Abstract
This study aimed to investigate the relationship of four chronic kidney disease–mineral and bone disorder (CKD–MBD) biomarkers, including intact parathyroid hormone (PTH), fibroblast growth factor 23 (FGF23), soluble klotho, and fetuin-A, with aortic stiffness in peritoneal dialysis (PD) patients, comparing those with and without diabetes mellitus (DM). A total of 213 patients (mean age 58 ± 14 years; 81 (38.0%) patients with DM) were enrolled. Their aortic pulse wave velocity (PWV) was measured using pressure applanation tonometry, while serum intact PTH, FGF23, α-klotho, and fetuin-A levels were measured using enzyme-linked immunosorbent assay. Overall, patients with DM had higher aortic PWV than those without (9.9 ± 1.8 vs. 8.6 ± 1.4 m/s, p < 0.001). Among the four CKD–MBD biomarkers, FGF23 levels were significantly lower in DM group (462 [127–1790] vs. 1237 [251–3120] pg/mL, p = 0.028) and log-FGF23 independently predicted aortic PWV in DM group (β: 0.61, 95% confidence interval: 0.06–1.16, p = 0.029 in DM group; β: 0.10, 95% confidence interval: − 0.24–0.45, p = 0.546 in nonDM group; interaction p = 0.016). In conclusion, the association between FGF23 and aortic PWV was significantly modified by DM status in PD patients.
Similar content being viewed by others
Introduction
The high prevalence of end-stage renal disease (ESRD) and its related cardiovascular burden are major public health concerns worldwide. Cardiovascular disease (CVD) is the leading cause of death in ESRD, accounting for half of all mortality in patients undergoing dialysis1,2,3. Aside from the well-established traditional risk factors, chronic kidney disease–mineral and bone disorder (CKD–MBD), a dysregulation of mineral and bone metabolism exacerbated by worsening kidney disease, plays a crucial role in the pathogenesis of CVD4,5,6.
Compensatory changes in several serum CKD–MBD biomarkers are observed as CKD progresses7. Fibroblast growth factor 23 (FGF23), secreted primarily by osteocytes and osteoblasts, is the earliest elevated biomarkers regulating mineral bone metabolism. Its serum levels increase 1000-fold when patients develop ESRD8,9. Through binding to klotho, FGF23 inhibits renal phosphorus reabsorption by downregulating sodium/phosphate cotransporters in the proximal renal tubules. It also regulates the secretion of parathyroid hormone (PTH), which levels are elevated in advanced CKD stages10,11,12,13. In contrast, circulating soluble α-klotho, the extracellular domain of membranous klotho proteolytically cleaved by metalloproteinase, is reduced in early CKD stages7. Fetuin-A, a 59-kDa glycoprotein derived from the liver, is a potent inhibitor of vascular calcification. Its serum levels have steadily decreased since the early stages of CKD14,15. The aforementioned biomarker changes may be involved in the pathogenesis of distinctive vascular dysfunction in CKD.
As the most remarkable alteration in these serum CKD–MBD markers is observed at the ESRD stage, assessing their association with arterial stiffness in patients undergoing peritoneal dialysis (PD) is essential. Although dysregulated mineral metabolism is more severe in patients with diabetes mellitus (DM) than in those without16,17, it is unknown whether DM status modifies the association between serum CKD–MBD biomarkers and aortic stiffness.
Thus, we aimed to investigate the relationship of serum CKD–MBD biomarkers, including intact PTH, FGF23, soluble α-klotho, and fetuin-A, with aortic stiffness in patients with ESRD undergoing PD, comparing those with and without DM.
