Abstract
An inverse association between cancer and Alzheimer’s disease (AD) has been demonstrated; however, the association between cancer and mild cognitive impairment (MCI), and the association between cancer and cognitive decline are yet to be clarified. The AIBL dataset was used to address these knowledge gaps. The crude and adjusted odds ratios for MCI/AD and cognitive decline were compared between participants with/without cancer (referred to as C+ and C− participants). A 37% reduction in odds for AD was observed in C+ participants compared to C− participants after adjusting for all confounders. The overall risk for MCI and AD in C+ participants was reduced by 27% and 31%, respectively. The odds of cognitive decline from MCI to AD was reduced by 59% in C+ participants after adjusting for all confounders. The risk of cognitive decline from MCI to AD was halved in C+ participants. The estimated mean change in Clinical Dementia Rating-Sum of boxes (CDR-SOB) score per year was 0.23 units/year higher in C− participants than in C+ participants. Overall, an inverse association between cancer and MCI/AD was observed in AIBL, which is in line with previous reports. Importantly, an inverse association between cancer and cognitive decline has also been identified.
Similar content being viewed by others
Introduction
The presence of multiple chronic health conditions (referred to as comorbidities), such as cardiovascular disease, cancer, Alzheimer’s disease (AD), and diabetes, becomes more common as people age1. While the association between comorbidities and AD has been well studied, that between cancer and AD has not yet been comprehensively investigated. Most epidemiological studies have focused on cancer risk after the diagnosis of AD (exposure = AD, outcome = cancer) or AD risk in patients with cancer (exposure = cancer, outcome = AD). A reduction in cancer incidence rate was observed in individuals with AD, with the risk ratio (RR) ranging from 0.29 to 0.902,3,4,5,6,7,8,9,10,11, and reduced incidence rate of AD was noted in people with cancer2,3,6,10,11,12,13,14,15,16,17,18,19. Although contradictory results are sometimes observed14, most studies suggest that cancer reduces the incidence rate of AD and vice versa.
There are knowledge gaps that remain to be filled to clarify the association between cancer and AD. First, mild cognitive impairment (MCI), an important transitional phase prior to the development of AD is usually neglected2,10,11 in epidemiological studies, and the association between cancer and MCI is still inconclusive20. Second, the association between cancer and cognitive decline in AD is unclear. Unravelling this epidemiological association will lend support to further studies exploring the underlying mechanisms contributing to the interaction between cancer and MCI/AD, which has the potential to impact on the development of novel strategies to intervene cognitive decline in AD. Last but not least, although the association between cancer and AD has been explored in European6,13,16,17,18 and American studies2,3,10,11,12,14,15,19, and the influence of geographic and demographic factors on this association was noted, an Australian study is lacking.
To address these knowledge gaps, we leveraged longitudinal data from the Australian Imaging Biomarkers and Lifestyle (AIBL) study21,22 and examined the risk for MCI/AD in participants with cancer and the risk for cognitive decline (i.e. cognitive unimpaired [CU] to MCI, CU to AD, and MCI to AD) due to cancer. Confounding factors were adjusted for or stratified. In addition, change in Clinical Dementia Rating Scale Sum of Boxes scores over time (ΔCDR-SOB, a surrogate for cognitive decline) was calculated and compared between participants with and without cancer.
Material and methods
Participants
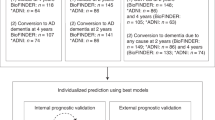
The AIBL study was approved by the institutional ethics committees at St. Vincent’s Health and the University of Melbourne, and all participants have provided written informed consent prior to study enrolment. All methods were performed in accordance with the Australian code for the responsible conduct of research. To date, 2854 participants have been recruited to AIBL. Longitudinal data was collected over an average 7.2-year period, with an overall participation rate of 84.9%. The selection process for participants in the current study is summarized in Fig. 1. Of the total 2854 AIBL participants, 718 participants were excluded from the study due to unknown cancer and/or cognitive status at enrolment. Of the included participants (n = 2136), 55.6% were female (n = 1187) and 44.4% were male (n = 949). The participants were categorized as CU, MCI, AD, and PRO (those who experienced progression in cognition category during the follow-up period). Cognitive assessment is detailed in the Clinical Diagnosis section below.
