Abstract
To compare the LDCT screening results between eligible and ineligible screening candidates in preventive health check-ups population. Using a real-world LDCT screening results among people who took yearly health check-up in health management center of West China Hospital between 2006 and 2017. Objects were classified according to the China National Lung Cancer Screening Guideline with Low-dose Computed Tomography (2018 version) eligibility criteria. Descriptive analysis were performed between eligible and ineligible screening candidates. The proportion of ineligible screening candidates was 64.13% (10,259), and among them there were 4005 (39.04%) subjects with positive screenings, 80 cases had a surgical lung biopsy. Pathology results from lung biopsy revealed 154 cancers (true-positive) and 26 benign results (false-positive), the surgical false-positive biopsy rate was 4.17%, and ineligible group (7.69%) was higher than eligible group (2.47%), P < 0.05. Further, in ineligible screening candidates, the proportion of current smokers was higher among males compared to females (53.85% vs. 4.88%, P < 0.05). Of the 69 lung cancer patients detected in ineligible screening candidates, lung adenocarcinoma accounts for a high proportion of lung cancers both in male (75.00%) and female (85.00%). The proportion of ineligible screening candidates and the surgical false-positive biopsy rate in ineligible candidates were both high in health check-ups population.
Similar content being viewed by others
Introduction
The incidence and mortality of lung cancer rank first among cancers in China1. According to statistics from the International Organization for Cancer Research, the number of lung cancer cases in China had exceeded 774,000, and the number of lung cancer deaths had exceeded 690,000 in 20182. In comparison to the previous reports in 2015, the incidence and mortality of lung cancer have increased by 5.6% and 13.1% respectively1,2. Mortality of lung cancer can be decreased by early screening and early diagnosis effectively. Since 2011, the National Lung Screening Trial (NLST) in the United States confirmed that low-dose computed tomography (LDCT) screening for smokers at high risk of lung cancer can effectively reduce lung cancer mortality3, professional organizations have issued guidelines recommending high-risk lung cancer candidates4,5,6,7. Recently, a growing number of researches have indicated that the risks and benefits of lung cancer screening will need to be weighed if incorporating into real world practices8,9. Screening high-risk lung cancer individuals is most effective. However, previous studies have shown that an estimated 40–60% of lung cancer patients do not meet the United States Preventive Task Force (USPTF) criteria derived from the NLST eligibility criteria10,11. In the 2019 Behavioral Risk Factor Surveillance System Survey, only 20.9% met all screening eligibility criteria12. What is obviously different from the NLST screening technology plan, the definition of high-risk groups for lung cancer in China is more flexible. This includes13,14,15 selecting the starting age based on lung cancer incidence data in each region; smoking ≥ 20 packs per year; other important risk factors in each region can also be used as conditions for screening high-risk groups. This is related to the actual situation of large differences in16. Our previous study had found that missed diagnosis rate of lung cancer was high in ineligible candidates for preventive health check-ups according to current guidelines17. The conclusion still remains controversial, it still warrants further analysis. More and more health check-up institutions have listed LDCT as a routine screening item, which has resulted in most of the subjects who do not meet the LDCT screening criteria. In the real world, whether the application of LDCT screening in non-high-risk populations has more advantages or disadvantages is still unknown. Also, the characteristics of those individuals who were screened despite not meeting eligibility criteria were not known. Consequently, to evaluate the difference of LDCT screening results between eligible screening candidates and ineligible screening candidates in preventive health check-ups population is necessary.
Results
Baseline characteristics
A total of 15,996 people participated in the LDCT baseline screening, with an average age of 50.3 ± 14.8 years, including 9801 males (61.3%) and 6195 females (38.7%). More detail of baseline characteristics summarized in S1 Table as reported before. Further, baseline characteristics for the eligible and ineligible groups were shown in the Table 1. The proportion of individuals meeting eligible screening candidates was 35.87% (5737), with an average age of 58.75 ± 7.0 years. Among the eligible screening candidates, the proportion of males was higher than females (65.12% vs. 34.88%). Additional results are shown in Table 1.