Materials and methods
Patients
In this cross-sectional study, the association of serum CKD–MBD biomarkers with aortic stiffness in PD patients with and without DM was investigated. Patients with ESRD who had undergone PD for more than three months were screened at Hualien Tzu Chi Hospital, a tertiary medical center in eastern Taiwan, and its three branch hospitals in Taipei, Taichung, and Dalin. Patients were enrolled and baseline measurements were taken between February 2020 and May 2021. Patients who had an infection, acute myocardial infarction, decompensated heart failure, stroke, or amputation at the time of enrollment, or who refused to participate, were excluded from the study. The study was approved by Tzu Chi University and Hospital’s Institutional Review Board for the Protection of Human Subjects (IRB no. 108-219-A), and all participants provided informed consent before participating in this study. All methods were performed in accordance with the relevant guidelines and regulations.
The basic information, including age, gender, PD vintage, dialysis modalities, comorbidities, and medications used, was obtained from the electronic medical records. The diagnosis of DM was identified using the ICD-10 code from the electronic medical records.
Anthropometric and aortic pulse wave velocity measurements
A well-trained staff measured participants’ height and weight while they were barefoot and wearing light clothing, and their body mass index was calculated accordingly.
The aortic pulse wave velocity (PWV) was measured using a cuff-based volumetric displacement (SphygmoCor XCEL, AtCor Medical, Sydney, NSW, Australia)18. Briefly, the cuff of the XCEL device was placed on the participants’ left upper arm to measure blood pressure (BP) with an automatic recording of standard oscillometric brachial systolic and diastolic BP, immediately followed by reinflation of the cuff to a sub diastolic pressure level. For PWV assessment, the XCEL device uses the volumetric displacement waveform from a cuff around the upper thigh instead of femoral artery tonometry, and a tonometry is used in the XCEL device for carotid pulse acquisition. Pulse pressure was calculated by subtracting the brachial diastolic BP from the brachial systolic BP.
Biochemical investigations
Fasting blood samples were collected in the morning and centrifuged at 3000 × g for 10 min to separate serum samples, which were biochemically analyzed within one hour of collection. Serum levels of blood urea nitrogen, creatinine, glucose, albumin, total calcium, phosphorus, and total alkaline phosphatase were measured using an autoanalyzer (Siemens Advia 1800, Siemens Healthcare GmbH, Henkestr, Germany). Corrected calcium levels, calculated as total calcium (mg/dL) + 0.8 [4—serum albumin (mg/dL)], were adopted for analysis. Furthermore, 24-h urine and dialysate samples were collected to calculate weekly peritoneal and renal creatinine clearance19. Those who had residual urine output were defined as having preserved residual renal function.
Serum CKD–MBD biomarkers were quantified using commercial enzyme-linked immunosorbent assays for intact PTH (IBL International GmbH, Hamburg, Germany), FGF23 (C-terminal, Immutopics, Inc., San Clemente, CA), soluble α-klotho (Immuno-Biological Laboratories Co., Ltd., Fujioka-Shi, Gunma, Japan), and fetuin-A (BioVender Laboratory Medicine Inc., Modrice, Czech Republic).
Statistical analysis
Continuous data were assessed for normality using the Kolmogorov–Smirnov test. Normally distributed data were expressed as means and standard deviations and compared using the Student’s independent t-test, while nonnormally distributed data were expressed as medians and interquartile ranges and compared using the Mann–Whitney U test between DM and nonDM groups. Categorical data were expressed as numbers and percentages and compared using the χ2 test. The correlation of serum CKD–MBD biomarkers levels with clinical parameters and aortic PWV were analyzed using Pearson’s or Spearman’s coefficient analysis, as appropriate. Serum CKD–MBD biomarkers showed a right-skewed distribution and were log-transformed before regression analysis. A multivariate stepwise linear regression analysis was performed to determine the independency between CKD–MBD biomarkers and aortic PWV stratified by DM status. The potential modified effects of DM status on the association between CKD–MBD biomarkers and aortic PWV effects were tested by creating DM × mean-centering biomarkers interaction variables. Data were analyzed using the Statistical Package for the Social Sciences (SPSS) for Windows (Version 19.0; SPSS Inc., Chicago, IL, USA). P-values of less than 0.05 were considered statistically significant.