Study participants. The AIBL dataset included 2854 participants, of which 718 individuals were removed due to unknown cancer or cognitive status. 2136 participants remained for data analysis in the present study, with 1297 CU, 217 MCI and 369 AD participants. In addition, 253 participants exhibited changes in cognition category (i.e. cognitive decline) during follow-up period. Of these, 117 progressed from CU to MCI, 41 progressed from CU to AD, and 95 from MCI to AD. *CDR-SOB score was available for 1279 participants; APOE genotype was recorded for 1958 participants; smoking status, alcohol consumption, and years of education were known for 1934, 1830 and 2117 participants, respectively. CU cognitive unimpaired, MCI mild cognitive impairment, AD Alzheimer’s disease, PRO progression in cognition category during the follow-up period.
History of cancer (exposure)
History of cancer was self-reported at enrolment and the occurrence of cancer was self-reported during the follow-up period. Cancer status of the participants was categorized as (1) self-report of cancer at enrollment or during follow-up (C+); (2) no self-report of cancer at enrolment or during follow-up (C−). For participants with change in cognition category, only those who were diagnosed with cancer before cognition category change were included in the analysis.
Clinical diagnosis of MCI and AD (outcome)
The criteria used for clinical diagnosis of MCI and AD has been described in previous studies21,22. Cognitive status of the participants was determined by neurologists and neuropsychologists using amyloid PET imaging and neuropsychology tests. Participants who were identified as CU or MCI at enrolment but experienced cognition category change over the follow-up period (i.e. CU to MCI, CU to AD, and MCI to AD) were assigned to the PRO group. Participants who were identified as CU, MCI, or AD at enrolment and throughout the study were categorized into the CU, MCI, and AD groups.
Potential confounders
Sex, APOEε4 (carrier or noncarrier), smoking (never, former, current), alcohol (non/light/moderate/heavy drinker), and education were determined from self-report and medical records. In addition, a blood sample was taken for APOE genetic testing for participants who gave consent. Light, moderate, and heavy alcohol consumption was defined as < 3 days per week, 3 to 6 days per week, and daily consumption, respectively. Descriptive statistics for the potential confounders are provided in Supplementary Data Table S1.
Statistical analysis
Data analysis was performed using Stata statistical software (version 17.0; College Station, TX), where univariable/multivariable logistic regression and univariable linear regression programs were used. This study assessed (1) the odds ratio/risk ratio (OR/RR) for MCI and AD in C+ participants compared with C− participants; (2) the OR/RR of cancer exposure (C+) on cognitive decline (change of cognition category); (3) the impact of potential confounders on the associations measured in (1) and (2). In addition, the change in CDR-SOB score over time (ΔCDR-SOB) was compared between C+ and C− participants. As the time between the first and last measurement of the CDR-SOB score varied for each participant, the ΔCDR-SOB was normalized by time. All statistical tests performed were two-sided. Statistical significance and 95% confidence interval (CI) were determined, with statistical significance defined as p-value < 0.05. Figures were prepared by GraphPad Prism Software (Version 9.1.0) (Boston, MA).
Results
Characteristics of the study population
A total of 2136 participants were included in the present study, including 1297 (60.7%) CU, 217 (10.2%) MCI, 369 (17.3%) AD and 253 (11.8%) PRO (Table 1). Within the PRO group, 117 (46.3%) participants progressed from CU to MCI, 41 (16.2%) participants progressed from CU to AD, and 95 (37.5%) participants progressed from MCI to AD. Of the 2136 participants, 1590 (74.4%) had never diagnosed with cancer (C−), and 546 (25.6%) had a history of cancer (C+) at the time of enrollment (Table 1). Of the 1590 C− participants, 930 (58.5%), 170 (10.7%), 296 (18.6%), 194 (12.2%) belonged to the CU, MCI, AD, and PRO groups, respectively (Fig. 2A). Of the 546 C + participants, 367 (67.2%), 47 (8.6%), 73 (13.4%) and 59 (10.8%) belonged to the CU, MCI, AD, and PRO groups, respectively (Fig. 2B). The averaged age and distribution of sex for participants under each cognition group is also provided in Table 1.
