Abstract
Free-text analysis using machine learning (ML)-based natural language processing (NLP) shows promise for diagnosing psychiatric conditions. Chat Generative Pre-trained Transformer (ChatGPT) has demonstrated preliminary initial feasibility for this purpose; however, whether it can accurately assess mental illness remains to be determined. This study evaluates the effectiveness of ChatGPT and the text-embedding-ada-002 (ADA) model in detecting post-traumatic stress disorder following childbirth (CB-PTSD), a maternal postpartum mental illness affecting millions of women annually, with no standard screening protocol. Using a sample of 1295 women who gave birth in the last six months and were 18+ years old, recruited through hospital announcements, social media, and professional organizations, we explore ChatGPT’s and ADA’s potential to screen for CB-PTSD by analyzing maternal childbirth narratives. The PTSD Checklist for DSM-5 (PCL-5; cutoff 31) was used to assess CB-PTSD. By developing an ML model that utilizes numerical vector representation of the ADA model, we identify CB-PTSD via narrative classification. Our model outperformed (F1 score: 0.81) ChatGPT and six previously published large text-embedding models trained on mental health or clinical domains data, suggesting that the ADA model can be harnessed to identify CB-PTSD. Our modeling approach could be generalized to assess other mental health disorders.
Similar content being viewed by others
Introduction
In recent years, artificial intelligence (AI) and related machine learning (ML) analysis strategies have provided promising new options for understanding human language and, in associated applications, improving health care by extracting novel insights from text-based datasets1,2,3. Recent advancements in the field of natural language processing (NLP) computational methods have demonstrated that algorithms can analyze human language and derive understanding similar to human cognition4. Pre-trained large language models (PLMs) refer to massive Transformer models trained on extensive datasets5. These NLP models have achieved remarkable results in understanding contextual nuances of language in written texts4. NLP methods can extract and convert unstructured textual data into structured data, usable for a variety of ML tasks including text classification.
Combined with ML models, language models have been reported as useful in the classification of psychiatric conditions. For example, the MentalBERT and Mental-RoBERTa PLMs were trained to benefit the mental healthcare research community in identifying stress, anxiety, and depression6. The mental-xlnet-base-cased7 LLM was developed to identify various mental health conditions including stress, depression, and suicide attempts. Both studies found that language representations pretrained in the target domain improve model performance on mental health detection tasks. A survey of NLP models for depression detection showed reasonable accuracy for several models8. Language analysis has also been used for detection of schizophrenia with high accuracy9.
While these models are often extensively trained on large datasets, in certain circumstances, PLMs can often be used effectively without additional training (zero-shot learning) or training with few examples (few-shot learning)4. In zero-shot learning, a model uses its existing knowledge to understand tasks on which it was not explicitly trained4. In few-shot learning, a model can make accurate predictions after being trained on a very limited dataset for a particular task4.
The Chat Generative Pre-trained Transformer (ChatGPT) large language model (LLM) functions as a conversational agent proficient in following complex instructions and generating high-quality responses in diverse scenarios. Recently, the medical community became intrigued by its capabilities after it demonstrated its proficiency in passing medical board exams10, and its potential applications in medical care are wide-ranging11,12,13. In addition to its conversational abilities, ChatGPT has demonstrated remarkable performance on various other NLP tasks, including question-answering14, even in zero- or few-shot learning scenarios4. In these scenarios, ChatGPT was applied to new tasks with no fine-tuning using no training data (zero-shot learning) or a small number of training examples (few-shot learning)4.
In the mental health domain, ChatGPT has been employed for a variety of applications15,16,17, and was able to identify a single patient with schizophrenia and recommend a treatment that aligns with current clinical standards of care18. Chat-GPT (GPT-3.5 and GPT-4) has shown significant language processing capabilities in the realm of mental health analysis. For example, the performance of ChatGPT was evaluated in detecting stress, depression, and suicidality, showcasing its strong capability of usefully assessing mental health texts15. In another project, ChatGPT was also successful for early depression detection19. The performance of ChatGPT in identifying suicide and depression suggests a promising future for PLMs for mental health15,20,21.
ChatGPT has presented promising results in the healthcare domain, including applications in healthcare that collect and analyze patients’ clinical information including diagnosis, allergies, and details of previous visits. ChatGPT and similar models have been explored in various tests and clinical deployments for natural language processing in healthcare including applications of therapeutic chatbots, diagnostic assistance, patient education, mental health screening, and clinical documentation. However, in contrast with findings that ChatGPT has shown promising results for healthcare applications, recent reviews13,22,23 report that ChatGPT has achieved only moderate performance on a variety of clinical tests. Therefore, careful scrutiny and rigorous content verification are essential when considering ChatGPT’s clinical use. This is expected because ChatGPT was not designed for clinical applications.
Large language models such as clinicalBERT24 and BioGPT25, trained on domain-specific content, outperformed ChatGPT in clinical tasks13. These conflicting findings highlight the current lack of understanding regarding whether ChatGPT can effectively be used for clinical assessments. We next describe a mental health disorder for which clinical care can benefit by the use of ChatGPT analysis of text-based data.
