Abstract
The purpose of this study was to determine the long-term pattern of plasma aldosterone concentration (PAC) trajectories and to explore the relationship between PAC trajectory patterns and cardiovascular disease (CVD) risk in patients with hypertension. Participants were surveyed three times between 2010 and 2016, and latent mixed modeling was employed to determine the trajectory of PAC over the exposure period (2010–2016). A Cox regression analysis was used to examine the association between PAC trajectory patterns and the risk of CVD (stroke and myocardial infarction). Hazard ratios (HRs) with corresponding 95% confidence intervals (CIs) were calculated and reported. During a median follow-up of 4.10 (3.37–4.50) years, 82 incident CVD cases (33 myocardial infarction cases and 49 stroke cases) were identified. Among all three PAC models, the high-stability PAC pattern exhibited the highest risk of CVD. After full adjustment for all covariables, HRs were 2.19 (95% CI 1.59–3.01) for the moderate-stable pattern and 2.56 (95% CI 1.68–3.91) for the high-stable pattern in comparison to the low-stable pattern. Subgroup and sensitivity analyses verified this association. The presence of a high-stable PAC trajectory pattern is associated with an elevated risk of CVD in hypertensive patients. Nevertheless, more studies are warranted to confirm these findings.
Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) is the leading cause of mortality worldwide, posing a significant threat to human health1. In China, the burden of CVD is substantial, with 120.33 million individuals affected by CVD and 4.58 million CVD-related deaths recorded in 2019, placing strain on the healthcare system2. Hypertension, a preventable risk factor, plays a crucial role in the development of CVD and premature mortality globally3. Unfortunately, hypertension is highly prevalent in China and is projected to surge in the coming decades4. Among the Chinese population, hypertension represents the most significant risk factor for CVD5, accounting for 43% of CVD cases2,6. Therefore, the identification of high-risk individuals among hypertensive patients is crucial for alleviating the burden of CVD.
Plasma aldosterone concentration (PAC) is a notable and controllable risk factor for CVD that has a high degree of prognostic significance for the disease burden in the future7,8,9,10. Several studies have demonstrated that elevated PAC is an independent risk factor for incident CVD11,12,13,14,15. However, it is noteworthy that most published studies in this area have relied on a single measurement of PAC, neglecting the potential effects of heterogeneous long-term PAC patterns16,17,18,19. This limitation may bias the true relationship between PAC and CVD, favoring the null hypothesis. The formation of severe and complex intramural lesions leading to plaque rupture often takes years, despite the rapid manifestation of CVD20,21. Thus, longitudinal studies are essential for a comprehensive understanding of how long-term PAC trajectory patterns influence the development of CVD.
This study sought to ascertain the trajectories of PAC among 2254 hypertensive adults across a 6-year exposure period and investigate the relationship between these trajectories and the subsequent risk of CVD. We hypothesize that PAC trajectories can serve as predictors for the development of CVD. Therefore, examining patterns of change in PAC prior to the diagnosis of CVD may enhance the effectiveness of preventive and therapeutic interventions for this disease.
Material and methods
Study population
A cohort of 18,609 hypertensive adults was recruited from the People's Hospital of Xinjiang Uygur Autonomous Region and advised to undergo physical examinations at least once every 1 to 2 years. The initial three surveys (2010–2011, 2012–2013, and 2014–2015) enrolled 8179 participants. For the present analysis, 1124 participants were excluded due to a lack of follow-up data or less than 1 year of follow-up after 2016. Furthermore, we excluded 963 participants who had been diagnosed with myocardial infarction (MI), stroke, or cancer in or before 2016 (the baseline for this analysis). In addition, 3838 participants were excluded because PAC data from the three preceding surveys were unavailable. Therefore, a total of 2254 participants were ultimately included in the study (Fig. S1). PAC trajectory patterns were developed from 2010 to 2016 to predict CVD risk from 2016 to 2021 (Fig. 1). Ethical approval was secured from the Ethical Committee (No. KY2022080906), and the study adhered to the STROBE statement guidelines. We confirmed that all methods were performed in accordance with relevant guidelines and regulations, and all participants provided written informed consent.
