Abstract
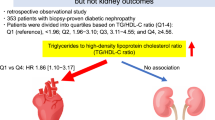
Hepatitis C virus (HCV) infection is prevalent in patients with type 2 diabetes mellitus (DM). We aimed to investigate whether HCV antibody (Ab) seropositivity is associated with diabetic micro- and macro-vascular diseases. In this hospital-based cross-sectional study, we retrospectively collected data from patients who participated in the diabetes pay-for-performance program and underwent HCV Ab screening in the annual comprehensive assessment between January 2021 and March 2022. We examined the relationships of HCV Ab seropositivity with the spot urinary albumin-to-creatinine ratio (UACR) and ankle-brachial index (ABI) in patients aged ≥ 50 years with type 2 DM. A total of 1758 patients were enrolled, and 85 (4.83%) of the enrolled patients had HCV Ab seropositivity. Multivariable regression analyses revealed that albuminuria showed a dose-dependent association with HCV Ab seropositivity (UACR [30–299 mg/g]: odds ratio [OR] = 1.463, 95% confidence interval [CI] 0.872‒2.456); UACR [≥ 300 mg/g]: OR = 2.300, 95% CI 1.160‒4.562; P for trend = 0.015) when compared with normal albuminuria (UACR < 30 mg/g). However, the proportion of patients with peripheral arterial disease, defined as an ABI ≤ 0.9, was not significantly different between the groups with and without HCV Ab seropositivity (3.5% vs. 3.9%, P = 0.999). In conclusion, severely increased albuminuria, but not the ABI, showed a significant association with HCV Ab seropositivity in patients aged ≥ 50 years with type 2 DM.
Similar content being viewed by others
Introduction
Hepatitis C virus (HCV) infection is a major cause of chronic liver disease, liver cirrhosis, and hepatocellular carcinoma1,2. The global prevalence of HCV antibody (HCV Ab) seropositivity increased from 2.3% in 1990 to 2.8% in 20053. The prevalence of HCV viremia was also reported to be approximately 1%4. Chronic hepatitis C infection and its sequelae place a global burden on the health care system and the economy1. In addition to hepatic sequelae, HCV causes several extrahepatic diseases that contribute significantly to the burden of this disease5. Type 2 diabetes mellitus (DM) is one of the most frequent and best characterized HCV-associated extrahepatic manifestations6. A higher risk of type 2 DM was reported in people with HCV infection than in those without HCV infection7, and the rate of HCV infection was also higher in people with type 2 DM than in those without type 2 DM8. Type 2 DM can cause several micro- and macro-vascular complications, such as nephropathy and cardiovascular disease (CVD)9, and HCV infection has also been reported to increase the risk of CVD and chronic kidney disease (CKD)10,11. Moreover, HCV treatment could reduce the risk of CVD and end-stage renal disease (ESRD) in patients with DM12. Therefore, early screening of HCV infection is an important concern for patients with DM.
Peripheral arterial disease (PAD) is a common macrovascular complication in patients with type 2 DM13. The ankle-brachial index (ABI) is a convenient tool to screen for PAD and is recommended for all patients with DM aged older than 50 years14. HCV infection increases the risk of developing PAD15. However, studies exploring the association between PAD based on ABI assessment and HCV infection in patients with DM are limited. On the other hand, albuminuria is a risk factor for CVD, diabetic kidney disease progression and all-cause mortality in patients with DM16,17. The spot urinary albumin-to-creatinine ratio (UACR) is widely recommended as a marker for quantifying proteinuria in patients with DM18. Increased albuminuria has been reported in patients with HCV infection19,20,21. However, to the best of our knowledge, studies exploring the association between the UACR and HCV infection have not focused on patients with type 2 DM.
Taiwan is a hyperendemic area for HCV infection22. The prevalence of HCV Ab seropositivity was reported to be 3.28% in the general population23, and to be 7.8% in the population with type 2 DM aged between 40 and 65 years24. To identify HCV infection is essential for the HCV elimination policy in Taiwan. According to the Taiwan hepatitis C policy guidelines25, people aged ≥ 45 years should be screened for HCV Ab. Furthermore, based on the recommendations of the diabetes pay-for-performance (P4P) program, an annual comprehensive assessment including the UACR and PAD should be performed for all patients with DM. We hypothesized that albuminuria and PAD would be associated with HCV infection. Therefore, we conducted a cross-sectional study with the aim of examining the prevalence of HCV Ab seropositivity in patients with type 2 DM categorized by the UACR or ABI.
