Abstract
Somatic symptoms are common in a wide range of medical conditions. In severe cases, they are associated with high individual and economic burden. To explore social inequalities in somatic symptom severity (SSS) and to identify social groups with highest SSS, we applied an intersectional research approach. Analyses are based on cross-sectional data of the adult population living in Germany (N = 2413). SSS was assessed with the Somatic Symptom Scale-8. A multiple linear regression model with three-way interaction of gender, income and history of migration and post-hoc pairwise comparison of estimated marginal means was conducted. Analyses revealed intersectional inequalities in SSS along the axis of gender, income, and history of migration. Highest SSS was found in males with low income whose parent(s) immigrated, females with low income who immigrated themselves, and females with low income and no history of migration. Intersectional approaches contribute to a more comprehensive understanding of health disparities. To reduce disparities in SSS, proportionate universal interventions combining universal screening and targeted treatment seem promising.
Similar content being viewed by others
Introduction
Somatic symptoms are one of the primary causes of medical consultations1. They appear in a wide range of physical, mental, and psychosomatic diseases like cancer2, coronary heart disease3, anxiety, depression4,5 or somatic symptom disorder6. Overall, the most frequent symptoms are exhaustion- and pain-related complaints7,8. Thereby, the vast majority of all somatic symptoms presented in primary care turn out to be either minor and self-limited (about 75%) or persistent (about 20%), whereas less than 5% are acutely serious1. Women, older aged people, and people with low socio-economic status more often report severe somatic symptoms7,9,10,11. Regarding race/ethnicity (or adapted to the German research context, history of migration) as another important social determinant of health, evidence is lacking. Severe somatic symptoms are associated with functional impairment, a lower quality of life, sick leave, and increased health care visits5,8,9,11,12. Adjusted for chronic illness, they are an independent predictor of ill health and mortality (in men)9,10,13.
To identify individuals with high somatic symptom severity (SSS), brief universal self-reported screening tools like the Somatic Symptom Severity Scale-8 (SSS-8) as the short form of the Patient Health Questionnaire-15 (PHQ-15) seem promising9,14. For targeted interventions, depending on the type and extent of somatic symptoms (self-limited or persistent), medication and exercises to reduce pain, fatigue or digestive problems1,15 as well as antidepressants and cognitive behavioral interventions turned out to be effective1,16,17,18. The interventional approach of combining universal screening and targeted treatment follows the proportionate universalism formulated by Marmot & Bell19 which seems most promising to reduce health disparities.
However, it is still unclear which social subgroups have highest SSS and therefore may need particular attention in proportionate interventions. As described above, research on SSS focuses on separate socio-demographic variables so far. However, to gain a comprehensive understanding of the social context of SSS, the interplay of relevant social determinants of health in SSS needs to be examined. According to the framework of social determinants of health developed by the World Health Organization20, income, education, gender, and race/ethnicity have proven to be key social predictors of poor health outcomes. Understanding the interplay of these (and further) social predictors is the objective of intersectional research21. Intersectionality can be understood as the interaction of multiple social categories leading to more than additive disadvantage, discrimination and inequality. The framework is based on the work of Kimberlé Crenshaw who initially criticized the double discrimination due to race and sex faced by black women compared to black men and white women in the United States (U.S.)22. Stress exposure due to e.g. racism or sexism and subsequent coping mechanisms can result in higher morbidity and mortality23. Besides experiences of discrimination on the individual level, multiple discrimination can occur on a structural level diminishing peoples’ social power and opportunity for political participation24. In addition, agency to resist against one’s social categories might moderate the effect of intersections on health outcomes25. Thereby, social mechanisms can occur either additive (following the double/triple jeopardy) or multiplicative (in accordance with the multiple jeopardy) or some combination. Additive effects represent the sum of privileges and/or disadvantages, whereas multiplicative effects imply that the effects of the social characteristics enhance each other25,26,27.
Research on intersectional inequalities in different health outcomes, mainly self-rated mental and/or physical health status, received increased attention in the last five to ten years, currently still primarily in the U.S.28,29. Thereby, research focuses on the intersections of gender, race/ethnicity (history of migration) and/or socio-economic status (indicated by income, education and/or occupation). Due to the diverse assessment of the intersectional categories as well as methodological aspects, comparability is limited and results are inconclusive28,29. For the European or German context, so far only few studies were conducted indicating intersectional inequalities according to female gender, low income, and history of migration30,31,32. Common to all studies and in accordance with theoretical assumptions21,22, multiple privilege is attributed to the intersection of males with high income born in the respective country, whereas multiple disadvantage is attributed to females with low income born outside the respective country. These assumptions also serve as the basis for the present study.