Covariate collection and definitions
Demographic, lifestyle, laboratory, medication, and medical history data were collected from electronic medical records for this study. Anthropometric data, including body mass index (BMI) and systolic and diastolic blood pressures (SBP and DBP), were collected using standardized methods. Alcohol use and smoking habits were categorized as either current or not. Blood samples were collected while the subjects were fasting. The central laboratory of the hospital measured the levels of high-density lipoprotein (HDL) cholesterol, low-density lipoprotein (LDL) cholesterol, fasting plasma glucose (FPG), total cholesterol (TC), triglycerides (TG), uric acid (UA), and high-sensitivity C-reactive protein (hs-CRP). PAC was measured using the radioimmunoassay method (DSL-8600 ACTIVE Aldosterone Coated Tube Radioimmunoassay Kit; Diagnostic Systems Laboratories, Webster, TX). Detailed descriptions of the measurement procedures can be found in previous studies22,23. The estimated glomerular filtration rate (eGFR) was calculated using the CKD-EPI formula24. A list of the medications used in the study can be found in Table S1. The medical history included records of hypertension, dyslipidemia, diabetes, chronic kidney disease (CKD), and primary aldosteronism (PA). For detailed information on the diagnostic criteria for the aforementioned medical history, please refer to the Supplemental Material. Comorbidities were characterized using the Charlson Comorbidity Index (CCI), as previously described25.
Outcome measurement and follow-up
The primary endpoint of the study was the first occurrence of CVD, which encompasses both stroke and MI. Comprehensive definitions of CVD can be found in the Supplemental Materials. To obtain information regarding each participant's endpoint event, we gathered data from various sources, including hospital records, regional sickness and death registration systems, reconciliation with the national health insurance system, and interviews for confirmation. The follow-up period began in 2016 and ended with the earliest occurrence of CVD diagnosis, death, or on December 31, 2021, whichever occurred first.
Statistical analysis
Latent mixture modeling in the SAS Proc Traj was utilized to identify patterns of PAC trajectories ranging from 2010 to 201626. The model with three classes was determined to have the best fit using the Bayesian information criterion (BIC), which was used to assess the model fit (Fig. 2 and Table S2). Missing covariate data (less than 10% missing) was imputed using 10 multiple imputations. To compare the disease-free survival rates between the groups, Kaplan–Meier and log-rank analyses were applied. The proportional hazards assumption was evaluated but not violated based on Schoenfeld residuals. Cox regression analyses were used to examine the relationship between PAC trajectory patterns and CVD risk. Hazard ratios (HR) and 95% confidence intervals (CI) were reported. Additionally, stratified analyses were performed, and interactions between subgroups were tested. Several sensitivity analyses were conducted to verify the reliability of the findings. More detailed information on statistical analysis is provided in the Supplemental Material. Any two-sided P value < 0.05 was statistically significant. Statistical analyses were performed using SAS 9.4 and R 4.1.1.
Results
Baseline characteristics
Table 1 provides a summary of the fundamental characteristics of 2254 hypertensive patients in 2016. These characteristics were based on the patterns of plasma aldosterone concentration (PAC) trajectories observed during the period of 2006–2010. Specifically, we identified three distinct patterns: low-stable (n = 1262), moderate-stable (n = 744), and high-stable (n = 248), as depicted in Fig. 2. Statistically significant differences were observed among the three groups in terms of heart rate, SBP, DBP, levels of TG, HDL cholesterol, FPG, UA, and BMI. Additionally, there were notable variations in the prevalence of diabetes, CKD, PA, and dyslipidemia, as well as differences in smoking status and the proportion of participants taking statins, aspirin, angiotensin-converting enzyme inhibitors (ACEIs)/angiotensin receptor blockers (ARBs), spironolactone, and glucose-lowering agents. However, no significant differences were observed among the three groups in terms of age, sex, TC, LDL cholesterol, eGFR, drinking status, or the proportion of participants taking beta-blockers and calcium channel blockers.
