Abstract
Urinary tract infection (UTI) caused by spinal cord injury (SCI) can have significant morbidity. There is currently a lack of relevant data in China. This study explores incidence and risk factors of UTI in hospitalized patients with SCI in China, and will help healthcare professionals to make informed clinical decisions to reduce the incidence of UTI. This retrospective study analyzed the medical records of patients with SCI who were hospitalized at three campuses of a hospital in central China between August 2014 and August 2023. The files of patients with SCI were reviewed for demographics and clinical characteristics. Logistic regression analysis was performed to identify risk factors associated with UTI. A total of 538 patients were included in this study. The incidence of UTI was 49.8%. Sex, hypoproteinemia, urinary incontinence, bladder irrigation, timing of rehabilitation, duration of indwelling urinary catheter were risk factors of UTI. The implementation of specific preventive measures is anticipated to result in a decrease in the occurrence of UTI among individuals with SCI, consequently enhancing their overall quality of life and prognosis.
Similar content being viewed by others
Introduction
The global incidence of spinal cord injury (SCI) ranges from 3.6 to 195.4 per million people and is increasing annually1. Urinary tract infection (UTI) is the most common infection in patients with SCI and a common cause of hospitalization2. UTI affects the patient's rehabilitation because it usually increases spasticity and may even require bed rest as well as prolonged hospitalization3. In a population-based survey conducted in Switzerland, 59% of patients with SCI developed UTI complications with 41% describing the complications as moderate or severe4. UTI reduces patients' quality of life, and can lead to hydronephrosis, acute kidney injury, urologic tumor development, sepsis, or renal failure, all of which can severely reduce patients' lives5,6.
Due to loss of sensation, the signs and symptoms of UTI in patients with SCI, such as urinary frequency, urgency, and difficulty in urination are not specific. They sometimes may only have objective symptoms, such as chills and fever, leading to an often inability to make an early diagnosis7. Antibiotics can be efficacious in prevention and treatment; however repeated administration of antibiotics increases the risk of multi-drug resistance8.
With the development of rehabilitation medicine technology in recent years, catheterization techniques and materials for patients with SCI have been significantly improved, and urinary problems have been systematically managed. However, the incidence of UTI in patients with SCI is still high. A recent literature review, reported that UTI is common in patients with SCI, with a reported prevalence of 10–68% globally9. Different countries have reported different incidences of UTI suggesting that the incidence varies widely depending on the medical setting and patient characteristics. As a developing country with a large population, UTI in patients with SCI in China is of concern. However, China lacks a national SCI registry system. Therefore, there were no definitive results on the incidence of UTI in Chinese SCI patients. There were no previous reports on the analysis of risk factors associated with UTI in Chinese patients with SCI either. Exploring the associated risk factors will help healthcare professionals to make informed clinical decisions to effectively prevent and manage UTI in patients with SCI. Therefore, this retrospective study was conducted to investigate the incidence of UTI in hospitalized Chinese patients with SCI and to analyze the factors affecting the occurrence. The primary objective was to gain insight into the present condition and requirements of medical and nursing care for UTI in this specific patient population, with the ultimate aim of devising a more targeted approach for disease intervention.
Material and methods
Study population
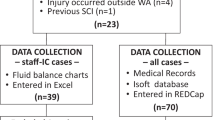
We analyzed the medical records of patients with SCI hospitalized in the Department of Rehabilitation Medicine, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, China, between August 2014 and August 2023. This is a Grade 3A general hospital located in the central region of China, encompassing three medical centers dispersed across various regions of Wuhan. Grade 3A hospitals are the highest level of hospitals in mainland China, and are hospitals above the regional level that provide high-level medical and health services to multiple regions and perform higher education and scientific research tasks. Tongji Hospital has more than 7000 beds and treats patients from all over the country. The number of patients with SCI treated annually is over 200, and the admission rate is over 60%. The rehabilitation department of this hospital holds the sixth position within China's rehabilitation sector and functions as the Hubei Provincial Rehabilitation Quality Control Center. The data from this study may represent a better level of SCI management in China and may be generalizable to SCI management in other parts of China. The study included patients diagnosed with SCI, according to the International Classification of Diseases Version 10 (ICD-10: T09.300). Figure 1 shows the flow chart for sampling.