Results
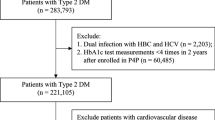
A total of 1758 patients with type 2 DM were enrolled in the study (Fig. 1), and their characteristics are shown in Table 1. There were 85 (4.83%) patients with HCV Ab seropositivity. Compared with the group without HCV Ab seropositivity, the group with HCV Ab seropositivity was older (69 ± 8 vs. 66 ± 9 years, P = 0.002) and had a higher systolic blood pressure (BP) (139 ± 17 vs. 133 ± 18 mm Hg, P = 0.004), a lower estimated glomerular filtration rate (eGFR) (68 ± 20 vs. 73 ± 22 mL/min/1.73 m2, P = 0.034), a higher UACR (274 ± 611 vs. 123 ± 433 mg/g, P = 0.002), a lower proportion of males (41.2% vs. 57.4%, P = 0.005), and a higher proportion of patients receiving insulin therapy (29.4% vs. 19.4%, P = 0.035). There was no significant difference in the proportion of patients with hypertension, the proportion of patients with CVD, diabetes duration, body mass index (BMI), diastolic BP, fasting glucose, hemoglobin A1c (HbA1c), total cholesterol, low density lipoprotein (LDL) cholesterol, high density lipoprotein (HDL) cholesterol, triglycerides, alanine aminotransferase (ALT), ABI, the proportion of patients with antiplatelet use, the proportion of patients with statin use, the proportion of patients with antihypertensive drug use, the proportion of patients with angiotensin-converting enzyme inhibitor or angiotensin II receptor antagonist use, or the proportion of patients with oral antihyperglycemic drug use between the groups with and without HCV Ab seropositivity.
The proportions of patients in different UACR categories between the groups with and without HCV Ab seropositivity are shown in Fig. 2. Patients with HCV Ab seropositivity had an increasing ratio trend in the severity of albuminuria compared to those without HCV Ab seropositivity; i.e., from normal albuminuria (49.4% vs. 67.2%) and moderately increased albuminuria (24.8% vs. 31.8%) to severely increased albuminuria (18.8% vs. 8.0%, P < 0.001). However, there was no significant difference in the proportion of patients with PAD between the groups with and without HCV Ab seropositivity (3.5% vs. 3.9%, P = 0.999).
To assess the potential risk factors for severely increased albuminuria, univariate regression analyses were performed (Table 2). Patients aged ≥ 65 years had a higher risk of severely increased albuminuria (odds ratio [OR] = 1.539, 95% confidence interval [CI] 1.082–2.188, P = 0.016) than subjects aged < 65 years; patients with hypertension had a higher risk of severely increased albuminuria (OR = 14.851, 95% CI 4.707–46.851, P < 0.001) than those without hypertension; and patients with a CVD history had a higher risk of severely increased albuminuria (OR = 3.243, 95% CI 2.072–5.076, P < 0.001) than those without a CVD history. Patients with a diabetes duration ≥ 10 years had a higher risk of severely increased albuminuria (OR = 2.078, 95% CI 1.420–3.043, P < 0.001) than those with a diabetes duration < 10 years. Patients with a BMI ≥ 25 kg/m2 had a higher risk of severely increased albuminuria (OR = 1.486, 95% CI 1.049–2.103, P = 0.026) than those with a BMI < 25 kg/m2; patients with a systolic BP ≥ 140 mm Hg had a higher risk of severely increased albuminuria (OR = 3.340, 95% CI 2.368‒4.711, P < 0.001) than those with a systolic BP < 140 mm Hg; and patients with a diastolic BP ≥ 90 mm Hg had a higher risk of severely increased albuminuria (OR = 3.360, 95% CI 2.203‒5.127, P < 0.001) than those with a diastolic BP < 90 mm Hg. An HbA1c level ≥ 7% was associated with a higher risk of severely increased albuminuria (OR = 2.149, 95% CI 1.523‒3.031, P < 0.001) than an HbA1c level < 7%; an LDL cholesterol level ≥ 2.59 mmol/L was associated with a higher risk of severely increased albuminuria (OR = 1.588, 95% CI1.086‒2.321, P = 0.017) than an LDL cholesterol level < 2.59 mmol/L; a low HDL cholesterol level was associated with a higher risk of severely increased albuminuria (OR = 1.873, 95% CI1.337‒2.625, P < 0.001) than a high HDL cholesterol level; and a triglyceride level ≥ 1.7 mmol/L was associated with a higher risk of severely increased albuminuria (OR = 4.918, 95% CI2.280‒10.608, P < 0.001) than a triglyceride level < 1.7 mmol/L. Patients with CKD had a higher risk of severely increased albuminuria (OR = 5.478, 95% CI 3.862‒7.771, P < 0.001) than those without CKD. Patients with an ABI ≤ 0.9 had a higher risk of severely increased albuminuria (OR = 2.962, 95% CI 1.604‒5.471, P < 0.001) than those with an ABI > 0.9. Patients who used antihypertensive drugs had a higher risk of severely increased albuminuria (OR = 2.359, 95% CI 1.645‒3.382, P < 0.001) than those who did not use antihypertensive drugs, and patients who received insulin therapy had a higher risk of severely increased albuminuria (OR = 4.023, 95% CI 2.846‒5.685, P < 0.001) than those who did not receive insulin therapy.