Lung cancer screening results
The total number of positive screen was 6779 as reported before17. A total of 180 patients (2.66%) had lung biopsy reports. Pathology results from lung biopsy revealed 154 cancers (true-positive) and 26 benign results (false-positive), the total surgical false-positive biopsy rate was 4.17%, and ineligible group (7.69%) exhibited a significantly higher surgical false positive rate than eligible group (2.47%), P < 0.05. The detection rate of positive screening, biopsy rate, the false-positive biopsy rate and the detection rate of lung cancer in eligible screening candidates were all higher than ineligible screening candidates (Table 2).
Gender, age and smoking status characteristics of lung cancer detected
Among the 154 lung cancer patients, 82 (53.24%) were male and 72 (46.75%) were female. There was no statistical significant difference in gender between eligible and ineligible groups (Fig. 1A). The proportion of lung cancer cases in current smokers (29.87%) was lower than never smoked group (70.13%), and there was no statistically significant difference in smoking status between the two groups (Fig. 1B). Further, in ineligible group, the proportion of current smokers was higher among males compared to females (53.85% vs. 4.88%, P < 0.05) (Fig. 1C). The population was divided into 12 age groups with a 5-year span in age. In ineligible group, the age distribution of lung cancer cases showed two double peaks, 40–44 years old group (23.19%) and ≥ 80 years old group (26.09%) respectively (Fig. 1D). Further analysis by gender, the age distribution of lung cancer cases’ two double peaks was different in males and females (Males: 45–49 years old group (23.08%), ≥ 80 years old group (30.77%) vs. Females: 40–44 years old group (31.71%), ≥ 75 years old group (17.07%)) (Fig. 1E).
The pathological classification and stage of lung cancer detected
Of the 154 lung cancer patients detected in this study, there were 120 cases of adenocarcinoma, 12 cases of adenocarcinoma in situ, 2 cases of adenosquamous carcinoma, 9 cases of minimally invasive adenocarcinoma, 5 cases of neuroendocrine tumor, and 6 cases of squamous carcinoma. Lung adenocarcinoma accounts for a high proportion of lung cancers both in ineligible group (79.71%) and eligible group (76.47%). More results were showed in Fig. 2A. Pathologic stages were stage I in 106 cases, stage II in 6 cases, stage III in 6 cases, stage IV in 18 cases, and 18 cases stage information were not available. Lung adenocarcinoma accounts for a high proportion of lung cancers both in ineligible group (79.71%) and eligible group (76.47%). More results were showed in Fig. 2B.
Gender, and smoking status characteristics of pathological classification and stage of lung cancer in ineligible screening candidates
We further conducted a subgroup analysis of lung cancer case characteristics by gender and smoking status among ineligible group. 69 patients with lung cancer were identified in ineligible group, lung adenocarcinoma accounts for a high proportion of lung cancers both in male (75.00%) and female (85.00%). Squamous cell carcinoma was detected only in male (6.00%), but not in female. More results were showed in Fig. 3A. Whether male or female, pathological staging is dominated by stage I (Fig. 3B). Lung adenocarcinoma proportions are higher in non-smoking group (85.00%) than in smoking group (68.00%) (Fig. 3C). The pathological staging of lung cancer in smoking group and non-smoking group was mainly stage I, and the proportion of stage IV in male (18.00%) was higher than in female (2.00%). More results were showed in Fig. 3D.
Discussion
In the present study, we investigated the LDCT screening results in ineligible candidates. The proportion of ineligible screening candidates was as high as 64.13%. This rate is similar to that reported by others11,18. A retrospective study of Asian lung cancer patients treated at New York reported that the percentage of Asian patients meeting the NLST criteria is similar to the United States population19. Although the overall rate of ineligibility for screening was similar to the rates reported previously, its internal composition was indeed quite different from previously reported. We found that the proportion of current smokers in males was almost ten times compared to females in ineligible screening candidates. At present, many studies have shown that we should pay enough attention to female and non-smokers20. Matthew Koshy analyzed differences in gender sensitivity of USPSTF screening guidelines that are based solely on age and smoking history, they found that the sensitivities for screening by the USPSTF 2013 were 46.7% for women and 64.6% for men and by the USPSTF 2021 were 56.8% and 71.8%, respectively21. The results of a large cross-sectional study showed that the odds of eligibility were lower for women compared with men (adjusted odds ratio, 0.88; 95% CI, 0.79–0.99) by the current revised USPSTF 202122. Nearly two-thirds of lung cancer patients were non-smokers and an additional one-thirds were smokers, comprised mostly of female patients. The most important change in the newly revised LDCT screening eligibility guidelines in China was that lung cancer risk factors besides smoking were considered for the identification of high-risk population, mitigating the exclusion of female non-smokers from potential screening benefits13,14. A study about epidemiology of lung cancer and lung cancer screening programs in China and the United States revealed that the incidence of lung cancer in non-smokers that was significantly higher in China than in the United States, and was particularly notable in female23. Tony Kirby reported a young non-smoker diagnosed with lung cancer that who believed the system should be improved in many ways, from raising awareness in doctors and the public, removing stigma, and expanding screening for those who are excluded by the current screening guidelines24.
