Abstract
Contraception and abortion topics are variably, but often poorly, addressed in medical school curricula. Restrictions on contraceptive and abortion care at faith-based hospitals may hinder comprehensive family planning training for medical students during Ob/Gyn clerkships. Here we investigated whether medical students at faith-based and non-faith-based clerkships experienced different observations during their Ob/Gyn clerkship and/or differences in self-perceived competency in patient counseling, objective knowledge, and perceived adequacy of training in contraception and abortion topics post-clerkship. A survey was distributed to third- and fourth-year medical students at New York Institute of Technology, College of Osteopathic Medicine. Across all clerkship sites (n = 102 students), observations of, and competency in, contraceptive care was higher than in abortion care. Students at non-faith-based clerkship sites (n = 54) reported the highest levels of observation of contraceptive and abortion care (19.6–90.7%), while those at Catholic sites (n = 26) typically reported the lowest (7.7–34.6%). Students at non-faith-based sites reported significantly higher competency in contraceptive care and some aspects of abortion care, than those at Catholic, and some other faith-based sites (n = 48). Clerkship training at faith-based sites, specifically Catholic sites, resulted in poorer Ob/Gyn training, particularly in contraceptive care. Training outcomes in abortion care were poor at all Ob/Gyn clerkship sites.
Similar content being viewed by others
Introduction
Family planning services, specifically contraception and abortion, are essential healthcare needs utilized by millions of patients each year. For many medical students, initial hands-on training in these topics occurs during their Ob/Gyn clerkship. While contraceptive and abortion care are included as educational objectives in nationwide guidelines for Ob/Gyn clerkships1, previous research has shown that these topics are poorly represented in Ob/Gyn curricula2,3,4,5,6.
One potential barrier to robust clerkship training is that many clerkships take place at faith-based hospitals or practices, some of which place restrictions on contraceptive and abortion care. In particular, Catholic-affiliated sites are expected to follow the “Ethical and Religious Directives for Catholic Healthcare Services” (ERDs)7. The ERDs place restrictions on the use of contraception and induced abortion procedures broadly across Catholic-affiliated hospitals and practices. Yet institutional objections and hospital-specific restrictions limiting family planning care have also been documented at faith-based hospitals of other religious denominations8,9,10. Together, this restrictive health care landscape likely affects the ability of Catholic and other faith-based institutions to provide comprehensive family planning training during clerkships. Previous research has shown that students at one Catholic medical school felt their clinical contraception and abortion training was overwhelmingly inadequate6 and standardized examination scores following the Ob/Gyn clerkship at another institution were lower for students at Catholic-affiliated sites11. These trends are also mirrored in residency programs, where many faith-based programs were found to be somewhat deficient in contraception training, and even more so in abortion training12.
Here, we evaluated whether medical students at New York Institute of Technology, College of Osteopathic Medicine (NYIT COM) who performed their Ob/Gyn clerkships at faith-based sites experienced differential outcomes compared to students at non-faith-based clerkship sites. NYIT COM is composed of two geographically separate sites (Old Westbury, New York and Jonesboro, Arkansas). Both sites follow the same educational curriculum and learning objectives, and at both sites Ob/Gyn clerkships take place at a mix of faith-based and non-faith-based sites. Specifically, regarding contraception and abortion training we evaluated if there was a difference in 1) what students observed during the Ob/Gyn clerkship, 2) self-perceived competency in patient counseling following the clerkship, 3) objective contraception and abortion knowledge, and 4) perceived adequacy of training received during the clerkship, between faith-based and non-faith-based sites. We hypothesized that students at faith-based clerkship sites, and in particular Catholic sites, would have lower outcomes in all four areas (1–4 above). Given the common Ob/Gyn educational curriculum, we did not expect to see any differences in clerkship outcomes between the two NYIT COM campus sites.
Results
Study demographics
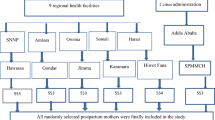
E-mail survey invitations were sent to 845 eligible third- and fourth-year students, including two follow-up reminder emails. From this, 150 students opened the survey and 116 were returned completed (completion rate of 77.3% following CHERRIES guidelines13). Fourteen participants were excluded because they did not provide an identifiable clerkship site, resulting in a final total of 102 participants. Of these, 19 incorrectly reported, or did not know, the religious affiliation of their clerkship site. Following verification and correction, this resulted in a total of 28 clerkship sites represented in the sample (OW: 15; JB: 13) with 54 students at non-faith-based sites, 26 at Catholic sites, 15 at Jewish sites, and 7 at Protestant clerkship sites (Table 1). There were no significant associations between student religious identity or gender and the religious affiliation of the clerkship site they attended (Supplementary Table S1).