To shed further light on the social context of SSS and to identify the ones with highest SSS, an intersectional approach is needed. Accordingly, we investigated the following research questions: To which degree is the adult population living in Germany affected by SSS? Is SSS more pronounced in people of female gender, low income, and history of migration, indicating social inequalities in SSS? If so, do gender, income and history of migration interact, indicating intersectional inequalities in SSS? And relatedly, have the more disadvantaged intersections (including female gender, low income, and a history of migration) significantly higher SSS than the more privileged ones (including male gender, high income, and no history of migration)?
Methods
Study design and sample
Analyses are based on cross-sectional data of the adult population (age ≥ 18 years) living in Germany. Data was collected via a telephone survey (computer assisted telephone interviews) from March until May 2022 by a company specialized on market and social research. By applying a dual frame approach with random-digit-dialing, 70% registered and computer generated as well as 30% mobile phone numbers were included in the sample33. Within households, respondents were randomly chosen via the Kish selection-grid34. Sample size calculation was based on a vignette design applied in the study (for details, please see the published study protocol35). These vignettes were not used in the present analyses. Interviews were conducted in German language. Accordingly, people with insufficient German language skills were excluded. The sample consisted of N = 2413 participants. The response rate was 45%. Data was weighted following a standardized three steps approach33,36. First, the distribution of household sizes in the sample was weighted according to the official distribution in the population. Second, design weights were calculated to correct for differing probabilities of selection rooted in the sampling design, including the household size and number of household and mobile phone numbers. Third, continuing bias in the distribution of socio-demographic characteristics due to e.g. higher non-response of certain groups of people was adjusted by applying the iterative proportional fitting including age, gender, education, and place of residence. After the three-steps weighting approach, the weighted study sample, regarding the fitted variables age, gender, and education (see Table 1) corresponded to the socio-demographic distribution of the official 2022 German statistics. Informed consent was obtained from all subjects and/or their legal guardian(s).
The survey is part of a large interdisciplinary project on persistence of somatic symptoms. The framework and study design of the Research Unit 5211 “Persistent SOMAtic Symptoms ACROSS Diseases: From Risk Factors to Modification (SOMACROSS)” and the subproject “Social Inequalities in Aggravating Factors of Persistent Somatic Symptoms (SOMA.SOC)” have been described in detail in the published study protocols35,37.
Measures
Social inequalities: Age, gender, education, net household income per month, and history of migration were assessed by a standardized questionnaire. Since only two respondents reported their gender as diverse, they were excluded from the analyses and the variable was dichotomized into male and female. The net monthly household income was converted into the equivalent income to take differences in household size and composition into account. First, to convert the categorical income variable into a metric scale, the range of each category was replaced by the respective mean value. In case of the lowest category, the mean value was set at 750 Euro and for the highest category at 5250 Euro. The values were then weighted according to the household size (first person factor 1, other persons aged ≥ 15 years factor 0.5, children aged < 15 years factor 0.3)38. The equivalent income was divided into terciles with the following categories: low (≤ 1250 Euro), medium (1251– < 2250 Euro), and high (≥ 2250 Euro) income. Years of education was categorized according to the International Standard Classification of Education into the following three levels of education: low (≤ 9 years), medium (10 years), and high (≥ 12 years)39. According to the definition of migration background by the Federal Statistical Office40, history of migration was assessed based on the nationality (German nationality and/or another) and country of birth of participant as well as the country of birth of both parents (born in Germany yes/no). Accordingly, participants could be allocated to the following three categories: no history of migration, people whose parents (one or both) have immigrated, and people who have immigrated themselves. Due to the historical context of so called guest workers, late emigrants, and refugees, German research mostly assesses history of migration instead of race/ethnicity23,40.
Somatic symptom severity (SSS): To assess SSS, the German version of the Somatic Symptom Scale-8 (SSS-8)9 was used as the short version of the Patient Health Questionnaire (PHQ-15) . The scale consists of eight items asking about the most frequent somatic symptoms, using a time interval of the last seven days. Each item can be scored on a 5-point Likert scale (0 = not bothered at all to 4 = bothered very much). The total score of the sum scale ranges from 0 to 32 with higher scores indicating higher SSS. The German version of the SSS-8 has good internal consistency with Cronbach α = 0.819. In the present study, Cronbach α was 0.82. Additionally, to assess different somatic symptom patterns, the eight items of the SSS-8 can be assigned to four subscales: gastrointestinal (1 item: stomach or bowel problems), pain (3 items: back pain; pain in arm, legs, joints; headache), cardiopulmonary (2 items: chest pain or shortness of breath; dizziness), and fatigue (2 items: feeling tired or having low energy; trouble sleeping). For comparability, the mean of each of the three subscales containing two or three items (pain, cardiopulmonary, fatigue) was weighted according to the number of items. The score of the four subscales ranges from 0 to 4.