Our results are important for another reason. As the results shown in Table 2, the cumulative detection rate of lung cancer in ineligible screening candidates (0.27%) was lower than in eligible screening candidates (3.06%). It would appear that the yield of CT screening in ineligible subjects has a yield of diagnosis of lung cancer of less than 10% of that in eligible subjects. Clearly, such results may increase the challenges for recruiting female non-smokers into the screening process. According to current lung cancer screening guidelines, high-risk groups are defined according to factors such as age and smoking4,5,6,7. China’s lung cancer screening guidelines define high-risk groups in terms of passive smoking, smoking, family medical history, occupational exposure, history of chronic lung disease, and so on. However, it seems that factors other than age and smoking, there is lack of universal and unified other factors quality evaluation standards. The data in this study was derived from real-world data. China has not yet clarified the best age range for screening. Taking into account the cost and benefit of screening, the current recommended age range for screening is between 50 and 74 years old. With the promotion of lung cancer screening and the improvement of medical awareness, the onset of lung cancer has showed a younger trend16. However, there are significant differences in the study populations and the cost-effectiveness of supplemental screening for female non-smokers has yet to be evaluated. Prospective, multi-center or community-derived research support is still needed.
In practice, we also want to know whether there was a high false-positive rate for surgical pathology biopsies among ineligible candidates? It was surprising to find no differences in the false-positive biopsy rate between ineligible and eligible groups. Despite this, we were not yet confident in extrapolating this result. Of the 80 biopsy positive cases in ineligible group, there were 11 false negative diagnoses (5 surgical excision, 2 rans-thoracic needle biopsy and 4 image guided bronchoscopy). LDCT lung cancer screening has been shown to significantly reduce lung cancer mortality, but also more false-positive results, unnecessary testing and invasive procedures, overdiagnosis, etc.25,26. The proportion of invasive procedures following a false positive also increased significantly from 0.7 to 2.0% in the National Lung Screening Trial27. Our results found that the total population surgical false-positive biopsy rate was 4.17%, and the ineligible group (7.69%) was higher than the eligible group (2.47%). This would suggested that the surgical false-positive biopsy rate would likely be higher in a real-world setting, especially in ineligible candidates from health check-ups population. In 2019, West China Hospital of Sichuan University launched a full-process management project for pulmonary nodules/lung cancer patients, which could enables a standard follow-up screening procedure and treatment system28. All individuals aged 40 and older who participated in LDCT health check-ups in West China Hospital could received the green channel for diagnosis and treatment. This will provide an opportunity to gain more evidence about the cost-effectiveness of LDCT screening in ineligible candidates, female non-smokers in particular. Note that besides relying on current treatment guidelines, there are also other methods for selecting high-risk candidates. Pan-Canadian Early Detection of Lung Cancer (PanCan) Study selected participants for lung cancer screening by risk modeling29. A risk-based predictive model based on family history of lung cancer and female gender may improve lung cancer screening efficiency, according to a Taiwanese Lung Cancer Screening Project study30. Lung cancer screening using computed tomography can reduce mortality, but it is also critical to optimize the balance of benefits and risks by increasingly selecting high-risk groups. At present, more and more studies have confirmed that screening high-risk groups of lung cancer based on individualized risk is a very effective way to participate in LDCT screening, even better than guideline standards31.
