Abstract
Early preventive measures against depression have become important with unprecedented global aging. Increase in one’s perceived value (PV) may correspond to better mental health outcomes. This cross-sectional observation study aimed to clarify whether the PV of adopting new behaviors is associated with depressive symptoms. The participants were 5266 community-dwelling older adults aged ≥ 65 years. We developed a questionnaire to measure the PV of adopting new behaviors, specifically activities beneficial for preventing depressive symptoms (physical, cognitive, and social activities) in older adults. The questionnaire asked whether adopting the ten selected behaviors was valuable. The scores were added, and the total score ranged from − 20 to 20. The odds ratios (OR) of depressive symptoms were calculated using binomial logistic regression according to the PV score quartiles. Depressive symptoms were reported by 595 (11.3%) participants. After adjusting for potential confounders, higher quartiles of PV scores were significantly associated with lower prevalence of depressive symptoms: vs Q1; Q2 OR 0.76 (95% confidence interval: 0.59–0.97); Q3 0.67 (0.51–0.87); Q4 0.54 (0.40–0.73) (P for trend < .001). Having a higher PV of adopting new behaviors may prevent depressive symptoms among older adults. Healthcare professionals need to pay attention to poor value orientation among older adults.
Similar content being viewed by others
Introduction
Depression is a common mental health disorder among the older population and a major cause of adverse life and health outcomes, such as low quality of life, worsening of comorbid illnesses, functional and cognitive decline, and the development of disabilities1,2,3,4. A pooled analysis of 24 studies involving community-based older adults reported that the prevalence of depressive disorders among older adults is 17.1%5. With unprecedented global aging, early preventive measures are particularly important.
Engaging in regular physical, cognitive, and social activities is beneficial for preventing frailty and depressive symptoms6,7,8,9,10,11,12,13,14. Systematic reviews and meta-analyses of longitudinal observations and intervention studies have shown a protective effect of physical activity against depressive symptoms9,10. Physical activity can contribute to the natural production of endorphins (endogenous opioid neuropeptides including serotonin, dopamine, and noradrenaline), which help reduce depressive symptoms15. The relationship between cognitive activity and reduced depressive symptoms has been reported in some observational studies. However, other than the commonality that cognitive decline is accompanied by depressive symptoms, the underlying mechanisms remain unclear8,9,11. Various definitions of social aspects (e.g., social activity, interaction, and networks) have been found to have a protective effect on depression8,12,13,14. However, inducing behavior change is generally challenging16.
The role of values has gained attention in recent years17,18,19,20. Values are defined as cognitive beliefs about what is important, good, and worthwhile for individuals or societies, and what is not17. Personal values determine what we consider important and worthwhile in life and are widely believed to serve as behavioral and motivational guides21,22. Studies on values in relation to health have revealed that values correlate with subjective well-being, life satisfaction, quality of life, and mental health disorders, such as depression17,18,19,20. Research has assessed values using Schwartz's theory of basic human values and demonstrated that openness to change values are negatively correlated with depressive symptoms in adolescents18,20. Openness to change reflects one’s readiness for change; thus, how people perceive to be valuable for change may be associated with depressive symptoms. In the case of health behaviors such as physical, cognitive, and social activities, perceived value (PV) may be associated with engagement in those activities; in turn, an increase in the PV of adopting new behaviors could correspond to better long-term mental health outcomes.
Intervention trials have shown that perceptions can be modified through experience or appropriate education23,24. Cognitive behavioral therapy, a well-known psychological treatment for psychiatric disorders, involves changing patients’ perceptions and thinking patterns through psychoeducation, homework, behavioral activation, and problem-solving, used alone or in combination25. This indicates that identifying those with a low PV of adopting new behaviors and enhancing their PV through education or other means may contribute to behavioral change and promoting mental health, consequently preventing depressive symptoms.
To date, the relationship between the PV of adopting new behaviors and depressive symptoms remains unclear. Therefore, this study aimed to clarify whether the PV of adopting new behaviors is associated with depressive symptoms in community-dwelling older adults.
