Abstract
When pregnancy occurs in adolescence, the growth and development of the mother and fetus may be impaired due to strong competition for nutrients between the still-growing adolescent and the fetus. Pregnant adolescents constitute an underserved population; they lack adequate nutritional knowledge. Therefore, this study investigated the effect of nutritional behavior change communication (NBCC) through alliance for development (AFD) on the nutritional status and gestational weight gain (GWG) of pregnant adolescents. A two-arm parallel cluster randomized controlled community trial was conducted in the West Arsi Zone, central Ethiopia, from August 2022 to July 2023. The nutritional status of the pregnant adolescent was assessed using mid-upper arm circumference. Weight was measured at baseline and at the end of the intervention. A total of 207 and 219 pregnant adolescents participated in the intervention and control clusters, respectively. The intervention started before 16 weeks of gestation, and the intervention group attended four NBCC sessions. The NBCC was based on the health belief model (HBM) and was given at the participants’ homes with their husbands. The NBCC intervention was delivered by AFDs and community-level health actors. Pregnant adolescents in the control group received routine nutrition education from the health care system. A linear mixed-effects model and difference in difference (DID) were used to measure the intervention effect after adjusting for potential confounders. After the implementation of the trial, the mean mid-upper arm circumference (MUAC) in the intervention arm significantly increased from baseline (p ≤ 0.001), 23.19 ± 2.1 to 25.06 ± 2.9 among intervention group and 23.49 ± 2.1 to 23.56 ± 2.0 among control group and the mean difference in the MUAC (DID) was 1.89 ± 2 cm (p ≤ 0.001); the mean GWG in the intervention arm significantly increased from baseline; 51.54 ± 4.7 to 60.98 ± 4.6 among intervention group and 52.86 ± 5.27 to 58 ± 5.3 among control group; the mean GWG in the intervention group was 9.4 kg, and that in the control group was 5.14 kg, and the difference in difference was 4.23 kg and this was statically significant p ≤ 0.001). This study demonstrated that the use of the HBM for NBCC delivered through the AFD was effective at improving the nutritional status and GWG of pregnant adolescents. These results imply the need for the design of model-based nutritional counseling guidelines.
Clinical trial registration: PACTR202203696996305, Pan African Clinical Trials Registry, date of first registration: 16/03/2022.
Similar content being viewed by others
Introduction
When pregnancy occurs in adolescence, the growth and development of the mother and fetus may be hampered due to strong competition for nutrients between the still-growing adolescent mother and her fast-developing fetus, commonly known as “nutrient partitioning”1,2. Alternative theories that may be used in conjunction with nutrient partitioning include the idea that due to gynecological immaturity, safe delivery is sacrificed to allow for optimal fetal growth3,4.
A desirable amount of weight to be gained is associated with optimal outcomes for mothers and infants. A Joint FAO/WHO/UNU Expert Consultation report recommended that healthy, well-nourished women should gain 10–14 kg during pregnancy. This will increase the likelihood of giving birth to full-term infants with an average birth weight of 3.3 kg and to lower the risk of fetal and maternal complications5,6.
Behavior change communication (BCC) refers to the methodical application of communication that has a positive impact on people’s understanding, attitudes, and behaviors. This encourages people to take charge of their own health. BCC can promote dietary improvement and account for individual health beliefs and practices7. Nutrition behavior change communication (NBCC) is an approach for changing nutrition-related behaviors through the use of different strategies, techniques, and teaching materials to bring about practice changes that lead to improved health through optimal feeding practices and improved dietary habits8. BCC is a straightforward strategy for altering behavior. It differs from traditional information education communication (IEC) because, in contrast to BCC, IEC considers only spreading awareness and providing information9.
In low- and middle-income (LMIC) countries, as of 2019, there were approximately 21 million pregnancies among teenagers aged 15–1910. Regarding the magnitude of child marriage in Eastern and Southern Africa, Ethiopia is among the top three nations. The vast majority of people give birth during adolescence after marrying as children11,12,13. The intergenerational effect of malnutrition has been recognized as a major contributing factor to Ethiopia’s inclusion among countries with the highest rates of maternal and newborn mortality in the world14,15.
Pregnancy involves a variety of adverse reactions, including nausea, vomiting, fatigue, heartburn, constipation, hemorrhoids, food cravings and aversions16. These problems may be alleviated by the NBCC. Many expectant mothers in developing nations restrict their food intake for different reasons, such as through the false belief that smaller babies will have fewer delivery complications and through the belief that cultural influences will increase the size and difficulty of delivery17,18. This illustrates the lack of adequate information and false beliefs about dietary behaviors among expectant mothers19,20,21.
AFDs (alliances for development), originally known as women development armies [WDAs], are community health volunteers who are in charge of 30 houses, each of which has one to five networks. Six different one-to-five connections formed one WDA22. Ethiopia is an excellent example of a community health initiative with a well-structured health extension package. The country's primary healthcare unit (PHCU) is at the forefront of PHC23. A study conducted on the contribution of the Women’s Development Army or by its new name, AFDs, to maternal and child health showed that they have contributed to the improvement of child immunization service use, the minimization of maternal mortality, improved skilled delivery attendance and skilled ANC24, an experience that can be extended to nutrition education, and other developing countries might adapt it.