To assess the association between albuminuria and the presence of HCV Ab seropositivity, we selected age, sex, and other potential confounding risk factors that were significantly associated with both HCV Ab seropositivity (in Table 1) and severely increased albuminuria (in Table 2) for the multivariable logistic regression analyses (Table 3). Patients with a UACR ≥ 300 mg/g had a significantly higher risk of HCV Ab seropositivity (OR = 2.300, 95% CI 1.160‒4.562, P = 0.017) than patients with normal albuminuria. Although patients with a UACR of 30–299 mg/g had an increased risk of HCV Ab seropositivity compared with patients with normal albuminuria (OR = 1.463, 95% CI 0.872‒2.456, P = 0.150), the difference did not reach statistical significance. It is notable that the risk of HCV Ab seropositivity showed a significantly increasing trend with the severity of albuminuria (the P value for trend was 0.015 from normal albuminuria, moderately increased albuminuria, to severely increased albuminuria). Moreover, patients aged ≥ 65 years also had a significantly higher risk of chronic HCV infection (OR = 1.774, 95% CI 1.063‒2.959, P = 0.028) than those aged < 65 years, and male patients had a significantly lower risk of HCV Ab seropositivity (OR = 0.554, 95% CI 0.353‒0.868, P = 0.010) than female patients.
Discussion
The main finding of the current study was that severely increased albuminuria, but not PAD, was significantly associated with HCV Ab seropositivity in patients with type 2 DM aged ≥ 50 years. In the Third National Health and Nutrition Examination Survey (NHANES III), the prevalence of DM was twice as high in subjects who test positive for HCV antibody, and HCV Ab seropositivity was reported to be associated with an increased UACR (≥ 30 mg/g) in the subgroup without DM19. Similarly, Tsui et al. also reported that increased albuminuria and CKD were significantly associated with HCV Ab seropositivity, but only an increased UACR and not CKD was an independent factor for HCV Ab seropositivity after adjusting for confounding factors based on the NHANES III20. According to a community-based study of subjects aged 40–65 years in southern Taiwan, DM was associated with proteinuria detected using urine dipstick measurements, and HCV Ab seropositivity was significantly associated with proteinuria in the subgroup without DM21. The strength of the present study is that we explored the association between HCV Ab seropositivity and albuminuria in patients with type 2 DM. In particular, patients with severely increased albuminuria were at higher risk for HCV Ab seropositivity than patients with moderately increased albuminuria in comparison with patients with normal albuminuria, which emphasizes the dose-dependent association between the UACR and HCV Ab seropositivity. Kurbanova et al. also reported that HCV Ab seropositivity was associated with 50% and 95% higher odds of an increased UACR with cutoff values of 30 mg/g and 300 mg/g, respectively, in the NHANES III population, in which most individuals did not have DM26.
The exact mechanisms involved in proteinuria and HCV infection remain unclear. One of the possible mechanisms is that HCV infection can lead to insulin receptor defects, which induce insulin resistance27. Kawaguchi et al.28 reported that HCV promoted proteasomal degradation of insulin receptor substrates 1 and 2 via suppressor of cytokine signaling (SOCS) 3 expression in an in vitro study of transfected human hepatoma cells and an in vivo study of mice. Moreover, HCV-associated hepatic inflammation and damage may also cause insulin resistance. Konrad et al.29 reported that insulin sensitivity is inversely correlated with the histological activity index and fibrosis score based on liver biopsy. Narita et al.30 also reported that 27.5% of subjects with chronic hepatitis C infection but without known DM had abnormal glucose tolerance based on oral glucose tolerance tests, and abnormal glucose tolerance was significantly associated with the percentage of fibrosis based on liver biopsy. Shintani et al.31 found that in HCV transgenic mice, the ability of insulin to lower the plasma glucose level was impaired. Insulin resistance with hyperinsulinemia can contribute to renal injury through increased intrarenal production of insulin-like growth factor-1 and transforming growth factor-β and the expression of angiotensin II receptors in mesangial cells, which enhances the harmful effects of angiotensin II in the kidney. Increased endothelin-1 levels and oxidative stress and reduced nitric oxide synthesis by insulin resistance could induce renal injury32.
In addition to insulin resistance, antibodies induced by HCV-activating B lymphocytes may cause immune-mediated complexes, which deposit in the nephron and cause glomerular inflammation33,34. It is also hypothesized that HCV can directly damage the nephron because HCV particles have been found in renal tissues by electron microscopy35,36. Although the eGFR was lower in patients with HCV Ab seropositivity than in those without HCV Ab seropositivity, CKD was not an independent risk factor for HCV Ab seropositivity after adjusting for confounding factors in the present study. Several studies have reported that hepatitis C viral load is predictive of CKD in longitudinal follow-up37,38. However, according to the Taiwan National Health Insurance Research Database (NHRID), newly diagnosed HCV in patients aged ≥ 50 years did not significantly predict CKD during a mean follow-up of 7.12 years39. However, we did not collect data on HCV infection duration in this cross-sectional study.
