapy is likely associated with a statistically significant CR compared with prednisolone alone. This finding is consistent with various international guidelines4,13.
LN patients who did not respond completely or partially to induction therapy after 6 to 12 months were significantly more likely to have non-response after long-term follow-up than their counterparts. Related studies have found that patients who achieve a partial or complete response after induction therapy had a greater CR than non-responders after long-term follow-up28,41. In this study, LN patients taking prophylactic cotrimoxazole achieved a statistically significant CR better than NR as compared to patients not taking prophylaxis. This is due to the benefit of cotrimoxazole in preventing infections caused by the immunosuppressant drugs used in LN42. In various studies, the intention of using cotrimoxazole was as a prophylaxis for opportunistic infections, but in the current study, we come up with a new hypothesis of using cotrimoxazole to increase the complete response in patients due to the reduction of antibodies related to B-cell productions secondary to bone marrow suppressions.
Survival of patients attaining complete response at the last follow-up visit was more than 90%. This finding was in keeping with two previous studies16,43. In this study, 14.4% of patients were non-responders at the end of the follow-up visit. This finding is lower than previous studies done in Italy25 (17.2%) and Chicago16 (32.0%) but higher than a study done in Egypt36 (12.9%). The incongruity could be ascribed to the differences in sample size, class of LN, the definition of remission, diagnosis by biopsy, age, and genetics.
Our survival analysis revealed that patients attaining complete response after induction therapy were shown to have an excellent prognosis. The current study finding unveiled that those patients achieving complete and partial responses to induction therapy decreased the risk of non-responders by 93.1% and 75.1%, respectively. So, non-response to induction therapy negatively influenced patient survival. This finding was consistent with three previous studies16,25,28.
Our study had the strength of being a dual center with a relatively higher number of patients compared with most other studies. Moreover, most of our patients have stayed on follow-up for more than 24 months and treatment outcomes were evaluated individually. Nevertheless, our study may have been limited by its retrospective study design and variation of treatment regimens used to treat LN which resulted in variations in treatment outcomes. Besides this, around 28% of patients were diagnosed with LN without renal biopsy in our study even though renal biopsy was the gold standard diagnostic method for LN. Furthermore, the reasons for those patients who have been lost to follow-up have not been captured. Lastly, due to the high cost and interrupted supply of immunosuppressive medications, some LN patients were shifted from one regimen to another which may have impacted treatment outcomes.
Conclusion
Treatment of LN sounds better in terms of treatment outcome and patient survival in our study setting. More than three-fourths of LN patients respond to drug therapy. Our findings revealed that the use of pulse steroids, complete response or partial response at the induction therapy, administration of MMF with prednisolone, AZA with prednisolone, and use of prophylactic cotrimoxazole were significantly associated with a favorable treatment outcome whereas the presence of leucopenia, comorbidity, induction duration more than six months, non-response to induction therapy and severe disease index were significantly associated with lower probability of complete or partial response (Supplementary Information S1).
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- ANA:
-
Antinuclear antibodies
- AOR:
-
Adjusted odds ratio
- AZA:
-
Azathioprine
- COR:
-
Crude odds ratio
- CR:
-
Complete response
- CYC:
-
Cyclophosphamide
- ESRD:
-
End stage renal disease
- LN:
-
Lupus nephritis
- NR:
-
Non-response
- PR:
-
Partial response
- TASH:
-
Tikur Anbessa specialized hospital
- SLE:
-
Systemic lupus erythematous
- SPHMMC:
-
Saint Paul Hospital Millennium Medical College
References
Simmons, C., Malherbe, M., van Rensburg, B. J. & Joubert, G. Clinical feautures of patients with systemic lupus erythematosus (SLE) attending the SLE outpatient clinic at Universitas Hospital in Bloemfontein South Africa. SA Fam. Pract. 50, 68–75 (2008).
Hong, W., Ren, Y.-L., Chang, J., Luo, G. & Ling-Yun, S. A systematic review and meta-analysis of prevalence of biopsy-proven lupus nephritis. Arch. Rheumatol. 33, 17 (2018).
Sada, K.-E. & Makino, H. Usefulness of ISN/RPS classification of lupus nephritis. J. Korean Med. Sci. 24, S7–S10 (2009).
Hahn, B. H. et al. American College of Rheumatology guidelines for screening, treatment, and management of lupus nephritis. Arthritis Care Res. 64, 797–808 (2012).