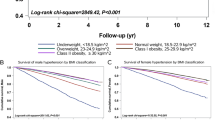
Relationship between PAC trajectory patterns and CVD risk
During a median follow-up period of 4.10 (3.37–4.50) years, we identified 82 cases of incident CVD, consisting of 33 cases of MI and 49 cases of stroke. The Kaplan–Meier curve demonstrated that participants in the high-stable PAC group exhibited a significantly elevated risk of CVD, stroke, and MI compared to other trajectory groups (log-rank P < 0.001 for all) (Fig. 3A–C). Among the three PAC models, the high-stability pattern was associated with the highest risk of CVD (Table 2). In model 4, the HRs were 2.19 (95% CI 1.59–3.11) for the moderate-stable pattern and 2.56 (95% CI 1.68–3.91) for the high-stable pattern as opposed to the low-stable pattern. The results for stroke and MI were consistent with those for CVD.
Subgroup and sensitivity analysis
The associations between patterns of PAC trajectories and CVD, stratified by age, sex, BMI, smoking status, drinking status, and diabetes, are presented in Table 3. No significant interactions were found between the PAC trajectory patterns and age, sex, BMI, smoking or drinking status, or diabetes (P for interaction > 0.05 for all). The results did not change substantially in the sensitivity analysis by excluding subjects diagnosed with CVD in the two years before follow-up, individuals with a history of PA, or participants with CCI ≥ 2 (Tables S3–S5). Moreover, analyses without multiple imputations of covariates produced results that aligned with those of the primary analysis (Table S6). Accounting for the competing risk of mortality in an additional analysis yielded outcomes comparable to those in the primary analysis (Table S7). Furthermore, we observed that significant correlations between PAC trajectories and CVD risk continued to persist, even after further adjusting for the baseline level of PAC (Table S8). Lastly, the E-values computed for the study's outcomes ranged from 3.35 to 5.13, indicating a moderate strength of evidence against potential unmeasured confounding variables (Table S9).
Discussion
This study represents the first longitudinal investigation, to our knowledge, that comprehensively examines the effect of observed changes in PAC on the risk of CVD. In our investigation, we categorized PAC trajectory patterns between 2010 and 2016 into three distinct groups: low-stable, moderate-stable, and high-stable. We found that hypertensive patients with a persistently high PAC level over the long term had a significantly elevated risk of CVD during the follow-up period, compared to those in the low-stable group. Importantly, these findings were consistent across various sensitivity and subgroup analyses, reinforcing their robustness. These results suggest that monitoring changes in PAC trajectory could serve as a valuable approach for identifying individuals at risk of CVD and aiding in the prevention of new-onset CVD in hypertensive patients.
Several observational studies in patients with heart failure have shown that PAC levels are closely linked to an elevated risk of recurrent myocardial infarction, severe heart failure, or cardiovascular mortality16,18,19,27. In a cohort of patients scheduled for coronary angiography, variation in PAC levels within the normal range was associated with increased all-cause and CVD mortality, independent of other major CVD risk factors28. Similarly, Hillaert et al. demonstrated that in patients with stable coronary artery disease, PAC levels were independently linked with the risk of major vascular events, vascular death, and atherosclerotic burden29. Ivanes et al. also found a strong independent association between PAC levels and the occurrence of acute ischemic events in patients with coronary artery disease without heart failure or acute myocardial infarction16. Notably, they observed a stronger association between higher PAC levels and overall CVD mortality and sudden cardiac death in patients with lower renal function14. A community-based cohort study conducted in the United States revealed a nonlinear relationship between higher PAC levels and increased CVD risk, independent of known cardiovascular risk factors. The use of renin–angiotensin–aldosterone system antagonists does not affect the relationship between PAC and CVD11. However, it is worth noting that a limited number of studies have reported a nonsignificant relationship between PAC and CVD. For instance, the KORA F4 study found a nonsignificant trend suggesting a positive association between higher PAC levels and cardiovascular mortality, stroke, and composite cardiovascular endpoints, but not with MI30. Another cohort study of patients with chronic renal insufficiency showed that higher PAC levels were independently associated with the development of congestive heart failure but not with end-stage renal disease, atherosclerotic events, or death13. These conflicting findings may be attributed to the fact that previous studies primarily focused on absolute PAC levels at baseline and subsequent CVD risk rather than considering changes in PAC over time. To address this gap in knowledge, our study adopted a longitudinal cohort design to explore the association between PAC trajectory patterns and CVD. By examining the relationship between PAC trajectory patterns and cardiovascular health status, our study contributes to the limited available evidence and introduces a potential novel indicator for the prevention of CVD.