Results
This study enrolled 213 patients undergoing PD, 38.0% of whom (n = 81) had DM and 62.0% (n = 132) did not. Table 1 summarizes the clinical characteristics of patients undergoing PD. The mean age was 58 ± 14 years, and the median PD vintage was 48 months. Among these patients, 55.4% were female, 91.1% had hypertension, 46.0% had hyperlipidemia, 33.8% received continuous ambulatory PD, and 57.3% underwent automated PD. Calcium carbonate, active vitamin D, and statins were used by 69.0%, 22.1%, and 31.0% of patients, respectively.
Compared to patients without DM, patients with DM were older, had a shorter PD vintage, more preserved residual renal function, and higher body mass index, systolic BP, pulse pressure, and aortic PWV (9.9 ± 1.8 vs. 8.6 ± 1.4 m/s, p < 0.001). Notably, among four CKD–MBD biomarkers, patients with DM had significantly lower FGF23 levels (462 [127–1790] vs. 1237 [251–3120] pg/mL, p = 0.028). However, the serum levels of the other three biomarkers were comparable between groups.
Table 2 presents the simple correlations of log-transformed CKD–MBD biomarkers levels with clinical and laboratory parameters in patients with and without DM. In patients with DM, PD vintage was positively correlated with intact PTH (r = 0.31) and FGF23 (r = 0.33), while renal creatinine clearance was negatively correlated with FGF23 (r = − 0.28). In both patients with and without DM, serum FGF23 was positively correlated with calcium (r = 0.36 and 0.31), phosphorus (r = 0.27 and 0.45), and calcium × phosphorus (r = 0.37 and 0.52), while fetuin-A was positively correlated with albumin (r = 0.27 and 0.25). For biomarker intercorrelation, FGF23 was positively correlated with intact PTH (r = 0.23) and α-klotho (r = 0.25), while α-klotho was positively correlated with fetuin-A (r = 0.38) in patients with DM. However, similar intercorrelations among CKD biomarkers were not observed in patients without DM.
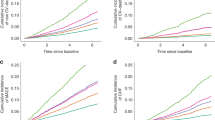
Figure 1 depicts scatter plots and Pearson’s correlation analysis of the association between serum CKD–MBD biomarkers and aortic PWV in patients with and without DM. FGF23 had a positive correlation with aortic PWV in patients with DM (r = 0.28, p = 0.012) but not in those without (r = − 0.01, p = 0.984). The other three biomarkers were not associated with aortic PWV in patients with or without DM.
Table 3 shows the association of CKD–MBD biomarkers with aortic PWV in PD patients with and without DM using univariable and multivariable linear regression analysis. After adjusting for age, gender, PD vintage, residual renal function, hypertension, hyperlipidemia, alkaline phosphatase, calcium-phosphorus product, and calcium carbonate and active vitamin D use, log-FGF23 (β: 0.61, 95% confidence interval: 0.06–1.16, p = 0.029) was an independent predictor of aortic PWV in patients with DM but not in those without (β: 0.10, 95% confidence interval: − 0.24–0.45, p = 0.546). The DM status significantly modified the association between FGF23 and aortic PWV (interaction p = 0.016).
Discussion
This study investigated the association of four serum CKD–MBD biomarkers with aortic stiffness between PD patients with and without DM. The study’s novel finding is that serum FGF23 independently predicted aortic PWV only in PD patients with DM, albeit with lower serum FGF23 levels.
