Abstract
Photon-counting detector (PCD)-CT allows for reconstruction of virtual non-iodine (VNI) images from contrast-enhanced datasets. This study assesses the diagnostic performance of aortic valve calcification scoring (AVCS) derived from VNI datasets generated with a 1st generation clinical dual-source PCD-CT. AVCS was evaluated in 123 patients (statistical analysis only comprising patients with aortic valve calcifications [n = 56; 63.2 ± 11.6 years]), who underwent contrast enhanced electrocardiogram-gated (either prospective or retrospective or both) cardiac CT on a clinical PCD system. Patient data was reconstructed at 70 keV employing a VNI reconstruction algorithm. True non-contrast (TNC) scans at 70 keV without quantum iterative reconstruction served as reference in all individuals. Subgroup analysis was performed in 17 patients who received both, prospectively and retrospectively gated contrast enhanced scans (n = 8 with aortic valve calcifications). VNI images with prospective/retrospective gating had an overall sensitivity of 69.2%/56.0%, specificity of 100%/100%, accuracy of 85.4%/81.0%, positive predictive value of 100%/100%, and a negative predictive value of 78.2%/75.0%. VNI images with retrospective gating achieved similar results. For both gating approaches, AVCSVNI showed high correlation (r = 0.983, P < 0.001 for prospective; r = 0.986, P < 0.001 for retrospective) with AVCSTNC. Subgroup analyses demonstrated excellent intra-individual correlation between different acquisition modes (r = 0.986, P < 0.001). Thus, VNI images derived from cardiac PCD-CT allow for excellent diagnostic performance in the assessment of AVCS, suggesting potential for the omission of true non-contrast scans in the clinical workup of patients with aortic calcifications.
Similar content being viewed by others
Introduction
Since the introduction of transcatheter aortic valve implantation (TAVI) in 2002, there has been tremendous advancement concerning not only the procedure itself, but also the associated imaging for treatment planning and device selection1. Today, computed tomography angiography (CTA) represents the established reference standard for evaluation of the access route, annular sizing, and risk determination for periprocedural annular injury2,3.
To date, additional non-contrast CT for aortic valve calcium quantification is not considered an essential portion of clinical routine imaging, but may have utility in a number of special settings and clinical scenarios4. Since aortic stenosis (AS) severity is known to correlate well with the aortic valve calcium load, CT-based calcium scoring can be problem solving when Doppler echo-cardiographic assessment of AS severity is hampered5,6. For instance, individuals with low-flow/low-gradient AS due to left ventricular dysfunction with limited left ventricular ejection fraction constitute one patient group benefiting from this scoring approach. Several studies have tried to find gender-specific aortic valve calcium score cut-off values that indicate the presence of high-grade AS5,6,7,8. In this context, an aortic valve calcification score (AVCS) ≥ 1300 in women or ≥ 2000 in men can be considered severe4. Moreover, aortic valve calcifications, when protruding into the lumen, are associated with increased risk of post-interventional complications, including para-valvular leakage, prosthesis dislodgement, obstruction of coronary ostia, calcific embolism/stroke and annular rupture, the latter being associated with particularly high mortality9,10,11,12. Nonetheless, both the SCCT (Society of Cardiovascular Computed Tomography) and ESCR (European Society of Cardiovascular Radiology) deem non-contrast CT with quantification of AVCS only necessary in selected patients prior to TAVI2,3. While this recommendation may be associated with increased examination complexity and a concomitant increase of radiation dose, it must be stated that the latter is modest and should not raise major concerns regarding the eligible population for TAVI.
Recently introduced photon-counting detectors (PCD) offer a wide spectrum of promising advantages in cardiovascular CT imaging when compared to conventional energy-integrating detector (EID)-based scanners13,14,15,16. PCD technology allows for energy discrimination at high temporal and spatial resolution by individually counting every incoming photon, and weighting it with regard to its transported energy17,18. Similar to dual-energy computed tomography approaches like dual-source, dual-layer or rapid kVp switching technology19, this offers possibilities for multi-material differentiation with the opportunity to create virtual non-iodine (VNI) images from CTA datasets20,21. In the context of pre-TAVI CT evaluation, this means that a true non-contrast (TNC) scan, which is normally required for aortic valve calcium scoring, can potentially be omitted, possibly diminishing both the cumulative radiation dose and examination time. Whereas VNI was predominantly proposed in the context of “classic” coronary artery calcium scoring in terms of a cardiovascular risk-stratification thus far22,23, a recent study by Mergen et al. demonstrated the potential of this technique for valvular calcium quantification from late iodine enhancement cardiac scans24.