Each year, approximately 140 million women give birth worldwide. For approximately one-third of this population, childbirth may be a source of substantial acute stress or trauma26,27,28,29, and a significant minority will develop childbirth-related post-traumatic stress disorder (CB-PTSD)30,31. Historically, PTSD has been associated with military combat or severe sexual assault32. In recent years, however, childbirth has become increasingly acknowledged as a significant PTSD trigger30,33,34.
Of the global childbearing population, approximately 6% will manifest full CB-PTSD33, which translates to 8 + million affected women per year. Untreated CB-PTSD is associated with negative effects in the mother and, by extension, her child35,36, and these consequences carry significant societal costs37,38. Early treatment for CB-PTSD facilitates improved outcomes39. This underscores the imperative need for effective strategies that can predict the development of CB-PTSD soon after a traumatic birth. Currently, the evaluation of CB-PTSD relies on clinician evaluations, which do not meet the need for a rapid, low-cost assessment. Patients’ self-reporting of their symptoms via questionnaires may entail under-reporting due to stigma, social desirability bias, fears of infant separation, and lack of awareness that can lead to significant under-diagnoses40,41.
Alternatively, the narrative style and language that individuals use when recounting traumatic events have been suggested to provide deep insights into their mental well-being42,43,44. Research has shown that the way in which individuals remember and describe traumatic events, encompassing the language used in the narrative, is connected to the expression of their post-traumatic stress symptoms45. The words in individuals’ trauma narratives may reflect post-trauma adjustment even before deep psychological analysis occurs46.
To date, the potential of using childbirth narratives analyzed via advanced text-based computational methods and ML for early detection of individuals showing signs of traumatic stress post-childbirth has been minimally explored (e.g.,47). We previously used the embeddings of sentence-transformers PLMs to train an ML classifier for identifying women at risk for developing CB-PTSD, using childbirth narratives as the data source; the model achieved good performance (F1 score of 0.76) in identifying women at risk of CB-PTSD via classification47. However, more research is required to characterize how word usage in birth narratives indicates maternal mental health, and understanding and analyzing trauma narratives remains a research area ripe for exploration.
This paper explores the capabilities of ChatGPT and the text-embedding-ada-002 (ADA) model, both developed by OpenAI, in analyzing childbirth narratives to identify potential markers of CB-PTSD. Through the lens of ChatGPT and associated models, we aim to bridge the gap between trauma narratives and early detection of psychiatric dysfunction, offering a novel approach to identifying women at risk for CB-PTSD. To achieve this aim, we collected textual narratives of recent childbirth experiences of postpartum women. Using OpenAI’s models, we tested whether the text of narratives, alone, could be used to identify postpartum women with probable CB-PTSD. To validate the developed model, we compare its performance to six previously published PLMs that were trained on medical or psychiatric domains.
Materials and methods
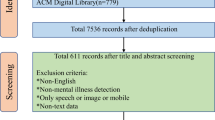
Study design
This investigation is part of a research study focused on the impact of childbirth experience on maternal mental health. Women who gave birth to a live baby in the last six months and were at least 18 years old participated by providing information about their mental health and childbirth experience through an anonymous web survey. Participants were given the opportunity to recount their childbirth stories at the end of the survey. These narratives were collected, on average, 2.73 ± 1.82 months post-childbirth (ranging from 0.02 to 8.34 months). The analyzed sample consists of 1295 women who provided narratives of length 30 words or more, which length was selected to facilitate meaningful analysis, consistent with previous work that noted limitations in analyzing shorter narratives47,48. Subject population characteristics are provided in Table 1.
Recruitment took place from November 2016 to April 2017, and from April 2020 to December 2020. Participants were recruited through hospital announcements, social media, and professional organizations. This study received exemption from the Partners Healthcare (Mass General Brigham) Human Research Committee (PHRC). All research was performed in accordance with the relevant guidelines and regulations. Implied consent was obtained from all participants; they were informed that by providing responses to the study measures, they are implying their consent to participate in the study.
Measures
We gathered narratives of childbirth in the form of open-ended, unstructured written text-based accounts, highlighting each participant’s personal and recent experience of childbirth. These narratives were procured using a free recall methodology, in which participants were asked to provide a brief account of their recent childbirth experience, focusing specifically on the most distressing elements, if any. This focus on the most distressing aspects of the birth experience aligns with standard procedures used in non-postpartum trauma sequelae research49,50.
For each participant, we assessed PTSD symptoms associated with childbirth using the Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5)34,51, a 20-item self-report measure employed to ascertain the presence and severity of DSM-5 PTSD symptoms after a designated traumatic event over the preceding month. The PCL-5 is widely recognized for its strong alignment with diagnostic assessments by clinicians and is used to establish a provisional PTSD diagnosis34,52 (i.e., a presumptive disease state without a formal diagnosis), and is validated in postpartum samples34. The clinical cutoff for this measure in non-postpartum samples is reported to be 31–3353, with a high specificity level using this cutoff34, and in accordance with this, and to reduce false negatives34, we used values of 31 + to define high scores for this study (potential CB-PTSD). The reliability of this tool was high, as indicated by Cronbach’s α = 0.934. For 14 participants, missing items in the PCL-5 assessment were coded as 0.