The Ethics Committee of Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology reviewed and approved this study (Ethics No. TJ-IRB202402063). Our study has been performed in accordance with the Declaration of Helsinki. We confirm that all methods were performed in accordance with the relevant guidelines and regulations. The need for individual informed consent for this retrospective study was waived.
Patient and public involvement statement
Patients or the public were not involved in the design, or conduct, or reporting, or dissemination plans of our research.
Exclusion criteria
Age < 18 years.
Patients in spinal shock: During spinal shock, the patient's nervous system is in an unstable state, and many ratings are inaccurate10. Additionally, there are differences in treating the disease during spinal shock compared to managing the non-shock period11. These factors can impact the accuracy of the study.
Patients with congenital malformations of the urinary system or polycystic kidney disease: UTI are more likely to occur in this condition due to structural abnormalities in the urinary tract or impaired kidney function12. These factors can impact the accuracy of the study.
Patients with pregnancy, tuberculosis, tumors, delirium, severe cardiopulmonary and cerebral diseases: Many changes occur in the patient's body during pregnancy, including hormone levels and metabolic rate. Tumors may cause an abnormal response of the immune system. Severe cardiopulmonary and cerebral diseases encompass a range of conditions such as myocardial infarction, heart failure, respiratory failure, stroke, craniocerebral injury, and other conditions that can lead to impaired heart, lung, and brain function that may affect the patient's physiological state and metabolic function13. Therefore, to ensure the accuracy and reliability of the results, these factors that may affect the results were excluded from this study.
Variables and definitions
Variables were selected based on published studies, accessibility, and professional knowledge. Variables included were: age, sex, etiology, injury completeness, neurological level, hypoproteinemia, urinary incontinence, bladder irrigation, timing of rehabilitation, duration of indwelling urinary catheter, and Barthel Index scores14,15,16,17.
UTI were defined in accordance with the International Spinal Cord Society Urinary Tract Infection Basic Data Set18. UTI is defined as the new onset of symptoms accompanied by laboratory findings (bacteriuria, leukocyturia, and positive urine culture). Unlike UTI in people without other medical conditions, signs and symptoms of suspected UTI in people with SCI include fever, the first occurrence of urinary incontinence or increased frequency of urinary incontinence (including leakage of urine between the indwelling catheter and the urethra), increased spasmodic state, Suprapubic pain, malaise, hematuria without other causes, lethargy or sensory disturbances, cloudy urine with increased odor, discomfort or pain in the renal/bladder area, difficulty in urinating, or abnormal autonomic reflexes18,19.
The extent of injury was based on the American Spinal Injury Association impairment scale (AIS). Serum albumin < 30 g/L was considered hypoproteinemia. Symptoms or urodynamic studies were used to diagnose urinary incontinence. Bladder irrigation was determined by whether bladder irrigation had been performed before UTI. The timing of rehabilitation was calculated from the onset of injury to the time the patient started the rehabilitation program. (Including exercise training, physical therapy, bladder management, etc.). Duration of indwelling urinary catheter stands for the total number of days of voiding with an indwelling catheter before the first UTI in a patient with SCI.
Statistical analysis
Microsoft Excel (version 16.0) and IBM SPSS Statistics (version 23.0) were used to perform statistical analysis. Data entry was done independently by two different researchers. One researcher entered the collected data into Excel spreadsheets, while the other researcher checked the entered data to eliminate bias and data entry errors, ensuring the comprehensiveness and accuracy of the data. Categorical nominal variables were presented as percentages and analyzed using Pearson’s chi-square test or Fisher’s exact test. Since all continuous variables in this study were non-normal distributed, they were presented as medians and interquartile ranges (IQR) And the nonparametric test (Mann–Whitney U test) was used for analysis. .Logistic regression analysis was used to determine the factors affecting UTI, and odds ratios (OR) and 95% confidence intervals (CI) were calculated. P-value < 0.05 was considered statistically significant; P-value < 0.01 was considered highly statistically significant.
Ethics approval and consent to participate
This study was reviewed and approved by the Ethics Committee of Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology (Ethics No.TJ-IRB202402063). Our study has been performed in accordance with the Declaration of Helsinki. We confirm that all methods were performed in accordance with the relevant guidelines and regulations.