Thus, the purpose of our study was to assess the diagnostic performance of first generation dual-source PCD-CT VNI imaging for quantification of aortic valve calcification, mass, and volume score from coronary CT angiographic (cCTA) images.
Materials and methods
Patient population and study design
The institutional review board of the University of Würzburg (Germany) approved the design of this retrospective single-center study and waived the need for additional written informed consent. The research was carried out in accordance with local legislation and the Declaration of Helsinki. From a total of 150 patients who underwent CT as part of routine diagnostic workup in suspected coronary artery disease (CAD) between November 2022 and June 2023, 123 patients (56 male, 67 female; mean age 63.2 ± 11.6 years) were included for final analysis. All patients received a TNC scan, which served as the reference standard for AVCS. Depending on the heart rate and rhythm, electrocardiogram-gated cCTA was either performed in a prospective (in form of an ultra-fast gated high-pitch “flash” scan; ≤ 62 bpm, rhythmic) or in a retrospective (≥ 63 bpm and/or arrhythmic) manner. In 17 patients of the prospective group, cCTA needed to be repeated as a retrospective acquisition, resulting in a subgroup featuring both, prospective and retrospective VNI datasets. Detailed information concerning the study design is presented in Fig. 1.
Flowchart shows selection of study population. Twenty-seven patients were excluded because of lacking a true non-contrast/virtual non-iodine scan or due to distinct artifacts. A total of 140 scans in 123 patients were available for final evaluation. CAD—Coronary artery disease, cCTA—coronary CT angiography, TNC—true non-contrast, VNI—virtual non-iodine.
CT scan acquisitions
All scans were acquired using a clinical 1st generation dual-source PCD-CT (Naeotom Alpha, Siemens Healthineers, Forchheim, Germany) equipped with two cadmium-telluride based photon-counting detectors (QuantaMax, Siemens Healthineers) and running the software version VA40. A collimation of 144 × 0.4 mm was employed for all examinations. First, unenhanced TNC data was acquired with a tube voltage of Sn 100 kVp (0.4 mm tin filter) and tube-current time product defined by an image quality index of 19. Of note, Apfaltrer et al. showed excellent agreement in calcium scoring protocols between 120 kVp and Sn 100 kVp despite significant radiation dose reduction25. Second, cCTA data was acquired with a tube voltage of 120 kVp in QuantumPlus mode and an IQ level of 64. Gantry rotation time was 0.25 s each. Automated tube-current modulation (CARE Dose4D, Siemens Healthineers) and tube-potential control (Care keV, Siemens Healthineers) were applied in all cCTA examinations. The same amount of contrast medium was administered in prospective and retrospective cCTA protocols. Detailed acquisition, radiation dose and contrast protocol parameters are provided in Table 1.
Calcium scoring image reconstruction
The cCTA datasets were postprocessed by applying a VNI algorithm (PureCalcium, Siemens Healthineers) as previously described20. According to recent literature as well as the vendors recommendation, monoenergetic TNC reconstructions at 70 keV without quantum iterative reconstruction (QIR) served as the reference standard22,23,26. All images for calcium scoring were reconstructed with identical parameters (recommended by the vendor; factory protocol), which are summarized in Table 1.
Image analysis
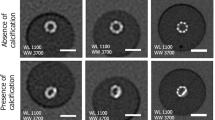
Two radiologists (with 1 and 13 years of experience in cardiovascular imaging, respectively) evaluated all calcium-scoring CT datasets side by side in a random order for AVCS, using a commercially available software (syngo.via VB60, Siemens Healthineers). According to current consensus documents, only valvular calcifications were segmented, ensuring the exclusion of coronary, left ventricular outflow tract, and aortic wall calcifications2,4. Figure 2 shows an example of how aortic valve calcium segmentation was performed. For every dataset, the Agatston score, aortic valve calcification mass and volume were evaluated.