Methods
Study design and participants
This cross-sectional study enrolled community-dwelling older adults from a sub-cohort of the National Center for Geriatrics and Gerontology Study of Geriatric Syndromes, which is a population-based national cohort study that aims to establish a screening system for geriatric syndromes and validate evidence-based interventions to prevent them26. This sub-cohort included older adults aged ≥ 65 years in March, 2017, who resided in Tokai city, a residential suburb in Nagoya, Japan. Invitation letters for baseline health checkup were sent to 20,248 independent residents aged ≥ 65 years who were not hospitalized, in residential care, or participating in another study. Written informed consent was obtained from all participants before they participated in the study. The study protocol was conducted in accordance with the Declaration of Helsinki and approved by the ethics committee of the National Center for Geriatrics and Gerontology (No. 1440-5).
A total of 5,563 older adults in Tokai City participated in health checkups. For our analysis, we excluded participants with incomplete responses to questions about their perceptions toward adopting new behaviors (n = 98), those with a history of dementia (n = 11), Parkinson’s disease (n = 17), depression (n = 97), severe cognitive decline [Mini-Mental State Examination scores (MMSE) < 18 (n = 21)]8,27, those with a lack of independence in basic activities of daily living [such as eating, bathing, grooming, walking, and stair-climbing (n = 13)], and those with functional disabilities as certified by the national long-term care insurance system (n = 27). We also excluded patients with incomplete responses to depressive symptoms (n = 13). Finally, 5266 participants were included in the final analysis. All assessments were performed by well-trained study assistants at community centers.
Measurements
Depressive symptoms
Depressive symptoms were assessed using the 15-item Geriatric Depression Scale (short form)28, which has demonstrated adequate validity as a measure of depression among older adults. This short version was developed by selecting the 15 items that had the highest correlation with depressive symptoms and was validated with a high overall correlation with the original version (r = 0.89)29, A cut-off score of ≥ 6 was confirmed to have a sensitivity of 82% and specificity of 75% compared with a structured interview for clinical depression30.
PV questionnaire
There is no questionnaire to measure the PV of adopting new behaviors. The questions were developed by consulting gerontology experts who had a Ph.D. in health and social science or rehabilitation science to assess whether participants perceived to be valuable for adopting new health behaviors. Ten behaviors were selected, focusing on physical, cognitive, and social activities that relate to reduced geriatric syndrome including depressive symptoms. These activities are often closely interrelated; for example, physical activities include exercising or sports, which can be performed alone or with other people, and team sports, which provide social interaction. Some cognitive activities, such as participating in group discussions, also have social aspects. Thus, behaviors were selected to include physical and cognitive activities as well as social interactions that accompany reported health behaviors such as playing ground golf, taking enrichment classes, and attending a community meeting8,31. In addition, because the sense of economy, a lack of occupation, and loneliness, may influence one’s participation in activities, the ten behaviors included starting a paid activity, having a job, and some behaviors related to social networking and contacts that are opposite of loneliness6,32,33. We asked participants whether adopting the following behaviors was valuable: (1) making a new friend, (2) making a new chatting acquaintance, (3) starting a new paid activity, (4) belonging to a new group, (5) interacting with people of different ages and sexes, (6) starting a new exercise or sport, (7) starting a new cognitive activity, (8) starting to participate in social activities, (9) increasing opportunities to talk to new people, and (10) starting a new job with no experience. For each question, participants chose their responses from “not at all = − 2,” “not so much = − 1,” “somewhat valuable = 1,” and “very valuable = 2.” These values were added to obtain the total score that ranged from − 20 to 20.
Potential confounding factors
The potential confounders of depressive symptoms were selected based on previous studies30,34,35,36,37,38. The demographic characteristics included age, sex, years of education, and living status (whether one lived alone). We also included annual household income, alcohol consumption, and smoking as demographic characteristics because they may be associated with depressive symptoms39,40. Health factors included history of heart disease, stroke, hypertension, hyperlipidemia, diabetes, body mass index, cognitive status (MMSE), and slow gait. Pain was also included as a health factor because an association between pain and depression has been reported41. Data on these factors were obtained through interviews and measurements conducted by nurses and trained staff. Walking speed was measured by asking the participants to walk for 6.4 m at a comfortable speed on a flat, carpeted surface with no shoes, and a walking speed of 2.4 m in the middle of the whole walkway was measured. A digital stopwatch was used to automatically determine when participants walked past infrared sensors at the start and end of the measurement area. A walking speed less than 1.0 m/s was defined as a slow gait37. Physical, cognitive, and social activities were included as an engagement in activities. Engagement in physical and cognitive activities was assessed using a leisure activity score that consisted of 11 physical activities (playing tennis or golf, swimming, bicycling, dancing, participating in group exercises, playing team games (e.g., bowling), walking for exercise, climbing more than two flights of stairs, doing housework, and babysitting) and 6 cognitive activities (reading books or newspapers, writing for pleasure, doing crossword puzzles, playing board games or cards, participating in organized group discussions, and playing musical instruments)42. Participants reported their frequency of engagement as “daily,” “several days a week,” “once weekly,” monthly,” “occasionally,” or “never,” and the scores were calculated according to frequency, ranging from 0 to 77 for physical activity and 0 to 42 for cognitive activity. Social activities were assessed based on how many of the following behaviors the participants engaged in: (1) going out for tea or dining with friends, (2) shopping with friends, (3) having conversations with anyone, and (4) having paid work8,13.