The mechanisms linking a high-stable PAC trajectory to CVD risk are not completely understood. Several plausible mechanisms may contribute to this observation. Through a number of mechanisms, including the suppression of endothelial function, persistent intravascular fluid retention, and the production of target-organ inflammation and fibrosis, aldosterone probably aids in the development and/or progression of CVD31,32. First, the traditional action of excessive aldosterone causing incorrect volume retention directly causes increases in cardiac output, BP, glomerular filtration rate, and intracardiac volume33,34. Elevated BP, stemming from increased intravascular volume, raises the risk of heart disease, stroke, and CKD35,36,37,38. Chronic increases in left atrial volume can predispose to arrhythmias, particularly atrial fibrillation, whereas chronic increases in intracardiac volume are likely to raise the chance of developing heart failure, particularly in the presence of uncontrolled hypertension39,40,41,42. Renal plasma blood flow increases along with an increase in circulating volume. Increased glomerular dysfunction, such as proteinuria, is brought on by the corresponding rise in intraglomerular pressure and glomerular filtration rate43,44,45. Additionally, aldosterone may exert other effects on the pathophysiology of CVD, including atherogenesis, heightened sympathetic activity, impaired pressure reflex function, and increased thrombosis31,46,47.
To our knowledge, this is the first study to investigate the impact of PAC trajectory patterns on CVD risk in Chinese hypertensive patients. The strengths of this study encompass its longitudinal design, large sample size, repeated measurements of study variables, and robustness of the observed associations. Nevertheless, certain limitations should be acknowledged. Firstly, due to the observational nature of the study, causal conclusions cannot be drawn. Secondly, despite controlling for a range of potential confounders, we cannot completely exclude all residual and unmeasured confounders, such as genetic predisposition, diet, medication, and family history. Thirdly, the focus of data collection on stroke and MI may underestimate the overall incidence of CVD. Fourthly, this study population included only Chinese hypertensive patients and therefore should be extended to other population groups with caution. Fifthly, only three different stable trajectories were found in the current study, and further studies of other populations with less stable trajectories are required to investigate the role of PAC changes in the development of CVD. Lastly, multiple PAC measurements may be needed in clinical practice before determining the trajectory of patients, making their use limited in daily clinical practice.
Conclusion
In summary, long-term PAC patterns were linked to altered CVD risk, and higher levels of PAC over time were significantly associated with an elevated risk of CVD in patients with hypertension. These findings underscore the potential of monitoring long-term PAC patterns as a valuable tool for identifying individuals at heightened risk of CVD. Nevertheless, additional studies need to be conducted to validate these findings.
Data availability
The manuscript contains all the evidence that supports the findings. The datasets used and/or analyzed in this study are available from the corresponding author on request if necessary.
References
Roth, G. A. et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: Update from the GBD 2019 study. J. Am. Coll. Cardiol. 76(25), 2982–3021 (2020).
Zhao, D., Liu, J., Wang, M., Zhang, X. & Zhou, M. Epidemiology of cardiovascular disease in China: Current features and implications. Nat. Rev. Cardiol. 16(4), 203–212 (2019).
Lewington, S. et al. The burden of hypertension and associated risk for cardiovascular mortality in China. JAMA Intern. Med. 176(4), 524–532 (2016).
Wang, J. G., Zhang, W., Li, Y. & Liu, L. Hypertension in China: Epidemiology and treatment initiatives. Nat. Rev. Cardiol. 20, 531–545 (2023).
Yin, R. et al. Hypertension in China: Burdens, guidelines and policy responses: A state-of-the-art review. J. Hum. Hypertens. 36(2), 126–134 (2022).
Wang, Z. et al. Status of hypertension in China: Results from the China hypertension survey, 2012–2015. Circulation. 137(22), 2344–2356 (2018).
Parksook, W. W. & Williams, G. H. Aldosterone and cardiovascular diseases. Cardiovasc. Res. 119(1), 28–44 (2023).
Monticone, S. et al. Cardiovascular events and target organ damage in primary aldosteronism compared with essential hypertension: A systematic review and meta-analysis. Lancet Diabetes Endocrinol. 6(1), 41–50 (2018).