Observations
Across all sites students more frequently observed patient care related to contraception than any abortion-related care (Table 2, Fig. 1). Overall, 69.6% of students witnessed patient counseling on contraceptive methods and 62.7% observed prescription of contraception versus a maximum observation frequency of 28.4% for any abortion care topic. Among clerkship site affiliations, students at non-faith-based sites reported the highest levels of observation for most of the patient care topics presented (5 of 8). Students at Catholic sites reported the lowest levels of observation for 6 of 8 topics, and students at Jewish and Protestant sites tended to report intermediate levels of observation (Table 2; Fig. 1). Pairwise Fisher’s tests showed that students at non-faith-based sites observed significantly more contraceptive counseling compared to students at Catholic or Jewish sites (pairwise Fisher’s test: P < 0.001 and P < 0.01, respectively; Table 2) and significantly more prescribing of contraception compared to students at Catholic sites (pairwise Fisher’s test: P < 0.001). Students at non-faith-based sites also observed significantly more follow-up visits with a patient who recently had an abortion than students at Catholic sites (pairwise Fisher’s test: P < 0.05). Student observations of non-directive patient counseling about pregnancy termination options also showed a significant effect of clerkship site religious affiliation (Fisher’s exact test: P < 0.05), however no post-hoc pairwise tests reached the level of significance (Table 2). Only 1.9% of students at non-faith-based sites reported observing ‘none of the above’, significantly less than students at Catholic sites (42.3%, pairwise Fisher’s test: P < 0.001) and Jewish sites (26.7%, pairwise Fisher’s test: P < 0.05). Students at Protestant sites also reported moderate frequencies of ‘none of the above’ (28.6%), though this was not significantly different from students at non-faith-based sites (pairwise Fisher’s test: P = 0.065), likely because the sample size of the former was small (n = 7).
Results of student observations regarding family planning topics. All questions began with the prompt, “During my OB/GYN clerkship, I observed…”. All results are standardized by percentage of student responses for the religious affiliation of the clerkship site. Bars and asterisks represent a significant difference between religious affiliation of the clerkship (pairwise Fisher’s tests) at either the P < 0.05*, P < 0.01**, or P < 0.001*** level.
Self-perceived competency in patient counseling
Irrespective of campus site or clerkship affiliation, the self-perceived competency of contraceptive counseling was higher than that of abortion counseling. Students felt they were most knowledgeable to discuss methods of contraception with patients (3.3 ± 1.3; Fig. 2, Table 3). Students were only slightly less confident in counseling patients regarding the benefits, risks, and appropriate use of contraception, and in counseling on different methods of contraception (3.2 ± 1.3, 3.1 ± 1.3, respectively). Self-perceived competency regarding topics of abortion care was low (Fig. 2, Table 3). Of abortion care topics, students were most competent in adequately explaining all options of an unintended pregnancy to patients (2.6 ± 1.3) and least competent in their confidence and ability to adequately explain to patients what to expect from an abortion (2.3 ± 1.2).
Results of self-assessed student competency in contraceptive and abortion counseling. All questions began with a prompt regarding their Ob/Gyn clerkship, “After the clerkship…”. All results are standardized by percentage of student responses within a religious affiliation category. Bars and asterisks represent a significant difference between religious affiliation of the clerkship site (pairwise Tukey differences resulting from linear model) at either the P < 0.05*, P < 0.01**, or P < 0.001*** level.