Statistical analysis
Participants’ characteristics were compared between participants with and without depressive symptoms using unpaired t-tests or Pearson’s chi-square tests. Internal consistency was evaluated using Cronbach’s alpha coefficient and was considered adequate (> 0.70)43. The test–retest reliability of each component was assessed using the intraclass correlation coefficient (ICC). Based on the 95% confidence intervals (CIs) of the ICC estimate, values less than 0.5, between 0.5 and 0.75, between 0.75 and 0.9, and greater than 0.90 are indicative of poor, moderate, good, and excellent reliability, respectively44. The participants were divided into quartiles of PV scores. The variables were compared using one-way analysis of variance and Pearson’s chi-square test. The association between the score and the presence of depressive symptoms was examined using binomial logistic regression analysis with crude and adjusted models for potential confounding factors. Data were presented as odds ratios (ORs) with 95% CIs. All analyses were performed using IBM SPSS Statistics, version 28 (IBM Japan, Tokyo). Statistical significance was set at a two-tailed probability of P < 0.05.
Results
Participants enrolled in this study were 5,266 older adults (mean age with standard deviation (SD) = 74.1 ± 5.6 years; women = 55%). The differences in characteristics between participants with and without depressive symptoms are shown in Table 1. Of the 5266 participants, those who had depressive symptoms (595; 11.3%) were older, had fewer years of education and lower annual household income, lived alone, consumed less alcohol, smoked more, had more heart diseases, stroke, hyperlipidemia, pain, and cognitive decline, and had lower body mass index, slower gait, and less engagement in social activities (P < 0.05).
The internal reliability of the PV questionnaire, assessed using Cronbach’s alpha, was 0.925. The inter-item correlations were high for the scale (item test), and the coefficients ranged from 0.64 to 0.78. The ICC (1, 2) for the total score was 0.79 (95% CI 0.51–0.92) and indicated moderate to excellent test–retest reliability. The mean ± SD scores for the PV items ranged from 0.19 ± 1.34 to 0.98 ± 1.13 (Table 2). The mean, median, and interquartile ranges of the total scores were 6.38, 8, and 0–13, respectively. Each question item was significantly negatively associated with the GDS score, with correlation coefficients ranging from − 0.146 to − 0.216 (All, P < 0.001). All of the question items significantly correlated with physical, cognitive, and social activities (All, P < 0.001).
Table 3 shows participants’ characteristics according to the quartiles of the PV scores. Differences were observed in participants’ engagement in physical, cognitive, and social activities (P < 0.001); higher PV indicated more engagement in these activities. The ORs and 95% CIs estimated by both crude and adjusted binomial logistic regression analyses for depressive symptoms are shown in Table 4. The PV scores were significantly associated with depressive symptoms. In the adjusted model, compared to the Q1, higher PV scores were independently associated with lower prevalence of depressive symptoms (score range = -20–0, the lowest quartile) (Q2 OR = 0.76, 95% CI = 0.59–0.97; Q3 OR = 0.67, 95% CI = 0.51–0.87; Q4 OR = 0.54, 95% CI = 0.40–0.73; P for trend < 0.001).
Discussion
This study aimed to develop a new instrument to measure the PV of adopting new behaviors and clarify whether the PV of adopting new behaviors is associated with depressive symptoms. The internal consistency of the PV questionnaire was acceptable, with a Cronbach’s alpha coefficient of 0.925 and test–retest reliability, as measured by an ICC, of 0.7943,44. Higher PV scores were independently associated with a lower risk for depressive symptoms. To the best of our knowledge, this is the first study to clarify the association between the PV of adopting new behaviors and depressive symptoms among older adults.