A systematic review and meta-analysis conducted in 2021 showed that the pooled estimated prevalence of teenage pregnancy in Ethiopia was 23.59%25. There are several efforts from the government of Ethiopia to address adolescent health and nutritional problems. For example, adolescent and youth health (AYH) programmes, including those focused on sexual and reproductive health (SRH) and youth development, have gained attention26 The National Adolescent and Youth Health (AYRH) strategy of 200727, Comprehensive National Adolescent and Youth Health (AYH) strategy of 201628 and National Nutrition Programme (NNP II) 2016–202029; however, these programmes were not effective at the expected level because adolescents and youth-related interventions in Ethiopia are uncoordinated, fragmented under various ministries, lacked effective policy implementation, underfunded, project oriented, and lacked meaningful engagement from young people30.
Compared to adult women, pregnant at any age during adolescence is associated with a greater possibility of experiencing eclampsia, puerperal endometritis anemia, systemic infections, low birthweight, preterm delivery, and neonatal mortality31,32,33. Pregnant adolescents constitute an underserved population; therefore, they can benefit greatly from receiving prenatal health and nutritional education. Adolescents often experience unplanned pregnancy. Several studies have shown that as few as 27% of pregnant adolescents receive ANC services34,35, which makes them even more vulnerable to undernutrition and other adverse health outcomes. To the best of our literature search, no community-based interventional study has investigated the effect of a behavioral change model-based NBCC through community-level health volunteers (AFDs) on nutritional status and weight gain among pregnant adolescents; therefore, this study can help policymakers and planners improve nutritional counseling practices at local and national levels.
Methods
Study design, setting and participants
This study was a cluster randomized controlled community trial with a two-arm parallel design that lasted for one year. This study was conducted in the West Arsi Zone, Oromia region, Central Ethiopia; 250 km from Addis Ababa, the nation's capital. There are 16 districts in the West Arsi Zone (13 rural districts and three towns). A total of 2,929,894 people were estimated to live there by mid-2022. A total of 12,556 km2 make up the zone, which has a climate of 45.5% highland, 39.6% medium land, and 14.9% lowland36. According to the Zonal report of 2022, there are 417 public health facilities, 5 of which are hospitals, 324 of which are health posts, 88 of which are health centers, and 203 of which are private medium and higher clinics, including one nongovernmental hospital and two private hospitals providing health services. At least one sexual and reproductive health (SRH) service was utilized in the zone; in 2019, it was 58.6%37. The study was conducted between August 2022 and July 2023. This trial included pregnant adolescents before 16 weeks of pregnancy who intended to remain in the study region until delivery. Adolescents who refused to give their informed consent were not included in the study.
Sample size determination and sampling technique
The sample size was calculated using G*Power 3.0.10. The required sample size was determined using the following assumptions: a 95% confidence interval, a 5% margin of error, 80% power, and an intra-cluster correlation (ICC) of 0.03 (based on a comparable published study ICC)38 for the difference between two independent means (two groups). A 10% loss to follow-up was considered, and a design effect of two was employed. A total of 488 people constituted the computed sample sizes. As a result, both intervention and control groups of 244 pregnant adolescents were included. Twenty-eight clusters were used, and the average cluster size was 19. A single-stage cluster sampling technique was applied in this study.
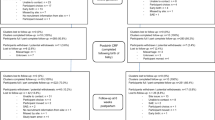
Recruitment, randomization and intervention allocation
Five of the zone's 16 districts had nutritional education interventions; thus, they were excluded from the study. Four districts, namely, Dodola Rural, Adaba, Gedeb Hasasa, and Siraro, were chosen from among the remaining eligible districts by simple random sample (SRS) technique. Samples of nonadjacent kebeles (clusters) from the four districts were chosen using SRS. Six clusters each from the Dodola Rural and Adaba districts, as well as eight clusters each from the Gedeb Hasasa and Siraro districts, were selected based on their proportion to size allocation and considering cluster allocation in the intervention and control groups. Kebeles (the smallest administrative entity in Ethiopia) were used as the randomization unit (clusters). Clusters for the intervention and control groups were distributed using the lottery (SRS) approach. The Consolidated Standards of Reporting Trials (CONSORT) guidelines were used to report the results (Fig. 1).
A cluster randomized trial was used to avoid message contamination because pregnant teenagers in the same cluster were likely to communicate and discuss intervention messages. To avoid information leakage, all pregnant adolescents who met the criteria in one cluster were enrolled in the same arm (either the intervention or control arm). Buffer zones (none selected clusters) were also positioned39,40.
The study included all pregnant teenagers who met the inclusion criteria. The study participants were screened and enrolled by nurses, and the clusters were randomly assigned. A house-to-house survey was performed, and pregnant teenagers who met the criteria were screened by first date of their last menstrual period and urine HCG test was used to confirm their pregnancy. Urine-based pregnancy tests and urine HCG levels were used. The procedure involved dipping a test strip into a urine sample. The test strip contained chemicals, monoclonal antibodies that reacted to the presence of the pregnancy hormone HCG (human chorionic gonadotropin). The results are displayed as lines on the test strip.
Intervention
The intervention strategy used in this study was a community-based nutritional behavioral change communication intervention (NBCC) based on the Health Belief Model (HBM). The recommendations of the World Health Organization, the blended training module on nutritional counseling developed by the Federal Ministry of Health of Ethiopia, EFDRE/MOH, and related interventional studies41,42,43,44 served as the basis for preparing the intervention package. Additionally, the baseline study, conducted at the start of this study, served as a direction for the development of intervention tools; the NBCC included the husbands of the pregnant teens and a demonstration of how to prepare meals. The intervention items included a training manual for nutrition counsellors, leaflets with key messages for pregnant adolescents and their families, and counseling checklist cards.