Results
This study comprised a sample size of 538 participants, with UTI occurring in 268 subjects. Thus, the incidence of UTI was 49.8%. Table 1 shows the characteristics of the patients. Among the patients, 78.6% (n = 423) were men and the median age was 45 years (IQR 21). The primary cause of SCI was traffic accidents (n = 137). The distribution of completeness, based on the AIS, revealed that grade A, B, C, and D injuries constituted 43.8% (n = 235), 22.3% (n = 120), 22.5% (n = 121), and 11.4% (n = 61) of the total cases, respectively. There were 107(19.9%) patients had urinary incontinence and 172(32.0%) patients underwent bladder irrigation. The median number of days between injury and the start of rehabilitation of the participants was 21 days (IQR 14). The median duration of the indwelling urinary catheters was 34 days (IQR 21). The median Barthel Index scores for the patients was 15 (IQR 15).
Table 2 presents the symptoms and laboratory findings of SCI patients with UTI This study identified the prevailing symptoms observed in patients with SCI during UTI episodes, namely fever, hematuria, and turbid urine. Additionally, a subset of patients reported suprapubic pain, new onset urinary incontinence, and scrotal pain. The most common laboratory findings were leukocyturia, positive urine culture and bacteriuria. Table 3 shows the distribution of microorganisms isolated from urine cultures of SCI patients with UTI. It can be noticed that the most common microorganisms were E. coli.
Table 4 and Fig. 2 shows the results of multivariable regression analyses. We found that sex (OR = 1.772; 95% CI 1.03–3.048), hypoproteinemia (OR = 3.891; 95% CI 2.144–7.063), urinary incontinence (OR = 5.498; 95% CI 3.106–9.732), bladder irrigation (OR = 1.642; 95% CI 1.04–2.594), timing of rehabilitation (OR = 1.037; 95% CI 1.022–1.052), duration of indwelling urinary catheter (OR = 1.038; 95% CI 1.016–1.06) were risk factors of UTI. We further performed stratified analysis by sex (Table 5). Male have a higher rate of UTI than female, and they also have indwelling urinary catheters for a longer period of time compared to female.
Figure 3 and Table 6 characterize the annual incidence of UTI and associated factors for each year from 2014 to 2023. As can be seen in Fig. 3, there is a decreasing trend in incidence rates. Table 6 shows that the proportion of hypoproteinemia and urinary incontinence are also decreasing. Notably, since 2020, no bladder irrigation has been performed on patients. At the same time, the duration of the indwelling catheter was progressively shorter, and rehabilitation interventions for patients were earlier (Fig. 3).
Discussion
Since China is an important developing country, the study aimed to investigate the prevalence and risk factors of UTI in Chinese hospitalized patients with SCI. Given the significance of UTI prevention in the medical management of patients with SCI, this study holds substantial value. The findings presented herein can aid healthcare teams in acquiring a more comprehensive comprehension of the specific needs of this vulnerable population in China and in implementing appropriate preventive strategies to alleviate the incidence of UTI and associated complications.
Incidence of UTI in patients with SCI
A recent literature review has indicated that the global prevalence of UTI in patients with SCI ranges from 10 to 68%9. This prevalence demonstrates significant variation across different countries, implying that the incidence of UTI is heavily influenced by the healthcare environment and patient-specific factors. In our own study, we observed a prevalence of 49.8%. The findings from these reports and the outcomes of this study indicate that UTI remain prevalent among individuals with SCI and exhibit a higher incidence rate in China. This suggests the need for further development of targeted measures to effectively mitigate the occurrence of UTI.
The prevalent symptoms of UTI in the general populace encompass urinary frequency, urgency, dysuria, and low back pain. Nevertheless, these symptoms may not be readily discernible to individuals with SCI, who may encounter difficulties in accurately articulating their discomfort. The findings of this study indicate that fever is the most common and predominant symptom (> 90%) observed among SCI patients during UTI episodes. Consequently, healthcare professionals should be alert to the possibility of a UTI when a patient presents with fever7.