The prevalence of depressive symptoms in this study was 11.3%. This result was similar to the findings of a report on Japanese older adults and the estimates from a meta-analysis of 24 studies worldwide5,12. Differences were found between those with and without depressive symptoms in demographic characteristics, such as age, education, annual household income, living situation, and smoking, health factors, such as history of heart disease and stroke, pain, cognitive decline, and slow gait, and engagement in activities, such as going out for tea or dining with friends and shopping with friends. These characteristics were generally consistent with the results of previous studies in Japan and other countries9,11,13,35,38.
Participants with a higher PV of adopting new behaviors were more likely to engage in physical, cognitive, and social activities than those with lower PV. The association between higher PV and higher engagement in activities observed in this study was not unexpected. Values guide, motivate, and influence attitudes and behaviors45. Although direct comparisons cannot be made, owing to the lack of reports examining the association between PV and actual engagement in health behaviors, consumer science research has focused on the relationship between PV and attitudes and intentions22,46,47. Ma et al. researched the effect of novel and environmentally friendly foods on consumer acceptance and found that PV had a significantly positive effect on attitude, and attitude also had a positive effect on purchase intention46. In Li et al.’s study, PV positively affected the behavioral intention of older adults to use remote health management services47. These studies showed a positive association between PV, intention, and behavior. In this context, our results can be considered reasonable.
The major finding of this study was that a higher PV is associated with a lower prevalence of depressive symptoms even after adjusting for engagement of activities. The finding of an inverse association between high PV and depressive symptoms was similar to that of previous studies involving adolescents18,20. These studies reported a negative association with Schwartz’s concept of openness to change values in all domains of values. Although Schwartz’s concept was not investigated in this study, the PV of adopting new behaviors assessed in this study may have a similar role to that of openness to change values among the various value domains21. An independent association between PV and depressive symptoms and actual engagement in the activities can be explained by the hierarchical effect of values, attitudes, and behaviors (ie, the value-attitude-behavior model)22,48. In this model, higher value orientation levels lead to higher individual attitude levels, and consequently, higher individual behavioral intentions and actual behavior48. For example, the aforementioned study of environmentally friendly foods showed that the higher the consumers’ perception of green value, the higher their attitude towards plant-based meat alternatives; then, the higher the attitude towards plant-based meat alternatives, the higher the purchase behavior of plant-based meat alternatives46. These linear correlations may also affect the degree of actual behavior. Thus, the intensity or density of the activity, which cannot be measured by questionnaires asking only about engagement in activities may have been affected by the degree of PV. In addition, those who participated in the activities may have simultaneously participated in activities other than those included in this study, and the high intensity or density of the activity guided by high PV may have suppressed depressive symptoms.
This study had several limitations. First, the study design was cross-sectional; therefore, we could not determine a causal relationship between the PV of adopting new behaviors and depressive symptoms. As depressive symptoms are accompanied by negative emotions and mood, we could not rule out that the PV may be lower because of the presence of depressive symptoms. Future studies should confirm the effects of PV on depressive symptoms and validate the questionnaire. A causal relationship, predictability of future development of depression, and the minimal clinically important difference above indicators should be explored through longitudinal observations or interventions. Second, the participants were assumed to be relatively healthy because they could voluntarily participate in health checkups conducted at community centers. This may have excluded individuals with severe depressive symptoms or other conditions. In addition, our participants were single ethnic and individual regions of people who were relatively mentally healthy, limiting the extent to which our conclusions can be extrapolated to broader populations. Future research with more diverse samples is needed to enhance the external validity and generalizability of our results. Third, engagement in activities was assessed using frequency or dichotomous responses. Future studies should use measurements that can evaluate both the quantity and quality of activities. Fourth, unadjusted variables such as employment and marital status may confound the association between PV and depressive symptoms; however, the E-value for the odds ratio for the Q4 group was 3.18 (CI, 2.12), which indicates the association of unadjusted confounding factor would have to be stronger than 3.18 to overturn the result49. Despite these limitations, the major strengths of this study are the large sample size of community-dwelling older adults and comprehensive set of assessments.