Statistical analysis
Shapiro–Wilk tests were conducted to assess the normal distribution of metrically-scaled variables. If normally distributed, items are presented as mean ± standard deviation, otherwise as median with interquartile range. Classification functions of diagnostic accuracy were calculated separately for VNI images derived from prospective “flash” and retrospective spiral acquisitions. Pearson's correlation coefficient was computed to assess the relationship between measurements in true non-contrast and virtual non-iodine datasets. P values ≤ 0.05 were considered to indicate the significance of test results. Analyses were performed employing dedicated statistical software (SPSS 28, IBM, Armonk, USA).
Results
Aortic valve calcium scoring
In 67 patients, no aortic valve calcifications were ascertained (AVCSTNC of 0). In the remaining 56 patients, which were enrolled for statistical calculations, the median AVCSTNC, massTNC, and volume scores were 119 (54–603), 20 mg (9–121 mg), and 111 mm3 (52–495 mm3), respectively. Six male individuals displayed an AVCSTNC > 2000, while no female individuals exceeded an AVCSTNC > 1300.
For both cCTA based approaches, AVCSVNI showed high correlation with AVCSTNC (r = 0.983, P < 0.001 for prospective; r = 0.986, P < 0.001 for retrospective). Similarly, massVNI and volumeVNI score each showed high correlation with massTNC and volumeTNC (mass: r = 0.997, P < 0.001 for prospective; r = 0.988, P < 0.001 for retrospective/volume: r = 0.982, P < 0.001 for prospective; r = 0.982, P < 0.001 for retrospective).
Prospective cCTA-based VNI images had sensitivity of 69.2% (95% confidence interval: 52.4%, 83.0%), specificity of 100% (91.8%, 100%), accuracy of 85.4% (75.8%, 92.2%), positive predictive value of 100% (87.2%, 100%), and a negative predictive value of 78.2% (69.1%, 85.1%) for the assessment of aortic valve calcifications (Fig. 3). Retrospective cCTA-based VNI images showed nearly identical results, demonstrating an overall sensitivity of 56.0% (34.9%, 75.6%), specificity of 100% (89.4%, 100%), accuracy of 81.0% (68.6%, 90.1%), positive predictive value of 100% (76.8%, 100%), and a negative predictive value of 75.0% (65.8%, 82.4%), for assessment of aortic valve calcifications (Fig. 3).
With regard to the established AVCS cut-off values (Agatston score > 1300 for women and > 2000 for men suggesting the presence of severe AS), in only one out of 56 patients with aortic valve calcifications, stenosis estimation changed due to incorrectly low AVCS in retrospective VNI images (AVCSTNC 2227 vs. AVCSVNI 1808). However, in a total of 15 patients, all of which presented with very low AVCSTNC < 60 [median 51; range 4–60], AVCSVNI scores were false negative (Fig. 4).
Subgroup analysis
In the subgroup of 17 patients who received both cCTA acquisition protocols, 9 individuals did not exhibit any aortic valve calcifications in either TNC or VNI images (AVCS of 0). In the remaining 8 patients, which were enrolled for statistical calculations, the median AVCSTNC, massTNC, and volumeTNC scores were 112 (46–160), 18 mg (7–27 mg), and 107 mm3 (46–138 mm3), respectively.
In the intra-individual comparison, both cCTA based approaches showed high correlation of AVCS (r = 0.986, P < 0.001), mass (r = 0.992, P < 0.001), and volume (r = 0.987, P < 0.001) scores.
Discussion
This retrospective study on 123 patients demonstrated that virtual non-iodine postprocessing of spectral dual-source photon-counting detector CT data is a reliable technique for aortic valve calcification scoring. Iodine from contrast-enhanced scans can be digitally subtracted, allowing for aortic valve calcifications to be assessed and analyzed quantitatively without the necessity of acquiring a true non-contrast scan. For both prospective and retrospective gating-approaches, quantitative analyses of virtual non-iodine data provide high diagnostic accuracy and excellent correlation to true non-contrast imaging.