Narrative analysis
We tested the performance of ChatGPT via two model configurations (Model #1: zero-shot classification, and Model #2: few-shot learning) by utilizing the gpt-3.5-turbo-16k Pre-trained Large Language Model (PLM) via OpenAI’s API. The gpt-3.5-turbo-16k PLM by OpenAI is a powerful transformer model that excels in natural language understanding and generation tasks. Its variation gpt-3.5-turbo-16k has the same capabilities as the standard gpt-3.5-turbo model but can process narratives that are four times longer, of up to 16,384 tokens. In addition, we tested the performance of our developed Model #3 that utilizes the embeddings of the text-embedding-ada-002 model via OpenAI’s API. Figure 1 presents a summary of the three tested models.
The three models employed in this study via OpenAI’s API: (1) Model #1 utilizes gpt3.5-turbo-16k for zero-shot classification, (2) Model #2 utilizes gpt3.5-turbo-16k for few-shot learning, and (3) Model #3 utilizes the text-embedding-ada-002 model to train a neural network machine learning (ML) model to screen via classification for childbirth-related post-traumatic stress disorder (CB-PTSD). In the Results section, we also present the results of testing Model #3 with other large text-embedding models.
Model #1—Zero-shot classification: With no previous examples given to the model, we designed a prompt that includes a description of the task, followed by the narrative to be classified. The category associated with the model’s highest-confidence response was ‘1’ (Class 1: CB-PTSD) or ‘0’ (Class 0: No CB-PTSD) as the predicted class for the narrative. We experimented with several versions of prompts. As a summary, only the prompt that yielded the best results is presented (Table 2). Using OpenAI’s API, we sent this prompt to the gpt-3.5-turbo-16k model, which returned a response (1 or 0) to each prompt. The ‘temperature’ variable was set to 0, to make the model deterministic, i.e., always choosing the most likely next token in the sequence.
Model #2—Few-shot classification:We provided two narratives (one written by a woman with CB-PTSD, and one written by a woman without CB-PTSD) and their associated labels in a conversation format to guide the model towards the classification task (Table 2). The gpt-3.5-turbo-16k model with ‘temperature’ = 0 then used these examples to classify the expected output for the subsequent narrative. Increasing the number of examples up to 4 provided similar model performances.
Model #3—Training an ML classifier: We converted narratives to numerical vector representations (embeddings) using the text-embedding-ada-002 model by OpenAI. The model takes narratives as input and generates 1536-dimensional embedding vectors, capturing relationships between words and phrases. These embeddings serve as inputs for our developed Model #3. More specifically, we trained a neural network (NN) ML model using the generated embeddings, to classify narratives as markers of endorsement (Class 1), or no endorsement (Class 0), of CB-PTSD. Appendix A presents the four steps to build and test Model #3, summarized in Fig. A1.
Note that all of the models tested in this study rely exclusively on textual features to identify CB-PTSD.
In Step #1 of Appendix A, we label narratives associated with PCL-5 ≥ 31 as ‘CB-PTSD’ (Class 1; 190 subjects), else ‘no CB-PTSD’ (Class 0; 1105 subjects).
In Step #2, we discarded narratives with < 30 words and balanced the dataset using down-sampling by randomly sampling the majority Class 0 to fit the size of the minority Class 1, resulting in 190 narratives in each class. We constructed the Train and Test datasets as described in Step #2, resulting in 170 narratives in each class.
To identify similar or contextually relevant narratives, which involve shared characteristics, content, and context, in Step #3 we adopted the approach used in our previous work47. This approach analyzes pairs of narratives as training examples, thus substantially increasing the number of training examples. We created three sets of sentence-pairs using the Train set: Set #1: All possible pairs of sentences (C(n, r) = C(1720, 2) = 14,365) in Class 1 (CB-PTSD). Set #2: All possible pairs of sentences (14,365) in Class 0. Set #3: Pairs of sentences (28,730), one randomly selected from Class 1 and another randomly selected from Class 0. We labeled sets #1 and #2 as positive examples as they contained semantically or contextually similar pairs of sentences (i.e., either a pair of narratives of individuals with, or without, CB-PTSD). We labeled set #3 as negative examples as it contained pairs of non-semantically or non-contextually similar pairs of sentences. This data augmentation process produced 57,460 training examples in the Train set.
Next, we mapped each narrative using the text-embedding-ada-002 model into a 1536-dimensional vector. Lastly, we computed the Hadamard product (◦)54 among each of the 57,460 embedding (emb) vectors of pairs of sentences (u, v) in sets #1 to #3 of the Train set (Appendix A), such that z = (emb(u) ◦ emb(b)) (Appendix A).