The intervention method was tested for one week in an environment similar to the research site, and adjustments were made in light of the results. The counseling manual's core contents included eating a range of foods, especially iron-rich foods, animal products, fruits, and vegetables, and increasing the meal frequency and portion size as gestational age increased. The main components of counseling guidance also included taking iodized salt and iron/folic acid supplements. Additional messages about the core components included reduced workload, day rest, the use of impregnated bed nets, and the use of medical services.
It was also emphasized how undernutrition can harm a person’s development and how vulnerable pregnant adolescents need to eat. The benefits of eating enough meals that are diverse and the challenges in maintaining a balanced diet were also highlighted in the NBCC guidebook. Throughout her pregnancy, each pregnant adolescent attended four counseling sessions. Personalized NBCC based on trimester was provided during home visits. Counselors used a client-centered approach to identify specific dietary preferences and needs. Before allowing the teenagers to choose easily accessible, agreeable, and affordable guidance at their location, counselors considered the needs of the pregnant adolescents, their household income, and any gaps they had discovered. Counseling was conducted using the GALIDRAA approach (Greet, Ask, Listen, Identify, Discuss, Repeat, Agree, and Appoint)45.
A counseling guide that included the necessary information was used to conduct each counseling session for the NBCC, which lasted 45–60 min. The first appointment concentrated on the basics of nutrition, food groups, selecting foods that provide a balanced diet, showing how to prepare meals, the frequency of meals, and the use of iodized salt before 16 weeks of pregnancy. The second and third counseling sessions, which covered the whole of the counseling manual, were offered during the second trimester. Final counseling, which focuses on weight gain and incorporates all the module's important messages, was provided based on the gaps that were discovered during the previous trimesters of pregnancy.
Each pregnant adolescent in the intervention arm received a leaflet containing the key themes in Afan Oromo and Amharic (local languages) and appropriate images. Anyone at home who could read was asked to read the leaflet to the pregnant adolescent if the adolescent could not read it.
Health extension workers chose 14 AFD [formerly known as WDAs] counselors based on their performance and prior involvement with public health services. The 14 AFDs were carefully supervised by four BSc nurses. Role-playing exercises and fieldwork using the training handbook were part of rigorous one-week training for counselors and supervisors. After the intervention had been in place for 2 months, the supervisors and counsellors received three additional days of training to ensure that the providers continued to adhere to standardized practices.
Intervention fidelity
Criteria were created to assess the integrity of the intervention based on the best practice suggestions developed by the National Institutes of Health Behavioral Change Consortium46. The criteria47, included checklists to assess the intervention design, counselor training, counseling process, receipt of the intervention, and implementation of the skills picked up during the intervention. Nonadjacent clusters were selected to prevent information contamination. The intervention and control groups had an equal number of clusters from each district to balance differences.
The intervention strategy was tested before the experiment. Additionally, each pregnant adolescent received the same number and frequency of counseling sessions, and the lengths of interactions within the intervention group were comparable to standardize the method. Counselor training was given in a group environment using a training booklet, role-playing, and simulated counseling sessions. Tests administered before and after training, as well as a practical evaluation, were utilized to evaluate counselors’ skills and knowledge. The process observer graded the counselors using a “yes/no” rating system and looked at things such as using a counseling guide, covering the whole subject, the duration and frequency of counseling, preparation, accuracy, and the counselor’s ability to respond to questions appropriately. Pregnant adolescents’ understanding of food throughout pregnancy was assessed through interviews via checklists to determine their knowledge of the main components of the intervention.
Participants, counselors, and data collectors were blinded to the study’s objective; participant allocation concealment was impractical given the nature of the intervention. Until the analysis was complete, the groups were given a unique nonidentifiable number that also served to blind the data entry clerk. The counseling process was supervised by the main investigator and counseling supervisors.
Data collection procedure and measurements
The primary outcome of this study was nutritional status as measured by the MUAC, while the secondary outcome was GWG. The mid-upper arm circumference (MUAC) is the recommended assessment tool for nutritional status because of its simplicity and sensitivity in detecting undernutrition. In low-resource settings, where girls have minimal subcutaneous fat, it is the preferred measurement method because changes in the MUAC are more likely to reflect changes in muscle mass48. It has been demonstrated that a low maternal MUAC is useful for detecting unfavorable delivery outcomes, such as intrauterine growth restriction, preterm birth, and asphyxia at birth49. The left mid-upper arm circumference (MUAC) was measured at the anatomical landmark at the midpoint of the acromion and olecranon processes of the nondominant hand, with the palm facing upward and the women's elbows flexed to 90°. The measurements were taken twice by employing inelastic MUAC tape and interpreting the measurements to the nearest 0.1 cm.
A pretested structured questionnaire was used to obtain the data. Sociodemographic characteristics, meal frequency, use of medical services, types of diet, and Household Food Insecurity Access Scale (HFIAS) scores were collected. Six clinical nurses and two master of public health (MPH) holders worked as data collectors and supervisors, respectively. Pregnancy tests were performed by three female laboratory technologists. The data collectors conducted in-person interviews with the participants at their homes to administer the questionnaire. To the best extent possible, the adolescent's privacy was protected by prohibiting access to the site where the interviews took place.