Missing data
In total, about 18% of individual items across all variables were missing (at random). This was mostly due to missing values on the income variable. For the other variables, the amount of missing values was about 3%. The missing data pattern was analyzed, and missing data was imputed using the multivariate imputation by chained equations method41. The method for imputing missing values depends on the variable’s nature. For continuous variables, predictive mean matching was applied, while logistic regressions were used for binary variables.
Statistical analyses
To provide an overview of the study sample in terms of SSS, we first calculated arithmetic means with standard deviations (SD) for the SSS-8 sum scale and the four subscales. We then tested the hypothesis of higher SSS (in higher age, female gender, low income, and history of migration with analyses of variance.
Second, to gain a deeper understanding of (intersectional) social inequalities in SSS, we conducted multivariate analyses. As intersectional approaches have a high degree of complexity, we further analyzed the sum scale of the SSS-8 and refrained from including the subscales. We initially conducted a multiple linear regression model including the SSS-8 sum scale as the dependent variable, gender, income, and history of migration as predictors, and age as a covariate. To explore intersectional social inequalities in SSS, we then applied a descriptive intercategorical approach with multiplicative scale interaction24. Therefore, a second linear regression model was conducted with the SSS-8 sum scale as the dependent variable, gender, income, and history of migration as a three-way interaction term, and age as a covariate. Thereby, the intersections of gender, income, and history of migration represent not only characteristics on individual level, but broader social contexts24. Checks for multicollinearity revealed no collinearity issues. Concerning homoscedasticity and multivariate normality, deviation of residuals was observed due to the right-skewed distribution of the outcome. Hence, robust standard errors were used to ensure heteroscedasticity-consistent estimation42. Estimated marginal means with robust standard errors were calculated based on the multiple linear regression model including intersections. To identify the intersection with highest SSS, pairwise comparison of the estimated marginal means between the 18 intersections of gender, income, and history of migration (18 = 2 × 3 × 3) was carried out. Thereby, males with high income and no history of migration were set as the intersection of highest privilege, whereas females with low income who immigrated themselves were hypothesized as the most disadvantaged intersection. All other intersections represented a mix of privilege and disadvantage. To consider multiple testing, p-values were corrected with the false discovery rate according to Benjamin & Hochberg43. Performance of the different models (including explained variance and the interclass correlation coefficient, among others) was compared and tested with Vuong’s test to see if including the three-way interaction term of gender, income, and history of migration in the linear regression model was beneficial44,45. To assess the type of underlying social mechanism, we refer to significant interaction terms and Vuong’s test25. For all analyses, the weighted data set was used. The significance level for p-values was set at p < 0.05. Analyses were conducted with the R packages “sjPlot”46, “ggeffects”47, “easystats”48, and “ggplot2”49.
Ethical approval
The study design was approved by the Ethics Commission of the Hamburg Medical Chamber (No. 2020-10194-BO-ff). All research was performed in accordance with relevant guidelines/regulations and the Declaration of Helsinki.
Results
As presented in Table 1, mean age of participants was 51.4 years (SD = 18.8). Gender was equally distributed. About one third of respondents had a low (≤ 9 years), medium (10 or 11 years) or high education (≥ 12 years). The distribution of age, gender, and education corresponds to official German statistics50,51,52. The equivalent income of about one third of respondents could be rated as low (≤ 1250 Euro), medium (1251– < 2250 Euro) or high (≥ 2250 Euro). About 20% of participants had a history of migration. For the latter two, comparison with official German statistics was not possible since data was not available for the population aged 18 years or older53,54.
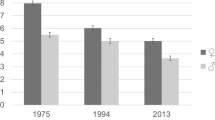
Means of the SSS-8 sum scale and the four subscales are presented in Table 2. Mean of the SSS-8 sum scale was 5.8 (SD = 5.7). Regarding the four subscales, respondents were more bothered by fatigue (mean = 1.1, SD = 1.1) and pain-related symptoms (mean 0.8, SD = 0.9) compared to gastrointestinal (mean = 0.5, SD = 0.9) or cardiopulmonary symptoms (mean 0.4, SD = 0.7).
Analyses of variance revealed significant differences in SSS within socio-demographic variables. Highest scores were found in females, middle aged people (41–60 years), people with low income, and people whose parent(s) immigrated. Similar patterns were found for the four subscales; Except no significant (p = 0.712) age difference showed for the gastrointestinal subscale and no significant (p = 0.551) gender difference appeared for the cardiopulmonary subscale. Moreover, for both of these subscales, highest values were found in people who immigrated themselves. Altogether, these bivariate analyses revealed social inequalities in SSS.