Finally, using the 57,460 vectors, following the modeling approach in47, we trained a deep feedforward neural network (DFNN) model to classify pairs of sentences in sets #1 to #3 as semantically similar or not. DFNN models process information in one direction, and they enable the efficient processing of nonlinear data. Following preliminary work testing logistic regression and decision trees, which performed less accurately than DFNN, we elected to use a DFNN model. For training, we used the Keras Python library and constructed a DFNN with an input layer of 1536 neurons, 2 hidden layers of 400 and 50 neurons, and an output neuron. All layers had a rectified linear unit (ReLU) activation function, except the output neuron, which had a Sigmoid activation function. We used 50 epochs, applying the Adam optimizer with a learning rate of 1e−4, batch size of 32, and binary cross-entropy loss to monitor training performance. To avoid overfitting, we stopped training when there was no loss improvement for 3 consecutive epochs. We used 20% of the Train dataset for validation during the training process.
Steps #1 to #3 of Model #3 (Appendix A) were repeated 10 times to capture different narratives for creating an accurate representation of Classes 0 and 1.
Model evaluation In Step #4, Models #1 and #2 were evaluated on the entire dataset. Model #3 was trained on a Train set and evaluated on a Test set. This process was repeated 10 times, similar to a ten-fold cross-validation process. We tested and compared the performances of Models #1 to #3, using (1) the F1 score, which is a measure integrating precision (positive predictive value) and recall (sensitivity), and (2) the area under the curve (AUC).
Previous research reported that ChatGPT’s performance in the biomedical domain is moderate or satisfactory in various tests13. Currently, ChatGPT is not reliable for clinical deployment due to its design, which does not prioritize clinical applications13. Research indicates that specialized natural language processing (NLP) models trained on biomedical datasets remain the recommended approach for clinical uses13. Therefore, to evaluate our model, we compared the performance of our Model #3 with different embeddings generated by six PLMs that were trained on different domains, including clinical and mental health domains: all-mpnet-base-v247, mental-roberta-base6, mental-bert-base-uncased6, mental-xlnet-base-cased7, Bio ClinicalBERT24, and BioGPT25. We used the HuggingFace repository55 with Python coding to work with the evaluated PLMs. The models that we compared were evaluated using two Evaluation Methods on the dataset published in47:
Evaluation Method 1: We fine-tuned each of the six evaluated PLMs on a down-stream task of classifying narratives as CB-PTSD (Class 1) or not (Class 0). We used 30% and 70% of the data for the Test and Train split, respectively.
Evaluation Method 2: We used the developed Model #3 with embeddings of the six evaluated PLMs. Following Step 2 of Appendix A, we split the Train and Test sets 10 times (similar to a ten-fold cross-validation process).
Results
Following the data processing (Steps #1 and #2, Appendix A), for Class 1 (CB-PTSD) and Class 0 (no CB-PTSD), the mean word counts were 194.67 and 155.39, and median word counts were 158 and 106, respectively.
The results of applying Models #1 to #3 to the narrative datasets are presented in Table 3. Model #3 outperformed all other models in terms of AUC, F1 score, sensitivity.
The results from ChatGPT Model #1 and Model #2 highlight a common challenge: these models struggle to classify narratives in a specific domain of expertise because they have not been trained on it. In other words, they are pre-trained models that have not been tailored to the specialized subject matter. Model #3, however, successfully addressed this problem and outperformed the other models. It did so by using 57,460 examples and being trained on the specific classification task. This specialized training used embeddings to create a classification system designed to detect CB-PTSD. By training the model in this way, it was better suited for the specialized task of CB-PTSD detection.
As reported in Table 3 and, in particular, regarding the F1 score (0.81) and AUC (0.80), our model for CB-PTSD classification derived from birth narratives achieved overall good performance (Fig. 2).
Comparison of Receiver Operating Characteristic (ROC) curves of binary classification Models #1 to #3. The three models directly predict class labels (0 or 1) instead of probabilities. The ‘stepped’ appearance of the ROC curves is due to the models’ binary output, which allows for only 0 or 1 thresholds.
Results of Evaluation Method 1: The results show F1 score lower than 0.2 for all PLM models.
Results of Evaluation Method 2: The results show (Table 4) that our Model #3 with OpenAI’s text-embedding-ada-002 embeddings outperformed Model #3 with other embeddings of PLMs (including embeddings of PLMs trained on clinical or mental health domains) in identifying CB-PTSD using narrative data only.
Discussion
AI- and ML-based analyses of free-text data sources via natural language processing (NLP), including the ChatGPT platform, hold significant promise for improving the assessment and diagnosis of mental health disorders. However, the examination of these technologies for mental health assessment remains in early stages, with previous findings about the utility of ChatGPT being mixed, and previous reports suggesting that ML models trained on application-specific corpuses of text might be necessary for accurate model performance. This study sought to explore the performance of different variations of ChatGPT, and text embedding of different models, for the purpose of identifying probable cases of childbirth-related post-traumatic stress disorder (CB-PTSD) using brief childbirth narratives of postpartum women.