Conclusion
Actual behavior may be influenced by PV, which is inversely associated with depressive symptoms independent of actual engagement in physical, cognitive, and social activities in community-dwelling older adults. Healthcare professionals and those involved in social welfare must pay attention to poor value orientation in older adults, suggesting the need to develop interventions to promote mental health by enhancing PV through education on the benefits of engagement in physical, cognitive, and social activities and sharing success experiences.
Data availability
The datasets used and/or analyzed during the present study are available from the corresponding author upon reasonable request.
References
Norton, S., Matthews, F. E., Barnes, D. E., Yaffe, K. & Brayne, C. Potential for primary prevention of Alzheimer’s disease: An analysis of population-based data. Lancet Neurol. 13, 788–794. https://doi.org/10.1016/s1474-4422(14)70136-x (2014).
Blazer, D. G. Depression in late life: Review and commentary. J. Gerontol. A Biol. Sci. Med. Sci. 58, 249–265. https://doi.org/10.1093/gerona/58.3.m249 (2003).
Sivertsen, H., Bjørkløf, G. H., Engedal, K., Selbæk, G. & Helvik, A. S. Depression and quality of life in older persons: A review. Dement. Geriatr. Cogn. Disord. 40, 311–339. https://doi.org/10.1159/000437299 (2015).
Schillerstrom, J. E., Royall, D. R. & Palmer, R. F. Depression, disability and intermediate pathways: A review of longitudinal studies in elders. J. Geriatr. Psychiatry Neurol. 21, 183–197. https://doi.org/10.1177/0891988708320971 (2008).
Luppa, M. et al. Age- and gender-specific prevalence of depression in latest-life—systematic review and meta-analysis. J. Affect. Disord. 136, 212–221. https://doi.org/10.1016/j.jad.2010.11.033 (2012).
Sacha, J., Sacha, M., Soboń, J., Borysiuk, Z. & Feusette, P. Is It time to begin a public campaign concerning frailty and pre-frailty? A review article. Front. Physiol. 8, 484. https://doi.org/10.3389/fphys.2017.00484 (2017).
Ijaz, N. et al. Interventions for frailty among older adults with cardiovascular disease: JACC state-of-the-art review. J. Am. Coll. Cardiol. 79, 482–503. https://doi.org/10.1016/j.jacc.2021.11.029 (2022).
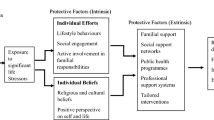
Uemura, K. et al. Behavioral protective factors of increased depressive symptoms in community-dwelling older adults: A prospective cohort study. Int. J. Geriatr. Psychiatry 33, e234–e241. https://doi.org/10.1002/gps.4776 (2018).
Maier, A., Riedel-Heller, S. G., Pabst, A. & Luppa, M. Risk factors and protective factors of depression in older people 65+. A systematic review. PLoS ONE 16, e0251326. https://doi.org/10.1371/journal.pone.0251326 (2021).
Pearce, M. et al. Association between physical activity and risk of depression: A systematic review and meta-analysis. JAMA Psychiatry 79, 550–559. https://doi.org/10.1001/jamapsychiatry.2022.0609 (2022).
Zheng, F., Zhong, B., Song, X. & Xie, W. Persistent depressive symptoms and cognitive decline in older adults. Br. J. Psychiatry 213, 638–644. https://doi.org/10.1192/bjp.2018.155 (2018).
Bae, S. et al. A new social network scale for detecting depressive symptoms in older Japanese adults. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph17238874 (2020).
Katayama, O. et al. Are non-face-to-face interactions an effective strategy for maintaining mental and physical health?. Arch. Gerontol. Geriatr. 98, 104560. https://doi.org/10.1016/j.archger.2021.104560 (2022).
Kim, Y. R. & Jung, H. S. Effects of social interaction and depression on homeboundness in community-dwelling older adults living alone. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph19063608 (2022).
Matei, D. et al. The endocannabinoid system and physical exercise. Int. J. Mol. Sci. https://doi.org/10.3390/ijms24031989 (2023).
Guthold, R., Stevens, G. A., Riley, L. M. & Bull, F. C. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob. Health 6, e1077–e1086. https://doi.org/10.1016/S2214-109X(18)30357-7 (2018).