According to the Food and Nutrition Technical Assistance (FANTA) III recommendation from the United States Agency for International Development (USAID) and the Food and Agricultural Organization (FAO), dietary intake was determined using 24-h recalls50. The objective was to ascertain whether the meals consumed by pregnant teenagers varied. Ten food groups were used to compute dietary diversity; grain, dairy, meat, white roots and tubers; nuts and seeds; eggs; dark green leafy vegetables; poultry and fish; plantains; other fruits and other vegetables; and other fruits and vegetables high in vitamin A are among the ten food groups listed in the recommendations. Adequate dietary diversity is achieved if pregnant adolescents consumed food from 5 or more food groups within 24 h of day/before data collection; minimum dietary diversity for women (MDD-W) was used51,52. The participants were asked to remember every meal they consumed during the previous 24 h; both inside and outside the home. The participants were also asked if they could remember any between-meal snacks they may have consumed. Food items received a “1” rating if consumed during the reference period and a “0” rating if not.
The HFIAS (Household Food Insecurity Access Scale) Guideline53 was used to assess food security. The HFIAS was used to evaluate the households’ level of food security and included nine questions. Prior to this, the questions were validated for use in developing nations54. Food-secure households experienced fewer food insecurity indicators than did the first two food insecurity indicators. Households that experienced between two and ten, eleven to seventeen, or more than seventeen food insecurity indicators were considered mildly, moderately, or severely food insecure, respectively.
The household’s wealth index was derived using principal component analysis (PCA), taking into account access to a latrine, a water source, household durable assets, and agricultural land. The responses to the none dummy variables were all split into three groups. A code of 1 is allocated to the highest rating. The two smaller digits, however, were given a code of 0. Using variables with a commonality value larger than 0.5, PCA factor scores were produced. The first primary component score for each family is kept to calculate the wealth score. Quintiles of the wealth score were created to classify households as poorest, poor, medium, rich, or richest55.
The autonomy of the pregnant adolescents was evaluated using eight questions. Code one was provided for each question when a decision was made by the girl, by herself or jointly with her husband; otherwise, code zero was provided. The mean score was used to determine the pregnant adolescent's decision-making capacity44.
Data management and analysis
The data were entered using the Kobo Toolbox and exported to SPSS version 25 for analysis. The baseline variations in the two groups’ sociodemographic characteristics were examined using a Chi-square test. Paired t tests and independent t tests were used to determine within- and between-group differences.
The effect of the intervention on changes in the nutritional status and gestational weight gain of pregnant adolescents over time was estimated using a linear mixed-effects model. This model was chosen because of the repeated assessments (pre- and postintervention) and the clustering of individuals, which allowed us to explain how the results were correlated. The Akaike information criterion (AIC) was used to help us choose the best statistical model. The model that displayed the lowest AIC was selected. The bivariate linear mixed regression model's variables with p 0.2 were chosen as potential candidates for the multivariate linear mixed model analysis. By analyzing how time and the intervention interacted, the effectiveness of the intervention was evaluated.
Participants were examined as random effects during model fitting. A linear mixed-effects model also makes it possible to manage the impact of various confounding variables. The intra-cluster correlation coefficient of the final model was 0.04, indicating that constructing a third-level model was not necessary. The intercept-only model was created initially. To take into consideration time-invariant variables at the individual level, a two-level model was fitted. The effect of intervention was estimated by testing the interaction term between treatment allocation and time.
Ethical considerations
Ethical approval was obtained from the Jimma University IRB/ethics committees with reference number JUIH/IRB/194/22, and the Oromia Regional Health Office provided support. All methods were performed in accordance with the relevant guidelines and regulations; the study was performed in accordance with the Declaration of Helsinki. Each study participant received a thorough description of the study's title, goal, protocol, and duration, as well as the potential risks and benefits, prior to providing informed consent. Each teenager provided verbal, written, and signed informed consent prior to any interview or measurement. Informed consent was obtained from the LAR (legally authorized representative) for study participants aged 18 years and younger. Participants were made aware of the publication of their anonymous comments. Informed consent was obtained from participants prior to the commencement of interviews. The researcher remained truthful to the academic and ethical requirements. Finally, the researcher kept the data in a locked file cabinet in a safe place after the completion of the study. Informed consent was obtained from both the adolescent and their husband or parents. Finally, any ethical issues that arose during this research were resolved through discussion between the researcher and JU’s IRB.
Results
The overall follow-up of the study participants throughout the trial was summarized in the CONSORT guideline flow chart (Fig. 1).
Sociodemographic characteristics of pregnant adolescents
Of the 459 participants initially sampled, 426 (IG = 207, CG = 219) pregnant teenage participants in this study followed the protocol exactly and were included in the analysis. The mean follow-up week was 15 weeks. The sociodemographic features of the intervention and control groups did not significantly differ at baseline according to the Chi-square test (p > 0.05). The baseline characteristics of the pregnant adolescents are shown in Table 1.
Health belief model construct scores and their correlation with the MUAC and GWG
At baseline, there was no significant difference in the HBM construct scores between the intervention and control groups. All the HBM constructs had a significant positive correlation with the nutritional status and GWG of the pregnant women, except for the perceived barrier (p < 0.05) (Table 2).