The close relationship between FGF23 and aortic stiffness in CKD and ESRD is explained by several mechanisms. FGF23 accelerates phosphate-induced calcification of vascular smooth muscle cells by stimulating osteoblastic differentiation20, activates the renin–angiotensin–aldosterone system21, and directly impairs endothelial vasorelaxation22. Notably, a recent study conducted by Vergara et al. showed that FGF23 treatment transformed vascular smooth muscle cells from a contractile to a synthetic phenotype in vitro, through the downregulation of microRNA-221/222 and phosphorylation of FGFR1 and Erk1/223. Furthermore, FGF23 expression and serum levels are elevated in inflammatory states24,25. Several clinical observational studies have demonstrated associations between serum FGF23 levels and vascular stiffness at various stages of CKD. The large-scale Prospective Investigation of the Vasculature in Uppsala Seniors (PIVUS) study found that serum FGF23 was associated with arterial stiffness in community subjects with impaired renal function (estimated glomerular filtration rate less than 60 mL/min/1.73 m2)26. The association between serum FGF23 and total body atherosclerosis was also confirmed in a PIVUS subsample27. In patients on hemodialysis, serum FGF23 was associated with aortic calcification28 and accelerated the progression of coronary arterial calcification29,30. In patients undergoing PD, elevated serum FGF23 levels have been linked to vascular calcification31 and carotid artery intima-media thickness32. However, studies comparing the potentially different impacts of FGF23 on aortic stiffness in patients with and without DM are scarce.
In our study, serum FGF23 levels were positively associated with aortic stiffness in PD patients with DM but not in those without. Consistent with our finding, a significant positive association between serum FGF23 levels and aortic stiffness was found in non-CKD patients with type 1 DM but not in those with no DM33. In patients with coronary artery disease, serum FGF-23 levels predicted adverse cardiovascular outcomes only in those with type 2 DM but not in those without34. This suggested that DM status may modify FGF23’s effects on vascular pathology and clinical cardiovascular events. Although the underlying mechanisms remain unclear, some DM-specific vascular pathological factors, such as advanced glycosylated end products, insulin resistance, and reactive oxygen species, may interplay in the complex pathogenesis of CKD–MBD and act synergistically with FGF23 on changing vascular wall structure.
In the Predictors of Arrhythmic and Cardiovascular Risk in End Stage Renal Disease (PACE) cohort, primarily comprising incident hemodialysis patients of African American descent, elevated serum FGF-23 levels were associated with a higher prevalence of coronary artery calcification. However, contrary to our findings, higher FGF-23 levels were linked to lower baseline PWV and reduced PWV progression during follow-up, particularly among patients with DM35. The exact cause of these discrepancies remains unclear, but they might be attributed to differences in ethnic populations, patient selection, and study design.
Several DM-related factors, such as advanced glycated end product and glycerol-3-phosphate accumulation and enhanced chronic inflammation, are known to stimulate FGF23 secretion16. In patients with CKD who did not undergo dialysis, those with DM have higher FGF23 levels17 and more rapidly rising serum levels36 than those without DM. Surprisingly, our PD patients with DM had significantly lower serum FGF23 levels. A similar finding had been reported in the Japan Dialysis Outcomes and Practice Patterns study (J-DOPPS) and the Hemodialysis (HEMO) cohort, two large prevalent hemodialysis cohorts in Japan and the United States, respectively37,38. This finding could be attributed in part to patient selection. In these ESRD populations, patients with DM tended to have a shorter dialysis vintage and more preserved residual renal function, two major determinants of serum FGF23 levels39,40. Furthermore, a recent study demonstrated that insulin suppressed FGF23 production by inhibiting the transcription factor forkhead box protein O141. Nevertheless, the positive correlation between relatively lower serum FGF23 levels and aortic PWV values in DM suggests that FGF23 is a more sensitive biomarker for aortic stiffness in PD patients with DM.
In our study, serum fetuin-A, a potent circulatory inhibitor of vascular calcification, was not associated with aortic stiffness in either the DM or nonDM groups. A similar finding was reported in two other dialysis cohorts42,43. As we all know, vascular calcification is a hallmark of CKD, but it is not the only factor contributing to aortic stiffness. Nevertheless, serum fetuin-A levels were found to be positively correlated with serum albumin levels in both PD patients with and without DM. High circulating fetuin-A levels reduced the inflammatory process, resulting in higher albumin levels44,45. Wang and colleagues found that lower serum fetuin-A levels in patients undergoing PD were associated with malnutrition, as assessed by serum albumin assay and subjective global assessment46.