The proportions of each cognition category for AIBL participants with and without cancer (C+ and C−). (A) Of the 1590 C− participants, 58.5%, 10.7%, 18.6% and 12.2% were categorized as CU, MCI, AD and PRO, respectively. (B) Of the 546 C+ participants, 67.2%, 8.6%, 13.4%, and 10.8% were categorized as CU, MCI, AD and PRO, respectively. CU cognitive unimpaired, MCI mild cognitive impairment, AD Alzheimer’s disease, PRO progression in cognition category during the follow-up period.
The association (OR) between cancer and AD is significant but not for cancer and MCI
To measure the association between cancer and MCI/AD, the crude and adjusted ORs were calculated (Table 2). Of the 217 MCI participants, 47 (21.7%) had cancer. A crude logistic regression model revealed a 0.70-fold relative decrease (OR 0.70 [0.50–0.99], p = 0.043) in the odds of MCI in C+ participants when compared to C− participants. The association between cancer and MCI remained to be statistically significant after individual adjustment for sex (0.67 [0.48–0.95], p = 0.025), APOE ε4 (0.65 [0.43–0.99], p = 0.046), and smoking (0.68 [0.48–0.98], p = 0.019). However, the association became statistically nonsignificant after adjusting for all confounders (0.62 [0.38–1.01], p = 0.056) (Table 2, + All, column 1). In summary, there was no significant inverse association between cancer and MCI after all confounders were adjusted for. Of the 369 AD participants, 73 (19.7%) had cancer. Crude regression model revealed that cancer was associated with approximately 40% lower odds of AD (0.62 [0.47–0.83], p = 0.001). Similar observations were also noted in individual confounder-adjusted regression models (Table 2, + Sex, + APOE ε4, + Smoking, + Alcohol, + Education, column 2). The odds of AD were significantly reduced by 0.63-fold (0.63 [0.43–0.92], p = 0.017) in C + participants compared to C- participants after adjusting for all confounders (Table 2, + All, column 2). In conclusion, an inverse association between cancer and AD was observed and remained significant even after adjusting for all confounders in this study.
The association (RR) between cancer and MCI/AD is moderated by sex and APOE ε4 allele type
The crude risk of MCI (RR 0.73 [0.54–0.99], p = 0.042) and AD (RR 0.69 [0.54–0.87], p = 0.001) was significantly reduced in C+ participants when compared to C− participants (Table 3). Stratum-specific RR for confounders (sex and APOE ε4-allele type) was calculated. The risk reduction for the occurrence of MCI (0.63 [0.42–0.96], p = 0.025) or AD (0.69 [0.50–0.95], p = 0.018) remained statistically significant in male C+ participants compared to male C− participants. However, only the risk reduction of AD (RR 0.66 [0.47–0.93], p = 0.015), but not that of MCI, in female C + participants compared to female C- participants was statistically significant (Table 3, + Sex, columns 1 & 2). When examining the stratum-specific RR for the APOE ε4 allele type, only the risk reduction for the occurrence of AD (0.74 [0.55–0.99], p = 0.036), but not that for MCI, reached statistical significance for C + participants carrying the APOE ε4 allele compared with C- participants (Table 3, + APOE ε4, column 2). When the data were stratified by both sex and APOE ε4 allele type, all RRs were not statistically significant, except for male APOE ε4 carriers (RR 0.40 [0.16–0.99], p = 0.031). Detailed statistics can be found in Supplementary Data Table S2. In conclusion, a significant inverse association was observed between cancer and MCI/AD. However, the stratum-specific RR showed that the association between cancer and MCI/AD contained differences for each stratum of the confounder. The stratum-specific RR was not calculated for smoking (three subgroups), alcohol (four subgroups), education (six subgroups), or their combinations, given the small sample size resulting from stratification.