Effect of nutritional behavioral change communication on the nutritional status of pregnant adolescents
At baseline, there was no statistically significant difference in the mean MUAC (23.19 ± 2.1 vs 23.49 ± 2.1, p = 0.20) between the two groups. After the implementation of the trial, the mean MUAC in the intervention arm significantly increased from the baseline (p = < 0.001) (Table 3).
The variance in the individual-level residual errors or variability in the average MUAC across individuals was 2.79, which was statistically significant (p = < 0.001). The intraindividual correlation coefficient was 0.55, which indicated the importance of accounting for individual-level time-invariant variables (fitting a two-level model). After controlling for food security, wealth index, DDS, and meal frequency, the intervention group showed a significant improvement in nutritional status at the end of the study (p < 0.01) (Table 4).
Effect of nutritional behavioral change communication on gestational weight gain (GWG) in pregnant adolescents
At baseline, there was no statistically significant difference in the mean GWG in kg (52.86 ± 5.27 vs 51.54 ± 4.7, p = 0.34) between the two groups. After the implementation of the trial, the mean GWG in the intervention arm significantly increased from baseline. The mean weight gain was 9.4 kg in the intervention group and 5.14 kg in the control group; the difference was 4.23 kg, and this difference was statistically significant (p = < 0.001) (Table 3).
The variance of the individual-level residual errors of the average GWG across individuals was 5.53, which was statistically significant (p = < 0.001). The intraindividual correlation coefficient was 0.139, which indicated the importance of accounting for individual-level variables (fitting a two-level model). After controlling for age, occupation, DDS, female decision-making and meal frequency, the intervention group showed significant improvement in GWG at the end of the study (β = 5/59, p < 0.01) (Table 5).
Discussion
This study showed that the nutritional status and GWG of pregnant adolescents were improved by NBCC delivered through AFDs using the HBM. The mean MUAC and GWG of adolescents in the intervention group were significantly greater than those of adolescents in the comparison group. These results persist after controlling for potential confounders.
The finding on improvement of nutritional status is consistent with those of Eastern Shoa Zone, Ethiopia44; West Gojjam Zone, Ethiopia43; Lahore, Pakistan56, and Iran57, who reported significant improvements in the nutritional status of pregnant individuals who attended nutritional education. A possible explanation for these findings is that human behavior can be changed by well-designed adequate nutritional education, which ultimately leads to improvements in nutritional status and better health.
Another important finding is that the NBCC resulted in significant improvement in the GWG of pregnant adolescents within the recommended weight gain range, and these results are consistent with other research58,59,60. This might be because the NBCC made participants change their perception and increase their understanding of good nutrition.
For the HBM constructs, perceived barriers were the main problem among participants, and perceived benefits brought about more significant changes. This finding is consistent with the findings of other studies61,62,63. Perceived barriers are often the most predictive constructs and are often more difficult to change than other constructs; therefore, more attention needs to be given to perceived barriers. Addressing perceived barriers often requires considering and addressing the broader context in which the behavior occurs. Perceived barriers are influenced by various contextual factors, such as social, cultural, economic, and environmental factors64,65.
The findings from this study provide some evidence that carefully selected, intensively trained, and closely supervised AFDs can be used actively in the health care system for NBCC and other similar health care services, thereby decreasing the overload on health care providers. These are promising findings, especially for developing countries, where the health care provider-to-population ratio is very small61 and where community-level actors such as AFDs can play great roles.
It is not possible to solve nutritional problems in a sustainable way through supplementation in the form of capsules or tablets or nutritional therapeutic interventions. It would be too difficult to organize, and the costs would be too high; therefore, such a model-based NBCC intervention would lead to sustainable improvements in the nutritional status and overall health of mothers and their fetuses. Community health workers (CHWs) or AFDs are critical for improving access to different health services, as this study revealed that they can contribute significantly to NBCC interventions and health policy makers. Government and nongovernmental organizations need to continue actively involving them in organized ways with periodic performance measurements and improvements in their knowledge and skills.
There are several possible explanations for the significant improvement in nutritional status and GWG resulting from the NBCC intervention in this study; these include the use of HBM, husbands’ participation in education sessions, the use of the GALIDRAA counseling technique, teaching aids such as leaflets, cooking demonstration techniques and providing trimester-based nutrition education.
Once a pregnancy occurs in adolescence, it is desirable to successfully manage it by proper nutrition and all ANC services. Further studies are needed to explore what other behavioral change communication models can be used. These findings have wider practical implications for the need to implement adolescent nutrition guidelines to prevent intergenerational cycles of malnutrition that occur during adolescent pregnancy66. The results also imply the great potential of leveraging existing community-level structures, such as AFDs, for improving adolescent nutrition during pregnancy.
The strengths of this study include the use of community-based theory-based NBCC, cooking demonstrations, and the involvement of pregnant adolescents in the NBCC; however, the limitations includes, except for those concerning the measurement of MUAC, others were based on the pregnant adolescents’ recall, self-reports, and honesty in answering the questions.