Among clerkship sites, significant differences between religious affiliations existed for all contraception statements, and for one of the abortion statements (Table 4). Students at non-faith-based clerkships sites were significantly more confident in their ability to counsel patients regarding the benefits, risks, and appropriate use of contraception compared to students at religiously affiliated sites (Linear Model [LM]: P < 0.05; Fig. 2, Table 4). They also reported being significantly more knowledgeable in terms of discussing methods of contraception compared to students at religiously affiliated sites (LM: P < 0.05). Students at non-faith-based clerkships rated their ability to counsel patients on the different methods of contraception significantly higher than students at Catholic-affiliated sites (LM: P < 0.05). Among abortion statements, students at non-faith-based sites reported higher competence in adequately explaining all options to a patient with an unintended pregnancy, compared to students at Catholic and Jewish clerkship sites (LM: P < 0.05). For only two questions was the factor of NYIT COM site (OW vs. JB) significant (Tables 3 and 4). Both were statements of contraception competency for which religious affiliation also had a significant effect. For both, students at the JB site felt 1.1–1.2 points more competent than students at the OW site. Nevertheless, the effect of religious affiliation across both sites was the same polarity (Table 3).
Objective knowledge
Students scored higher on the contraception questions (1.8 ± 0.7 of 3) compared to the abortion questions (1.4 ± 1.0 of 5; Table 5). There were no significant differences between religious affiliation of the clerkship site, nor were there any differences between campus sites on either the contraception or abortion questions, nor on the total score. Overall, student performance on the objective knowledge assessment, especially the abortion questions, was poor, and no student received a full score.
Perceived adequacy of training
Students overwhelmingly agreed that clinical experience in contraceptive and abortion care is important to offer in medical school (4.6 ± 0.7 and 4.5 ± 0.8, respectively; Table 3). Students were neutral as to whether the preclinical curriculum regarding contraception adequately prepared them for patient counseling (3.0 ± 1.1) and somewhat disagreed that their preclinical curriculum prepared them to counsel patients on abortion (2.3 ± 1.1). Students also overwhelming thought that NYIT COM should include more information about contraception and abortion during their first- and second-year curriculum (87% Yes, 6% No, 7% Don’t know/Unsure) and during the third-year core Ob/Gyn clerkship (81% Yes, 8% No, 8% Don’t know/Unsure). There were no significant differences between religious affiliation of clerkship site nor between campus location for any questions regarding the adequacy of training.
Discussion
Overall, NYIT COM medical students felt more competent in areas of contraceptive care compared to abortion care. Religious affiliation of the clerkship site did affect Ob/Gyn clerkship training and outcomes. Students at faith-based sites tended to observe less contraceptive care compared to those at non-faith-based sites. Concomitantly, self-perceived competency in contraceptive counseling for students at faith-based sites was lower than that of students at non-faith-based sites. This shortfall was particularly apparent in students who attended Catholic-affiliated clerkship sites (Figs. 1 and 2). Clerkship religious affiliation had less of an effect on students’ observations of, and self-perceived competency in, abortion care. Overall competency in abortion-related topics was low across all clerkship sites. Though in some key areas of abortion care, students at non-faith-based sites still observed more and perceived themselves as more competent (Figs. 1 and 2). Despite overall low scores on the objective knowledge questions, students showed higher competency in contraception topics than in abortion topics. Our results suggest a shortfall in family planning training, particularly in contraceptive care at faith-based, and particularly Catholic, sites and in abortion care overall. Indeed, nearly half of students (42.3%) at Catholic-affiliated sites observed none of the listed contraception or abortion care topics during their Ob/Gyn clerkship compared to just 1.9% at non-faith-based sites. As expected, few differences in clerkship outcomes existed between campus sites. Our data also show that students desire more family planning training at both the preclinical and clinical level.
Objective outcomes of medical student training at clerkship sites of differing religious affiliation have only been documented in one prior study. Bringley et al.11 found that students who performed their clerkships at Catholic sites displayed significantly lower contraception Objective Structured Clinical Exam scores compared to peers at non-faith-based sites. This is consistent with the results regarding contraceptive care observations and competency herein.
Differences in family planning competency between faith-based and non-faith-based sites have also been seen at the residency level12,14,15. Residents who completed their training at faith-based hospitals were less satisfied with their training, and less competent, in contraceptive and abortion care than residents in non-faith-based programs14,15. Residents at Catholic programs also spent more time post-residency gaining the family planning training needed to meet the competency of their peers14. Catholic residency programs specifically, even when compared to other faith-based programs, also displayed poor abortion training. Nationwide, 47% of residency directors at Catholic programs reported poor abortion training compared to 0% at other faith-based residency locations; however all faith-based residencies reported adequate contraceptive training12. Thus the effect of religious affiliation on family planning training appears to exist, to varying extents, at all medical training levels.