These social inequalities in SSS were also found in the multiple linear regression model 1 (Table 3). Age, female gender, low income, and history of migration were all significant predictors of higher SSS. The explained variance was 6.0%. Table 3 additionally presents model 2 including the interaction terms of gender, income, and history of migration. Here, female gender, low income and people who immigrated themselves remained significant predictors of higher SSS. Additionally, these predictors were significant in certain interaction terms, namely female*low income (p = 0.035), low income*parent(s) immigrated (p = 0.002), and female*low income*parent(s) immigrated (p < 0.001). The explained variance was 7.2%. Moreover, model 2 showed better performance than model 1 although Vuong’s test did not reach statistical significance (p = 0.052; see Supplementary Table S2).
Table 4 presents the age-adjusted estimated marginal means (emm) with 95% confidence intervals (CI) of SSS in the 18 intersections of gender, income, and history of migration based on the multiple linear regression model 2. The three intersections with highest SSS were males with low income whose parent(s) immigrated (emm = 9.83, 95%CI 6.58–13.07), females with low income who immigrated themselves (emm = 9.47, 95%CI 6.88–12.05), and females with low income and no history of migration (emm = 7.83, 95%CI 6.70–8.96). In contrast, males with high income and no history of migration (emm = 4.22, 95%CI 3.66–4.78) had lowest SSS, followed by males with high income whose parent(s) immigrated (emm = 4.40, 95%CI 3.48–6.12), and males with medium income and no history of migration (emm = 4.87, 95%CI 4.04–5.71). Significant differences between the above mentioned intersections with highest and lowest SSS became also apparent in the post-hoc pairwise comparison of the estimated marginal means of all 18 intersections with false discovery rate controlling (see Supplementary Table S1, with +/− indicating significant differences between the intersections with highest and lowest SSS).
Discussion
Summary of main results and discussion of current state of research
With our study, we shed further light on the social context of SSS in Germany. By applying an intersectional approach, we combined three important social determinants of health, namely gender, income, and history of migration, which were previously examined separately, if at all. Thereby, differentiating between parent(s) immigration and own immigration provides new insights into the intersections of people with a history of migration which were mostly divided into born inside/outside of the respective country in previous intersectional research28,29.
Our analyses revealed intersectional social inequalities in SSS, indicated by the significant interaction terms. The significant three-way interaction term female*low income*parent(s) immigrated reflects unexpected low SSS in this intersection. Intersections with highest SSS were males with low income whose parent(s) immigrated, females with low income who immigrated themselves, and females with low income and no history of migration. The intersections with lowest SSS were males with high income and no history of migration, males with high income whose parent(s) immigrated, and males with medium income and no history of migration. In post-hoc pairwise comparison, the intersections with highest and lowest SSS differed significantly from each other.
The score of the most affected intersection (emm = 9.83) was more than twice as high compared to the least affected intersection (emm = 4.22). According to the validation study by Gierk et al.9, this corresponds to an increase of the SSS-8 severity category from low (4–7 points) to medium (8–11 points). This is relevant for health care, since in the validation study, an increase of each SSS-8 severity category was associated with a 53% (95%CI 44–63%) increase in health care visits. In addition, the difference of the highest and lowest emm (9.83–4.22 = 5.61) can be rated as clinically relevant, since the minimal clinically important difference of the SSS-8 was estimated as a 3-point change12. As hypothesized, the intersection a priori defined as the most privileged one, namely males with high income and no history of migration, had lowest SSS. However, the intersection a priori set as the most disadvantaged, namely females with low income who immigrated themselves, showed (only) second highest SSS. In the intersections of mixed privilege and disadvantage no clear trend emerged. For instance, males whose parent(s) immigrated with low income had highest SSS but second lowest for the ones with high income. In relation to the impact of the three social characteristics, all intersections including low income (except males with no history of migration) were found among the ones with highest SSS. In contrast, no such trend emerged regarding gender or history of migration. Therefore, our study revealed further evidence for the great importance of economic deprivation in the light of other social characteristics like history of migration23.
Regarding the type of social mechanism (additive and/or multiplicative effect), inconclusive patterns emerged. On the one hand, there was indication for a multiplicative effect, since the multiple linear regression model included some significant interaction terms and showed better model performance25. On the other hand, the (just about) insignificant Vuong’s test confirmed no benefit of the three-way interaction term in the linear regression model. However, as currently discussed, the latter does not disprove intersectionality in SSS, “as it is above all a framework to understand heterogeneity and social power rather than a hypothesis”25.