Conclusion
This study demonstrated that HBM-based NBCC combined with husband involvement through AFDs was effective at improving the nutritional status and gestational weight gain of pregnant adolescents. Utilizing AFDs ensures that the NBCC is a sustainable and low-cost intervention. Thus, it is recommended that the HBM be included in nutritional counseling guidelines. This reproducible NBCC intervention may be scaled up and sustained at a low cost through existing health systems and community structures.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- AFD:
-
Alliance for development
- AIC:
-
Akaike information criterion
- BCC:
-
Behavior change communication
- DID:
-
Difference in difference
- FAO:
-
Food and Agricultural Organization
- GWG:
-
Gestational weight gain
- HBM:
-
Health belief model
- HFIAS:
-
Household Food Insecurity Access Scale
- ICC:
-
Intracluster correlation
- IEC:
-
Information Education Communication
- LMIC:
-
Low- and middle-income
- MUAC:
-
Mid-upper arm circumference
- NBCC:
-
Nutritional Behavior Change Communication
- PCA:
-
Principal component analysis
- PHCU:
-
Primary healthcare unit
- SRS:
-
Simple random sample
- WDA:
-
Women development army
- WHO:
-
World Health Organization
References
Rah, J. H. et al. Pregnancy and lactation hinder growth and nutritional status of adolescent girls in rural Bangladesh. J. Nutr. 138(8), 1505–1511. https://doi.org/10.1093/jn/138.8.1505 (2008).
Wallace, J. M. Nutrient partitioning during pregnancy: Adverse gestational outcome in over nourished adolescent dams. Proc. Nutr. Soc. 59(1), 107–117. https://doi.org/10.1017/S0029665100000136 (2000).
Zahiruddin, S. et al. Obstetrical and perinatal outcomes of teenage pregnant women attending a secondary hospital in Hyderabad. Open J. Obstet. Gynecol. 7(5), 503–510. https://doi.org/10.4236/ojog.2017.75052 (2017).
Kaplanoglu, M. et al. Gynecologic age is an important risk factor for obstetric and perinatal outcomes in adolescent pregnancies. Women Birth 28(4), e119–e123. https://doi.org/10.1016/j.wombi.2015.07.002 (2015).
Saldanha, L. S. et al. Policies and program implementation experience to improve maternal nutrition in Ethiopia. Food Nutr. Bull. 33(2_suppl 1), S27–S50 (2012).
Physiological changes in pregnancy. Obstetrics by ten teachers, 20th edn. 19, 20–37. https://doi.org/10.1201/9781315382401 (2017).
Chen, P. F. Planning Behavior Change Communication (BCC) Interventions: A Practical Handbook (UNFPA Country Technical Services Team for East and Southeast Asia, 2011).
Mahumud, R. A., Uprety, S., Wali, N., Renzaho, A. M. & Chitekwe, S. The effectiveness of interventions on nutrition social behavior change communication in improving child nutritional status within the first 1000 days: Evidence from a systematic review and meta-analysis. Matern. Child Nutr. 18(1), 13286 (2022).
Ngigi, S. & Busolo, D. N. Behavior change communication in health promotion: Appropriate practices and promising approaches. Int. J. Innov. Res. Dev. 7(9), 84–93 (2018).
World Health Organization (WHO). Adolescent pregnancy (2023). Accessed Aug 2023.
Fund, U.N.C.S. Ending Child Marriage: A Profile of Progress in Ethiopia. https://www.unicef.org/ethiopia/reports/ending-child-marriage (UNICEF, 2018).
Erulkar, A. S. & Eunice, N. Muthengi Building Evidence Base to Delay Marriage in Sub-Saharan Africa, Population Council. https://doi.org/10.31899/pgy3.1020 (2015).
Erulkar, A., Medhin, G. & Weissman, E. The impact and cost of child marriage prevention in three African settings (2017).
WHO, Maternal mortality, fact sheet. https://www.who.int/news-room/fact-sheets/detail/maternal-mortality (2019).
Tessema, Z. T. & Tesema, G. A. Incidence of neonatal mortality and its predictors among live births in Ethiopia: Gompertz gamma shared frailty model. Ital. J. Pediatr. 46(1), 1–10. https://doi.org/10.1186/s13052-020-00893-6 (2020).
Han, Z. et al. Low gestational weight gain and the risk of preterm birth and low birthweight: A systematic review and meta-analyses. Acta Obstet. Gynecol. Scand. 90(9), 935–954. https://doi.org/10.1111/j.1600-0412.2011.01185.x (2011).
Oluleke, M. O., Ogunwale, A. O., Arulogun, O. S. & Adelekan, A. L. Dietary intake knowledge and reasons for food restriction during pregnancy among pregnant women attending primary health care centers in Ile-Ife, Nigeria. Int. J. Popul. Stud. 2(1), 103–106 (2016).
Gebremariam, H. Food taboos during pregnancy and its consequence for the mother, infant and child in Ethiopia: A systemic review. http://www.ijpbsf.com (2017).
Kuche, D., Singh, P. & Moges, D. Dietary practices and associated factors among pregnant women in Wondo Genet District, southern Ethiopia. J. Pharm. Sci. Innov. 4(5), 270–275 (2015).
Daba, G. et al. Assessment of nutritional practices of pregnant mothers on maternal nutrition and associated factors in Guto Gida Woreda, east Wollega zone, Ethiopia. Sci. Technol. Arts Res. J. 2(3), 105–113. https://doi.org/10.4172/2161-0509.1000130 (2013).
Pena, M. & Bacallao, J. Malnutrition and poverty. Annu. Rev. Nutr. 22(1), 241–253. https://doi.org/10.1146/annurev.nutr.22.120701.141104 (2002).
Maes, K., Closser, S., Vorel, E. & Tesfaye, Y. Using community health workers: Discipline and hierarchy in Ethiopia’s women’s development army. Ann. Anthropol. Pract. 39(1), 42–57 (2015).