Fanouriakis, A. et al. (BMJ Publishing Group Ltd, 2020).
Alsuwaida, A. O. et al. The long-term outcomes and histological transformation in class II lupus nephritis. Saudi Med. J. 39, 990 (2018).
Rašić, S. et al. Long-term outcome of patients with lupus nephritis: a single center experience. Bosn. J. Basic Med. Sci. 10, S63 (2010).
Gunes, C., Keles, M., Uyanik, A., Cetinkaya, R. & Sari, R. A. Treatment results of patients with lupus nephritis: A single center’s experience. Euras. J. Med. 42, 132 (2010).
Navarro, D. Treatment of lupus nephritis-past, present and (near) future. Portug. J. Nephrol. Hypertension 34, 42–50 (2020).
Davidson, J. E. et al. Renal remission status and longterm renal survival in patients with lupus nephritis: A retrospective cohort analysis. J. Rheumatol. 45, 671–677 (2018).
Gasparotto, M., Gatto, M., Binda, V., Doria, A. & Moroni, G. Lupus nephritis: Clinical presentations and outcomes in the 21st century. Rheumatology 59, v39–v51 (2020).
Nakano, M. et al. Delayed lupus nephritis in the course of systemic lupus erythematosus is associated with a poorer treatment response: A multicentre, retrospective cohort study in Japan. Lupus 28, 1062–1073 (2019).
Rovin, B. H. et al. KDIGO 2021 clinical practice guideline for the management of glomerular diseases. Kidney Int. 100, S1–S276 (2021).
Hanaoka, H. et al. Comparison of renal response to four different induction therapies in Japanese patients with lupus nephritis class III or IV: A single-centre retrospective study. PLoS One 12, e0175152 (2017).
Fangtham, M. & Petri, M. 2013 update: Hopkins lupus cohort. Curr. Rheumatol. Rep. 15, 360 (2013).
Chen, Y. E., Korbet, S. M., Katz, R. S., Schwartz, M. M. & Lewis, E. J. Value of a complete or partial remission in severe lupus nephritis. Clin. J. Am. Soc. Nephrol. 3, 46–53 (2008).
Abate, D., Aman, M. A., Nasir, B. B., Gebremariam, G. T. & Fentie, A. M. Assessment of quality of care using information on patient satisfaction at adult oncology Center of Tikur Anbessa Specialized Hospital, Ethiopia: A cross-sectional study. Patient Prefer. Adher. 14, 847 (2020).
Hailu, G.-M. T., Hussen, S. U., Getachew, S. & Berha, A. B. Management practice and treatment outcomes of adult patients with Lupus Nephritis at the Renal Clinic of St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia. BMC Nephrol. 23, 214 (2022).
Gladman, D. D., Ibanez, D. & Urowitz, M. B. Systemic lupus erythematosus disease activity index 2000. J. Rheumatol. 29, 288–291 (2002).
Dooley, M., Aranow, C. & Ginzler, E. Review of ACR renal criteria in systemic lupus erythematosus. Lupus 13, 857–860 (2004).
Chan, T.-M., Tse, K.-C., Tang, C.S.-O., Mok, M.-Y. & Li, F.-K. Long-term study of mycophenolate mofetil as continuous induction and maintenance treatment for diffuse proliferative lupus nephritis. J. Am. Soc. Nephrol. 16, 1076–1084 (2005).
Haddiya, I. et al. Features and outcomes of lupus nephritis in Morocco: analysis of 114 patients. Int. J. Nephrol. Renovasc. Dis. 6, 249 (2013).
Mansour, M. et al. Prognostic aspects of Lupus Nephritis at Aristide Le Dantec University Hospital in Dakar. Open J. Nephrol. 8, 124–132 (2018).
George, J. et al. Lupus nephritis in Indian children: Flares and refractory illness. Indian Pediatr. 55, 478–481 (2018).
Moroni, G. et al. The long-term outcome of 93 patients with proliferative lupus nephritis. Nephrol. Dial. Transplant. 22, 2531–2539 (2007).
Zaid, F. & Salem, M. Predictive Factors and Long Term Outcome in Lupus Nephritis in Libya. Rheumatology (Sunnyvale) 8, 2161–1149.1000234 (2018).