The association (RR) between cancer and cognitive decline is moderated by different PRO categories
The association between cancer and cognitive decline was examined in the PRO group (Table 4, column 1), and no significant association was observed from either crude or adjusted models. Different categories of PRO (i.e. CU to MCI, MCI to AD, and CU to AD) were therefore analyzed meticulously. Progression from CU to MCI occurred in 88 participants, of whom 29 (24.79%) were C+. Unadjusted and adjusted logistic regression models revealed a nonsignificant association between cancer and progression from CU to MCI (Table 4, column 2). A total of 41 participants experienced cognitive decline from CU to AD, of whom 15 (36.59%) were C+; however, no statistically significant association was observed (Table 4, column 3). The same analyses were performed for participants who progressed from MCI to AD (n = 95), of whom 15 (15.79%) were C+. The crude logistic regression model showed a 0.48-fold relative decrease (OR 0.48 [0.27–0.84], p = 0.010) in the progression from MCI to AD in C+ participants compared with C− participants. In adjusted logistic regression models, cancer was inversely associated with the progression from MCI to AD, after separate adjustment for each confounder (ORs 0.45–0.51). A similar association was also found when all confounders were accounted for (0.41 [0.21–0.82], p = 0.011), and all these odds ratios reached statistical significance (Table 4, column 4).
The association (RR) between cancer and progression from MCI to AD is significant, while that between cancer and progression from CU to MCI or CU to AD is nonsignificant
The risk reduction of cognitive decline in C+ compared to C− participants was not statistically significant (0.80 [0.61–1.05], p = 0.105) (Table 5, PRO). RRs in each cognitive decline category were therefore assessed. Only the association between cancer and progression from MCI to AD was significant but not for any other cognitive decline categories. A 0.5-fold reduction (0.50 [0.29–0.85], p = 0.008) in the risk of progression from MCI to AD was observed in C+ participants compared with C− participants (Table 5, MCI to AD). The stratum-specific RR was not calculated for sex (two subgroups), APOE ε4 allele type (two subgroups), smoking (three subgroups), alcohol (four subgroups), education (six subgroups), or their combinations due to small sample size resulting from subgrouping that were impractical for analysis.
The increase in CDR-SOB score over time is slower in participants with history of cancer than those without
The CDR-SOB is a global score regularly used in clinical and research settings to stage dementia severity23. Generally, more severe cognitive impairment was associated with a higher score. To understand the association between cancer and cognitive decline, the estimated mean change in CDR-SOB scores normalized by time (ΔCDR-SOB) was compared between C+ and C− participants (Fig. 3). The ΔCDR-SOB score was 0.34 and 0.57 units/year for C+ and C− participants, respectively (Table 6).
ΔCDR-SOB for AIBL participants with/without cancer. The ΔCDR-SOB was plotted for C− (without cancer, left boxplot) and C+ (with cancer, right boxplot) participants. The lowest ΔCDR-SOB for C− participants was −1 and the highest was 12. The lowest ΔCDR-SOB for C+ participants were −0.5 and the highest was 6. The mean ΔCDR-SOB for C− and C+ was 0.57 and 0.34 units/year, respectively.
Discussion
The present study examined the association between cancer and MCI/AD in AIBL participants. We noted that C+ participants were less likely to develop AD than C− participants, which is consistent with previous studies6,11,16,17,18,24,25. Our studies have also revealed a nonsignificant association between cancer and MCI. It must be emphasized that studying the association between cancer and MCI is challenging as MCI can be caused by different conditions, including AD, Lewy body dementia, Parkinson’s disease and even chemotherapy26,27,28,29. In future studies, MCI should be carefully characterized to eliminate disease heterogeneity from analysis; for example, the brain levels of amyloid-beta (Aβ) can be assessed, so that the association between cancer and Aβ-positive MCI can be precisely investigated.