The strains and drug resistance observed in the urine of patients with SCI may exhibit variations compared to those found in able-bodied patients20. Urine culture tests serve as a valuable tool for healthcare professionals in confirming the diagnosis of UTI and determining appropriate and efficacious treatment strategies. However, the present study reveals that urine culture was conducted in only 76.1% of patients with UTI, indicating a lack of appropriate utilization in the management of patients with SCI in China21. Because urine culture testing allows for early diagnosis, guides treatment, and monitors efficacy, it should be performed when a patient develops new symptoms and suspects a UTI. Based on the test results, we can guide the use of antibiotics. To develop a targeted UTI prevention and treatment program, we also collected microbial distributions from urine cultures. As can be seen in Table 3, the most common microorganism was E. coli (38.7%), followed by Klebsiella spp. (17.0%) and Enterococcus spp. (14.6%). This result is similar to the results of other studies22,23.
Relationship between sex and UTI
This study showed that sex is a factor that affects UTI. This is inconsistent with previous studies, which reported that sex was not associated with UTI14. There is a view that women are underrepresented among patients with SCI, therefore, it is difficult to compare the effect of sex on complications, including UTI24. Therefore, the findings regarding sex factors on SCI are limited to making incomplete comparisons. Additionally, we conducted a stratified analysis based on sex, revealing that males exhibited a prolonged duration of indwelling catheters compared to females across all identified UTI risk factors. A Korean study also suggests that this may be a result of sex being associated with a higher percentage of male patients having indwelling catheters than female patients, instead of a correlation between UTI and sex15. There are significant sex-stratified differences in bladder management after SCI, which should be noted by healthcare professionals.
Relationship between hypoproteinemia and UTI
Our study showed that hypoproteinemia is a risk factor for UTI in patients with SCI. Human serum albumin is a unique multifunctional protein provides essential fatty acids for neural membrane repair, induces neuroprotection and suppress inflammatory responses after SCI25,26,27. A decreased albumin indicates a reduced ability to resist infection27,28. Hypoproteinemia affects the repair of the spinal cord and the immunity of the body, leading to an increased incidence of UTI27. In this study, the prevalence of hypoproteinemia in Chinese patients with SCI was as high as 18.6% (n = 100). These data suggest healthcare professionals should be concerned about hypoproteinemia while preventing and treating UTI in patients with SCI. Regular blood tests play a crucial role in the prevention of hypoproteinemia among patients with SCI, while ensuring adequate protein supplementation serves as the primary preventive measure against hypoproteinemia28.
Relationship between urinary incontinence and UTI
Like the findings of previous studies, this study showed that urinary incontinence is a risk factor for UTI in patients with SCI29. In this study, the prevalence of urinary incontinence in Chinese patients with SCI was as high as 19.9% (n = 107). Urinary incontinence in patients with SCI is often caused by overactivity of the forced urinary muscles30. Overactivity of the detrusor muscle may lead to mucosal ischemia, and inadequate tissue perfusion affecting the natural protection of the mucosa by blood and reducing the release of inflammatory cells, thus promoting the proliferation of microorganisms31. Nevertheless, it is imperative to acknowledge that this study is deficient in terms of comprehensive data regarding the absence of urodynamic evaluations among Chinese patients with SCI, as such examinations are not routinely conducted. Consequently, the incapacity to ascertain the specific classification of neurogenic bladder in these patients represents a limitation of this study. This underscores the significance of conducting urodynamic assessments to determine the type of bladder dysfunction in patients afflicted with neurogenic bladder within our clinical practice. Furthermore, early identification of the etiology of urinary incontinence in individuals with SCI and the provision of targeted interventions to effectively manage incontinence symptoms assumes paramount importance.
Relationship between bladder irrigation and UTI
This study showed that bladder irrigation is a significant risk factor for UTI in patients with SCI. Excessive bladder irrigation can produce mechanical damage to the bladder wall, damaging the bladder mucosa and increasing the risk of infection32. It is believed that bladder irrigation instead produces more pathogenic strains of bacteria and increases the risk of infection33. However, several studies have shown that effective pharmacologic bladder irrigation for specific UTI can improve treatment outcomes. Linezolid use as a bladder irrigation may be a feasible route of administration in anuric, critically ill patients with VREfm and few antimicrobial options34 Bladder irrigation with amphotericin B can improve the curative effect of fungal infection in the urinary tract35. Therefore, patients with SCI should avoid unnecessary bladder irrigation and pay attention to aseptic operations when performing bladder irrigation to reduce the risk of UTI.
