Abstract
The use of intraoperative sub-anesthetic esketamine for postoperative analgesia is controversial. In this study, the impact of sub-anesthetic esketamine on postoperative opioid self-administration was determined. Patients who underwent spinal surgery with patient-controlled analgesia (PCA) from January 2019 to December 2021 were respectively screened for analysis. Postoperative PCA was compared between patients who received a sub-anesthetic esketamine dose and patients who were not treated with esketamine (non-esketamine group) with or without propensity score matching. Negative binomial regression analysis was used to identify factors associated with postoperative PCA. Patients who received intraoperative sub-anesthetic esketamine self-administered less PCA (P = 0.001). Azasetron, esketamine, and dexamethasone lowered the self-administration of PCA (IRR with 95% confidential interval, 0.789 [0.624, 0.993]; 0.581 [0.458, 0.741]; and 0.777 [0.627, 0.959], respectively). Fixation surgery and drinking were risk factors for postoperative PCA (1.737 [1.373, 2.188] and 1.332 [1.032, 1.737] for fixation surgery and drinking, respectively). An intraoperative sub-anesthetic dose of esketamine decreases postoperative opioid self-administration. Azasetron and dexamethasone also decrease postoperative opioid consumption. The study is registered at www.chictr.org.cn (ChiCTR2300068733).
Similar content being viewed by others
Introduction
Postoperative pain is a common complication after spinal surgery. The postoperative pain significantly hinders postoperative rehabilitation and affects overall physical and mental health1. Effective postoperative pain management is challenging for clinicians, and many patients suffer from moderate to severe pain after surgery2. Postoperative pain is a complex physiological and psychological response, arising from multiple factors, including wound stimulation, inflammatory response, and increased neural sensitivity. In severe cases, postoperative pain can lead to serious complications, including chronic pain and deep vein thrombosis3. Opioids are the most widely used medication for postoperative analgesia. However, complications, including respiration depression, constipation, tolerance, hyperalgesia, and addiction, limit the use of opioids. Non-opioid analgesic adjuvants are a promising approach for postoperative analgesia to avoid opioid-related complications.
Esketamine is used to treat depression and depressive disorders. Recently, esketamine has been used for postoperative analgesia. We previously demonstrated that a sub-anesthetic dose of esketamine decreases pain and anxiety after thyroid and breast surgery4. However, a recent large multi-center study demonstrated that intraoperative ketamine did not exhibit any analgesic effects5. In a recent meta-analysis, intravenous esketamine decreased pain intensity and opioid requirements after surgery, but the level of certainty was moderate to low6. Thus, the effects of intraoperative esketamine on postoperative pain are unclear. A high dose of esketamine may increase postoperative complications. Therefore, we determined the impact of a sub-anesthetic dose of intraoperative esketamine on postoperative opioid self-administration in the setting of patient-controlled analgesia (PCA) after spinal surgery.
Methods
This study followed the Declaration of Helsinki and was approved by the Ethics Committee of Xiangyang Central Hospital, which is affiliated with Hubei University of Arts and Science. The study was registered at www.chictr.org.cn (ChiCTR2300068733). Patient written informed consent was waived by the Ethics Committee of Xiangyang Central Hospital, and patient information was deidentified before the data analysis.
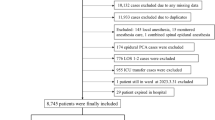
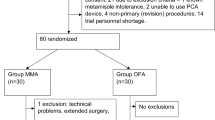
Patients who underwent spinal surgery with postoperative PCA in our tertiary hospital from January 2019 to December 2021 were eligible for the study. Patient exclusion criteria included extubation failure after surgery. The PCA pump (Jiangsu Renxian Medical Manufacture Technology) recorded information about the time and the number of PCA pushes. All patients were returned to the wards with a numerical rating scale (NRS) for pain of less than 4 and were educated to push the button if their NRS was equal to or higher than 4. The 100-mL PCA pump contained 10 mg of hydromorphone and 20 mg of azasetron. The parameters were set at a rate of 2 mL/h, 1.5 mL per push, and a lock-out time of 15 min.