Klotho is an antiaging protein, and its declining levels may be related to accelerated vascular aging. In the National Health and Nutrition Examination Survey (NHANES), a large cohort of the general population in the United States, serum klotho was found to be negatively associated with pulse pressure47. In contrast, in a general Chinese population, serum klotho levels did not predict BP or aortic PWV48. Similarly, in the KoreaN Cohort Study for Outcome in Patients With Chronic Kidney Disease (KNOW-CKD) cohort, serum klotho levels were not associated with brachial-to-ankle PWV in patients with advanced non-dialysis CKD49. In our patients undergoing PD, serum klotho was not associated with aortic PWV or pulse pressure. The discrepancy among these studies may be explained by differences in study populations and ethics.
The present study has several limitations that should be acknowledged. First, there was no image evaluation for aortic or coronary calcification, as well as other indices of vascular dysfunction, in this study. Second, neither vitamin D status nor inflammatory markers were assessed in this study. Third, the causal relationship between serum FGF23 and aortic stiffness cannot be established in this cross-sectional study, and longitudinal analyses are warranted to determine whether higher serum FGF23 levels contribute to accelerated aortic stiffness in patients with DM.
In conclusion, among CKD–MBD biomarkers, serum FGF23 was an independent predictor of aortic stiffness in PD patients with DM but not in those without DM. Further studies are needed to clarify the potential mechanisms underlying the effect of FGF23 and DM status interaction on aortic stiffness in patients undergoing PD.
Data availability
The datasets analysed during the current study are available from the corresponding author on reasonable request.
References
Gansevoort, R. T. et al. Chronic kidney disease and cardiovascular risk: Epidemiology, mechanisms, and prevention. Lancet 382, 339–352. https://doi.org/10.1016/S0140-6736(13)60595-4 (2013).
Foley, R. N., Parfrey, P. S. & Sarnak, M. J. Epidemiology of cardiovascular disease in chronic renal disease. J. Am. Soc. Nephrol. 9, S16-23 (1998).
Cheung, A. K. et al. Cardiac diseases in maintenance hemodialysis patients: Results of the HEMO study. Kidney Int. 65, 2380–2389. https://doi.org/10.1111/j.1523-1755.2004.00657.x (2004).
Stevens, L. A., Djurdjev, O., Cardew, S., Cameron, E. C. & Levin, A. Calcium, phosphate, and parathyroid hormone levels in combination and as a function of dialysis duration predict mortality: Evidence for the complexity of the association between mineral metabolism and outcomes. J. Am. Soc. Nephrol. 15, 770–779. https://doi.org/10.1097/01.asn.0000113243.24155.2f (2004).
Yamada, S. & Giachelli, C. M. Vascular calcification in CKD–MBD: Roles for phosphate, FGF23, and Klotho. Bone 100, 87–93. https://doi.org/10.1016/j.bone.2016.11.012 (2017).
Hruska, K. A., Sugatani, T., Agapova, O. & Fang, Y. The chronic kidney disease–mineral bone disorder (CKD–MBD): Advances in pathophysiology. Bone 100, 80–86. https://doi.org/10.1016/j.bone.2017.01.023 (2017).
Pavik, I. et al. Secreted Klotho and FGF23 in chronic kidney disease stage 1 to 5: A sequence suggested from a cross-sectional study. Nephrol. Dial. Transplant. 28, 352–359. https://doi.org/10.1093/ndt/gfs460 (2013).
Isakova, T. et al. Fibroblast growth factor 23 is elevated before parathyroid hormone and phosphate in chronic kidney disease. Kidney Int. 79, 1370–1378. https://doi.org/10.1038/ki.2011.47 (2011).