Another important finding in our study was that the ABI was not significantly different between the groups with and without HCV Ab seropositivity. In line with our study, Cedarbaum et al.40 reported that HCV infection was not associated with PAD. In patients with regular hemodialysis, there was no significant difference in the ABI between those with or without HCV infection at baseline in an observational study41. The strength of our study is that a similar finding was validated in patients with type 2 DM. In contrast to the findings of the above cross-sectional studies, Sheen et al.42 reported that HCV was predictive of cardiovascular events in patients with type 2 DM enrolled in the P4P program. Hsu et al.15 reported that HCV infection was predictive of PAD according to the diagnostic codes retrieved from the Taiwan NHRID. During the 9-year cohort study, increased comorbidities were observed in patients with HCV infection, and HCV-associated comorbidities might contribute to the risk of PAD15. However, an ABI ≤ 0.9 had a low sensitivity in the diagnosis of PAD, especially in individuals with old age or DM43. The present study indicated that the ABI may have a low discriminative ability in the screening of PAD.
In the present study, HCV Ab seropositivity was associated with old age and female sex. In line with our findings, increased age and females were independent risk factors for HCV Ab seropositivity in a large Taiwanese cohort of volunteers in the Taiwan Biobank44. The higher prevalence of HCV Ab seropositivity in older people might result from a low seroreversion rate and persistent HCV Ab in serum that are detectable for many years45. Moreover, in this cross-sectional assessment, the old patients were born in the early years of a poor public health environment and had an increased risk of HCV infection46, such as unsterilized syringes and needles47. In a study using data from the Taiwan Biobank, males were reported to have a significantly lower risk for HCV Ab seropositivity than females45. However, the reason for increased HCV Ab seropositivity in females remains unknown.
We did not find a significant difference in ALT levels between patients with and without HCV Ab seropositivity in the present study. ALT levels could be associated with the severity of the necroinflammatory process and fibrosis, duration of chronic hepatitis, and HCV viral load48. Gulcan et al.49 reported that an increased ALT level was a risk factor for HCV Ab seropositivity in patients with DM. Korkmaz et al.50 also reported that ALT levels were positively correlated with the prevalence of HCV Ab seropositivity. In contrast, some studies reported that half of the patients with chronic HCV infections, even those who were untreated, displayed normal or minimally elevated serum ALT levels51.
There are several limitations in the present study. First, the causal relationship between HCV Ab seropositivity and albuminuria could not be established due to the cross-sectional design of the study. Second, we did not directly assess the mechanisms involved between HCV infection and the UACR in the study. Third, we did not have information on serum HCV ribonucleic acid (RNA) in the present study. Therefore, we could not assess the relationship between detectable HCV RNA and UACR or ABI in patients with HCV Ab seropositivity. The risk of kidney disease, defined as a UACR ≥ 30 mg/g or an eGFR < 60 mL/min/1.73 m2, has been reported to not be significantly different between resolved HCV infection (undetectable HCV RNA) and chronic HCV infection (detectable HCV RNA) in the patients with HCV Ab seropositivity; however, the risk of kidney disease might be higher in patients with HCV genotype 1 than in those with other HCV genotypes52. Fourth, we only included patients enrolled in the P4P program, which has been reported to attenuate chronic diabetic complications53,54,55. Fifth, we did not collect information on HCV Ab prior to the present study, and the duration of HCV infection was unknown. Finally, ABI was widely screened in patients aged ≥ 50 years in our hospital; therefore, the results cannot be applied to young patients because the prevalence of HCV infection and chronic diabetic complications are dependent on the age of the individuals in the population. It has been reported that the association between HCV Ab seropositivity and albuminuria was not significant in the population aged < 40 years20.
Conclusion
In patients with type 2 DM who were aged ≥ 50 years, severely increased albuminuria, but not the ABI, was associated with HCV Ab seropositivity. Furthermore, the UACR showed a dose-dependent association with HCV Ab seropositivity. For the efficient and effective identification of potential HCV infection, screening for HCV Ab seropositivity in individuals in the above population with severely increased albuminuria is warranted.