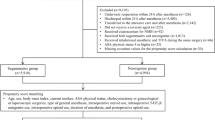
All patients used propofol, midazolam, sufentanil, rocuronium bromide, cisatracurium, and sevoflurane for anesthesia induction and maintenance. Patient information about intraoperative adjuvants was retrospectively collected from electronic records. The use of anesthesia adjuvants, including azasetron 10 mg, esketamine 0.2–0.5 mg/kg, dexamethasone 10 mg, flurbiprofen 50 mg, dezocine 5 mg, hydromorphone 0.4 mg, and dexmedetomidine 0.5 μg/kg/h, was determined by the anesthetists. Surgery types included internal fixation and non-fixation surgeries. Patient demographics (sex, age, BMI, and weight), previous comorbidities (smoking, drinking, lumbar surgery history, cerebrovascular disease, heart disease, pulmonary disease, hepatic disease, renal disease, hypertension, and diabetes mellitus [DM]), previous psychiatric illness (schizophrenia and depression), patient status (American Society of Anesthesiologists [ASA] physical status, heart function), laboratory test results (white blood cell count [WBC], neutrophil, uric acid, C-reactive protein [CRP]), surgery information (surgery duration, surgery with fixation or not), other intraoperative anesthesia adjuvants (azasetron, dexamethasone, flurbiprofen, dezocine, hydromorphine, and dexmedetomidine), and preoperative and postoperative analgesia usage (nonsteroidal antiinflammatory drug [NSAID] and opioid) were collected from the electronic health database and included in the relevant factor analysis. The follow-up time was 48 h after surgery.
Statistical analysis
Continuous and categorical data are presented as means (standard deviation, SD) and numbers (interquartile range, IQR), respectively. Propensity score matching was used as a sensitivity analysis. The “MatchIt” package for the R statistical software package was utilized for propensity score matching. Patient demographics, previous comorbidities, patient status, laboratory test results, intraoperative anesthesia adjuvants, and surgery information were adjusted with the nearest neighbor, and a caliper width of 0.2 standard deviations of the logit of the propensity score was used. Univariate and multivariable negative binomial regression analyses (“MASS” package for the R statistical software package) were used to identify factors associated with postoperative PCA use. In addition, PCA use was compared between different esketamine doses. Surgery type and sex-specific effects of esketamine and other therapies were analyzed. A P < 0.05 indicated a statistical difference.
Ethics approval and consent to participate
The study was approved by the ethics committee of Xiangyang Central Hospital, Affiliated with Hubei University of Arts and Science.
Results
Baseline characteristics
Patient baseline characteristics are shown in Table 1. During the study period, 590 patients received PCA after spinal surgery, and 121 patients received esketamine. Approximately half of patients (55%) were female. Fewer patients received flurbiprofen and more patients underwent fixation surgery in the esketamine group compared with the non-esketamine groups (P < 0.05). No significant differences in demographics (sex, age, BMI, or weight), previous comorbidities (smoking, drinking, lumbar surgery history, cerebrovascular disease, heart disease, pulmonary disease, hepatic disease, renal disease, hypertension, or DM), patient status (ASA physical status or heart function), laboratory test results (WBC, neutrophil, uric acid, or CRP), preoperative NSAID usage, surgery parameters (surgery duration or surgery with fixation), or other intraoperative anesthesia adjuvants (azasetron, dexamethasone, flurbiprofen, dezocine, hydromorphine, or dexmedetomidine) were detected. No patients were diagnosed with preoperative psychiatry illness, including schizophrenia, and depression, and no patients received opioids for analgesia before surgery. Postoperative PCA (the number of PCA pushes) was lower in the esketamine group compared with PCA use in the non-esketamine group (2.00 [0.00, 3.00] vs. 3.00 [1.00, 7.00], P = 0.001, Table 1). In addition, the postoperative NSAID requirement was less in the esketamine group compared with the non-esketamine group (19.8 vs. 33.7%, P = 0.005).