Previous studies have demonstrated the capability of PCD-CT to perform accurate coronary calcium scoring at various tube voltages, simultaneously offering potential for substantial radiation dose reduction when compared to conventional EID-CT26,27,28,29. Moreover, due to its intrinsic spectral resolution, PCD-CT offers the possibility to calculate virtual iodine-free images and thus render a separate scan for calcium scoring obsolete. Several investigations have evaluated the potential of PCD-CT derived VNI reconstructions for coronary artery calcium assessment and also for mitral annular and aortic valve calcification scoring20,22,23,24. Emrich et al. found, that the vendor-specific non-iodine algorithm named PureCalcium (used in the present study) outperforms standard virtual non-contrast reconstructions from spectral data20.
A comparatively low IQ level of 19 was applied for the TNC scan constituting the reference standard for AVCS analysis (compared to an IQ index of 64 in cCTA acquisitions), as higher IQ levels did not improve scoring accuracy in previous studies29. All reconstructions were computed at 70 keV. This keV level has been reported to show the least deviation of calcium scores derived from standard EID-CT and has therefore been established as diagnostic standard in PCD-CT-based calcium scoring28,29.
With one exception24, VNI technique was yet typically evaluated in the context of “classic” coronary artery calcium scoring as proposed by the 2019 American College of Cardiology/American Heart Association Guideline on Primary Prevention of Cardiovascular Disease30. Recently Mergen et al. showed that VNI created from cardiac late iodine enhancements scans offer accurate quantification, not only of coronary calcifications, but also of mitral annular and aortic valve calcifications24. However, there were some differences to our study setting. In addition to different software versions being used (VA40 vs. VA 50), we analyzed cCTA scans instead of late enhancement cardiac scans as “source data” for VNI generation. The lower attenuation of the blood pool on late iodine enhancement images might contribute to a more precise material decomposition, however, from a practical point of view, cCTA is more common in clinical routine, especially in the context of pre-TAVI evaluation were AVCS usually becomes relevant. It is worth mentioning that, in the study by Mergen et al., VNI reconstructions at 80 keV provided the best accuracy in AVCS, while reconstructions at other keV levels (e.g., 70 keV as used in our cohort) resulted in a significant underestimation of calcification score.
By allowing AVCS based on contrast-enhanced CT scans, concerns about prolonged examination protocols and higher radiation dose associated with additional TNC scans can be overcome. According to the ALARA—as low as reasonable achievable—principle, the positive side effect of dose saving is generally welcome, although one should not overestimate the relevance of radiation exposure in the aging population for which AV calcium quantification is usually considered, namely patients selected for TAVI procedures2,3. More important is the fact that up to 40% of patients show a discordant assessment of AS severity with echocardiography as the current reference standard test. Suchlike inaccuracies are commonly observed in patients with a severely decreased aortic valve area (≤ 1 cm2) but flow parameters only suggesting moderate disease (mean gradient < 40 mm Hg; peak flow < 4 m/s)31. The crucial advantage of performing AVCS assessment in this scenario is its independence of the hemodynamic situation. In summary, we do believe that VNI reconstructions could further strengthen the clinical acceptance of AVCS as a marker of stenosis severity, progression of valvular disease, and powerful predictor of adverse events4.
In our patient sample, we observed a relatively high number of false negative analyses (n = 15), resulting in a comparatively low negative predictive value. This observation is in line with findings from previous investigations, and most likely due to a combination of limited detectability of low-density calcifications, the reconstruction algorithm, and partial volume effects20,32. In this context, it should be emphasized that all individuals with false negative assessment in VNI datasets presented with a very low AVCSTNC < 60. Due to the fact that only Agatston scores markedly > 1000 are considered relevant for classification of severe AS4, the clinical impact of this finding is presumably rather low. However, in individual cases, this inaccuracy could possibly lead to incorrect grading of AS. On the other hand, a high positive predictive value of both prospective and retrospective cCTA-based synthetic non-contrast images (both 100%), emphasizes the potential role of VNI images as a diagnostic tool for validation of echo-based diagnosis of severe AS or as a superior alternative in challenging clinical scenarios, like low-flow/low-gradient AS with limited left ventricular ejection fraction.