Methods
Patients
Based on the clinical recommendation25, HCV Ab screening was performed in the outpatient department at the Division of Endocrinology and Metabolism of Taichung Veterans General Hospital (VGH) when the annual comprehensive assessment was conducted between January 2021 and March 2022 for patients who had enrolled in the diabetes P4P program but had no available HCV Ab data one year prior to enrollment. In this cross-sectional study, we retrospectively collected the medical information of patients who met the following inclusion criteria: (1) age ≥ 50 years, (2) type 2 DM, (3) enrollment in the P4P program, and (4) having undergone HCV Ab assessment in the annual comprehensive assessment between January 2021 and March 2022. We excluded patients from this study according to the following criteria: (1) no ABI data, (2) an ABI ≥ 1.4 or a history of lower-limb operation, (3) blood pressure not detected at any limb, (4) end-stage renal disease, (5) no UACR data, and (6) pregnancy. The study protocol was approved by the Institutional Review Board of the Taichung VGH in Taiwan (TCVGH-IRB No. CE22395B), with a waiver for obtaining informed consent. Anonymous demographic characteristics and laboratory data were obtained from the Clinical Informatics Research and Development Center of Taichung VGH after delinking the identification information. All methods were performed in accordance with the relevant guidelines and regulations.
Assessment
The study data were collected from electronic medical record records, including the medical history of diabetes duration and CVD; demographic characteristics of age, sex, height, body weight, systolic BP, and diastolic BP; laboratory data of plasma glucose levels, HbA1c levels, and serum levels of total cholesterol, LDL cholesterol, HDL cholesterol, triglycerides, ALT, and creatinine; the UACR; and the ABI during the annual comprehensive assessment. According to our standard procedure in clinical practice, blood samples and urine samples were collected in the morning after an overnight fast. The current use of antidiabetic, antihypertensive, and antiplatelet drugs and statins was recorded during the annual comprehensive assessment.
HCV Ab was assayed by Elecsys Anti-HCV II (Roche Diagnostics GmbH, Mannheim, Germany). HbA1c levels were measured using cation-exchange high-performance liquid chromatography (National Glycohemoglobin Standardization Program, G8, TOSOH, Tokyo, Japan). Biochemical analyses were performed using a photometric enzymatic method with a chemical analyzer (Hitachi 7600, Tokyo, Japan). The eGFR was calculated using the modification of diet in renal disease equation as follows:
ABI measurements were performed using a validated device (VP-1000 Plus; Omron Healthcare Co. Ltd., Kyoto, Japan). After patients had rested in a supine position for at least 5 min, cuffs that were connected to both a plethysmographic sensor for detecting volume change and an oscillometric pressure sensor for detecting blood pressure were placed on the upper arms and ankles. An ABI ≤ 0.90 was defined as PAD14.
Type 2 DM was clinically diagnosed by physicians, and the diagnosis was confirmed twice within 90 days before the patient was enrolled in the P4P program. CKD was defined as an eGFR < 60 mL/min/1.73 m2, and ESRD was defined as renal replacement therapy or an eGFR < 15 mL/min/1.73 m2. Poor glucose control was defined as a fasting glucose level ≥ 7.2 mmol/L (130 mg/dL) or an HbA1c level ≥ 7.0%56. Hypercholesterolemia was defined as a total cholesterol level ≥ 4.14 mmol/L (160 mg/dL) or an LDL level ≥ 2.59 mmol/L (100 mg/dL), and hypertriglyceridemia was defined as a triglyceride level ≥ 1.7 mmol/L (150 mg/dL) according to the reference target goals56. Low HDL cholesterol was defined as an HDL level < 1.0 mmol/L (40 mg/dL) in men or < 1.3 mmol/L (50 mg/dL) in women56. The UACR was calculated using the following formula: UACR = albumin (mg)/creatinine (g). Normal albuminuria was defined as a UACR < 30 mg/g, moderately increased albuminuria was defined as a UACR between 30 and 299 mg/g, and severely increased albuminuria was defined as a UACR ≥ 300 mg/g based on the current clinical practice recommendations from the American Diabetes Association18.
Statistical analysis
All continuous data are presented as the mean ± standard deviation (SD). The categorical data are presented as the number and percentage. Independent t tests were conducted to detect significant between-group differences in continuous variables. Chi-square tests were conducted to detect differences in categorical variables. Logistic regression model which estimated OR and 95% CI was used to determine the factors associated with albuminuria and HCV Ab seropositivity. A trend test was additionally performed to examine the linear increasing trend of the risk changes associated with the UACR levels. Statistical analysis was performed using SPSS version 22.0 software (IBM Corp., Armonk, NY, USA).
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Thrift, A. P., El-Serag, H. B. & Kanwal, F. Global epidemiology and burden of HCV infection and HCV-related disease. Nat. Rev. Gastroenterol. Hepatol. 14, 122–132. https://doi.org/10.1038/nrgastro.2016.176 (2017).
Adler, M., Goubau, P., Nevens, F. & Van Vlierberghe, H. Hepatitis C virus: The burden of the disease. Acta Gastroenterol. Belg. 65, 83–86 (2002).
Mohd Hanafiah, K., Groeger, J., Flaxman, A. D. & Wiersma, S. T. Global epidemiology of hepatitis C virus infection: new estimates of age-specific antibody to HCV seroprevalence. Hepatology 57, 1333–1342. https://doi.org/10.1002/hep.26141 (2013).