The strength of our study is that we employed a large longitudinal dataset from AIBL to study the association between cancer and cognitive decline, which has not yet been comprehensively studied. The cognition category for the participants was clearly defined in our longitudinal study, so that we can ensure the temporal sequence between exposure (i.e. cancer) and the outcome (i.e. change in cognition category) to avoid reverse causality. All participants were included in the study for data analysis, except for those who had no record for cancer history or cognitive status, which reduced the risk of survival bias. The average age and gender distribution of the current study was comparable to a community-based cohort study conducted by University of Kentucky Alzheimer’s Disease Research Center (UK-ADRC)30. We showed that C+ participants were less likely to progress from MCI to AD compared with C− participants, while no significant association between cancer and cognitive decline from CU to MCI was observed. This observation has demonstrated the potential role of cancer on the progression of MCI to AD, but not on the development of MCI. The association between cancer and cognitive decline from CU to AD (n = 41) was found to be nonsignificant, which is not consistent with the association between cancer and change in ΔCDR-SOB score over time. Comparing the estimated mean change in ΔCDR-SOB score per year, it is noted that cognitive decline is slower in C+ participants than C− participants (n = 546 for C+, n = 1590 for C−). This discrepancy could be due to a much smaller sample size available for the former analysis approach.
In our study, there are several limitations that need to be considered, which may restrict the inference of a true association between exposure and outcome. History of cancer was self-reported by participants, and therefore recall bias is possible, especially in old participants. In addition, details of chemotherapy and types of cancer were not recorded. Therefore, an investigation of the association between cancer therapies or specific cancer types and subsequent development of MCI, AD, or PRO was not possible. A systematic review has revealed that various types of cancer can have distinct effects on the risk of subsequent cognitive decline. It suggests that the association between cancer and disease progression is not uniform across all cancer types24. Therefore, recording more details on cancer subtypes should be considered for future AIBL studies. In addition, the composition of our cohort was mainly Caucasians residing in Victoria (60%), and Western Australia (40%). This will limit the generalizability of our results to Australians residing in regions outside of our study area and Australians with diverse ethnic backgrounds. In addition, the AIBL study excludes participants who had cancer in the past 5 years from recruitment (excluding skin or in situ prostate cancer), which can potentially contribute to selection bias.
The inverse association between cancer and AD can possibly be explained by the underlying pathobiological processes. At molecular level, the TP53 gene encodes the p53 protein, which is a well-recognized tumor suppressor31,32. In most cancer cases, the p53 gene is mutated and loses its tumor suppressive effect33.The accumulation of Aβ and hyperphosphorylation of tau are the hallmarks of AD34. Aβ promotes p53-dependent neuronal apoptosis by activating the p53 promoter, which is believed to be responsible for neurological disorders, such as AD35,36. The hyperphosphorylation of tau is also p53-dependent37. Other oncogenic molecules may also be involved in the inverse relationship between cancer and AD. Transforming growth factor beta (TGF-β) overexpression upregulates the expression of amyloid precursor protein (APP) and contribute to Aβ accumulation, while producing anti-proliferative effect that may suppress cancer38,39. Tumor overexpress PD-L1 helps tumor survival by suppressing the immune system40,41. Interestingly, PD-L1 suppresses neuroinflammation and the associated AD pathology42. The mitochondria regulate cell survival or apoptosis via regulating the production of reactive oxygen species (ROS). Moderate ROS production promotes the cancer cells growth and proliferation, while high levels of ROS in AD promote neurodegeneration43. P-glycoprotein at the blood–brain barrier clears Aβ from the brain44, while P-glycoprotein plays an immunosurveillance role in cancer45. A hypothetical pathobiological interaction between cancer and AD is illustrated in Fig. 4.
In conclusion, we observed a negative association between cancer and MCI/AD in AIBL, which is consistent with previous studies. We also highlighted a lower incidence and prevalence of MCI/AD progression in participants with cancer. In addition, cancer is associated with cognitive decline (change of CDR-SOB score) at a slower rate. Further studies are required to investigate the pathobiology underlying the two diseases to explain their inverse association observed in epidemiological studies.