Brown, N. J. Contribution of aldosterone to cardiovascular and renal inflammation and fibrosis. Nat. Rev. Nephrol. 9(8), 459–469 (2013).
Rossi, G., Boscaro, M., Ronconi, V. & Funder, J. W. Aldosterone as a cardiovascular risk factor. Trends Endocrinol. Metab. 16(3), 104–107 (2005).
Joseph, J. J. et al. Aldosterone, renin, cardiovascular events, and all-cause mortality among African Americans: The Jackson Heart Study. JACC Heart Fail. 5(9), 642–651 (2017).
Joseph, J. J. et al. Association of serum aldosterone and plasma renin activity with ambulatory blood pressure in African Americans: The Jackson Heart Study. Circulation. 143(24), 2355–2366 (2021).
Deo, R. et al. Serum aldosterone and death, end-stage renal disease, and cardiovascular events in blacks and whites: Findings from the Chronic Renal Insufficiency Cohort (CRIC) Study. Hypertension. 64(1), 103–110 (2014).
Tomaschitz, A. et al. Association of plasma aldosterone with cardiovascular mortality in patients with low estimated GFR: The Ludwigshafen Risk and Cardiovascular Health (LURIC) Study. Am. J. Kidney Dis. 57(3), 403–414 (2011).
Haze, T. et al. Association of aldosterone and blood pressure with the risk for cardiovascular events after treatments in primary aldosteronism. Atherosclerosis. 324, 84–90 (2021).
Ivanes, F. et al. Aldosterone, mortality, and acute ischaemic events in coronary artery disease patients outside the setting of acute myocardial infarction or heart failure. Eur. Heart J. 33(2), 191–202 (2012).
Inoue, K. et al. Serum aldosterone concentration, blood pressure, and coronary artery calcium: The multi-ethnic study of atherosclerosis. Hypertension. 76(1), 113–120 (2020).
Güder, G. et al. Complementary and incremental mortality risk prediction by cortisol and aldosterone in chronic heart failure. Circulation. 115(13), 1754–1761 (2007).
Beygui, F. et al. High plasma aldosterone levels on admission are associated with death in patients presenting with acute ST-elevation myocardial infarction. Circulation. 114(24), 2604–2610 (2006).
Okafor, O. N. & Gorog, D. A. Endogenous fibrinolysis: An important mediator of thrombus formation and cardiovascular risk. J. Am. Coll. Cardiol. 65(16), 1683–1699 (2015).
Thim, T., Hagensen, M. K., Bentzon, J. F. & Falk, E. From vulnerable plaque to atherothrombosis. J. Intern. Med. 263(5), 506–516 (2008).
Hu, J. et al. Relationship between plasma aldosterone concentrations and non-alcoholic fatty liver disease diagnosis in patients with hypertension: A retrospective cohort study. Diabetes Metab. Syndr. Obes. 16, 1625–1636 (2023).
Zhu, Q. et al. Higher plasma aldosterone concentrations are associated with elevated risk of aortic dissection and aneurysm: A case-control study. Hypertension. 79(4), 736–746 (2022).
Levey, A. S. et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 150(9), 604–612 (2009).
Sundararajan, V. et al. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J. Clin. Epidemiol. 57(12), 1288–1294 (2004).
Wu, S. et al. Association of trajectory of cardiovascular health score and incident cardiovascular disease. JAMA Netw. Open. 2(5), e194758 (2019).
Palmer, B. R. et al. Plasma aldosterone levels during hospitalization are predictive of survival post-myocardial infarction. Eur. Heart J. 29(20), 2489–2496 (2008).
Tomaschitz, A. et al. Plasma aldosterone levels are associated with increased cardiovascular mortality: The Ludwigshafen Risk and Cardiovascular Health (LURIC) study. Eur. Heart J. 31(10), 1237–1247 (2010).
Hillaert, M. A. et al. Aldosterone, atherosclerosis and vascular events in patients with stable coronary artery disease. Int. J. Cardiol. 167(5), 1929–1935 (2013).
Then, C. et al. Association of aldosterone with mortality in the general population. Exp. Clin. Endocrinol. Diabetes. 131(5), 307–313 (2023).