Relationship between timing of rehabilitation and UTI
This study showed that the timing of rehabilitation is a risk factor for UTI in patients with SCI. Early comprehensive rehabilitation treatment builds a reflex bladder, establishes regular filling and emptying, induces the formation of an autonomous voiding rhythm, and restores the patient's autonomous voiding function36. Early psychological rehabilitation interventions can help patients to understand neurogenic bladder correctly, build confidence in overcoming the disease, reduce disease stigma, improve patient cooperation, and avoid UTI37. This prompts healthcare professionals to initiate early rehabilitation in order to mitigate the probability of UTI.
Relationship between duration of indwelling urinary catheter and UTI
The findings of this study indicate a positive correlation between the duration of indwelling catheterization and the increased probability of developing UTI. Previous study have shown that patients have a 3–7% risk of developing a catheter-associated UTI, per extra day the indwelling urinary catheter remains in place38. EAU Guidelines on neurogenic lower urinary tract dysfunction state that indwelling transurethral catheterization should be avoided because it is a risk factor for UTI and significant long-term complications39. If the patient's vital signs are unstable or there are other compound injuries, the main focus is to save life and save other organ functions, and a urinary catheter can be temporarily placed. There is no consensus on when to remove the catheter40. Nevertheless, based on the extensive body of evidence elucidated above, it is strongly recommended that healthcare professionals expedite the removal of indwelling catheters for the optimal benefit of the patient.
The incidence and management of UTI in various time periods
Between 2014 and 2023, there is a decreasing trend in the incidence of UTI, which can be attributed to alterations in the healthcare approach towards managing the condition in individuals with SCI. First of all, it is clear that from 2020 no bladder irrigation was performed, which contributed to reduce the incidence of UTI. At the same time, a reduction in the percentage of patients with urinary incontinence and hypoproteinemia can be observed. In addition, rehabilitation interventions became earlier and urinary catheter retention became shorter. These factors collectively contribute to a decrease in the occurrence of UTI. All of these data suggest that the healthcare professionals in the hospitals of this study are more scientific and correct in managing the disease in patients with SCI. Therefore, it is very important to study the risk factors of UTI and manage the disease correctly. In China, the prevalence of UTI in SCI patients is as high as 49.8%, in which case healthcare professionals should pay more attention to the needs of the disease and learn the proper disease management in order to prevent the occurrence of UTI.
Limitation
This study is a retrospective analysis, which inevitably has many limitations. Firstly, since retrospective studies are based on existing data, there may be bias in the data collected or certain variables may be affected by other factors that may bias the results of the analysis, and therefore there may be problems such as information bias. Secondly, as retrospective studies usually involve the analysis of existing data and information, the choice of researcher may affect the conclusions. Although two researchers were used to collect data in this study, the issue of selection bias in retrospective studies is still unavoidable. Third, urodynamics is an important test for patients with SCI for determining bladder type, and as a reference for bladder management and rehabilitation. Unfortunately, because urodynamics is not widely used in Chinese SCI patients, only some patients in this study obtained urodynamic results, which is a non-negligible limitation. It is recommended in clinical work to improve the urodynamics of patients, which is critical for bladder management and diagnosis. Fourth, although we collected data from SCI patients in the three hospital districts of our hospital, only a small fraction of all SCI patients was identified, and it was not possible to determine the exact prevalence and disease management status of SCI patients in China. Fifth, this study was a single-hospital study, which may bring selection bias and decrease the representativeness of the sample. Sixth, although the hospitals in this study represent the better management of SCI in China and are of some reference value, they may not be generalizable to all hospitals.
Conclusions
Our findings suggest that the incidence of UTI in Chinese hospitalized patients with SCI was as high as 49.8%, which needs to be paid great attention by clinicians. We found that sex, hypoproteinemia, urinary incontinence, bladder irrigation, timing of rehabilitation, duration of indwelling urinary catheter were risk factors of UTI. Overall, it is of great significance to develop targeted preventive and management measures for these risk factors, which are expected to reduce the incidence of UTI in hospitalized SCI patients in China, and to improve patients' quality of life and rehabilitation outcomes.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Jazayeri, S. B., Beygi, S., Shokraneh, F., Hagen, E. M. & Rahimi-Movaghar, V. Incidence of traumatic spinal cord injury worldwide: A systematic review. Eur. Spine J. 24(5), 905–918 (2015).