Sudhakar, M., Woldie, M., Yitbarek, K. et al. Primary Care Systems Profiles and Performance (PRIMASYS): Ethiopian Case study. Alliance Heal Policy Syst Res (2017).
Yitbarek, K., Abraham, G. & Morankar, S. Contribution of women’s development army to maternal and child health in Ethiopia: A systematic review of evidence. BMJ Open 9, e025937. https://doi.org/10.1136/bmjopen-2018-025937 (2019).
Mamo, K., Siyoum, M. & Birhanu, A. Teenage pregnancy and associated factors in Ethiopia: A systematic review and meta-analysis. Int. J. Adolesc. Youth 26(1), 501–512. https://doi.org/10.1080/02673843.2021.2010577 (2021).
Ahmed, R. A. Analysis of Youth Policy Formulation and Implementation with a Special Emphasis on Youth Participation: A Multiple Case Analysis. http://etd.aau.edu.et/bitstream/handle/123456789/19652/Rona%20Ali.pdf?sequence=1&isAllowed=y (2019).
Federal Democratic Republic of Ethiopia Ministry of Health. National Adolescent and Youth Reproductive Health Strategy (2007–2015), Federal Ministry of Health. https://www.prb.org/National-Adolescent-and-Youth-Health-Strategy-2016-2020.Ethiopia.pdf (2007).
Federal Democratic Republic of Ethiopia Ministry of Health. National Adolescent and Youth Health Strategy (2016–2020). https://www.prb.org/wp-content/uploads/2018/05/National-Adolescent-and-Youth-Health-Strategy-2016-2020.Ethiopia.pdf (2016).
Federal Democratic Republic of Ethiopia, National Nutrition Program 2016–2020 (NNP II). https://www.advancingnutrition.org/resources/adolescent-resource-bank/national-nutrition-program-nnp-ii-2016-2020-ethiopia (2016).
Admassu, T. W., Wolde, Y. T. & Kaba, M. Ethiopia has a long way to go meeting adolescent and youth sexual reproductive health needs. Reprod. Health 19(Suppl 1), 130. https://doi.org/10.1186/s12978-022-01445-3 (2022).
Neal, S., Channon, A. A. & Chintsanya, J. The impact of young maternal age at birth on neonatal mortality: Evidence from 45 low- and middle-income countries. PLoS One 13, e0195731. https://doi.org/10.1371/journal.pone.0195731 (2018).
Torvie, A. J., Callegari, L. S., Schiff, M. A. & Debiec, K. E. Labor and delivery outcomes among young adolescents. Am. J. Obstet. Gynecol. 213, 95.e1-95.e8. https://doi.org/10.1016/j.ajog.2015.04.024 (2015).
Weng, Y. H., Yang, C. Y. & Chiu, Y. W. Risk assessment of adverse birth outcomes in relation to maternal age. PLoS One 9, e114843. https://doi.org/10.1371/journal.pone.0114843 (2014).
Kassa, G. M. et al. Adverse neonatal outcomes of adolescent pregnancy in Northwest Ethiopia. PLoS One 14(6), e0218259. https://doi.org/10.1371/journal.pone.0218259 (2019).
Alemayehu, T., Haider, J. & Habte, D. Utilization of antenatal care services among teenagers in Ethiopia: A cross sectional study. Ethiop. J. Health Dev. 24, 3. https://doi.org/10.4314/ejhd.v24i3.68389 (2010).
West Arsi zone area description. https://dbpedia.org/page/West_Arsi_Zone. Accessed on 27 June 2023.
Wachamo, D., Tegene, Y., Tibeso, A. & Washo, A. Sexual and reproductive health services utilization and associated factors among college students at West Arsi Zone in Oromia Region, Ethiopia. ScientificWorldJournal 2020, 3408789. https://doi.org/10.1155/2020/3408789 (2020).
Chowdhury, M., Raynes-Greenow, C., Alam, A. & Dibley, M. J. Making a balanced plate for pregnant women to improve birthweight of infants: A study protocol for a cluster randomized controlled trial in rural Bangladesh. BMJ Open 7(8), e015393 (2017).
McCann, R. S. et al. Reducing contamination risk in cluster-randomized infectious disease-intervention trials. Int. J. Epidemiol. 47(6), 2015–2024 (2018).
Puffer, S., Torgerson, D. J. & Watson, J. Cluster randomized controlled trials. J. Eval. Clin. Pract. 11(5), 479–483. https://doi.org/10.1111/j.1365-2753.2005.00568.x (2005).
Tunçalp, Ö. et al. WHO recommendations on antenatal care for a positive pregnancy experience-going beyond survival. BJOG 124, 860–862. https://doi.org/10.1111/1471-0528.14599 (2017).
Federal Ministry of Health Ethiopia. Blended and Integrated Nutrition Learning Module (BINLM) (Federal Ministry of Health Ethiopia, 2016).
Demilew, Y. M., Alene, G. D. & Belachew, T. Effect of guided counseling on nutritional status of pregnant women in West Gojjam zone, Ethiopia: A cluster-randomized controlled trial. Nutr. J. 19, 1–12. https://doi.org/10.1186/s12937-019-0518-3 (2020).
Wakwoya, E. B., Belachew, T. & Girma, T. Effects of intensive nutrition education and counseling on nutritional status of pregnant women in East Shoa Zone, Ethiopia. Front. Nutr. 10, 1144709. https://doi.org/10.3389/fnut.2023.1144709 (2023).