The importance of prompt and accurate screening for CB-PTSD cannot be overstated34,56, as early interventions are essential to prevent the progression of this disorder to chronic stages, complicating treatment. Despite this pressing need, standardized CB-PTSD screening protocols are not yet established57. By assessing several model variations of ChatGPT, and narrative embeddings generated by different language models, we systematically studied the capabilities and shortcomings of these models to assess maternal mental health using childbirth narratives. While Model #1 (zero-shot learning) and Model #2 (few-shot learning) that utilize the pre-trained ChatGPT model exhibited limitations, Model #3, drawing from OpenAI’s text-embeddings-ada-002 embeddings, demonstrated superior performance in identifying CB-PTSD.
Notably, Model #3’s performance surpasses both the basic implementations of ChatGPT, and other PLMs trained in clinical and mental health domains, supporting its potential to offer richer insights into maternal mental health following traumatic childbirth. Our Model #3’s capability, assessed across the analyzed dataset, achieves 85% sensitivity and 75% specificity (Table 3) in identifying CB-PTSD cases based on narrative language. Additionally, Model #3 outperforms previously established models, such as the one presented in our recent previous work47.
In contrast, as reported in Table 3, ChatGPT, in its current iteration (gpt-3.5-turbo-16k), manifests only modest results, confirming its previously reported non-specialized nature for clinical applications13,22,23. Existing evaluations, including ours, frequently categorize ChatGPT as not suitable for healthcare data analysis, with its appropriate applications mostly limited to controlled research settings13,22,23.
Our unique approach, based on unstructured childbirth narratives, introduces an innovative, patient-friendly data acquisition method that may permit the early identification of women at risk of CB-PTSD before other strategies may detect symptoms of this condition. Additionally, women sharing narratives of their childbirth experiences may avoid problems associated with social desirability bias in questionnaire responses41, and may circumvent under-reporting of symptoms due to shame or fear58. Preliminary assessments based on these narratives can identify high-risk women, facilitating timely medical intervention. Our model’s exclusive reliance on childbirth narratives as its data source presents an efficient mechanism for data collection during the vulnerable postpartum stage, circumventing potential pitfalls of using only medical records. The proposed model has the potential to fit seamlessly into routine obstetric care, and may serve as a foundation for commercial product development, facilitating its mainstream adoption. Importantly, this could improve the accessibility of CB-PTSD diagnosis, addressing socioeconomic, racial, and ethnic disparities associated with childbirth trauma59,60 by helping to identify minoritized women, who are at three times higher risk of experiencing post-traumatic stress symptoms60.
A period of six months postpartum involves the extended postpartum period, which is an important time for the establishment of chronic PTSD symptoms. However, the childbirth narratives analyzed in our study were collected, on average, 2.73 ± 1.82 months post-childbirth (range: 0.02 to 8.34 months). This indicates that our model can be used for early classification of women with and without CB-PTSD to offer an early tool for accurate identification and therefore support the possibility for early treatment.
While our results are promising, our study has several limitations. The potential enhancement of our model with data from additional sources remains unexplored; these sources can include patient self-report questionnaires, medical record data that might indicate the presence of birth trauma, and physiological assessments (e.g.,61). The sample includes women who gave birth before and during the COVID-19 pandemic62,63. This heterogeneity, including the possibility that women used different language in their narratives during the pandemic, may have affected our results and warrants replication in other postpartum samples. Additionally, while we assessed the presence of CB-PTSD using the PCL-5, which is a well validated self-report measure 34,51,64,65 and shows strong correspondence with clinical diagnostics34, clinician evaluations were not performed. A more diverse subject population is needed in future work to facilitate the development of a universally applicable tool for CB-PTSD assessment. Moreover, any use of PLM technology for mental health research warrants considerations involving the reliability of the content provided by ChatGPT and other PLMs66,67, and security and privacy concerns involving PLM analysis of medical texts66,67. Additionally, external validation is essential to further corroborate our findings using the DFNN model that employs text embeddings (Model #3).
Looking forward, we advocate for two principal enhancements to our model to identify CB-PTSD in postpartum women based on their childbirth narratives: (i) Specific fine-tuning of ChatGPT for CB-PTSD narrative language, optimizing embedding vector representation; and (ii) The integration of additional data types, including electronic medical records. Such augmentations can serve to enhance performance, improving the accuracy of computational methodologies in maternal mental health evaluation.