Limitations
This study has several limitations that need to be addressed. First, due to dose saving reasons, our clinical CAD protocol features a tin-filtered 100 kVp scan for TNC calcium scoring instead of a 120 kVp filtered back-projection protocol, generally considered as standard of reference when calcium quantification is demanded. However, it has recently been shown that 70 keV reconstructions derived from Sn 100 kVp acquisitions allow for accurate calcium score calculation when compared to 120 kVp EID-CT scans28. Second, in the present CAD collective, only few patients presented with very high aortic valve calcium loads (only 6 male patients exceeded an AVCS > 2000). Third, according to the vendor, newer software versions (syngo.via VA50) provide improved spectral image quality and material decomposition compared to the software version we used in the present study. Additional analyses in a TAVI-specific cohort with expectably higher AVCS in the majority of patients should be performed in future studies. Third, the impact of aortic valve sclerosis characteristics, such as plaque size and density on AVCSVNI, massVNI, and volumeVNI were not evaluated.
Conclusion
VNI images derived from PCD-cCTA showed excellent diagnostic performance for assessing AVCS. Displaying potential for TAVI-associated risk assessment, aortic valve stenosis grading, as well as radiation dose reduction in clinical routine, VNI-based AVCS analysis may render a separate TNC scan unnecessary in the future.
Data availability
The datasets generated and/or analyzed during this study are not publicly available as CT data and DICOM headers contain patient information. Data can be obtained on reasonable request from the corresponding author.
References
Cribier, A. et al. Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis: First human case description. Circulation 106, 3006–3008 (2002).
Blanke, P. et al. Computed tomography imaging in the context of transcatheter aortic valve implantation (TAVI)/transcatheter aortic valve replacement (TAVR): An expert consensus document of the society of cardiovascular computed tomography. JACC Cardiovasc. Imaging 12, 1–24 (2019).
Francone, M. et al. CT and MR imaging prior to transcatheter aortic valve implantation: Standardisation of scanning protocols, measurements and reporting-a consensus document by the European Society of Cardiovascular Radiology (ESCR). Eur. Radiol. 30, 2627–2650 (2020).
Pawade, T., Sheth, T., Guzzetti, E., Dweck, M. R. & Clavel, M.-A. Why and how to measure aortic valve calcification in patients with aortic stenosis. JACC Cardiovasc. Imaging 12, 1835–1848 (2019).
Clavel, M.-A. et al. The complex nature of discordant severe calcified aortic valve disease grading: New insights from combined Doppler echocardiographic and computed tomographic study. J. Am. Coll. Cardiol. 62, 2329–2338 (2013).
Clavel, M.-A. et al. Impact of aortic valve calcification, as measured by MDCT, on survival in patients with aortic stenosis: Results of an international registry study. J. Am. Coll. Cardiol. 64, 1202–1213 (2014).
Baumgartner, H. et al. Recommendations on the echocardiographic assessment of aortic valve stenosis: A focused update from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. Eur. Hear. journal. Cardiovasc. Imaging 18, 254–275 (2017).
Aggarwal, S. R. et al. Sex differences in aortic valve calcification measured by multidetector computed tomography in aortic stenosis. Circ. Cardiovasc. Imaging 6, 40–47 (2013).
Barbanti, M. et al. Anatomical and procedural features associated with aortic root rupture during balloon-expandable transcatheter aortic valve replacement. Circulation 128, 244–253 (2013).
Barbanti, M. et al. Transcatheter aortic valve replacement with new-generation devices: A systematic review and meta-analysis. Int. J. Cardiol. 245, 83–89 (2017).
Haensig, M. & Rastan, A. J. Aortic valve calcium load before TAVI: Is it important?. Ann. Cardiothorac. Surg. 1, 160–164 (2012).
Fassa, A.-A., Himbert, D. & Vahanian, A. Mechanisms and management of TAVR-related complications. Nat. Rev. Cardiol. 10, 685–695 (2013).
Rajendran, K. et al. First clinical photon-counting detector CT system: Technical evaluation. Radiology 303, 130–138 (2022).
Gruschwitz, P. et al. Photon-counting versus energy-integrating detector CT angiography of the lower extremity in a human cadaveric model with continuous extracorporeal perfusion. Invest. Radiol. 58, 740–745 (2023).