Regardless of religious affiliation, the trend shown here that training in contraception care was more comprehensive than in abortion care appears to be consistent across many studies. This trend has been documented in opinions of family planning curriculum adequacy at both the medical school2,6 (and herein) and residency level12. Indeed nearly 17% of medical schools report no formal education regarding abortion in either preclinical education or third-year Ob/Gyn clerkships2.
When differences in outcomes between faith-based and non-faith-based clerkship sites existed, those sites affiliated with the Catholic church typically had the lowest outcomes. The likely explanation for this is that Catholic hospitals are expected to follow the ERDs which contain many restrictions and regulations on contraceptive and abortion care7. Although these directives are applied to all Catholic-affiliated hospitals and practices, previous research has shown inconsistencies in the adherence to these policies14. Indeed, that students witnessed certain types of abortion and contraceptive care at Catholic sites at all, support this previous finding. Although the ERDs and religiously based restrictions resulting from them likely explain the lower competency seen for students in some family planning topics at Catholic clerkship sites, it does not address why students at Jewish and Protestant sites also show lower competency in some areas. While less is known regarding policy at non-Catholic healthcare sites, religiously based restrictions on family planning care have been documented at both Protestant and Jewish health care facilities8,9. However, restrictions at Protestant and Jewish facilities appear to be less uniform and expansive than those at Catholic health care sites8,9,10,12. Indeed, this mirrors our data in that students at Jewish and Protestant clerkship sites observed, and had self-perceived competency in, contraceptive and abortion care at levels that are intermediate to students at Catholic and non-faith-based sites. Whether the somewhat less comprehensive training at these sites is a result of lower levels of restrictive policy compared to Catholic-affiliated sites, may be due to an unrelated effect such as the overall quality of the clerkship site (see ‘Strengths and Limitations’ below), or any other factor, remains to be explored. It should be noted however that differences between Jewish/Protestant sites and non-faith-based sites were less consistent than those between Catholic and non-faith-based sites. Regardless, non-faith-based hospitals have, for nearly all outputs, higher scores than faith-based hospitals.
Addressing the differences in Ob/Gyn clerkship outcomes shown here may require medical schools to implement supplemental training to meet curricular standards. Research has shown that supplemental didactive sessions dedicated to contraceptive and abortion care result in both increased knowledge of, and comfort discussing, these topics at both the medical student16 and resident level17. Implementation of supplemental family planning training outside of clerkship sites may also become more imperative in light of recent legal turmoil following the Supreme Courts 2022 Dobb’s decision18. Increasing numbers of state-level restrictions regarding contraception and abortion are likely to further impede medical student training19. Without additional mechanisms to ensure family planning competency, the differences in family planning training shown here are likely to become more pronounced.
While our results show differences in some clerkship outputs during medical school, it remains unknown how this shortfall in training may impact patient care. Ob/Gyn residents who reported dissatisfaction with their family planning training at faith-based programs reported delayed competency in many areas of family planning and a hesitancy to provide some family planning services post-residency compared to their peers at non-faith-based programs14. Thus poor medical student training in family planning topics may result in a hesitancy to provide these types of care in the future. Limiting exposure to family planning care may also inhibit development of other aspects of training as well. For instance, exposure to clinical abortion training has been shown to improve attitudes regarding abortion and increase the understanding of the psychosocial context of patients seeking abortions at both a resident and medical student level20,21. Arming medical students with a comprehensive knowledge of family planning not only allows them to better counsel and treat their patients on these topics, but also fosters a humanistic understanding of patients.
Some limitations exist in our study. First, there may also be a self-selection bias in who completed this survey based on clerkship experience or passion regarding family planning access and training. Indeed, women completed the survey at about twice the rate of men (Table 1). However, it is unlikely that this affected our findings given that gender was not a significant factor in any of linear models of self-perceived competency (see Methods). Second, this study has a somewhat low response rate at a single institution. However, data on the effect of faith-based clerkship affiliation on family planning training is extremely limited. Given the large population of students at NYIT COM, the absolute number of survey participants is on par with, or greater than, other studies looking at this effect12,14. However, the sample size of some individual categories is quite low (e.g. n = 7 for Protestant sites), limiting the conclusions which can be drawn from these smaller groups. In addition, though this study focuses on only one institution, NYIT COM is unique in having two campuses in different regions of the United States. At both campus sites, students perform their Ob/Gyn clerkships at multiple regional locations. Thus, our data represents 28 total clerkship sites (OW: 15; JB: 13). Our results are therefore somewhat robust across a variety of locations. This does however raise a subsequent limitation regarding the inconsistency in quality between clerkship sites. Some clerkship sites may simply be of higher quality than others, and currently we have no data with which to control for this effect. Only additional information on other medical schools and clerkship locations can help to resolve these limitations.