Conclusions
In this investigation, we examine the utility of variations of the ChatGPT pre-trained large language model (PLM), and text embeddings of different language models to assess mental health using text-based personal narratives as the exclusive data source. Harnessing advanced natural language processing (NLP) and machine learning (ML) analysis strategies, we present the potential of these methods for analyzing narratives to advance maternal mental health assessment. We find that a ChatGPT model untrained on a specific clinical task shows inadequate performance in the task of identifying childbirth-related post-traumatic stress disorder (CB-PTSD), while our model trained on the embeddings of OpenAI’s text-embeddings-ada-002 model yields the best performance to date for this task, representing good performance. With refinements and enhancements pending in future work, this textual personal narrative-based assessment strategy employing NLP analysis has the potential to become an accurate, efficient, low-cost, and patient-friendly strategy for identifying CB-PTSD in the clinic, and facilitating timely interventions to mitigate this maternal mental health disorder. The PLM analysis strategies presented here hold promise for potential use in assessing diverse additional mental health disorders, and consequently improving outcomes.
Data availability
The de-identified datasets used and analyzed in the current study are available from the corresponding author on reasonable request.
Code availability
The code associated with this study is publicly available on GitHub at https://github.com/bartala/ChatCBPTSD.
References
Wang, L. et al. Boosting delirium identification accuracy with sentiment-based natural language processing: Mixed methods study. JMIR Med. Inform. 10(12), e38161 (2022).
Liu, N., Luo, K., Yuan, Z. & Chen, Y. A transfer learning method for detecting Alzheimer’s disease based on speech and natural language processing. Front. Public Health 10, 772592 (2022).
Levis, M., Westgate, C. L., Gui, J., Watts, B. V. & Shiner, B. Natural language processing of clinical mental health notes may add predictive value to existing suicide risk models. Psychol. Med. 51, 1382–1391 (2021).
Brown, T. et al. Language models are few-shot learners. Adv. Neural Inf. Proc. Syst. 33, 1877–1901 (2020).
Brants, T., Popat, A. C., Xu, P., Och, F. J. & Dean, J. Large language models in machine translation. In Proc. 2007 Joint Conf. Empirical Meth. Nat. Lang. Proc. Computat. Nat. Lang. Learn. Prague. 858–867 (2007).
Ji, S. et al. Mentalbert: Publicly available pretrained language models for mental healthcare. Preprint at http://arxiv.org/abs/2110.15621 (2021).
Ji, S. et al. Domain-specific continued pretraining of language models for capturing long context in mental health. arXiv. Preprint at http://arxiv.org/abs/2304.10447 (2023).
Belser, C. A. Comparison of natural language processing models for depression detection in chatbot dialogues. Doctoral dissertation. Massachusetts Institute of Technology. (2023).
Fu, J. et al. Sch-net: A deep learning architecture for automatic detection of schizophrenia. Biomed. Eng. Online 20, 75 (2021).
Gordijn, B. & ten Have, H. ChatGPT: Evolution or revolution?. Med. Health Care Philos. 26, 1–2 (2023).
Sallam, M. ChatGPT utility in healthcare education, research, and practice: Systematic review on the promising perspectives and valid concerns. Healthcare 11(6), 887 (2023).
Sohail, S. S. A promising start and not a panacea: ChatGPT’s early impact and potential in medical science and biomedical engineering research. Ann. Biomed. Eng. 1–5 (2023).
Li, J., Dada, A., Kleesiek, J. & Egger, J. ChatGPT in healthcare: A taxonomy and systematic review. Comput. Meth. Prog. Biomed. 245, 108013 (2024).
Bang, Y. et al. A multitask, multilingual, multimodal evaluation of ChatGPT on reasoning, hallucination, and interactivity. arXiv. Preprint at http://arxiv.org/abs/2302.04023 (2023).
Lamichhane, B. Evaluation of ChatGPT for NLP-based mental health applications. arXiv. Preprint at http://arxiv.org/abs/2303.15727 (2023).
Sohail, S. S. et al. Decoding ChatGPT: A taxonomy of existing research, current challenges, and possible future directions. J. King Saud Univ. Comput. Inf. Sci. 35(8), 101675 (2023).
Cheng, S. W. et al. The now and future of ChatGPT and GPT in psychiatry. Psychiatry Clin. Neurosci. 77(11), 592–596 (2023).
Galido, P. V., Butala, S., Chakerian, M. & Agustines, D. A case study demonstrating applications of ChatGPT in the clinical management of treatment-resistant schizophrenia. Cureus 15(4), e38166 (2023).
Danner, M. et al. Advancing mental health diagnostics: GPT-based method for depression detection. In 2023 62nd Ann. Conf. Soc. Instr. Contr. Eng. Japan (SICE). Tsu City. (2023).
Amin, M. M., Cambria, E. & Schuller, B. W. Will affective computing emerge from foundation models and general AI? A first evaluation on ChatGPT. arXiv. Preprint at http://arxiv.org/abs/2303.03186 (2023).
Qin, C. et al. Is ChatGPT a general-purpose natural language processing task solver?. arXiv. Preprint at http://arxiv.org/abs/2302.06476 (2023).
Vaishya, R., Misra, A. & Vaish, A. ChatGPT: Is this version good for healthcare and research?. Diabetes Metab. Syndr. Clin. Res. Rev. 17, 102744 (2023).
Farhat, F. ChatGPT as a complementary mental health resource: A boon or a bane. Ann. Biomed. Eng. 1–4 (2023).