Data availability
The dataset generated during and/or analyzed during the current study are available from the corresponding author on reasonable request, and subject to the approval by AIBL scientific committee.
References
Fillenbaum, G. G., Pieper, C. F., Cohen, H. J., Cornoni-Huntley, J. C. & Guralnik, J. M. Comorbidity of five chronic health conditions in elderly community residents: Determinants and impact on mortality. J. Gerontol. A Biol. Sci. Med. Sci. 55, M84-89. https://doi.org/10.1093/gerona/55.2.m84 (2000).
Driver, J. A. et al. Inverse association between cancer and Alzheimer’s disease: Results from the Framingham heart study. BMJ 344, e1442. https://doi.org/10.1136/bmj.e1442 (2012).
Freedman, D. M. et al. Associations between cancer and Alzheimer’s disease in a U.S. Medicare population. Cancer Med. 5, 2965–2976. https://doi.org/10.1002/cam4.850 (2016).
Ganguli, M., Dodge, H. H., Shen, C., Pandav, R. S. & DeKosky, S. T. Alzheimer disease and mortality: A 15-year epidemiological study. Arch. Neurol. 62, 779–784. https://doi.org/10.1001/archneur.62.5.779 (2005).
Kokmen, E. et al. Clinical risk factors for Alzheimer’s disease: A population-based case–control study. Neurology 41, 1393–1397. https://doi.org/10.1212/wnl.41.9.1393 (1991).
Musicco, M. et al. Inverse occurrence of cancer and Alzheimer disease: A population-based incidence study. Neurology 81, 322–328. https://doi.org/10.1212/WNL.0b013e31829c5ec1 (2013).
Ou, S. M. et al. Does Alzheimer’s disease protect against cancers? A nationwide population-based study. Neuroepidemiology 40, 42–49. https://doi.org/10.1159/000341411 (2013).
Realmuto, S. et al. Tumor diagnosis preceding Alzheimer’s disease onset: Is there a link between cancer and Alzheimer’s disease?. J. Alzheimers Dis. 31, 177–182. https://doi.org/10.3233/JAD-2012-120184 (2012).
Ren, R. J. et al. Association between Alzheimer’s disease and risk of cancer: A retrospective cohort study in Shanghai, China. Alzheimers Dement. 18, 924–933. https://doi.org/10.1002/alz.12436 (2022).
Roe, C. M., Behrens, M. I., Xiong, C., Miller, J. P. & Morris, J. C. Alzheimer disease and cancer. Neurology 64, 895–898. https://doi.org/10.1212/01.WNL.0000152889.94785.51 (2005).
Roe, C. M. et al. Cancer linked to Alzheimer disease but not vascular dementia. Neurology 74, 106–112. https://doi.org/10.1212/WNL.0b013e3181c91873 (2010).
Bowles, E. J. A. et al. Risk of Alzheimer’s disease or dementia following a cancer diagnosis. PLoS One 12, e0179857. https://doi.org/10.1371/journal.pone.0179857 (2017).
Chamberlain, J. D. et al. Investigating the association between cancer and the risk of dementia: Results from the Memento cohort. Alzheimers Dement. 17, 1415–1421. https://doi.org/10.1002/alz.12308 (2021).
Frain, L. et al. Association of cancer and Alzheimer’s disease risk in a national cohort of veterans. Alzheimers Dement. 13, 1364–1370. https://doi.org/10.1016/j.jalz.2017.04.012 (2017).
Nudelman, K. N. et al. Association of cancer history with Alzheimer’s disease onset and structural brain changes. Front. Physiol. 5, 423. https://doi.org/10.3389/fphys.2014.00423 (2014).
Ording, A. G. et al. Cancer and risk of Alzheimer’s disease: Small association in a nationwide cohort study. Alzheimers Dement. 16, 953–964. https://doi.org/10.1002/alz.12090 (2020).
Prinelli, F. et al. Different exposures to risk factors do not explain the inverse relationship of occurrence between cancer and neurodegenerative diseases: An Italian nested case-control study. Alzheimer Dis. Assoc. Disord. 32, 76–82. https://doi.org/10.1097/WAD.0000000000000204 (2018).