Baseline characteristics adjusted with propensity score matching
Because the data was imbalanced, variables were adjusted using propensity score matching. The baseline characteristics of 120 patient pairs identified by propensity score matching are listed in Table 2. No significant differences in demographics, previous comorbidities, patient status, laboratory test results, surgery information, and other intraoperative anesthesia adjuvants were detected between the two groups. The number of PCA pushes was higher in the esketamine group compared with the number of pushes in the non-esketamine group (2.00 [0.00, 3.00] vs. 3.00 [1.00, 6.25], P = 0.001, Table 2). However, postoperative NSAID requirements were not different between the two groups (esketamine, 20.0% vs. non-esketamine, 30.8%, P = 0.075).
Negative binomial regression analysis
The number of PCA pushes exhibited a negative binomial distribution. Therefore, the factors associated with postoperative PCA pushes were identified using negative binomial regression. Univariate negative binomial regression indicated that drinking, heart disease, preoperative NSAID use, azasetron, esketamine, dexamethasone, and fixation surgery were associated with postoperative PCA pushes. Multivariate negative binomial regression showed that azasetron, esketamine, and dexamethasone prevented postoperative PCA pushes, while fixation surgery and drinking were risk factors for postoperative PCA pushes (Table 3). The IRRs (95% confidential interval) were 0.789 [0.624, 0.993] for azasetron, 0.581 [0.458, 0.741] for esketamine, 0.777 [0.627, 0.959] for dexamethasone, 1.737 [1.373, 2.188] for fixation surgery, and 1.332 [1.032, 1.737] for drinking.
Esketamine dose for postoperative PCA
The effects of different esketamine doses on postoperative PCA were explored. Patients who received higher doses of esketamine used fewer PCA pushes (2.50 [1.00, 5.00] for 0.2 mg/kg, 2.00 [0.50, 3.00] for 0.3 mg/kg, 1.00 [0.00, 2.50] for 0.4 mg/kg, 1.00 [0.00, 3.00] for 0.5 mg/kg, P overall = 0.035, P for trend = 0.013, Supplementary Table 1).
Effects of esketamine and other therapies on PCA in different sexes and surgery types
Esketamine (P = 0.001 for males, P = 0.036 for females, Supplementary Table 2) and dexamethasone (P = 0.038 for males, P = 0.001 for females) decreased the number of postoperative PCA pushes in both males and females. Azasetron decreased postoperative pushes of PCA in females (2.00 [1.00, 4.00] vs. 4.00 [2.00, 8.75], P = 0.001), but not in males (2.00 [1.00, 6.00] vs. 4.50 [1.00, 8.75], P = 0.063). No significant differences in the number of PCA pushes related to intraoperative flurbiprofen, dezocine, hydromorphone, and dexmedetomidine were detected between males and females (P > 0.05).
Esketamine (P = 0.321 for fixation, P = 0.001 for non-fixation), azasetron (P = 0.141 for fixation, P = 0.001 for non-fixation), and dexamethasone (P = 0.336 for fixation, P = 0.001 for non-fixation) decreased the number of postoperative PCA pushes in patients who underwent fixation surgery, but not in patients who underwent non-fixation surgery (P > 0.05, Supplementary Table 3). No significant effects of intraoperative flurbiprofen, dezocine, hydromorphone, and dexmedetomidine on postoperative PCA pushes were detected in patients who underwent fixation or non-fixation surgeries.
Discussion
Our results demonstrated that an intraoperative sub-anesthetic dose of esketamine decreases postoperative opioid self-administration. Intraoperative azasetron, esketamine, and dexamethasone also reduce postoperative opioid self-administration, while fixation surgery and drinking are risk factors for increased postoperative opioid self-administration.