For the European or German context, only few intersectional analyses were conducted so far indicating different intersectional gradients in several health outcomes. Since these studies differentiate between people born in and outside of the respective country (instead of race/ethnicity in case of studies from the U.S.), they are particularly suitable to contextualize our findings regarding history of migration. For instance, Wandschneider et al.30 found an intersectional gradient of female sex, feminine gendered practice and immigration experience associated with worse subjective mental and physical health in Germany. For Sweden, Wamala et al.32 found an intersectional gradient of female gender, low income, and birth outside of Sweden in acute somatic symptoms. However, contrary to our findings, the study revealed a clear intersectional gradient and the highest burden was found among women with high income who were born outside Sweden. In another Swedish study by Wemrell et al.31, similar to our findings, the worst self-rated health was found in females with low income who were born outside of Sweden. More intersectional research is needed to provide further insights into the diverse social (intersectional) contexts regarding health outcomes.
The intersectional inequalities in SSS found in our study can be explained in two directions. First, as somatic symptoms are reported in various diseases, an unequal distribution of these underlying diseases may contribute to an unequal distribution of SSS. For instance, individuals with lower income have a higher burden of chronic diseases55, females with no history of migration are more affected by chronic physical diseases like coronary heart disease, and females with a history of migration more often suffer from mental disorders like depression56. All these diseases are related to higher SSS3,4,9. Furthermore, an association between a longer duration of stay in the country of immigration and a worse subjective health was found23. Nevertheless, it is important to acknowledge that not only the history of migration itself but associated socio-economic disadvantages and experiences of discrimination are responsible for higher health burden, as discussed above23. Psychosocial factors like lack of social support, traumatic or adverse life events, and loneliness revealed to be strong predictors of somatic symptoms57. Since these psychosocial factors in turn are closely linked to social disadvantage and immigration experiences, they might also contribute to higher SSS in more disadvantaged intersections20,23.
Limitations
Some methodical aspects have to be considered when interpreting our results. The study sample with N = 2413 made discriminating intersectional analyses possible. Nevertheless, in the 18 intersections, there was quite some variation in the number of respondents (see Table 4). For this reason, we refrained from stratifying our analysis by age but presented age-adjusted results. Since age was associated with SSS in the bivariate analyses as well as the multiple linear regression models, it can be assumed that there are important differences according to individual life stages, which we were not able to take into account. Future studies with larger sample sizes could solve this problem. Also, the participants who reported their gender as diverse had to be excluded from analyses due to insufficient sample size, although additional differentiations of gender would have been preferable21. In future studies, gender practice and/or sexual orientation could also be analyzed.
Furthermore, our study sample did not fully cover the population with a history of migration53, especially with own migration experiences, last but not least because insufficient German language skills were an exclusion criterion in the present study. Since history of migration showed to be a significant predictor of SSS, associations might be even stronger for some subgroups like refugees. Future migration-related research should cover different languages and focus on lived experiences of specific migration populations to address heterogeneity23. In 2023, the focus on migration-related experiences rather than the country of birth was included in the definition of the Federal Statistical Office based on recommendations of the Commission on Integration58. In light of the research aim of the present study a pairwise comparison based on a fixed effects model with interaction terms was reasonable to compare the social groups with highest and lowest SSS24,25. However, to further address heterogeneity and gain a more comprehensive understanding on underlying social mechanisms, random effects models like MAIHDA (multilevel analysis of individual heterogeneity and discriminatory accuracy) seem promising in quantitative health research to identify differences between and within intersections25,59. In adition, to explore the richness of individual experiences within intersections qualitative methods appear promising25.
Moreover, it can be assumed that crucial protective factors (like agency, resilience, social support), risk factors (like experiences of individual or structural discrimination) as well as individual chronic illness would have drawn a more comprehensive picture of the predictors of SSS. This is also reflected in the low explained variance. However, these additional factors were not focus of the present study but could be included in future studies as discussed above. Furthermore, to reduce collinearity, we solely chose income (and not education in addition) as an indicator of socio-economic status as income not only effects material conditions but also social participation60.
With a mean SSS-8 score of 5.8 (SD = 5.7), we found slightly higher SSS in our study population compared to the initial validation study9. This may be explained by a slightly higher mean age and a lower income level of our study population. Additionally, since the study is specific for the German context, transferability of results to other countries is limited.