The present study has some additional limitations. Firstly, there were insufficient data available regarding incidence of mortality and long-term lung cancer morbidity during the study periods included in this analysis. Secondly, the prevalence of smoking in the health check-ups female population presented in our database was low (4.88%), further research incorporating more female smokers is needed to serve as a control group. Also, whether our findings apply to more ethnically diverse populations awaits further study.
Conclusion
The proportion of ineligible screening candidates and the surgical false-positive biopsy rate in ineligible candidates were both high in health check-ups population.
Methods
Study design and participants
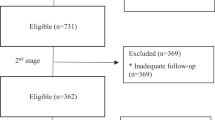
The study was a retrospective analysis, we have used data from a real-world study of low-dose computed tomography screening among people who took yearly health checkup. More details about the study design, entry criteria, screening protocol, and medical-record abstraction of this study have been previously published17. Baseline characteristics were showed in S1 Table. According to the eligible criteria, a total of 15,996 subjects were eventually included (Fig. 4).
Positive screening criteria
The criteria for a positive screen was according to the China National Lung Cancer Screening Guideline with Low-dose Computed Tomography (2018 version)13, a positive screen was defined as any of the following: (1) baseline screening: any of the following: (a) with a diameter of ≥ 5 mm pure or part-solid nodule; (b) any nonsolid nodules ≥ 8 mm; (c) Suspicious bronchial lesion or (and) tracheal lesion; (d) single or multiple nodules or lung cancer masses diagnosed as lung cancer by LDCT. (2) annual screening: any of the following: (a) discovery of new noncalcific nodules or airway lesions; (b) it is found that the original nodule is enlarged or the solid component is increased.
Ethical consideration
Before collecting data, this research had been approved by the Biomedical Ethics Review Committee of West China Hospital of Sichuan University (2015(202), 2019(195)). Informed consent for the study was obtained from each study participant and/or their legal guardian(s) before data collection and documented in a prepared format. Moreover, all methods in the present study were performed in accordance with the declarations of Helsinki and the relevant guidelines/regulations.
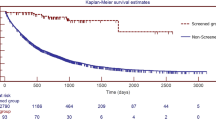
Follow-up time and vital status
The follow-up was a part of the routine procedure as recommended by the treating physician. We have a working mechanism for early warning of major positive diseases and a green channel (Specialized outpatient clinic for lung cancer, convenient for follow-up and standardized diagnosis and treatment). This study were followed-up from January 1, 2007 to June 1, 2022. The shortest follow-up time was 3.5 years, and the longest was 15.5 years. As previously reported17, we have trained professionals to follow-up. A special follow-up team is responsible for ascertaining probable vital status and determining whether the cause of death was lung cancer. We also evaluated harms’ outcomes, specifically false-positive biopsy. Lung cancer pathological typing was according to the International Association for the Study of Lung Cancer (IASLC) Eighth Edition of the TNM Classification for Lung Cancer32.
Grouping criteria
We used China National Lung Cancer Screening Guideline with Low-dose Computed Tomography (2018 version) as ineligible candidates grouping basis13. Eligible screening candidates: (a) aged 50–74 years, (b) who have at least a 20 pack-year smoking history, (c) and who currently smoke or have quit within the past 5 years. Ineligible screening candidates: the above conditions were not met.
Statistical analysis
Statistical analyses were performed using SPSS software (SPSS statistics 21.0; SPSS Inc.). The comparison of the continuous variable was analyzed using a two-sided t-test and the categorical variables was analyzed using a Chi-square testing or Fisher exact test. The Bonferroni post-test was used for further pairwise comparison. Considering the comparisons of age trends, linear trend Chi-square test had been applied. The test level α = 0.05 was considered statistically significant.
Data availability
Data are not publicly available but may be accessed upon reasonable request from the corresponding author (huairongtang1963@163.com).
References
Chen, W. et al. Cancer statistics in China, 2015. CA Cancer J. Clin. 66, 115–132. https://doi.org/10.3322/caac.21338 (2016).
Bray, F. et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 68, 394–424. https://doi.org/10.3322/caac.21492 (2018).
Aberle, D. R. et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N. Engl. J. Med. 365, 395–409. https://doi.org/10.1056/NEJMoa1102873 (2011).