Medical students who train at faith-based clerkship sites, particularly Catholic sites, show lower self-perceived competency in, and observations of, contraceptive care compared to their peers at non-faith-based sites. Overall self-perceived competency in, and observations of, abortion care was low regardless of clerkship site, though in some areas of abortion care students at non-faith-based still showed higher outputs than peers at faith-based-sites. To provide comprehensive family planning care to future patients, additional training in contraception and abortion should be provided throughout medical school and is highly desired by medical students.
Methods
Study sample
Ethical approval was obtained by the NYIT Institution Review Board, who determined this project to be exempt (BHS-1839). A survey was created to assess three main outcomes following the third-year Ob/Gyn clerkship: 1) student observations regarding contraception and abortion training during the clerkship, 2) self-perceived competency in contraception and abortion counseling confidence, ability, and knowledge following the clerkship, and 3) objective knowledge about abortion and contraception, and perceived importance and adequacy of training in these topics. The survey instructed students that the term ‘abortion’ as used in our questions included both medical and surgical abortions, but not spontaneous abortions. This nomenclature will be utilized when describing our results. The survey was distributed through REDCap22,23 to all students in the NYIT COM classes of 2023 and 2024 at both the Old Westbury, New York (OW) and Jonesboro, Arkansas (JB) sites. At both sites third-year students rotated to one of a number of regional hospitals and/or outpatient clinics selected based on either a matching system (OW and JB) or through application to specific sites directly (OW). Both campus sites followed the same learning objectives and followed a common educational curriculum for the Ob/Gyn clerkship, including didactics and supplemental online modules, cases, and questions. One minor difference between sites was that at JB, some students performed their clerkship at outpatient clinics not associated with a hospital, whereas at OW (and for most students at JB) any outpatient clinic work was performed at clinics associated with their clerkship hospital. At the time of invitation, all students had completed their core third-year Ob/Gyn clerkship. Subjects provided informed consent prior to completing the survey and all procedures herein followed NYIT and all other relevant guidelines and regulations.
Survey mechanism
Student observations during the clerkship were assessed using eight statements regarding a topic of care students may have witnessed during their Ob/Gyn clerkship. Two were specific to contraception training, six were specific to abortion training, and a ninth choice was “None of the above”. To assess self-perceived competency in patient counseling on contraception and abortion, students were asked seven Likert-scale questions (1, strongly disagree; 5, strongly agree) regarding their perceived abilities following the Ob/Gyn clerkship. Finally, objective knowledge of contraceptive and abortion care was assessed via eight multiple-choice questions (full question text and answer choices in Supplementary Note 1). All topics of care, statements, and questions regarding abortion were taken or adapted from Gardner et al.24, and those regarding contraception were developed using the APGO guidelines1. Students were asked an additional four Likert-style questions regarding their perspectives on the adequacy of the contraceptive and abortion training they received. Finally, students were asked two Yes/No-style questions regarding whether more family planning information should be included in their preclinical and clinical curriculum.
Students were additionally asked demographic data including their class year, gender, self-described racial identity, religion, medical school name and location, clerkship name and location, and the religious affiliation of their clerkship site, if known. Prior to data analysis, each response was checked, and the religious affiliation of the clerkship site verified, and corrected if necessary, by the researchers using public record information of the clerkship sites. This was done as students were not always aware if the clerkship site had a religious affiliation. Religious affiliation was coded as either: non-faith-based (NFB), Catholic (C), Jewish (J), or Protestant (P). Here, Protestant includes all Protestant denominational families, including Methodist and Baptist hospitals. This was done in part for practical reasons, as hospitals belonging to any Protestant religions were a minority of our data. Other religious affiliations were presented in the survey, as well as an option to specify an ‘Other’ religion, however, options beyond the four above yielded no responses.