Conclusion
Intersectionality examines the interaction of multiple forms of disadvantage or oppression and the influence on peoples’ (health) experiences. By applying this framework, the study revealed intersectional inequalities in SSS as well as the intersections with highest SSS, namely males with low income whose parent(s) immigrated, females with low income who immigrated themselves, and females with low income with no history of migration. Following the proportionate universalism, a combination of universal and target interventions located in the health care system seems promising to reduce health disparities related to SSS (besides the general effort to reduce income inequalities). These may consist of brief universal screening tools for SSS in different languages to identify the individuals affected by high SSS in combination with targeted treatment interventions. Future intersectional research should emphasize the lived experiences of disadvantage and privilege and apply random effects models as well as qualitative approaches to shed further light on the social context of SSS.
Data availability
The datasets generated in and/or analyzed in the current study are available from the corresponding author on reasonable request.
References
Kroenke, K. Patients presenting with somatic complaints: Epidemiology, psychiatric comorbidity and management. Int. J. Meth. Psych. Res. 12, 34–43 (2006).
Kroenke, K. et al. Somatic symptoms in patients with cancer experiencing pain or depression: Prevalence, disability, and health care use. Arch. Intern. Med. 170, 1686–1694 (2010).
Kohlmann, S., Gierk, B., Hümmelgen, M., Blankenberg, S. & Löwe, B. Somatic symptoms in patients with coronary heart disease: prevalence, risk factors, and quality of life. JAMA Intern. Med. 173, 1469–1471 (2013).
Katon, W., Lin, E. H. & Kroenke, K. The association of depression and anxiety with medical symptom burden in patients with chronic medical illness. Gen. Hosp. Psychiatry 29, 147–155 (2007).
Löwe, B. et al. Depression, anxiety and somatization in primary care: Syndrome overlap and functional impairment. Gen. Hosp. Psychiatry 30, 191–199 (2008).
Ladwig, K. H., Marten-Mittag, B., Lacruz, M. E., Henningsen, P. & Creed, F. Screening for multiple somatic complaints in a population-based survey: does excessive symptom reporting capture the concept of somatic symptom disorders? Findings from the MONICA-KORA Cohort Study. J. Psychosom. Res. 68, 427–437 (2010).
Hinz, A. et al. Frequency of somatic symptoms in the general population: Normative values for the patient health questionnaire-15 (PHQ-15). J. Psychosom. Res. 96, 27–31 (2017).
Beutel, M. E. et al. Somatic symptoms in the German general population from 1975 to 2013. Sci. Rep. 10, 1595 (2020).
Gierk, B. et al. The somatic symptom scale-8 (SSS-8): A brief measure of somatic symptom burden. JAMA Intern. Med. 174, 399–407 (2014).
Atasoy, S. et al. Gender specific somatic symptom burden and mortality risk in the general population. Sci. Rep. 12, 15049 (2022).
Creed, F. H. et al. The epidemiology of multiple somatic symptoms. J. Psychosom. Res. 72, 311–317 (2012).
Gierk, B., Kohlmann, S., Hagemann-Goebel, M., Löwe, B. & Nestoriuc, Y. Monitoring somatic symptoms in patients with mental disorders: Sensitivity to change and minimal clinically important difference of the Somatic Symptom Scale – 8 (SSS-8). Gen. Hosp. Psychiatry 48, 51–55 (2017).
Lee, S., Creed, F. H., Ma, Y.-L. & Leung, C. M. Somatic symptom burden and health anxiety in the population and their correlates. J. Psychosom. Res. 78, 71–76 (2015).
Zijlema, W. L. et al. How to assess common somatic symptoms in large-scale studies: A systematic review of questionnaires. J. Psychosom. Res. 74, 459–468 (2013).
Kroenke, K., Arrington, M. E. & Mangelsdorff, A. D. The prevalence of symptoms in medical outpatients and the adequacy of therapy. Arch. Intern. Med. 150, 1685–1689 (1990).
Hennemann, S. et al. Internet-based CBT for somatic symptom distress (iSOMA) in emerging adults: A randomized controlled trial. J. Consult. Clin. Psychol. 90, 353–365 (2022).
Kroenke, K. & Swindle, R. Cognitive-behavioral therapy for somatization and symptom syndromes: A critical review of controlled clinical trials. Psychother. Psychosom. 69, 205–215 (2000).
Salerno, S. M., Browning, R. & Jackson, J. L. The effect of antidepressant treatment on chronic back pain: A meta-analysis. Arch. Intern. Med. 162, 19–24 (2002).
Marmot, M. & Bell, R. Fair society, healthy lives. PublicHealth 126, S4–S10 (2012).
World Health Organization. A conceptual framework for action on the social determinants of health. Social determinants of health discussion paper 2. https://www.who.int/publications/i/item/9789241500852 (2010).
Krieger, N. Measures of racism, sexism, heterosexism, and gender binarism for health equity research: From structural injustice to embodied harm—An ecosocial analysis. Annu. Rev. Public Health 41, 37–62 (2020).