In a previous study, a sub-anesthetic dose of ketamine did not affect postoperative pain and opioid consumption in patients aged 60 years or older undergoing major surgery5. In contrast, a recent systematic review demonstrated that intraoperative ketamine decreases postoperative pain and opioid consumption7. The multi-center study with a large sample size did not agree with the single-center study with a small sample size. Our results indicate that intraoperative esketamine is analgesic and decreases postoperative opioid consumption. The opioid-saving effects may be due to antagonism of NMDA receptors. NMDA receptors are critical for pain signal transduction in the central nervous system, and inhibition of NMDA receptors prevents postoperative pain transmission and central sensitization8. We previously showed that intraoperative sub-anesthetic doses of esketamine decreased postoperative pain and anxiety. However, postoperative opioid use was not quantified, and the extent of decreased postoperative opioid consumption was unclear.
A recent study demonstrated that postoperative low-dose ketamine reduced hydromorphone requirements during the first 24 h after lumbar surgery in opioid-tolerant patients9. In contrast, our experiment was performed in non-opioid-dependent and tolerant patients. In addition, postoperative PCA was used instead of prescription opioids; thus, patient requirements were represented better. Overall, our results provide evidence that intraoperative esketamine decreases postoperative opioid consumption. We also explored the effects of different doses of esketamine on postoperative opioid consumption. Postoperative opioid consumption was significantly different among the four esketamine dose groups. Higher doses of esketamine resulted in less opioid consumption, suggesting that the analgesic effect of esketamine is dose-dependent from 0.2 to 0.5 mg/kg.
In addition to esketamine, the multivariate analysis demonstrated that azasetron and dexamethasone also lowered postoperative opioid self-administration. Azasetron is a 5HT3 receptor antagonist, and a previous study demonstrated that antagonism of 5HT3 receptors prevents inflammation10 and opioid antinociceptive tolerance11,12. Another study by our team demonstrated that azasetron reduced postoperative acute pain after thoracic surgery (in submission). In addition, several systematic reviews showed that a single dexamethasone dose decreases postoperative pain and opioid self-administration13,14,15. Dexamethasone may decrease postoperative pain by inhibiting the immune system response to surgery, including the formation and release of histamine and other toxic substances16,17. Thus, in addition to esketamine, azasetron and dexamethasone should also be considered for patients undergoing spinal surgery. Our results also demonstrate that drinking is a risk factor for postoperative opioid self-administration. Pain and alcohol share overlapping neural circuitry, and persistent drinking results in vitamin B1 deficiency, disrupted carbohydrate metabolism, and increased oxidative stress and mitochondrial load18,19. These pathological changes may contribute to enhanced cytokine production, increased mitogen-activated protein kinase, and microglial activation, which contribute to the development and maintenance of chronic pain20. Finally, our results showed that patients who underwent fixation surgery used more PCA. Fixation surgery causes more tissue and bone damage, resulting in more severe pain. Thus, fixation surgery and drinking are risk factors for more frequent postoperative opioid self-administration.
Previous studies demonstrated sex-based differences in pharmacokinetics and pharmacodynamics21,22. Pharmacokinetics represents the dosage of a drug and changes in drug concentrations in the body over time. Drug bioavailability, distribution, metabolism, and excretion affect pharmacokinetics. Gastric emptying, body fat proportion, plasma volume, hepatic enzymes, and renal function all contribute to sex-based differences in pharmacokinetics23. Thus, the same plasma concentration of a drug may result in different clinical outcomes due to sex-based differences in pharmacodynamics. We observed significant differences in the effects of azasetron but not esketamine or other pharmacotherapies on postoperative opioid consumption between males and females. A prospective randomized trial may confirm the pharmacological effects of esketamine on postoperative opioid consumption in different sexes. Our study also showed that the analgesic effects of esketamine, dexamethasone, and azasetron were more robust in patients undergoing fixation surgery compared with patients undergoing non-fixation surgery. Patients undergoing fixation surgery experience higher pain intensity and require higher opioid doses to control the pain. Thus, the analgesic effects were statistically significant in patients with higher pain intensity.