Gaddam, K. K., Pimenta, E., Husain, S. & Calhoun, D. A. Aldosterone and cardiovascular disease. Curr. Probl. Cardiol. 34(2), 51–84 (2009).
Connell, J. M., MacKenzie, S. M., Freel, E. M., Fraser, R. & Davies, E. A lifetime of aldosterone excess: Long-term consequences of altered regulation of aldosterone production for cardiovascular function. Endocr. Rev. 29(2), 133–154 (2008).
Náray-Fejes-Tóth, A. & Fejes-Tóth, G. The sgk, an aldosterone-induced gene in mineralocorticoid target cells, regulates the epithelial sodium channel. Kidney Int. 57(4), 1290–1294 (2000).
Fu, J. W. Aldosterone and mineralocorticoid receptors in the cardiovascular system. Prog. Cardiovasc. Dis. 52(5), 393–400 (2010).
Ku, E., Lee, B. J., Wei, J. & Weir, M. R. Hypertension in CKD: Core curriculum 2019. Am. J. Kidney Dis. 74(1), 120–131 (2019).
Li, C., Engström, G., Hedblad, B., Berglund, G. & Janzon, L. Blood pressure control and risk of stroke: A population-based prospective cohort study. Stroke. 36(4), 725–730 (2005).
Schieb, L. J., Greer, S. A., Ritchey, M. D., George, M. G. & Casper, M. L. Vital signs: Avoidable deaths from heart disease, stroke, and hypertensive disease—United States, 2001–2010. MMWR Morb. Mortal Wkly. Rep. 62(35), 721–727 (2013).
Rosendorff, C. et al. Treatment of hypertension in the prevention and management of ischemic heart disease: A scientific statement from the American Heart Association Council for High Blood Pressure Research and the Councils on Clinical Cardiology and Epidemiology and Prevention. Circulation. 115(21), 2761–2788 (2007).
Messerli, F. H., Rimoldi, S. F. & Bangalore, S. The transition from hypertension to heart failure: Contemporary update. JACC Heart Fail. 5(8), 543–551 (2017).
Bayés-Genís, A. & Díez, J. Transition to heart failure in hypertension: Going to the heart of the matter. Eur. Heart J. 43(35), 3332–3334 (2022).
Reddy, Y., Borlaug, B. A. & Gersh, B. J. Management of atrial fibrillation across the spectrum of heart failure with preserved and reduced ejection fraction. Circulation. 146(4), 339–357 (2022).
Inciardi, R. M. et al. Left atrial disease and left atrial reverse remodelling across different stages of heart failure development and progression: A new target for prevention and treatment. Eur. J. Heart Fail. 24(6), 959–975 (2022).
Hollenberg, N. K. Aldosterone in the development and progression of renal injury. Kidney Int. 66(1), 1–9 (2004).
Epstein, M. Aldosterone as a mediator of progressive renal disease: Pathogenetic and clinical implications. Am. J. Kidney Dis. 37(4), 677–688 (2001).
Shavit, L., Lifschitz, M. D. & Epstein, M. Aldosterone blockade and the mineralocorticoid receptor in the management of chronic kidney disease: Current concepts and emerging treatment paradigms. Kidney Int. 81(10), 955–968 (2012).
Buffolo, F., Tetti, M., Mulatero, P. & Monticone, S. Aldosterone as a mediator of cardiovascular damage. Hypertension. 79(9), 1899–1911 (2022).
Calhoun, D. A. Aldosterone and cardiovascular disease: Smoke and fire. Circulation. 114(24), 2572–2574 (2006).
Funding
This study was funded by the Major Science and Technology Projects of Xinjiang Uygur Autonomous Region (2022A03012-5).
Author information
Authors and Affiliations
Contributions
S.S. and X.C. did a complete data analysis and wrote the manuscript. J.H., D.S., H.M., and Q.Z. helped perform the analysis with constructive discussions. W.Y., J.H., D.Z., and Q.L. contributed to the conception of the study. N.L. gave guidance to the whole research process.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cai, X., Song, S., Hu, J. et al. Association of the trajectory of plasma aldosterone concentration with the risk of cardiovascular disease in patients with hypertension: a cohort study. Sci Rep 14, 4906 (2024). https://doi.org/10.1038/s41598-024-54971-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-54971-4
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.