Cunningham, K. et al. From didactic to personalized health and nutrition counseling: A mixed-methods review of the GALIDRAA approach in Nepal. Matern. Child Nutr. 15, e12681. https://doi.org/10.1111/mcn.12681 (2019).
Bellg, A. J. B. B. et al. Enhancing treatment fidelity in health behavior change studies: Best practices and recommendations from the NIH Behavior Change Consortium. Health Psychol. 23, 443–451. https://doi.org/10.1037/0278-6133.23.5.443 (2004).
Borrelli, B. The Assessment, monitoring, and enhancement of treatment fidelity in public health clinical trials. J. Public Health Dent. 71, S52–S63. https://doi.org/10.1111/j.1752-7325.2011.00233.x (2011).
Fakier, A., Petro, G. & Fawcus, S. Mid-upper arm circumference: A surrogate for body mass index in pregnant women. S. Afr. Med. J. 107, 606–610. https://doi.org/10.7196/SAMJ.2017.vi7197.12255 (2017).
Ricalde, A., Velásquez-Meléndez, G., Tanaka, A. & de Siqueira, A. Mid-upper arm circumference in pregnant women and its relation to birth weight. Rev. Saude Publica 32, 112–117 (1998).
FAO FHI360. Minimum Dietary Diversity for Women: A Guide for Measurement (FAO, 2016).
FAO U. Food and Nutrition Technical Assistance III Project (FANTA) (2016).
Coates, J., Swindale, A. & Bilinsky, P. Household Food Insecurity Access Scale (HFIAS) for Measurement of Food Access: Indicator Guide: Version 3 (2007).
Gebreyesus, S. H., Lunde, T., Mariam, D. H., Woldehanna, T. & Lindtjørn, B. Is the adapted Household Food Insecurity Access Scale (HFIAS) developed internationally to measure food insecurity valid in urban and rural households of Ethiopia? BMC Nutr. 1, 2. http://www.biomedcentral.com/bmcnutr/content/1//2 (2015).
Demilew, Y. M., Alene, G. D. & Belachew, T. Dietary practices and associated factors among pregnant women in West Gojjam Zone, Northwest Ethiopia. BMC Pregnancy Childbirth 20(1), 1–11 (2020).
Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia demographic and health survey 2016 (CSA and ICF, 2016).
Kaleem, R., Adnan, M., Nasir, M. & Rahat, T. Effects of antenatal nutrition counseling on dietary practices and nutritional status of pregnant women: A quasiexperimental hospital based study. Pak. J. Med. Sci. 36(4), 632 (2020).
Khoramabadi, M. et al. Effects of education based on health belief model on dietary behaviors of Iranian pregnant women. Glob. J. Health Sci. 8, 230–239 (2016).
Soylu, M. Effects of nutrition education on general health and nutrition status of pregnant women. Eu. J. Sustain. Dev. Res. 3(1), 18–23 (2019).
Garg, A. & Kashyap, S. Effect of counseling on nutritional status during pregnancy. Indian J. Pediatr. 73, 687–692. https://doi.org/10.1007/BF02898446 (2006).
Diana, R. & Rachmah, Q. Nutrition intervention of pregnant adolescents: A systematic review. Nutr. Food Sci. 51(2), 234–243 (2021).
Sulat, J. S., Prabandari, Y. S., Sanusi, R., Hapsari, E. D. & Santoso, B. The validity of health belief model variables in predicting behavioral change: A scoping review. Health Educ. 118(6), 499–512 (2018).
Rosenstock, I. M., Strecher, V. J. & Becker, M. H. The health belief model and HIV risk behavior change. In Preventing AIDS: Theories and Methods of Behavioral Interventions 5–24 (Springer US, 1994).
Orji, R., Vassileva, J. & Mandryk, R. Toward an effective health interventions design: An extension of the health belief model. Online J. Public Health Inform. https://doi.org/10.5210/ojphi.v4i3.4321 (2012).
Champion, V. L. & Skinner, C. S. The health belief model. Health Behav. Health Educ. Theory Res. Pract. 4, 45–65 (2008).
Abraham, C. & Sheeran, P. The health belief model. Predict. Health Behav. Res. Pract. Soc. Cogn. Models 16(2), 30–55 (2015).
MOH. Adolescent Nutrition Implementation Guideline for Ethiopia (2023).
Acknowledgements
The authors express their special thanks to all the study participants who participated in the study and all the staff of Dilla University, Jimma University colleague researchers, data collectors and supervisors who sacrificed their valuable time for the success of this study.
Funding
Dilla University and Jimma University collaboratively supported this study.
Author information
Authors and Affiliations
Contributions
A.T., D.T. and T.B. were involved in the study design, article selection, analysis and manuscript writing. All the authors were involved in the analysis and manuscript preparation and editing. All the authors read and approved the final draft of the manuscript. All the authors gave their final approval for the version that would be published, agreed on the journal to which the article would be submitted, and agreed to be responsible for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tesfaye, A., Tamiru, D. & Belachew, T. Effect of nutrition counseling on nutritional status and gestational weight gain of pregnant adolescents in West Arsi, Central Ethiopia: a cluster randomized controlled trial. Sci Rep 14, 5070 (2024). https://doi.org/10.1038/s41598-024-55709-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-55709-y
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.