Wood, D. E. et al. Lung cancer screening, version 3.2018, NCCN clinical practice guidelines in oncology. J. Natl. Compr. Cancer Netw. JNCCN 16, 412–441. https://doi.org/10.6004/jnccn.2018.0020 (2018).
Mazzone, P. J. et al. Screening for lung cancer: CHEST guideline and expert panel report. Chest 153, 954–985. https://doi.org/10.1016/j.chest.2018.01.016 (2018).
Mitchell, E. P. U. S. Preventive Services Task Force final recommendation statement, evidence summary, and modeling studies on screening for lung cancer. J. Natl. Med. Assoc. 113, 239–240. https://doi.org/10.1016/j.jnma.2021.05.012 (2021).
Wender, R. et al. American Cancer Society lung cancer screening guidelines. CA Cancer J. Clin. 63, 107–117. https://doi.org/10.3322/caac.21172 (2013).
Meza, R. et al. Evaluation of the benefits and harms of lung cancer screening with low-dose computed tomography: Modeling study for the US Preventive Services Task Force. JAMA 325, 988–997. https://doi.org/10.1001/jama.2021.1077 (2021).
Rivera, M. P. et al. Addressing disparities in lung cancer screening eligibility and healthcare access. An official American Thoracic Society Statement. Am. J. Respir. Crit. Care Med. 202, e95–e112. https://doi.org/10.1164/rccm.202008-3053ST (2020).
Nemesure, B. et al. Evaluating efficacy of current lung cancer screening guidelines. J. Med. Screen. 24, 208–213. https://doi.org/10.1177/0969141316689111 (2017).
Aldrich, M. C. et al. Evaluation of USPSTF lung cancer screening guidelines among African American adult smokers. JAMA Oncol. 5, 1318–1324. https://doi.org/10.1001/jamaoncol.2019.1402 (2019).
Liu, Y. et al. Assessment of uptake appropriateness of computed tomography for lung cancer screening according to patients meeting eligibility criteria of the US Preventive Services Task Force. JAMA Netw. Open 5, e2243163. https://doi.org/10.1001/jamanetworkopen.2022.43163 (2022).
Zhou, Q. et al. China national lung cancer screening guideline with low-dose computed tomography (2018 version). Zhongguo fei ai za zhi = Chin. J. Lung Cancer 21, 67–75. https://doi.org/10.3779/j.issn.1009-3419.2018.02.01 (2018).
Chinese Expert Group on Early Diagnosis and Treatment of Lung Cancer; China Lung Oncology Group. China national lung cancer screening guideline with low-dose computed tomography (2023 version). Zhongguo fei ai za zhi = Chin J. Lung Cancer 26, 1–9. https://doi.org/10.3779/j.issn.1009-3419.2023.102.10 (2023).
Zhou, Q. H. et al. China national lung cancer screening guideline with low-dose computed tomography (2015 version). Thorac. Cancer 6, 812–818. https://doi.org/10.1111/1759-7714.12287 (2015).
Qi, J. et al. National and subnational trends in cancer burden in China, 2005–20: An analysis of national mortality surveillance data. Lancet Public Health 8, e943–e955. https://doi.org/10.1016/s2468-2667(23)00211-6 (2023).
Ji, G. et al. Current lung cancer screening guidelines may miss high-risk population: A real-world study. BMC Cancer 21, 50. https://doi.org/10.1186/s12885-020-07750-z (2021).
Triplette, M. et al. Prediction of lung cancer screening eligibility using simplified criteria. Ann. Am. Thorac. Soc. 16, 1280–1285. https://doi.org/10.1513/AnnalsATS.201903-239OC (2019).
Kumar, V. et al. The performance of NLST screening criteria in Asian lung cancer patients. BMC Cancer 15, 916. https://doi.org/10.1186/s12885-015-1922-5 (2015).
Dubin, S. & Griffin, D. Lung cancer in non-smokers. Mo. Med. 117, 375–379 (2020).
Pasquinelli, M. M. et al. Addressing sex disparities in lung cancer screening eligibility: USPSTF vs PLCOm2012 criteria. Chest 161, 248–256. https://doi.org/10.1016/j.chest.2021.06.066 (2022).