Wolf, M. Update on fibroblast growth factor 23 in chronic kidney disease. Kidney Int. 82, 737–747. https://doi.org/10.1038/ki.2012.176 (2012).
Stubbs, J., Liu, S. & Quarles, L. D. Role of fibroblast growth factor 23 in phosphate homeostasis and pathogenesis of disordered mineral metabolism in chronic kidney disease. Semin. Dial. 20, 302–308. https://doi.org/10.1111/j.1525-139x.2007.00308.x (2007).
Prié, D., Torres, P. U. & Friedlander, G. Latest findings in phosphate homeostasis. Kidney Int. 75, 882–889. https://doi.org/10.1038/ki.2008.643 (2009).
Vervloet, M. G. & Larsson, T. E. Fibroblast growth factor-23 and Klotho in chronic kidney disease. Kidney Int. Suppl. 1, 130–135. https://doi.org/10.1038/kisup.2011.29 (2011).
Prié, D. & Friedlander, G. Reciprocal control of 1,25-dihydroxyvitamin D and FGF23 formation involving the FGF23/Klotho system. Clin. J. Am. Soc. Nephrol. 5, 1717–1722. https://doi.org/10.2215/cjn.02680310 (2010).
Mutluay, R. et al. Serum fetuin-A is associated with the components of MIAC (malnutrition, inflammation, atherosclerosis, calcification) syndrome in different stages of chronic kidney disease. Turk. J. Med. Sci. 49, 327–335. https://doi.org/10.3906/sag-1809-43 (2019).
Sevinc, C., Yilmaz, G. & Ustundag, S. The relationship between calcification inhibitor levels in chronic kidney disease and the development of atherosclerosis. Ren. Fail. 43, 1349–1358. https://doi.org/10.1080/0886022x.2021.1969248 (2021).
Yeung, S. M. H., Bakker, S. J. L., Laverman, G. D. & De Borst, M. H. Fibroblast growth factor 23 and adverse clinical outcomes in type 2 diabetes: A bitter-sweet symphony. Curr. Diabetes Rep. 20, 50. https://doi.org/10.1007/s11892-020-01335-7 (2020).
Wahl, P. et al. Earlier onset and greater severity of disordered mineral metabolism in diabetic patients with chronic kidney disease. Diabetes Care 35, 994–1001. https://doi.org/10.2337/dc11-2235 (2012).
Esposito, C. et al. Comparing central aortic pressures obtained using a SphygmoCor device to pressures obtained using a pressure catheter. Am. J. Hypertens. 35, 397–406. https://doi.org/10.1093/ajh/hpac010 (2022).
Nolph, K. D. et al. Cross-sectional assessment of weekly urea and creatinine clearances in patients on continuous ambulatory peritoneal dialysis. ASAIO J. (Am. Soc. Artif. Intern. Organs 1992) 38, M139–M142. https://doi.org/10.1097/00002480-199207000-00004 (1992).
Jimbo, R. et al. Fibroblast growth factor 23 accelerates phosphate-induced vascular calcification in the absence of Klotho deficiency. Kidney Int. 85, 1103–1111. https://doi.org/10.1038/ki.2013.332 (2014).
de Borst, M. H., Vervloet, M. G., ter Wee, P. M. & Navis, G. Cross talk between the renin-angiotensin-aldosterone system and vitamin D-FGF-23-Klotho in chronic kidney disease. J. Am. Soc. Nephrol. 22, 1603–1609. https://doi.org/10.1681/asn.2010121251 (2011).
Silswal, N. et al. FGF23 directly impairs endothelium-dependent vasorelaxation by increasing superoxide levels and reducing nitric oxide bioavailability. Am. J. Physiol. Endocrinol. Metab. 307, E426–E436. https://doi.org/10.1152/ajpendo.00264.2014 (2014).