Kasitanon, N., Fine, D., Haas, M., Magder, L. & Petri, M. Hydroxychloroquine use predicts complete renal remission within 12 months among patients treated with mycophenolate mofetil therapy for membranous lupus nephritis. Lupus 15, 366–370 (2006).
Zakharova, E. V., Makarova, T. A., Zvonova, E. V., Anilina, A. M. & Stolyarevich, E. S. Immunosuppressive treatment for lupus nephritis: long-term results in 178 patients. BioMed Res. Int. 2016 (2016).
Hsu, C. et al. Age-and gender-related long-term renal outcome in patients with lupus nephritis. Lupus 20, 1135–1141 (2011).
de Carvalho, J. F., Do Nascimento, A. P., Testagrossa, L. A., Barros, R. T. & Bonfá, E. Male gender results in more severe lupus nephritis. Rheumatol. Int. 30, 1311–1315 (2010).
Schwartzman-Morris, J. & Putterman, C. Gender differences in the pathogenesis and outcome of lupus and of lupus nephritis. Clin. Dev. Immunol. 2012 (2012).
Momtaz, M. et al. Retrospective analysis of nephritis response and renal outcome in a cohort of 928 Egyptian lupus nephritis patients: A university hospital experience. Lupus 26, 1564–1570 (2017).
Shivaprasad, S., Umesh, L., Ravi, S., Niranjan, M. & Shivanagouda, R. Clinical spectrum and short-term outcomes of lupus nephritis: Experience from a state run tertiary care centre in southern India. Int. J. Med. Res. Health Sci. 5, 431–437 (2016).
Chen, Y. et al. Combination immunosuppressant therapy and lupus nephritis outcome: A hospital-based study. Lupus 28, 658–666 (2019).
Tang, Y. et al. Clinicopathological and outcome analysis of adult lupus nephritis patients in China. Int. Urol. Nephrol. 47, 513–520 (2015).
Abdulrahman, M. A. & Sallam, D. E. Treatment response and progression to end stage renal disease in adolescents and young adults with lupus nephritis: A follow up study in an Egyptian cohort. Egypt. Rheumatol0 42, 189–193 (2020).
Tanaka, H., Tateyama, T. & Waga, S. Methylprednisolone pulse therapy in Japanese children with severe lupus nephritis. Pediatr. Nephrol. 16, 817–819 (2001).
Diagne, S. et al. Sun-428 lupus nephritis at aristide le dantec university hospital in dakar (senegal) about 99 cases: Histopathological, therapeutic, pronostic and evolutive aspects. Kidney Int. Rep. 5, S373–S374 (2020).
Rabbani, M. A. et al. Survival analysis and prognostic indicators of systemic lupus erythematosus in Pakistani patients. Lupus 18, 848–855 (2009).
Ginzler, E. M. et al. Mycophenolate mofetil or intravenous cyclophosphamide for lupus nephritis. N. Engl. J. Med. 353, 2219–2228 (2005).
Bertsias, G. K. et al. Joint European League Against Rheumatism and European Renal Association-European Dialysis and Transplant Association (EULAR/ERA-EDTA) recommendations for the management of adult and paediatric lupus nephritis. Ann. Rheum. Dis. 71, 1771–1782 (2012).
Ye, W.-L. et al. Underlying renal insufficiency: the pivotal risk factor for Pneumocystis jirovecii pneumonia in immunosuppressed patients with non-transplant glomerular disease. Int. Urol. Nephrol. 48, 1863–1871 (2016).
Korbet, S. M. et al. Factors predictive of outcome in severe lupus nephritis. Am. J. Kidney Dis. 35, 904–914 (2000).
Acknowledgements
We would like to extend our sincere gratitude to the data collectors for their immense support throughout the data collection period and hospital staff for their pleasurable cooperation in the expert review of the data collection instruments.
Author information
Authors and Affiliations
Contributions
O.S.M. and O.A. conceptualized and designed the study, wrote the original manuscript, and performed analysis and interpretation of data. B.W. assisted in the content validation of the data collection instruments, study design, and manuscript evaluation. M.H. edited and wrote the final version of the manuscript. All authors have made an intellectual contribution to the work and have approved the final version of the manuscript for submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Aliyi, O., Worku, B., Hassen, M. et al. Treatment outcome and survival status among adult patients treated for lupus nephritis in selected tertiary hospitals of Ethiopia. Sci Rep 14, 5603 (2024). https://doi.org/10.1038/s41598-024-56317-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-56317-6
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.