Reese, T. J. et al. Evaluation of revised US Preventive Services Task Force lung cancer screening guideline among women and racial/ethnic minority populations. JAMA Netw. Open 4, e2033769. https://doi.org/10.1001/jamanetworkopen.2020.33769 (2021).
Yang, D. et al. Epidemiology of lung cancer and lung cancer screening programs in China and the United States. Cancer Lett. 468, 82–87. https://doi.org/10.1016/j.canlet.2019.10.009 (2020).
Kirby, T. Young non-smoker diagnosed with lung cancer. Lancet Respir. Med. 8, 141–142. https://doi.org/10.1016/s2213-2600(20)30007-2 (2020).
Jonas, D. E. et al. Screening for lung cancer with low-dose computed tomography: Updated evidence report and systematic review for the US Preventive Services Task Force. JAMA 325, 971–987. https://doi.org/10.1001/jama.2021.0377 (2021).
Patz, E. F. Jr. et al. Overdiagnosis in low-dose computed tomography screening for lung cancer. JAMA Intern. Med. 174, 269–274. https://doi.org/10.1001/jamainternmed.2013.12738 (2014).
Pinsky, P. F., Bellinger, C. R. & Miller, D. P. Jr. False-positive screens and lung cancer risk in the National Lung Screening Trial: Implications for shared decision-making. J. Med. Screen. 25, 110–112. https://doi.org/10.1177/0969141317727771 (2018).
Liu, D. et al. Pulmonary nodules/lung cancer comprehensive management mode: Design and application. Zhongguo fei ai za zhi = Chin. J. Lung Cancer 23, 299–305. https://doi.org/10.3779/j.issn.1009-3419.2020.103.06 (2020).
Tammemagi, M. C. et al. Participant selection for lung cancer screening by risk modelling (the Pan-Canadian Early Detection of Lung Cancer [PanCan] study): A single-arm, prospective study. Lancet Oncol. 18, 1523–1531. https://doi.org/10.1016/s1470-2045(17)30597-1 (2017).
Wu, F. Z. et al. Assessment of selection criteria for low-dose lung screening CT among Asian ethnic groups in Taiwan: From mass screening to specific risk-based screening for non-smoker lung cancer. Clin. Lung Cancer 17, e45–e56. https://doi.org/10.1016/j.cllc.2016.03.004 (2016).
Tammemägi, M. C. et al. USPSTF2013 versus PLCOm2012 lung cancer screening eligibility criteria (International Lung Screening Trial): Interim analysis of a prospective cohort study. Lancet Oncol. 23, 138–148. https://doi.org/10.1016/s1470-2045(21)00590-8 (2022).
Goldstraw, P. et al. The IASLC Lung Cancer Staging Project: Proposals for revision of the TNM stage groupings in the forthcoming (Eighth) Edition of the TNM Classification for Lung Cancer. J. Thorac. Oncol. 11, 39–51. https://doi.org/10.1016/j.jtho.2015.09.009 (2016).
Acknowledgements
The team would like to thank the staff of West China Hospital Information Center and West China Hospital Pulmonary Nodule/Lung Cancer Management Center for their technical support during the extensive screening follow-up. This article was also supported by the National Clinical Key Specialty Construction Project.
Funding
This work was supported by Sichuan Province Science and Technology Support Program (2022YFS0130), National Key R&D Program of China (2017YFC0907501, 2017YFC0907504) and Sichuan University West China Hospital Disciplinary Excellence 1.3.5 Project Lung Cancer Early Research and application of early diagnosis and treatment system-West China Lung Cancer Project (No. ZYJC18001).
Author information
Authors and Affiliations
Contributions
H.T., Y.H., W.H., W.L. and T.B. designed the study, T.B., B.L. and H.Y. analyzed the results, T.B., B.L. and R.L. drafted the manuscript. Z.L. and G.J. participated in data collection and literature review. H.T., Y.H. and T.B. designed and executed the data analysis plan. W.H. and Y.W. contributed to and reviewed and edited the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bao, T., Liu, B., Li, R. et al. LDCT screening results among eligible and ineligible screening candidates in preventive health check-ups population: a real world study in West China. Sci Rep 14, 4848 (2024). https://doi.org/10.1038/s41598-024-55475-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-55475-x
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.