Statistical analysis
To first determine if students self-selected into faith-based clerkship sites based on either student religious identity or gender, Fisher’s exact tests were used to test for differences in student characteristics among clerkship site religious affiliation. For each characteristic (student religious identity and gender), four tests were run to determine if there were 1) differences in the student population between faith-based and non-faith-based sites for the whole sample, 2) differences in student characteristics among the four categories (NFB, C, J, P) of clerkship site for the whole sample, 3) or differences among the four categories (NFB, C, J, P) of clerkship site for each campus site individually.
Fisher’s exact tests were then used to test whether the number of students who observed a topic of contraceptive/abortion care differed between the four categories of religious affiliation. Post-hoc pairwise Fisher’s exact tests were then performed to investigate significant differences in each observational topic between specific religious affiliation categories. Linear models were used to compare outcomes between clerkship affiliations for the Likert-style questions as well as the objective knowledge questions. A linear model was constructed for each variable under consideration with religious affiliation set as a fixed effect. For these analyses, campus site was also included as a fixed effect. Significant differences between religious affiliations, and between sites, were determined using Tukey pairwise comparisons for linear models and family-wise error rates corrections25. For all Likert-scale questions, an additional linear model was constructed which also incorporated student religious identity and gender as factors. This was to determine if either of these had a significant effect on self-perceived competency or adequacy of training. However, in none of these models did student religious identity or gender have a significant effect, and in all cases the simpler model excluding these factors performed better as determined by lower Akaike Information Criterion values. Thus, only the simpler, better-performing models excluding these factors are presented. All data analysis was performed in R version 4.2.226 with some tests utilizing the package ‘multcomp’27.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Hampton B. S., Cox S. M., Craig L. B. et al. APGO Medical Student Educational Objectives, 11th Edition https://apgo.org/page/msostudent (2019).
Espey, E., Ogburn, T., Chavez, A., Qualls, C. & Leyba, M. Abortion education in medical schools: A national survey. Am. J. Obstet. Gynecol. 192, 640–643. https://doi.org/10.1016/j.ajog.2004.09.013 (2005).
Espey, E., Ogburn, T., Leeman, L., Nguyen, T. & Gill, G. Abortion education in the medical curriculum: A survey of student attitudes. Contraception 77, 205–208. https://doi.org/10.1016/j.contraception.2007.11.011 (2008).
Smith, K. G., Gilliam, M. L., Leboeuf, M., Neustadt, A. & Stulberg, D. Perceived benefits and barriers to family planning education among third year medical students. Med. Educ. Online. 13, 4474. https://doi.org/10.3402/meo.v13i.4474 (2008).
Cohen, P. et al. What should medical students be taught about abortion? An evaluation of student attitudes towards their abortion teaching and their future involvement in abortion care. BMC Med. Educ. 21, 4. https://doi.org/10.1186/s12909-020-02414-9 (2021).
Guiahi, M., Maguire, K., Ripp, Z. T., Goodman, R. W. & Kenton, K. Perceptions of family planning and abortion education at a faith-based medical school. Contraception 84(5), 520–524. https://doi.org/10.1016/j.contraception.2011.03.003 (2011).
United States Conference of Catholic Bishops. in Ethical and religious directives for Catholic health care services, sixth edition. 2018. Available at: https://www.usccb.org/resources/ethical-religious-directives-catholic-health-service-sixth-edition-2016-06_1.pdf. Accessed 7 Sept 2023. (2018).
Stulberg, D. B., Dude, A. M., Dahlquist, I. & Curlin, F. A. Obstetrician-gynecologists, religious institutions, and conflicts regarding patient-care policies. Am. J. Obstet. Gynecol. 207, 73e1. https://doi.org/10.1016/j.ajog.2012.04.023 (2012).
Hasselbacher, L. A., Hebert, L. E. & Stulberg, D. B. “My hands are tied”: Abortion restrictions and providers’ experiences in religious and non-religious health care systems. Perspect. Sex Repro. H. 52, 107–115. https://doi.org/10.1363/psrh.12148 (2018).
Merner, B., Haining, C. M., Wilmott, L., Savulescu, J. & Keogh, L. A. Institutional objection to abortion: A mixed-methods narrative review. Women’s Health 19, 17455057231152372. https://doi.org/10.1177/17455057231152373 (2023).
Bringley, J., Zu, V., Javlekar, A., Daoud Yilmaz, F. & Flink-Bochacki, R. Effects of rotating at a Catholic hospital on medical student contraceptive objective structured clinical exam scores. Contraception 106, 64–67. https://doi.org/10.1016/j.contraception.2021.09.002 (2022).