Although our study showed that esketamine is associated with fewer postoperative PCA pushes, our study has several limitations. This was a retrospective study and some possible confounding variables, including surgical techniques24 and preoperative anxiety levels25, could not be determined. In addition, the adverse effects of esketamine26, including delirium, hallucination, and nightmares, were not determined in this study. Thus, our results may overestimate the advantage of esketamine. Lastly, esketamine is used to treat depression27,28, and the anti-depressive effects could be masked by anesthesia29. However, no patients were diagnosed with depression preoperative in this study. Thus, the anti-depressive effects were not observed in our study. A prospective randomized controlled trial should be performed to provide robust support for the effects of esketamine on postoperative opioid self-administration.
Conclusions
In this study, it was found that a sub-anesthetic dose of esketamine decreased postoperative opioid self-administration after spinal surgery. Therefore, intraoperative esketamine, dexamethasone, and azasetron should be considered for patients undergoing spinal surgery.
Data availability
The data set analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- ASA:
-
American Society of Anesthesiologists
- CRP:
-
C-reactive protein
- DM:
-
Diabetes mellitus
- IRRs:
-
Incidence rate ratios
- IQR:
-
Interquartile range
- NRS:
-
Numerical rating scale of pain
- NSAID:
-
Nonsteroidal antiinflammatory drug
- PCA:
-
Patient-controlled analgesia
- SD:
-
Standard deviation
- WBC:
-
White blood cell count
References
Willingham, M. et al. Association between postoperative complications and lingering post-surgical pain: An observational cohort study. Br. J. Anaesth. 124, 214–221 (2020).
Peene, L., Le Cacheux, P., Sauter, A. R., Joshi, G. P. & Beloeil, H. Pain management after laminectomy: A systematic review and procedure-specific post-operative pain management (prospect) recommendations. Eur. Spine J. 30, 2925–2935 (2021).
van Boekel, R. et al. Relationship between postoperative pain and overall 30-day complications in a broad surgical population: An observational study. Ann. Surg. 269, 856–865 (2019).
Zhou, D. et al. Sub-anesthesia dose of S-ketamine reduces postoperative pain and anxiety in patients receiving breast and thyroid surgery: A randomized, controlled trial. Pain Phys. 26, 257–264 (2023).
Avidan, M. S. et al. Intraoperative ketamine for prevention of postoperative delirium or pain after major surgery in older adults: An international, multicentre, double-blind, randomised clinical trial. Lancet 390, 267–275 (2017).
Wang, X., Lin, C., Lan, L. & Liu, J. Perioperative intravenous S-ketamine for acute postoperative pain in adults: A systematic review and meta-analysis. J. Clin. Anesth. 68, 110071 (2021).
Riddell, J. M., Trummel, J. M. & Onakpoya, I. J. Low-dose ketamine in painful orthopaedic surgery: A systematic review and meta-analysis. Br. J. Anaesth. 123, 325–334 (2019).
Qiu, S. et al. An increase in synaptic Nmda receptors in the insular cortex contributes to neuropathic pain. Sci. Signal. 6, 34 (2013).
Boenigk, K. et al. Low-dose ketamine infusion reduces postoperative hydromorphone requirements in opioid-tolerant patients following spinal fusion: A randomised controlled trial. Eur. J. Anaesth. 36, 8–15 (2019).
Utsumi, D., Matsumoto, K., Amagase, K., Horie, S. & Kato, S. 5-Ht3 receptors promote colonic inflammation via activation of substance P/neurokinin-1 receptors in dextran sulphate sodium-induced murine colitis. Br. J. Pharmacol. 173, 1835–1849 (2016).
Liang, D. Y., Li, X. & Clark, J. D. 5-Hydroxytryptamine type 3 receptor modulates opioid-induced hyperalgesia and tolerance in mice. Anesthesiology 114, 1180–1189 (2011).