Crenshaw, K. Demarginalizing the intersection of race and sex: a black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. Univ. Chicago Legal Forum 1, 139–167 (1989).
Bartig, S. et al. Health of people with selected citizenships: Results of the study GEDA Fokus. J. Health Monit. 8, 7–33 (2023).
Bauer, G. R. & Scheim, A. I. Methods for analytic intercategorical intersectionality in quantitative research: Discrimination as a mediator of health inequalities. Soc. Sci. Med. 226, 236–245 (2019).
Holman, D. & Walker, A. Understanding unequal ageing: Towards a synthesis of intersectionality and life course analyses. Eur. J. Ageing 18, 239–255 (2021).
Bauer, G. R. Incorporating intersectionality theory into population health research methodology: Challenges and the potential to advance health equity. Soc. Sci. Med. 110, 10–17 (2014).
Abichahine, H. & Veenstra, G. Inter-categorical intersectionality and leisure-based physical activity in Canada. Health Promot. Int. 32, 691–701 (2017).
Trygg, N. F., Gustafsson, P. E. & Månsdotter, A. Languishing in the crossroad? A scoping review of intersectional inequalities in mental health. Int. J. Equity Health 18, 115 (2019).
Mena, E. et al. Intersectionality-based quantitative health research and sex/gender sensitivity: A scoping review. Int. J. Equity Health 18, 199 (2019).
Wandschneider, L., Miani, C. & Razum, O. Decomposing intersectional inequalities in subjective physical and mental health by sex, gendered practices and immigration status in a representative panel study from Germany. BMC Public Health 22, 683 (2022).
Wemrell, M., Karlsson, N., Perez Vicente, R. & Merlo, J. An intersectional analysis providing more precise information on inequities in self-rated health. Int. J. Equity Health 20, 54 (2021).
Wamala, S., Ahnquist, J. & Månsdotter, A. How do gender, class and ethnicity interact to determine health status?. J. Gend. Stud. 18, 115–129 (2009).
ADM. ADM research project ‘dual-frame approaches’ 2011/2012 research report. [ADM-Forschungsprojekt ‚Dual-Frame-Ansätze’ 2011/2012 Forschungsbericht]. Available at https://www.adm-ev.de/leistungen/arbeitsgemeinschaft-adm-stichproben/ (2012).
Kish, L. A procedure for objective respondent selection within the household. J. Am. Stat. Assoc. 44, 380–387 (1949).
von dem Knesebeck, O., Barbek, R. & Makowski, A. C. Social inequalities in aggravating factors of somatic symptom persistence (SOMA.SOC): study protocol for a mixed-method observational study focusing on irritable bowel syndrome and fatigue. BMJ open 13, e070635 (2023).
Kolenikov, S. Calibrating survey data using iterative proportional fitting (raking). Stat. J. 14, 22–59 (2014).
Löwe, B. et al. Persistent SOMAtic symptoms ACROSS diseases – from risk factors to modification: Scientific framework and overarching protocol of the interdisciplinary SOMACROSS research unit (RU 5211). BMJ open 12, e057596 (2022).
OECD. What are equivalence scales? OECD project on income distribution and poverty. www.oecd.org/social/inequality.htm (n.d.).
eurostat. International standard classification of education (ISCED). Available at https://ec.europa.eu/eurostat/statistics-explained/index.php?title=International_Standard_Classification_of_Education_%28ISCED%29#ISCED_1997_.28fields.29_and_ISCED-F_2013 (2020).
Federal Statistical Office. Data report 2021: a social report for the Federal Republic of Germany. [Datenreport 2021. Ein Sozialbericht für die Bundesrepublik Deutschland]. https://www.destatis.de/DE/Service/Statistik-Campus/Datenreport/Downloads/datenreport-2021.html (2021).
van Buuren, S. & Groothuis-Oudshoorn, K. mice: Multivariate imputation by chained equations in R. J. Stat. Soft. 45, 1 (2011).
Long, J. S. & Ervin, L. H. Using heteroscedasticity consistent standard errors in the linear regression model. Am. Stat. 54, 217–224 (2000).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J. R. Stat. Soc. Ser. B 57, 449–518 (1995).
Lüdecke, D. et al. Test if models are different. https://easystats.github.io/performance/reference/test_performance.html (n.d.).
Vuong, Q. H. Likelihood ratio tests for model selection and non-nested hypotheses. Econometrica 57, 307–333 (1989).
Lüdecke, D. Data visualization for statistics in social science [package sjPlot version 2.8.11]. https://cran.r-project.org/web/packages/sjPlot/index.html (2022).