Xie, J. Q. et al. Latent profile analysis of personal values among Chinese college students: Associations with mental health disorders and life satisfaction. Curr. Psychol. https://doi.org/10.1007/s12144-022-03861-x (2022).
Liu, P. et al. The benefits of self-transcendence: Examining the role of values on mental health among adolescents across regions in China. Front. Psychol. 12, 630420. https://doi.org/10.3389/fpsyg.2021.630420 (2021).
Bojanowska, A., Kaczmarek, ŁD., Koscielniak, M. & Urbańska, B. Changes in values and well-being amidst the COVID-19 pandemic in Poland. PLoS ONE 16, e0255491. https://doi.org/10.1371/journal.pone.0255491 (2021).
Heim, E., Maercker, A. & Boer, D. Value orientations and mental health: A theoretical review. Transcult. Psychiatry 56, 449–470. https://doi.org/10.1177/1363461519832472 (2019).
Schwartz, S. H. In Advances in Experimental Social Psychology vol. 25 (ed. Zanna, M. P.) 1–65 (Academic Press, 1992).
Tudoran, A., Olsen, S. O. & Dopico, D. C. The effect of health benefit information on consumers health value, attitudes and intentions. Appetite 52, 568–579. https://doi.org/10.1016/j.appet.2009.01.009 (2009).
Alvarez, M. D., Inelmen, K. & Yarcan, Ş. Do perceptions change? A comparative study. Anatolia 20, 401–418. https://doi.org/10.1080/13032917.2009.10518917 (2009).
Chiba, T. et al. An educational intervention improved knowledge of dietary supplements in college students. BMC Public Health 20, 633. https://doi.org/10.1186/s12889-020-08786-3 (2020).
López-López, J. A. et al. The process and delivery of CBT for depression in adults: A systematic review and network meta-analysis. Psychol. Med. 49, 1937–1947. https://doi.org/10.1017/s003329171900120x (2019).
Shimada, H. et al. Impact of cognitive frailty on daily activities in older persons. J. Nutr. Health Aging 20, 729–735. https://doi.org/10.1007/s12603-016-0685-2 (2016).
Folstein, M. F., Folstein, S. E. & McHugh, P. R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 12, 189–198. https://doi.org/10.1016/0022-3956(75)90026-6 (1975).
Yesavage, J. A. Geriatric depression scale. Psychopharmacol. Bull. 24, 709–711 (1988).
Lesher, E. L. & Berryhill, J. S. Validation of the Geriatric Depression Scale-Short Form among inpatients. J. Clin. Psychol. 50, 256–260. https://doi.org/10.1002/1097-4679(199403)50:2%3c256::aid-jclp2270500218%3e3.0.co;2-e (1994).
Friedman, B., Heisel, M. J. & Delavan, R. L. Psychometric properties of the 15-item geriatric depression scale in functionally impaired, cognitively intact, community-dwelling elderly primary care patients. J. Am. Geriatr. Soc. 53, 1570–1576. https://doi.org/10.1111/j.1532-5415.2005.53461.x (2005).
Bae, S. et al. Engagement in lifestyle activities is associated with increased Alzheimer’s disease-associated cortical thickness and cognitive performance in older adults. J. Clin. Med. https://doi.org/10.3390/jcm9051424 (2020).
Franco, M. R. et al. Older people’s perspectives on participation in physical activity: A systematic review and thematic synthesis of qualitative literature. Br. J. Sports Med. 49, 1268–1276. https://doi.org/10.1136/bjsports-2014-094015 (2015).
Hämmig, O. Health risks associated with social isolation in general and in young, middle and old age. PLoS ONE 14, e0219663. https://doi.org/10.1371/journal.pone.0219663 (2019).
Makizako, H. et al. Social frailty in community-dwelling older adults as a risk factor for disability. J. Am. Med. Dir. Assoc. 16(1003), e1007-1011. https://doi.org/10.1016/j.jamda.2015.08.023 (2015).
Tsutsumimoto, K. et al. Prospective associations between sedentary behaviour and incident depressive symptoms in older people: A 15-month longitudinal cohort study. Int. J. Geriatr. Psychiatry 32, 193–200. https://doi.org/10.1002/gps.4461 (2017).
Shimada, H. et al. Depressive symptoms and cognitive performance in older adults. J. Psychiatr. Res. 57, 149–156. https://doi.org/10.1016/j.jpsychires.2014.06.004 (2014).