Vergara, N. et al. The direct effect of fibroblast growth factor 23 on vascular smooth muscle cell phenotype and function. Nephrol. Dial. Transplant. 38, 322–343. https://doi.org/10.1093/ndt/gfac220 (2022).
Durlacher-Betzer, K. et al. Interleukin-6 contributes to the increase in fibroblast growth factor 23 expression in acute and chronic kidney disease. Kidney Int. 94, 315–325. https://doi.org/10.1016/j.kint.2018.02.026 (2018).
Egli-Spichtig, D. et al. Tumor necrosis factor stimulates fibroblast growth factor 23 levels in chronic kidney disease and non-renal inflammation. Kidney Int. 96, 890–905. https://doi.org/10.1016/j.kint.2019.04.009 (2019).
Mirza, M. A. I., Larsson, A., Lind, L. & Larsson, T. E. Circulating fibroblast growth factor-23 is associated with vascular dysfunction in the community. Atherosclerosis 205, 385–390. https://doi.org/10.1016/j.atherosclerosis.2009.01.001 (2009).
Mirza, M. A. I. et al. Relationship between circulating FGF23 and total body atherosclerosis in the community. Nephrol. Dial. Transplant. 24, 3125–3131. https://doi.org/10.1093/ndt/gfp205 (2009).
Nasrallah, M. M. et al. Fibroblast growth factor-23 (FGF-23) is independently correlated to aortic calcification in haemodialysis patients. Nephrol. Dial. Transplant. 25, 2679–2685. https://doi.org/10.1093/ndt/gfq089 (2010).
Khan, A. M., Chirinos, J. A., Litt, H., Yang, W. & Rosas, S. E. FGF-23 and the progression of coronary arterial calcification in patients new to dialysis. Clin. J. Am. Soc. Nephrol. CJASN 7, 2017–2022. https://doi.org/10.2215/CJN.02160212 (2012).
Ozkok, A. et al. FGF-23 associated with the progression of coronary artery calcification in hemodialysis patients. BMC Nephrol. 14, 241. https://doi.org/10.1186/1471-2369-14-241 (2013).
Asicioglu, E. et al. Fibroblast growth factor-23 levels are associated with vascular calcifications in peritoneal dialysis patients. Nephron Clin. Pract. 124, 89–93. https://doi.org/10.1159/000355859 (2013).
Zeng, Y. et al. Role of fibroblast growth factor-23 in the pathogenesis of atherosclerosis in peritoneal dialysis patients. Genet. Mol. Res. GMR 14, 719–729. https://doi.org/10.4238/2015.January.30.15 (2015).
Llauradó, G. et al. FGF-23/vitamin D axis in type 1 diabetes: The potential role of mineral metabolism in arterial stiffness. PLoS One 10, e0140222. https://doi.org/10.1371/journal.pone.0140222 (2015).
Tuñón, J. et al. Circulating fibroblast growth factor-23 plasma levels predict adverse cardiovascular outcomes in patients with diabetes mellitus with coronary artery disease. Diabetes/Metab. Res. Rev. 32, 685–693. https://doi.org/10.1002/dmrr.2787 (2016).
Fitzpatrick, J. et al. Calcification biomarkers, subclinical vascular disease, and mortality among multiethnic dialysis patients. Kidney Int. Rep. 5, 1729–1737. https://doi.org/10.1016/j.ekir.2020.07.033 (2020).
Isakova, T. et al. Longitudinal FGF23 trajectories and mortality in patients with CKD. J. Am. Soc. Nephrol. 29, 579–590. https://doi.org/10.1681/asn.2017070772 (2018).
Komaba, H. et al. Fibroblast growth factor 23 and mortality among prevalent hemodialysis patients in the japan dialysis outcomes and practice patterns study. Kidney Int. Rep. 5, 1956–1964. https://doi.org/10.1016/j.ekir.2020.08.013 (2020).