Alsentzer, E. et al. Publicly available clinical BERT embeddings. arXiv. Preprint at http://arxiv.org/abs/1904.03323 (2019).
Luo, R. et al. BioGPT: Generative pre-trained transformer for biomedical text generation and mining. Brief. Bioinform. 23, bbac409 (2022).
Sommerlad, S., Schermelleh-Engel, K., La Rosa, V. L., Louwen, F. & Oddo-Sommerfeld, S. Trait anxiety and unplanned delivery mode enhance the risk for childbirth-related post-traumatic stress disorder symptoms in women with and without risk of preterm birth: A multi sample path analysis. PLOS ONE 16, e0256681 (2021).
Thiel, F. & Dekel, S. Peritraumatic dissociation in childbirth-evoked posttraumatic stress and postpartum mental health. Arch. Women’s Ment. Health 23, 189–197 (2020).
Boorman, R. J., Devilly, G. J., Gamble, J., Creedy, D. K. & Fenwick, J. Childbirth and criteria for traumatic events. Midwifery 30, 255–261 (2014).
Jagodnik, K. M. et al. Screening for post-traumatic stress disorder following childbirth using the Peritraumatic Distress Inventory. J. Affect. Disord. 348, 17–25. https://doi.org/10.1016/j.jad.2023.12.010 (2024).
Dekel, S., Ein-Dor, T., Dishy, G. A. & Mayopoulos, P. A. Beyond postpartum depression: Posttraumatic stress-depressive response following childbirth. Arch. Women’s Ment. Health 23, 557–564 (2020).
Thiel, F., Ein-Dor, T., Dishy, G., King, A. & Dekel, S. Examining symptom clusters of childbirth-related posttraumatic stress disorder. Prim. Care Compan. CNS Disord. 20, 26912 (2018).
Dekel, S., Gilberston, M., Orr, S., Rauch, S. & Pitman, R. Trauma and post-traumatic stress disorder. Massachusetts General Hospital Comprehensive Clinical Psychiatry 2nd Edition, 380–394 (2016).
Yildiz, P. D., Ayers, S. & Phillips, L. The prevalence of posttraumatic stress disorder in pregnancy and after birth: A systematic review and meta-analysis. J. Affect. Disord. 208, 634–645 (2017).
Arora, I. H. et al. Establishing the validity of a diagnostic tool for childbirth-related post-traumatic stress disorder. Am. J. Obstetr. Gynecol. In Press. (2024). https://doi.org/10.1016/j.ajog.2023.11.1229.
Van Sieleghem, S. et al. Childbirth related PTSD and its association with infant outcome: A systematic review. Early Human Dev. 174, 105667 (2022).
Dekel, S., Thiel, F., Dishy, G. & Ashenfarb, A. L. Is childbirth-induced PTSD associated with low maternal attachment?. Arch. Women’s Ment. Health 22, 119–122 (2019).
Lyons-Ruth, K. & Yarger, H. A. Developmental costs associated with early maternal withdrawal. Child Dev. Perspect. 16, 10–17 (2022).
Luca, D. L., Garlow, N., Staatz, C., Margiotta, C. & Zivin, K. Societal costs of untreated perinatal mood and anxiety disorders in the United States. Math. Policy Res. 1 (2019).
Dekel, S. et al. Preventing posttraumatic stress disorder following childbirth: A systematic review and meta-analysis. Am. J. Obstetr. Gynecol. In Press. https://doi.org/10.1016/j.ajog.2023.12.013 (2024).
Anokye, R., Acheampong, E., Budu-Ainooson, A., Obeng, E. I. & Akwasi, A. G. Prevalence of postpartum depression and interventions utilized for its management. Ann. Gen. Psychiatry. 17, 1–8 (2018).
Jones, A. Postpartum help-seeking: The role of stigma and mental health literacy. Matern. Child Health J. 26, 1030–1037 (2022).
Vanaken, L., Smeets, T., Bijttebier, P. & Hermans, D. Keep calm and carry on: The relations between narrative coherence, trauma, social support, psychological well-being, and cortisol responses. Front. Psychol. 12, 558044 (2021).
Thiel, F. et al. Traumatic memories of childbirth relate to maternal postpartum posttraumatic stress disorder. J. Anx. Disord. 77, 102342 (2021).
Alvarez-Conrad, J., Zoellner, L. A. & Foa, E. B. Linguistic predictors of trauma pathology and physical health. Appl. Cogn. Psychol. 15, S159–S170 (2001).
Crespo, M. & Fernandez-Lansac, V. Memory and narrative of traumatic events: A literature review. Psychol. Trauma Theory Res. Pract. Policy 8, 149 (2016).
O’Kearney, R. & Perrott, K. Trauma narratives in posttraumatic stress disorder: A review. J. Traum. Stress. 19, 81–93 (2006).