Adriaansen, J. J. et al. Secondary health conditions in persons with spinal cord injury: A longitudinal study from one to five years post-discharge. J. Rehabil Med. 45(10), 1016–1022 (2013).
Unsal-Delialioglu, S. et al. Fever during rehabilitation in patients with traumatic spinal cord injury: Analysis of 392 cases from a national rehabilitation hospital in Turkey. J. Spinal Cord Med. 33(3), 243–248 (2010).
Brinkhof, M. W. et al. Health conditions in people with spinal cord injury: Contemporary evidence from a population-based community survey in Switzerland. J. Rehabil. Med. 48(2), 197–209 (2016).
Theisen, K. M. et al. Frequency of patient-reported UTIs is associated with poor quality of life after spinal cord injury: A prospective observational study. Spinal Cord 58(12), 1274–1281 (2020).
Groen, J. et al. Summary of European Association of Urology (EAU) Guidelines on Neuro-Urology. Eur. Urol. 69(2), 324–333 (2016).
Massa, L. M., Hoffman, J. M. & Cardenas, D. D. Validity, accuracy, and predictive value of urinary tract infection signs and symptoms in individuals with spinal cord injury on intermittent catheterization. J. Spinal Cord Med. 32(5), 568–573 (2009).
Poirier, C. et al. Prevention of urinary tract infections by antibiotic cycling in spinal cord injury patients and low emergence of multidrug resistant bacteria. Med. Mal. Infect. 46(6), 294–299 (2016).
Garcia-Arguello, L. Y. et al. Infections in the spinal cord-injured population: A systematic review. Spinal Cord 55(6), 526–534 (2017).
Hiersemenzel, L. P., Curt, A. & Dietz, V. From spinal shock to spasticity: Neuronal adaptations to a spinal cord injury. Neurology 54(8), 1574–1582 (2000).
Ko, H. Y. Revisit spinal shock: Pattern of reflex evolution during spinal shock. Korean J. Neurotrauma 14(2), 47–54 (2018).
Zhang, K., Zhang, Y., Chao, M. & Hao, Z. Prevalence, pathogenic bacterial profile and antimicrobial susceptibility pattern of urinary tract infection among children with congenital anomalies of the kidney and urinary tract. Infect. Drug Resist. 16, 4101–4112 (2023).
Tuszynski, M. H. et al. Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP Panel: Clinical trial inclusion/exclusion criteria and ethics. Spinal Cord 45(3), 222–231 (2007).
Krebs, J., Wollner, J. & Pannek, J. Risk factors for symptomatic urinary tract infections in individuals with chronic neurogenic lower urinary tract dysfunction. Spinal Cord. 54(9), 682–686 (2016).
Kim, Y. et al. Incidence and risk factors of urinary tract infections in hospitalised patients with spinal cord injury. J. Clin. Nurs. 30(13–14), 2068–2078 (2021).
Shekelle, P. G., Morton, S. C., Clark, K. A., Pathak, M. & Vickrey, B. G. Systematic review of risk factors for urinary tract infection in adults with spinal cord dysfunction. J. Spinal Cord Med. 22(4), 258–272 (1999).
Bakke, A. & Vollset, S. E. Risk factors for bacteriuria and clinical urinary tract infection in patients treated with clean intermittent catheterization. J. Urol. 149(3), 527–531 (1993).
Goetz, L. L. et al. International spinal cord injury urinary tract infection basic data set. Spinal Cord. 51(9), 700–704 (2013).
Pannek, J. Treatment of urinary tract infection in persons with spinal cord injury: Guidelines, evidence, and clinical practice: A questionnaire-based survey and review of the literature. J. Spinal Cord Med. 34(1), 11–15 (2011).
Biering-Sorensen, F., Bagi, P. & Hoiby, N. Urinary tract infections in patients with spinal cord lesions: Treatment and prevention. Drugs 61(9), 1275–1287 (2001).
Kwon, J. H., Fausone, M. K., Du, H., Robicsek, A. & Peterson, L. R. Impact of laboratory-reported urine culture colony counts on the diagnosis and treatment of urinary tract infection for hospitalized patients. Am. J. Clin. Pathol. 137(5), 778–784 (2012).