Shimada, H. et al. Prevalence of psychological frailty in Japan: NCGG-SGS as a Japanese National Cohort Study. J. Clin. Med. https://doi.org/10.3390/jcm8101554 (2019).
Patel, K. V. et al. Symptom burden among community-dwelling older adults in the United States. J. Am. Geriatr. Soc. 67, 223–231. https://doi.org/10.1111/jgs.15673 (2019).
Ridley, M., Rao, G., Schilbach, F. & Patel, V. Poverty, depression, and anxiety: Causal evidence and mechanisms. Science https://doi.org/10.1126/science.aay0214 (2020).
Tiguman, G. M. B., Silva, M. T. & Galvão, T. F. Prevalence of depressive and anxiety symptoms and their relationship with life-threatening events, tobacco dependence and hazardous alcohol drinking: A population-based study in the Brazilian Amazon. J. Affect. Disord. 298, 224–231. https://doi.org/10.1016/j.jad.2021.10.059 (2022).
Hajihasani, A., Rouhani, M., Salavati, M., Hedayati, R. & Kahlaee, A. H. The influence of cognitive behavioral therapy on pain, quality of life, and depression in patients receiving physical therapy for chronic low back pain: A systematic review. Pm r 11, 167–176. https://doi.org/10.1016/j.pmrj.2018.09.029 (2019).
Verghese, J. et al. Leisure activities and the risk of dementia in the elderly. N. Engl. J. Med. 348, 2508–2516. https://doi.org/10.1056/NEJMoa022252 (2003).
Terwee, C. B. et al. Quality criteria were proposed for measurement properties of health status questionnaires. J. Clin. Epidemiol. 60, 34–42. https://doi.org/10.1016/j.jclinepi.2006.03.012 (2007).
Koo, T. K. & Li, M. Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 15, 155–163. https://doi.org/10.1016/j.jcm.2016.02.012 (2016).
Boer, D. & Fischer, R. How and when do personal values guide our attitudes and sociality? Explaining cross-cultural variability in attitude-value linkages. Psychol. Bull. 139, 1113–1147. https://doi.org/10.1037/a0031347 (2013).
Ma, C. C. & Chang, H. P. The effect of novel and environmentally friendly foods on consumer attitude and behavior: A value-attitude-behavioral model. Foods https://doi.org/10.3390/foods11162423 (2022).
Li, W. et al. Determinants of intention with remote health management service among urban older adults: A Unified Theory of Acceptance and Use of Technology perspective. Front. Public Health 11, 1117518. https://doi.org/10.3389/fpubh.2023.1117518 (2023).
Yan, C. et al. Bi-dimensional values and attitudes toward online fast food-buying intention during the COVID-19 pandemic: An application of VAB model. Front. Nutr. 9, 894765. https://doi.org/10.3389/fnut.2022.894765 (2022).
VanderWeele, T. J. & Ding, P. Sensitivity analysis in observational research: Introducing the E-value. Ann. Intern. Med. 167, 268–274. https://doi.org/10.7326/M16-2607 (2017).
Acknowledgements
We are grateful to the residents and officers of Tokai City and our healthcare staff members. We would also like to thank Editage for English language editing.
Funding
This work was funded by AMED (Grants 15dk0207019h0001, 18dk0110021h0003, and 18le0110004h0002), Research Funding for Longevity Sciences (27-22 and 28-30) from the National Center for Geriatrics and Gerontology (NCGG) and Kao Corporation, and Grant-in-Aid for Early-Career Scientists (grant number: 23K16836). The funders did not have a role in the study design, in the collection, analysis, and interpretation of data, in the writing of the report, or in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
C.N., S.L., and H.S. conceptualized and designed the study. C.N. conducted data analysis and drafted the manuscript. O.K., S.L., K.M., K.H., M.M., K.T., R.Y., K.F., Y.M., C.N., and H.S. collected the data and contributed to the editorial process and review of the manuscript. All authors carried out a critical revision of the manuscript for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nishijima, C., Katayama, O., Lee, S. et al. Association between the perceived value of adopting new behaviors and depressive symptoms among older adults. Sci Rep 14, 4569 (2024). https://doi.org/10.1038/s41598-024-55301-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-55301-4
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.