Bartal, A., Jagodnik, K. M., Chan, S. J., Babu, M. S. & Dekel, S. Identifying women with post-delivery posttraumatic stress disorder using natural language processing of personal childbirth narratives. Am. J. Obstetr. Gynecol. MFM. 5, 100834 (2023).
Bartal, A. et al. Enrichrbot: Twitter bot tracking tweets about human genes. Bioinformatics 36, 3932–3934 (2020).
Booker, J. A. et al. Narratives in the immediate aftermath of traumatic injury: Markers of ongoing depressive and posttraumatic stress disorder symptoms. J. Traum. Stress. 31, 273–285 (2018).
Dekel, S. & Bonanno, G. A. Changes in trauma memory and patterns of post-traumatic stress. Psychol. Traum. Theor. Res. Pract. Policy 5, 26 (2013).
Blevins, C. A., Weathers, F. W., Davis, M. T., Witte, T. K. & Domino, J. L. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. J. Traum. Stress 28, 489–498 (2015).
Wortmann, J. H. et al. Psychometric analysis of the PTSD Checklist-5 (PCL-5) among treatment-seeking military service members. Psychol. Assess. 28, 1392 (2016).
Kruger-Gottschalk, A. et al. The German version of the Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Psychometric properties and diagnostic utility. BMC Psychiatr. 17, 1–9 (2017).
Davis, C. The norm of the Schur product operation. Numerische Mathematik. 4, 343–344 (1962).
Wolf, T. et al. HuggingFace’s transformers: State-of-the-art natural language processing. arXiv. Preprint at http://arxiv.org/abs/1910.03771 (2019).
Dekel, S. A call for a formal diagnosis for childbirth-related PTSD. Nature Ment. Health. Accepted. (2024).
Sachdeva, J. et al. Trauma informed care in the obstetric setting and role of the perinatal psychiatrist: A comprehensive review of the literature. J. Acad. Consult. Liaison Psychiatr. 63, 485–496 (2022).
Vigod, S. N. & Dennis, C. L. Advances in virtual care for perinatal mental disorders. World Psychiatr. 19(3), 328 (2020).
Chan, S. J. et al. Risk factors for developing posttraumatic stress disorder following childbirth. Psychiatr. Res. 290, 113090 (2020).
Iyengar, A. S. et al. Increased traumatic childbirth and postpartum depression and lack of exclusive breastfeeding in Black and Latinx individuals. Int. J. Gynecol. Obstetr. 158, 759–761 (2022).
Chan, S. J. et al. Validation of childbirth-related posttraumatic stress disorder using psychophysiological assessment. Am. J. Obstetr. Gynecol. 227, 656–659 (2022).
Mayopoulos, G. A. et al. COVID-19 is associated with traumatic childbirth and subsequent mother-infant bonding problems. J. Affect. Disord. 282, 122–125 (2021).
Mayopoulos, G. A., Ein-Dor, T., Li, K. G., Chan, S. J. & Dekel, S. COVID-19 positivity associated with traumatic stress response to childbirth and no visitors and infant separation in the hospital. Sci. Rep. 11(1), 13535 (2021).
Forkus, S. R. et al. The Posttraumatic Stress Disorder (PTSD) Checklist for DSM–5: A systematic review of existing psychometric evidence. Clin. Psychol. Sci. Pract. 30, 110 (2023).
Orovou, E., Theodoropoulou, I. M. & Antoniou, E. Psychometric properties of the Post Traumatic Stress Disorder Checklist for DSM-5 (PCL-5) in Greek women after cesarean section. PLOS ONE 16, e0255689 (2021).
Singh, O. P. Artificial intelligence in the era of ChatGPT—Opportunities and challenges in mental health care. Indian J. Psychiatr. 65, 297 (2023).
Garg, R. K. et al. Exploring the role of ChatGPT in patient care (diagnosis and treatment) and medical research: A systematic review. Health Promot. Perspect. 13(3), 183–191 (2023).
Acknowledgements
A.B. was supported by the Data Science Institute (DSI) at Bar-Ilan University. K.M.J. was funded by a Mortimer B. Zuckerman STEM Leadership Program postdoctoral fellowship. S.D. was funded by National Institutes of Health (NIH) National Institute of Child Health and Human Development (NICHD) grants R01HD108619, R21HD109546, and R21HD100817.
Author information
Authors and Affiliations
Contributions
A.B. provided guidance on the artificial intelligence analyses, developed the machine learning models, performed analyses, generated all figures and Tables 2–4, prepared all supplementary materials, and wrote and revised the manuscript. K.M.J. wrote and revised the manuscript. S.J.C. contributed to data collection and performed descriptive data analysis, prepared Table 1, and contributed to revising the manuscript. S.D. is the principal investigator of the larger study. She collected data, developed the project concept, wrote and revised the manuscript, and supervised the project. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bartal, A., Jagodnik, K.M., Chan, S.J. et al. AI and narrative embeddings detect PTSD following childbirth via birth stories. Sci Rep 14, 8336 (2024). https://doi.org/10.1038/s41598-024-54242-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-54242-2
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.