Polaris Observatory HCV Collaborators. Global prevalence and genotype distribution of hepatitis C virus infection in 2015: A modelling study. Lancet Gastroenterol. Hepatol 2, 161–176. https://doi.org/10.1016/S2468-1253(16)30181-9 (2017).
Younossi, Z., Park, H., Henry, L., Adeyemi, A. & Stepanova, M. Extrahepatic manifestations of hepatitis C: A meta-analysis of prevalence, quality of life, and economic burden. Gastroenterology 150, 1599–1608. https://doi.org/10.1053/j.gastro.2016.02.039 (2016).
Songtanin, B. & Nugent, K. Burden, outcome, and comorbidities of Extrahepatic manifestations in hepatitis C virus infection. Biology 12, 23. https://doi.org/10.3390/biology12010023 (2022).
Naing, C., Mak, J. W., Ahmed, S. I. & Maung, M. Relationship between hepatitis C virus infection and type 2 diabetes mellitus: Meta-analysis. World J. Gastroenterol. 18, 1642–1651. https://doi.org/10.3748/wjg.v18.i14.1642 (2012).
Mason, A. L. et al. Association of diabetes mellitus and chronic hepatitis C virus infection. Hepatology 29, 328–333. https://doi.org/10.1002/hep.510290235 (1999).
Zheng, Y., Ley, S. H. & Hu, F. B. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat. Rev. Endocrinol. 14, 88–98. https://doi.org/10.1038/nrendo.2017.151 (2018).
Babiker, A. et al. Risk of cardiovascular disease due to chronic hepatitis C infection: a review. J. Hepatol. 5, 343–362. https://doi.org/10.1016/j.jhep.2016.07.039 (2017).
Butt, A. A., Wang, X. & Fried, L. F. HCV infection and the incidence of CKD. Am. J. Kidney Dis. 57, 396–402. https://doi.org/10.1053/j.ajkd.2010.09.023 (2011).
Hsu, Y. C. et al. Antiviral treatment for hepatitis C virus infection is associated with improved renal and cardiovascular outcomes in diabetic patients. Hepatology 59, 1293–1302. https://doi.org/10.1002/hep.26892 (2014).
Fowkes, F. G. et al. Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: A systematic review and analysis. Lancet 382, 1329–1340. https://doi.org/10.1016/S0140-6736(13)61249-0 (2013).
Gerhard-Herman, M. D. et al. 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: A report of the American college of cardiology/American heart association task force on clinical practice guidelines. Circulation 135, e726–e779. https://doi.org/10.1161/CIR.0000000000000471 (2017).
Hsu, Y. H. et al. Hepatitis C virus infection increases the risk of developing peripheral arterial disease: A 9-year population-based cohort study. J. Hepatol. 62, 519–525. https://doi.org/10.1016/j.jhep.2014.09.022 (2015).
Dunkler, D. et al. Risk prediction for early CKD in type 2 diabetes. Clin. J. Am. Soc. Nephrol. 10, 1371–1379. https://doi.org/10.2215/CJN.10321014 (2015).
Gerstein, H. C. et al. Albuminuria and risk of cardiovascular events, death, and heart failure in diabetic and nondiabetic individuals. JAMA 286, 421–426. https://doi.org/10.1001/jama.286.4.421 (2001).
ElSayed, N. A. et al. 11. Chronic kidney disease and risk management: standards of care in diabetes-2023. Diabetes Care 46, S191–S202. https://doi.org/10.2337/dc23-S011 (2023).
Liangpunsakul, S. & Chalasani, N. Relationship between hepatitis C and microalbuminuria: results from the NHANES III. Kidney Int. 67, 285–290. https://doi.org/10.1111/j.1523-1755.2005.00080.x (2005).
Tsui, J. I., Vittinghoff, E., Shlipak, M. G. & O’Hare, A. M. Relationship between hepatitis C and chronic kidney disease: Results from the third national health and nutrition examination survey. J. Am. Soc. Nephrol. 17, 1168–1174. https://doi.org/10.1681/ASN.2005091006 (2006).
Huang, J. F. et al. Viral hepatitis and proteinuria in an area endemic for hepatitis B and C infections: another chain of link?. Intern. Med. 260, 255–262. https://doi.org/10.1111/j.1365-2796.2006.01686.x (2006).
Bennett, H. et al. A review of the burden of hepatitis C infection in China, Japan, South Korea and Taiwan. Hepatol. Int. 9, 378–390. https://doi.org/10.1007/s12072-015-9629-x (2015).
Yu, M. L. et al. Huge gap between clinical efficacy and community effectiveness in the treatment of chronic hepatitis C: A nationwide survey in Taiwan. Medicine 94, e690. https://doi.org/10.1097/MD.0000000000000690 (2015).