Chonchol, M., Greene, T., Zhang, Y., Hoofnagle, A. N. & Cheung, A. K. Low vitamin D and high fibroblast growth factor 23 serum levels associate with infectious and cardiac deaths in the HEMO study. J. Am. Soc. Nephrol. 27, 227–237. https://doi.org/10.1681/asn.2014101009 (2016).
Isakova, T. et al. Fibroblast growth factor 23 in patients undergoing peritoneal dialysis. Clin. J. Am. Soc. Nephrol. CJASN 6, 2688–2695. https://doi.org/10.2215/CJN.04290511 (2011).
Yamada, S. et al. Relationship between residual renal function and serum fibroblast growth factor 23 in patients on peritoneal dialysis. Ther. Apheresis Dial. Off. Peer Rev. J. Int. Soc. Apheresis Jpn. Soc. Apheresis Jpn. Soc. Dial. Ther. 18, 383–390. https://doi.org/10.1111/1744-9987.12170 (2014).
Bär, L. et al. Insulin suppresses the production of fibroblast growth factor 23 (FGF23). Proc. Natl. Acad. Sci. U. S. A. 115, 5804–5809. https://doi.org/10.1073/pnas.1800160115 (2018).
Hermans, M. M. et al. Study on the relationship of serum fetuin-A concentration with aortic stiffness in patients on dialysis. Nephrol. Dial. Transplant. 21, 1293–1299. https://doi.org/10.1093/ndt/gfk045 (2006).
Stompór, T. et al. Pulse wave velocity and proteins regulating vascular calcification and bone mineralization in patients treated with peritoneal dialysis. Nephrol. Dial. Transplant. 21, 3605–3606. https://doi.org/10.1093/ndt/gfl409 (2006).
Schafer, C. et al. The serum protein alpha 2-Heremans-Schmid glycoprotein/fetuin-A is a systemically acting inhibitor of ectopic calcification. J. Clin. Invest. 112, 357–366. https://doi.org/10.1172/jci17202 (2003).
Ketteler, M. et al. Association of low fetuin-A (AHSG) concentrations in serum with cardiovascular mortality in patients on dialysis: A cross-sectional study. Lancet 361, 827–833. https://doi.org/10.1016/s0140-6736(03)12710-9 (2003).
Wang, A. Y. et al. Associations of serum fetuin-A with malnutrition, inflammation, atherosclerosis and valvular calcification syndrome and outcome in peritoneal dialysis patients. Nephrol. Dial. Transplant. 20, 1676–1685. https://doi.org/10.1093/ndt/gfh891 (2005).
Alkalbani, M., Prabhu, G., Lagbo, J. & Qayyum, R. Serum Klotho and pulse pressure; Insight from NHANES. Int. J. Cardiol. 355, 54–58. https://doi.org/10.1016/j.ijcard.2022.02.021 (2022).
Liang, W.-Y. et al. No significant association of serum klotho concentration with blood pressure and pulse wave velocity in a Chinese population. Sci. Rep. 11, 1–8 (2021).
Kim, H. J. et al. The association between soluble klotho and cardiovascular parameters in chronic kidney disease: Results from the KNOW-CKD study. BMC Nephrol. 19, 51. https://doi.org/10.1186/s12882-018-0851-3 (2018).
Funding
This work was supported by a grant from the Buddhist Tzu Chi Medical Foundation, Hualien, Taiwan (TCMF-A 106-01-09 and TCRD 111-056). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
B.-G.H. conceived and designed the experiments. B.-G.H., C.-H.W., J.-P.T., Y.-H.C., and S.-C.H. performed the experiments. Y.-L.L. analyzed the data. H.-J.H. and Y.-L.L. wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Huang, HJ., Hsu, BG., Wang, CH. et al. Diabetes mellitus modifies the association between chronic kidney disease–mineral and bone disorder biomarkers and aortic stiffness in peritoneal dialysis patients. Sci Rep 14, 4554 (2024). https://doi.org/10.1038/s41598-024-55364-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-55364-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.