Togan, T., Azap, O. K., Durukan, E. & Arslan, H. The prevalence, etiologic agents and risk factors for urinary tract infection among spinal cord injury patients. Jundishapur J. Microbiol. 7(1), e8905 (2014).
Cardenas, D. D. & Hooton, T. M. Urinary tract infection in persons with spinal cord injury. Arch. Phys. Med. Rehabil. 76(3), 272–280 (1995).
Edokpolo, L. U., Stavris, K. B. & Foster, H. E. Jr. Intermittent catheterization and recurrent urinary tract infection in spinal cord injury. Top Spinal Cord Inj. Rehabil. 18(2), 187–192 (2012).
Cain, L. D. et al. Serum albumin improves recovery from spinal cord injury. J. Neurosci. Res. 85(7), 1558–1567 (2007).
Tong, B. et al. Serum albumin predicts long-term neurological outcomes after acute spinal cord injury. Neurorehabil. Neural Repair 32(1), 7–17 (2018).
Frisbie, J. H. Anemia and hypoalbuminemia of chronic spinal cord injury: Prevalence and prognostic significance. Spinal Cord 48(7), 566–569 (2010).
Gatta, A., Verardo, A. & Bolognesi, M. Hypoalbuminemia. Intern. Emerg. Med. 7(Suppl 3), S193–S199 (2012).
Karstens, L. et al. Does the urinary microbiome play a role in urgency urinary incontinence and its severity?. Front. Cell Infect. Microbiol. 6, 78 (2016).
Shimizu, N. et al. Molecular mechanisms of neurogenic lower urinary tract dysfunction after spinal cord injury. Int. J. Mol. Sci. 24(9), 7885 (2023).
Rodrigues, P., Hering, F. & Campagnari, J. C. Involuntary detrusor contraction is a frequent finding in patients with recurrent urinary tract infections. Urol. Int. 93(1), 67–73 (2014).
Elliott, T. S., Reid, L., Rao, G. G., Rigby, R. C. & Woodhouse, K. Bladder irrigation or irritation?. Br. J. Urol. 64(4), 391–394 (1989).
Jahromi, M. S., Mure, A. & Gomez, C. S. UTIs in patients with neurogenic bladder. Curr. Urol. Rep. 15(9), 433 (2014).
Hill, D. M., Wood, G. C. & Hickerson, W. L. Linezolid bladder irrigation as adjunctive treatment for a vancomycin-resistant Enterococcus faecium catheter-associated urinary tract infection. Ann. Pharmacother. 49(2), 250–253 (2015).
Xiang, Y. Y., Lv, Y., Guo, R. & Xue, J. Effect of bladder irrigation with amphotericin B for treatment of urinary tract fungal infection: A meta-analysis. Nan Fang Yi Ke Da Xue Xue Bao. 38(4), 466–470 (2018).
Ku, J. H. The management of neurogenic bladder and quality of life in spinal cord injury. BJU Int. 98(4), 739–745 (2006).
Ramakrishnan, K. et al. Early access to vocational rehabilitation for inpatients with spinal cord injury: A qualitative study of patients’ perceptions. Top Spinal Cord Inj Rehabil. 22(3), 183–191 (2016).
Lo, E. et al. Strategies to prevent catheter-associated urinary tract infections in acute care hospitals: 2014 update. Infect. Control Hosp Epidemiol. 35(Suppl 2), S32-47 (2014).
Stohrer, M. et al. EAU guidelines on neurogenic lower urinary tract dysfunction. Eur. Urol. 56(1), 81–88 (2009).
Nicolle, L. E. Catheter associated urinary tract infections. Antimicrob. Resist. Infect. Control 3, 2s3 (2014).
Funding
This study was supported by a grant of the China Association of Persons with Physical Disability (2020098).
Author information
Authors and Affiliations
Contributions
J.L.: study design, data collection, data analysis, original draft writing and editing. X.H. and X.S.: data collection. X.S. and R.C.: data analysis. T.X.: study design, data analysis, original draft editing, supervision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, J., Hao, X., Shang, X. et al. Incidence and risk factors of urinary tract infection in hospitalized patients with spinal cord injury in a hospital of China. Sci Rep 14, 3579 (2024). https://doi.org/10.1038/s41598-024-54234-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-54234-2
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.