Guiahi, M., Teal, S., Kenton, K., DeCesare, J. & Steinauer, J. Family planning training at Catholic and other religious hospitals: A national survey. Am. J. Obstet. Gynecol. 222(273), e1–e9. https://doi.org/10.1016/j.ajog.2019.09.012 (2020).
Eysenbach, G. Improving the quality of web surveys: The checklist for reporting results of internet e-surveys (CHERRIES). J. Med. Internet Res. 6, e34. https://doi.org/10.2196/jmir.6.3.e34 (2004).
Guiahi, M., Hoover, J., Swartz, M. & Teal, S. Impact of Catholic hospital affiliation during obstetrics and gynecology residency on the provision of family planning. J. Grad. Med. Educ. 9, 440–446. https://doi.org/10.4300/JGME-D-16-00496.1 (2017).
Guiahi, M., Westhoff, C. L., Summers, S. & Kenton, K. Training at a faith-based institution matters for obstetrics and gynecology residents: Results from a regional survey. J. Grad. Med. Educ. 5, 244–251. https://doi.org/10.4300/JGME-D-12-00109.1 (2013).
Masini, I. et al. Medical student-led implementation of preclinical abortion didactic session at a California medical school. BMC. Med. Educ. 23, 440. https://doi.org/10.1186/s12909-023-04395-x (2023).
Guiahi, M. et al. Addressing ob/gyn family planning educational objectives at a faith-based institution using the TEACH program. Contraception 83, 367–372. https://doi.org/10.1016/j.contraception.2010.07.012 (2011).
Dobbs V. Jackson Women’s Health Organization, No 19-1392, 597 US. https://www.supremecourt.gov/opinions/21pdf/19-1392_6j37.pdf (2022).
Gyuras, H. J., Field, M. P., Thornton, O., Bessett, D. & McGowan, M. L. The double-edged sword of abortion regulations: Decreasing training opportunities while increasing knowledge requirements. Med. Educ. Online. 28, 2145104. https://doi.org/10.1080/10872981.2022.2145104 (2023).
Kumar, V., Herbitter, C., Karasz, A. & Gold, M. Being in the room: Reflections on pregnancy options counseling during abortion training. Fam. Med. 42, 41–46 (2010).
Espey, E., Ogburn, T. & Dorman, F. Student attitudes about a clinical experience in abortion care during the obstetrics and gynecology clerkship. Acad. Med. 79, 96–100. https://doi.org/10.1097/00001888-200401000-00020 (2004).
Harris, P. A. et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 42, 377–381. https://doi.org/10.1016/j.jbi.2008.08.010 (2009).
Harris, P. A. et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 95, 103208. https://doi.org/10.1016/j.jbi.2019.103208 (2019).
Gardner, H., Zimmerman, M., Flanigan, M. & Baldwin, M. A comparison of medical student competency, attitudes and knowledge of abortion care after a structured clinical curriculum. Res. Sq. https://doi.org/10.21203/rs.2.22383/v3 (2020).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J. R. Stat. Soc. Ser. B Methodol. 57, 289–300. https://doi.org/10.1111/j.2517-6161.1995.tb02031.x (1995).
R Core Team. R: A language and environment for statistical computing. In R Foundation for statistical computing. https://www.R-project.org/ (2022).
Hothorn, T., Bretz, F. & Westfall, P. Simultaneous inference in general parametric models. Biom. J. 50, 346–363. https://doi.org/10.1002/bimj.200810425 (2008).
Acknowledgements
We would like to thank the Academic Medicine Scholars Program at NYIT COM for housing this project as well as Dr. S. Hoffmann, and two anonymous reviewers for their comments.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
R.N.F. and N.E.T. conceived the study. R.N.F., S.R.L., and N.E.T. designed the study. R.N.F. and N.E.T. collected and analyzed the data. R.N.F. and N.E.T. wrote the original draft of the manuscript. R.N.F., S.R.L., and N.E.T. reviewed and edited the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Feltman, R.N., Lewis, S.R. & Thompson, N.E. Family planning competency following medical school Ob/Gyn clerkships at faith-based and secular sites. Sci Rep 14, 3667 (2024). https://doi.org/10.1038/s41598-024-54304-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-54304-5
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.