Sun, M., Wang, Y., Sundquist, J., Sundquist, K. & Ji, J. The association between cancer and dementia: A national cohort study in Sweden. Front. Oncol. 10, 73. https://doi.org/10.3389/fonc.2020.00073 (2020).
Yarchoan, M. et al. Association of cancer history with Alzheimer’s disease dementia and neuropathology. J. Alzheimers Dis. 56, 699–706. https://doi.org/10.3233/JAD-160977 (2017).
van der Willik, K. D. et al. Mild cognitive impairment and dementia show contrasting associations with risk of cancer. Neuroepidemiology 50, 207–215. https://doi.org/10.1159/000488892 (2018).
Fowler, C. et al. Fifteen years of the Australian imaging, biomarkers and lifestyle (AIBL) study: Progress and observations from 2,359 older adults spanning the spectrum from cognitive normality to Alzheimer’s disease. J. Alzheimers Dis. Rep. 5, 443–468. https://doi.org/10.3233/ADR-210005 (2021).
Ellis, K. A. et al. The Australian imaging, biomarkers and lifestyle (AIBL) study of aging: Methodology and baseline characteristics of 1112 individuals recruited for a longitudinal study of Alzheimer’s disease. Int. Psychogeriatr. 21, 672–687. https://doi.org/10.1017/S1041610209009405 (2009).
O’Bryant, S. E. et al. Staging dementia using clinical dementia rating scale sum of boxes scores: A Texas Alzheimer’s research consortium study. Arch. Neurol. 65, 1091–1095. https://doi.org/10.1001/archneur.65.8.1091 (2008).
Ma, L. L. et al. Association between cancer and Alzheimer’s disease: Systematic review and meta-analysis. J. Alzheimers Dis. 42, 565–573. https://doi.org/10.3233/JAD-140168 (2014).
Papageorgakopoulos, T. N., Moraitou, D., Papanikolaou, M. & Tsolaki, M. The association between Alzheimer’s disease and cancer: Systematic review—Meta-analysis. Hell J Nucl Med 20(Suppl), 45–57 (2017).
Mounier, N. M., Abdel-Maged, A. E., Wahdan, S. A., Gad, A. M. & Azab, S. S. Chemotherapy-induced cognitive impairment (CICI): An overview of etiology and pathogenesis. Life Sci. 258, 118071. https://doi.org/10.1016/j.lfs.2020.118071 (2020).
Shigemizu, D. et al. Prognosis prediction model for conversion from mild cognitive impairment to Alzheimer’s disease created by integrative analysis of multi-omics data. Alzheimers Res. Ther. 12, 145. https://doi.org/10.1186/s13195-020-00716-0 (2020).
Weil, R. S., Costantini, A. A. & Schrag, A. E. Mild cognitive impairment in Parkinson’s disease—What is it?. Curr. Neurol. Neurosci. Rep. 18, 17. https://doi.org/10.1007/s11910-018-0823-9 (2018).
Hemminghyth, M. S., Chwiszczuk, L. J., Rongve, A. & Breitve, M. H. The cognitive profile of mild cognitive impairment due to dementia with Lewy bodies—An updated review. Front. Aging Neurosci. 12, 597579. https://doi.org/10.3389/fnagi.2020.597579 (2020).
Karanth, S. D. et al. Cancer diagnosis is associated with a lower burden of dementia and less Alzheimer’s-type neuropathology. Brain 145, 2518–2527. https://doi.org/10.1093/brain/awac035 (2022).
Hu, J. et al. Targeting mutant p53 for cancer therapy: Direct and indirect strategies. J. Hematol. Oncol. 14, 157. https://doi.org/10.1186/s13045-021-01169-0 (2021).
Patil, M. R. & Bihari, A. A comprehensive study of p53 protein. J. Cell Biochem. 123, 1891–1937. https://doi.org/10.1002/jcb.30331 (2022).