Huang, J. F. et al. Hepatitis C viremia increases the association with type 2 diabetes mellitus in a hepatitis B and C endemic area: An epidemiological link with virological implication. Am. J. Gastroenterol. 102, 1237–1243. https://doi.org/10.1111/j.1572-0241.2007.01181.x (2007).
Taiwan hepatitis C policy guidelines 2018–2025. Taipei City: Ministry of Health and Welfare, Executive Yuan Taiwan. https://www.globalhep.org/evidence-base/taiwan-hepatitis-c-policy-guidelines-2018-2025 (2019).
Kurbanova, N. & Qayyum, R. Association of hepatitis C virus infection with proteinuria and glomerular filtration rate. Clin. Transl. Sci. 8, 421–424. https://doi.org/10.1111/cts.12321 (2015).
Aytug, S., Reich, D., Sapiro, L. E., Bernstein, D. & Begum, N. Impaired IRS-1/PI3-kinase signaling in patients with HCV: A mechanism for increased prevalence of type 2 diabetes. Hepatology 38, 1384–1392. https://doi.org/10.1016/j.hep.2003.09.012 (2003).
Kawaguchi, T. et al. Hepatitis C virus down-regulates insulin receptor substrates 1 and 2 through up-regulation of suppressor of cytokine signaling 3. Am. J. Pathol. 165, 1499–1508. https://doi.org/10.1016/S0002-9440(10)63408-6 (2004).
Konrad, T. et al. Severity of HCV-induced liver damage alters glucose homeostasis in noncirrhotic patients with chronic HCV infection. Digestion 62, 52–59. https://doi.org/10.1159/000007778 (2000).
Narita, R. et al. Insulin resistance and insulin secretion in chronic hepatitis C virus infection. J. Hepatol. 41, 132–138. https://doi.org/10.1016/j.jhep.2004.03.020 (2004).
Shintani, Y. et al. Hepatitis C virus infection and diabetes: Direct involvement of the virus in the development of insulin resistance. Gastroenterology 126, 840–848. https://doi.org/10.1053/j.gastro.2003.11.056 (2004).
Sarafidis, P. A. & Ruilope, L. M. Insulin resistance, hyperinsulinemia, and renal injury: Mechanisms and implications. Am. J. Nephrol. 26, 232–244. https://doi.org/10.1159/000093632 (2006).
Johnson, R. J. et al. Membranoproliferative glomerulonephritis associated with hepatitis C virus infection. N. Engl. J. Med. 328, 465–470. https://doi.org/10.1056/NEJM199302183280703 (1993).
Fabrizi, F. et al. Hepatitis C virus infection, mixed cryoglobulinemia, and kidney disease. Am. J. Kidney Dis. 61, 623–637. https://doi.org/10.1053/j.ajkd.2012.08.040 (2013).
Sabry, A. et al. HCV associated glomerulopathy in Egyptian patients: Clinicopathological analysis. Virology 334, 10–16. https://doi.org/10.1016/j.virol.2005.01.013 (2005).
Habas, E. et al. Hepatitis virus C-associated nephropathy: A review and update. Cureus 14, e27322. https://doi.org/10.7759/cureus.27322 (2022).
Lai, T. S. et al. High hepatitis C viral load and genotype 2 are strong predictors of chronic kidney disease. Kidney int. 92, 703–709. https://doi.org/10.1016/j.kint.2017.03.021 (2017).
Lai, T. S. et al. Hepatitis C viral load, genotype, and increased risk of developing end-stage renal disease: REVEAL-HCV study. Hepatology 66, 784–793. https://doi.org/10.1002/hep.29192 (2017).
Chen, Y. C., Lin, H. Y., Li, C. Y., Lee, M. S. & Su, Y. C. A nationwide cohort study suggests that hepatitis C virus infection is associated with increased risk of chronic kidney disease. Kidney int. 85, 1200–1207. https://doi.org/10.1038/ki.2013.455 (2014).
Cedarbaum, E. et al. Contributions of HIV, hepatitis C virus, and traditional vascular risk factors to peripheral artery disease in women. AIDS 33, 2025–2033. https://doi.org/10.1097/QAD.0000000000002319 (2019).
Matsumae, T. et al. What factors accelerate aortic stiffening in hemodialysis patients? An observational study. Hypertens. Res. 33, 243–249. https://doi.org/10.1038/hr.2009.219 (2010).
Sheen, Y. J., Hsu, C. C., Kung, P. T., Chiu, L. T. & Tsai, W. C. Impact of chronic hepatitis on cardiovascular events among type 2 diabetes patients in Taiwan pay-for-performance program. Sci. Rep. 12, 11720. https://doi.org/10.1038/s41598-022-15827-x (2022).