Lüdecke, D. Ggeffects: Tidy data frames of marginal effects from regression models. J. Open Source Softw. 3, 722 (2018).
Lüdecke, D. et al. easystats: framework for easy statistical modeling, visualization, and reporting. CRAN. https://easystats.github.io/easystats/ (2022).
Wickham, H. ggplot2. Elegant Graphics for Data Analysis (Springer, 2016).
Federal Statistical Office. Population by nationality and gender (quarterly figures). [Bevölkerung nach Nationalität und Geschlecht (Quartalszahlen)]. https://www-genesis.destatis.de/genesis//online?operation=table&code=12111-0001&bypass=true&levelindex=0&levelid=1701698283915#abreadcrumb (2023).
Federal Statistical Office. Population: Germany, reference date, years of age. [Bevölkerung: Deutschland, Stichtag, Altersjahre]. https://www-genesis.destatis.de/genesis//online?operation=table&code=12111-0004&bypass=true&levelindex=0&levelid=1701698354729#abreadcrumb (2023).
Federal Statistical Office. Germany, years, gender, age groups, general school education. [Deutschland, Jahre, Geschlecht, Altersgruppen, Allgemeine Schulausbildung]. https://www-genesis.destatis.de/genesis//online?operation=table&code=12211-0100&bypass=true&levelindex=0&levelid=1701698246731#abreadcrumb (2023).
Federal Statistical Office. Statistical report - Microcensus - Population by migration background. First results 2022. [Statistischer Bericht - Mikrozensus - Bevölkerung nach Migrationshintergrund. Erstergebnisse 2022]. https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Bevoelkerung/Migration-Integration/Publikationen/_publikationen-innen-migrationshintergrund.html (2023).
Federal Statistical Office. Income distribution (net equivalent income) in Germany. [Einkommensverteilung (Nettoäquivalenzeinkommen) in Deutschland]. https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Einkommen-Konsum-Lebensbedingungen/Lebensbedingungen-Armutsgefaehrdung/Tabellen/einkommensverteilung-mz-silc.html (2023).
Lampert, T., Kroll, L. E., Kuntz, B. & Hoebel, J. Health inequality in Germany and in international comparison: developments and trends over time: [Gesundheitliche Ungleichheit in Deutschland und im internationalen Vergleich: Zeitliche Entwicklungen und Trends]. J. Health Monit. 3, 1 (2018).
Robert Koch-Institute. Health situation of women in Germany—important facts at a glance (2023). [Gesundheitliche Lage der Frauen in Deutschland—wichtige Fakten auf einen Blick (2023)]. https://www.rki.de/DE/Content/GesundAZ/F/Frauengesundheit/GBE-Broschuere.html (2023).
Loeb, T. B. et al. Predictors of somatic symptom severity: The role of cumulative history of trauma and adversity in a diverse community sample. Psychol. Trauma 10, 491–498 (2018).
Canan, C. & Petschel, A. The implementation of the concept “immigration history” in the microcensus 2022. [Die Umsetzung des Konzepts “Einwanderungsgeschichte” im Mikrozensus 2022.]. Wirtsch. Stat., 61–73 (2023).
Merlo, J. Multilevel analysis of individual heterogeneity and discriminatory accuracy (MAIHDA) within an intersectional framework. Soc. Sci. Med. 203, 74–80 (2018).
Marmot, M. The influence of income on health: views of an epidemiologist. Health Aff. 21, 31–46 (2002).
Acknowledgements
We would like to thank Dr. Daniel Lüdecke, who supported our statistical analyses with his expertise, and Andrea V. Parkhouse for the language editing.
Funding
Open Access funding enabled and organized by Projekt DEAL. This work was carried out within the framework of Research Unit 5211 (FOR 5211) 'Persistent SOMAtic Symptoms ACROSS Diseases: From Risk Factors to Modification (SOMACROSS)', funded by the German Research Foundation (Deutsche Forschungsgemeinschaft, DFG). The DFG grant number for this project (P 06) “Social Inequalities in Aggravating Factors of Somatic Symptom Persistence (SOM.SOC)” is 445297796.
Author information
Authors and Affiliations
Contributions
R.B. made substantial contributions to the conception, the analysis and interpretation of data, and drafted the manuscript. A.T. substantively revised the manuscript. B.L. substantively revised the manuscript. O.v.d.K. made substantial contributions to the conception and the analysis, and substantively revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Barbek, R., Toussaint, A., Löwe, B. et al. Intersectional inequalities in somatic symptom severity in the adult population in Germany found within the SOMA.SOC study. Sci Rep 14, 3820 (2024). https://doi.org/10.1038/s41598-024-54042-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-54042-8
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.