Rivlin, N., Brosh, R., Oren, M. & Rotter, V. Mutations in the p53 tumor suppressor gene: Important milestones at the various steps of tumorigenesis. Genes Cancer 2, 466–474. https://doi.org/10.1177/1947601911408889 (2011).
Hampel, H. et al. The amyloid-beta pathway in Alzheimer’s disease. Mol. Psychiatry 26, 5481–5503. https://doi.org/10.1038/s41380-021-01249-0 (2021).
Shafi, O. Inverse relationship between Alzheimer’s disease and cancer, and other factors contributing to Alzheimer’s disease: A systematic review. BMC Neurol. 16, 236. https://doi.org/10.1186/s12883-016-0765-2 (2016).
Ohyagi, Y. et al. Intracellular Abeta42 activates p53 promoter: A pathway to neurodegeneration in Alzheimer’s disease. FASEB J. 19, 255–257. https://doi.org/10.1096/fj.04-2637fje (2005).
Hooper, C. et al. p53 is upregulated in Alzheimer’s disease and induces tau phosphorylation in HEK293a cells. Neurosci. Lett. 418, 34–37. https://doi.org/10.1016/j.neulet.2007.03.026 (2007).
Batlle, E. & Massague, J. Transforming growth factor-beta signaling in immunity and cancer. Immunity 50, 924–940. https://doi.org/10.1016/j.immuni.2019.03.024 (2019).
Burton, T., Liang, B., Dibrov, A. & Amara, F. Transforming growth factor-beta-induced transcription of the Alzheimer beta-amyloid precursor protein gene involves interaction between the CTCF-complex and Smads. Biochem. Biophys. Res. Commun. 295, 713–723. https://doi.org/10.1016/s0006-291x(02)00725-8 (2002).
Riella, L. V., Paterson, A. M., Sharpe, A. H. & Chandraker, A. Role of the PD-1 pathway in the immune response. Am. J. Transplant. 12, 2575–2587. https://doi.org/10.1111/j.1600-6143.2012.04224.x (2012).
Sakuishi, K. et al. Targeting Tim-3 and PD-1 pathways to reverse T cell exhaustion and restore anti-tumor immunity. J. Exp. Med. 207, 2187–2194. https://doi.org/10.1084/jem.20100643 (2010).
Kummer, M. P. et al. Microglial PD-1 stimulation by astrocytic PD-L1 suppresses neuroinflammation and Alzheimer’s disease pathology. EMBO J. 40, e108662. https://doi.org/10.15252/embj.2021108662 (2021).
Zablocka, A. et al. Inverse Alzheimer’s disease and cancer: Short overview. Mol. Neurobiol. 58, 6335–6349. https://doi.org/10.1007/s12035-021-02544-1 (2021).
Pan, Y. et al. Cognitive benefits of lithium chloride in APP/PS1 mice are associated with enhanced brain clearance of beta-amyloid. Brain Behav. Immun. 70, 36–47. https://doi.org/10.1016/j.bbi.2018.03.007 (2018).
Bradley, G. & Ling, V. P-glycoprotein, multidrug resistance and tumor progression. Cancer Metastasis Rev. 13, 223–233. https://doi.org/10.1007/BF00689638 (1994).
Acknowledgements
The salary of Y.P. and APC were funded by National Health and Medical Research Council (grant number GNT2007912) and Alzheimer’s Association USA (grant number 23AARF-1020292).
Author information
Authors and Affiliations
Contributions
The study conception and design were elaborated by L.M., E.T., L.J. & Y.P. C.J.F & C.L.M. recruited the study participants and collected the data. Data processing was performed by Y.Z. and Y.W. Data analysis was performed by Y.L., C.C. & L.M. Manuscript was drafted by L.M. & Y.L. and edited by all other co-authors. All authors reviewed and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ma, L., Low, Y.L.C., Zhuo, Y. et al. Exploring the association between cancer and cognitive impairment in the Australian Imaging Biomarkers and Lifestyle (AIBL) study. Sci Rep 14, 4364 (2024). https://doi.org/10.1038/s41598-024-54875-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-54875-3
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.