Dachun, Xu. et al. Sensitivity and specificity of the ankle–brachial index to diagnose peripheral artery disease: A structured review. Vasc. Med. 15, 361–369. https://doi.org/10.1177/1358863X10378376 (2010).
Wang, A. C., Geng, J. H., Wang, C. W., Wu, D. W. & Chen, S. C. Sex difference in the associations among risk factors with hepatitis B and C infections in a large Taiwanese population study. Front. Public Health 10, 1068078. https://doi.org/10.3389/fpubh.2022.1068078 (2022).
Lefrère, J. J. et al. Full or partial seroreversion in patients infected by hepatitis C virus. J. Infect. Dis. 175, 316–322. https://doi.org/10.1093/infdis/175.2.316 (1997).
Chen, C. H. et al. Estimation of seroprevalence of hepatitis B virus and hepatitis C virus in Taiwan from a large-scale survey of free hepatitis screening participants. J. Formos. Med. Assoc. 106, 148–155. https://doi.org/10.1016/S0929-6646(09)60231-X (2007).
Sun, C. A. et al. Persistent hyperendemicity of hepatitis C virus infection in Taiwan: The important role of iatrogenic risk factors. J. Med. Virol. 65, 30–34 (2001).
Akkaya, O., Kiyici, M., Yilmaz, Y., Ulukaya, E. & Yerci, O. Clinical significance of activity of ALT enzyme in patients with hepatitis C virus. World J. Gastroenterol. 13, 5481–5485. https://doi.org/10.3748/wjg.v13.i41.5481 (2007).
Gulcan, A., Gulcan, E., Toker, A., Bulut, I. & Akcan, Y. Evaluation of risk factors and seroprevalence of hepatitis B and C in diabetic patients in Kutahya, Turkey. J. Investig. Med. 56, 858–863. https://doi.org/10.2310/JIM.0b013e3181788d28 (2008).
Korkmaz, H. et al. Assessment of evidence for positive association and seroprevalence of hepatitis B and C in diabetic patients in a developing country. J. Investig. Med. 63, 251–257. https://doi.org/10.1097/JIM.0000000000000126 (2015).
Puoti, C., Castellacci, R. & Montagnese, F. Hepatitis C virus carriers with persistently normal aminotransferase levels: Healthy people or true patients?. Dig. Liver Dis. 32, 634–643. https://doi.org/10.1016/s1590-8658(00)80850-6 (2000).
Chen, Y. C., Wang, H. W., Huang, Y. T. & Jiang, M. Y. Association of hepatitis C virus infection status and genotype with kidney disease risk: A population-based cross-sectional study. PLoS One 17, e0271197. https://doi.org/10.1371/journal.pone.0271197 (2022).
Lee, I. T. et al. Pay-for-performance for shared care of diabetes in Taiwan. J. Formos. Med. Assoc. 118, S122–S129. https://doi.org/10.1016/j.jfma.2019.08.011 (2019).
Chen, Y. C., Liao, Y. H., Ku, L. E. & Wang, J. D. Pay-for-performance and continuity of care synergistically reduced amputation of lower extremity in patients with diabetes: A population-based cohort study. BMC Health Serv. Res. 22, 748. https://doi.org/10.1186/s12913-022-08075-2 (2022).
Hsieh, H. M. et al. The association between participation in a pay-for-performance program and macrovascular complications in patients with type 2 diabetes in Taiwan: A nationwide population-based cohort study. Prev. Med. 85, 53–59. https://doi.org/10.1016/j.ypmed.2015.12.013 (2016).
Diabetes Association of The Republic of China Taiwan. Executive summary of the DAROC clinical practice guidelines for diabetes care- 2018. J. Formos. Med. Assoc. 119, 577–586. https://doi.org/10.1016/j.jfma.2019.02.016 (2020).
Acknowledgements
We thank the Diabetes Care Center and Clinical Informatics Research and Development Center of Taichung Veterans General Hospital for their support. Statistical analysis was performed by the Biostatistics Task Force of Taichung Veterans General Hospital.
Funding
This work was supported by a grant from Taichung Veterans General Hospital, Taichung, Taiwan [Grant Number TCVGH-1123501C] and the Ministry of Science and Technology, Taiwan [Grant Number MOST 110-2314-B-075A-004-MY3]. The funding bodies had no role in the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
Y.C., T.L., H.L., Y.L., H.L., M.S., and I.L. were involved in the conception, design, and conduct of the study. Y.C. and I.L. were involved in the analysis and interpretation of the results. Y.C. wrote the draft of the manuscript. I.L. and M.S. critically revised the draft of the manuscript. All authors edited, reviewed, and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cheng, YC., Lee, TY., Li, YH. et al. Hepatitis C virus antibody seropositivity is associated with albuminuria but not peripheral artery disease in patients with type 2 diabetes. Sci Rep 14, 4607 (2024). https://doi.org/10.1038/s41598-024-55352-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-55352-7
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.