Kimura, M., Obata, H. & Saito, S. Peripheral nerve injury reduces analgesic effects of systemic morphine via spinal 5-hydroxytryptamine 3 receptors. Anesthesiology 121, 362–371 (2014).
Singh, N. P., Makkar, J. K., Yadav, N., Goudra, B. G. & Singh, P. M. The analgesic efficacy of intravenous dexamethasone for post-caesarean pain: A systematic review with meta-analysis and trial sequential analysis. Eur. J. Anaesth. 39, 498–510 (2022).
Heesen, M. et al. Effect of intravenous dexamethasone on postoperative pain after spinal anaesthesia—A systematic review with meta-analysis and trial sequential analysis. Anaesthesia 74, 1047–1056 (2019).
Fan, Z. et al. The efficacy of dexamethasone reducing postoperative pain and emesis after total knee arthroplasty: A systematic review and meta-analysis. Int. J. Surg. 52, 149–155 (2018).
Wang, K. et al. Effects of dexmedetomidine on perioperative stress, inflammation, and immune function: Systematic review and meta-analysis. Br. J. Anaesth. 123, 777–794 (2019).
Straub, R. H. & Cutolo, M. Glucocorticoids and chronic inflammation. Rheumatology 55, 6–14 (2016).
de la Monte, S. M. & Kril, J. J. Human alcohol-related neuropathology. Acta Neuropathol. 127, 71–90 (2014).
Miguel-Hidalgo, J. J. Molecular neuropathology of astrocytes and oligodendrocytes in alcohol use disorders. Front. Mol. Neurosci. 11, 78 (2018).
Robins, M. T., Heinricher, M. M. & Ryabinin, A. E. From pleasure to pain, and back again: The intricate relationship between alcohol and nociception. Alcohol Alcohol. 54, 625–638 (2019).
Farkouh, A., Riedl, T., Gottardi, R., Czejka, M. & Kautzky-Willer, A. Sex-related differences in pharmacokinetics and pharmacodynamics of frequently prescribed drugs: A review of the literature. Adv. Ther. 37, 644–655 (2020).
Soldin, O. P. & Mattison, D. R. Sex differences in pharmacokinetics and pharmacodynamics. Clin. Pharmacokinet. 48, 143–157 (2009).
Zucker, I. & Prendergast, B. J. Sex differences in pharmacokinetics. Handb. Exp. Pharmacol. 282, 25–39 (2023).
Rawal, N. Current issues in postoperative pain management. Eur. J. Anaesth. 33, 160–171 (2016).
Reddi, D. Preventing chronic postoperative pain. Anaesthesia 71(Suppl 1), 64–71 (2016).
Hollmann, M. W., Rathmell, J. P. & Lirk, P. Optimal postoperative pain management: Redefining the role for opioids. Lancet 393, 1483–1485 (2019).
Reif, A. et al. Esketamine nasal spray versus quetiapine for treatment-resistant depression. N. Engl. J. Med. 389, 1298–1309 (2023).
Swainson, J. et al. Esketamine for treatment resistant depression. Expert Rev. Neurother. 19, 899–911 (2019).
Lii, T. R. et al. Randomized trial of ketamine masked by surgical anesthesia in patients with depression. Nat. Ment. Health 1, 876–886 (2023).
Acknowledgements
This research is funded by Grants from the Natural Science Foundation of Hubei province (2023AFD041) and Xiangyang (2021YL017).
Author information
Authors and Affiliations
Contributions
Designed and supervised the study: X.R.G.; Data acquisition and sorting: H.Y.Z., P.Z., X.Z. and Q.C.; Statistical analysis and interpretation of data: S.N.S., and X.R.G.; Drafting and critical revision of the article: X.R.G., and Q.C.; All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zheng, H., Zhang, P., Shi, S. et al. Sub-anesthetic dose of esketamine decreases postoperative opioid self-administration after spine surgery: a retrospective cohort analysis. Sci Rep 14, 3909 (2024). https://doi.org/10.1038/s41598-024-54617-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-54617-5
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.