Pannenbecker, P. et al. Photon-counting CT for diagnosis of acute pulmonary embolism: Potential for contrast medium and radiation dose reduction. Eur. Radiol. 33, 7830–7839 (2023).
van der Bie, J. et al. Photon-counting detector CT in patients pre- and post-transcatheter aortic valve replacement. Radiol. Cardiothorac. imaging 5, e220318 (2023).
Willemink, M. J., Persson, M., Pourmorteza, A., Pelc, N. J. & Fleischmann, D. Photon-counting CT: Technical principles and clinical prospects. Radiology 289, 293–312 (2018).
Kreisler, B. Photon counting detectors: Concept, technical challenges, and clinical outlook. Eur. J. Radiol. 149, 110229 (2022).
Siegel, M. J. et al. White paper of the society of computed body tomography and magnetic resonance on dual-energy CT, part 1. J. Comput. Assist. Tomogr. 40, 841–845 (2016).
Emrich, T. et al. Coronary computed tomography angiography-based calcium scoring: In vitro and in vivo validation of a novel virtual noniodine reconstruction algorithm on a clinical, first-generation dual-source photon counting-detector system. Invest. Radiol. 57, 536–543 (2022).
Sharma, S. P. et al. Coronary calcium scoring on virtual non-contrast and virtual non-iodine reconstructions compared to true non-contrast images using photon-counting computed tomography. Eur. Radiol. https://doi.org/10.1007/s00330-023-10402-y (2023).
Fink, N. et al. Photon counting detector CT-based virtual noniodine reconstruction algorithm for in vitro and in vivo coronary artery calcium scoring: Impact of virtual monoenergetic and quantum Iterative reconstructions. Invest. Radiol. 58, 673–680 (2023).
Fink, N. et al. Radiation dose reduction for coronary artery calcium scoring using a virtual noniodine algorithm on photon-counting detector computed-tomography phantom data. Diagnostics (Basel, Switzerland) 13, 1540 (2023).
Mergen, V. et al. Cardiac virtual noncontrast images for calcium quantification with photon-counting detector CT. Radiol. Cardiothorac. imaging 5, e220307 (2023).
Apfaltrer, G. et al. High-pitch low-voltage CT coronary artery calcium scoring with tin filtration: Accuracy and radiation dose reduction. Eur. Radiol. 28, 3097–3104 (2018).
van der Werf, N. R. et al. Dose reduction in coronary artery calcium scoring using mono-energetic images from reduced tube voltage dual-source photon-counting CT data: A dynamic phantom study. Diagnostics (Basel, Switzerland) 11, 2192 (2021).
Symons, R., Sandfort, V., Mallek, M., Ulzheimer, S. & Pourmorteza, A. Coronary artery calcium scoring with photon-counting CT: First in vivo human experience. Int. J. Cardiovasc. Imaging 35, 733–739 (2019).
Mergen, V. et al. Tube voltage-independent coronary calcium scoring on a first-generation dual-source photon-counting CT-a proof-of-principle phantom study. Int. J. Cardiovasc. Imaging https://doi.org/10.1007/s10554-021-02466-y (2021).
Eberhard, M. et al. Coronary calcium scoring with first generation dual-source photon-counting CT-first evidence from phantom and in-vivo scans. Diagnostics (Basel, Switzerland) 11, 1708 (2021).
Arnett, D. K. et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 140, 596–646 (2019).
Clavel, M.-A., Burwash, I. G. & Pibarot, P. Cardiac imaging for assessing low-gradient severe aortic stenosis. JACC Cardiovasc. Imaging 10, 185–202 (2017).
van Praagh, G. D. et al. Coronary artery calcium scoring: Toward a new standard. Invest. Radiol. 57, 13–22 (2022).
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
B.P. and P.F. designed the study concept. H.H. was responsible for data acquisitions. B.P., P.F., M.S. and J.P.G. were responsible for data analyses and interpretation as well as drafting of the manuscript. N.C., P.P., T.A.B, H.H. and J.F.H. were involved in data interpretation and drafting of the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Feldle, P., Scheuber, M., Grunz, JP. et al. Virtual non-iodine photon-counting CT-angiography for aortic valve calcification scoring. Sci Rep 14, 4724 (2024). https://doi.org/10.1038/s41598-024-54918-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-54918-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.