Abstract
This study aimed to explore the effectiveness and safety of azvudine, nirmatrelvir/ritonavir, and molnupiravir in adult patients with mild-to-moderate COVID-19. This retrospective cohort study included patients with mild-to-moderate COVID-19 (asymptomatic, mild, and common types) at the First Hospital of Changsha (Hunan Province, China) between March and November 2022. Eligible patients were classified into the azvudine, nirmatrelvir/ritonavir, or molnupiravir groups according to the antiviral agents they received. The outcomes were the times to nucleic acid negative conversion (NANC). This study included 157 patients treated with azvudine (n = 66), molnupiravir (n = 66), or nirmatrelvir/ritonavir (n = 25). There were no statistically significant differences in the time from diagnosis to NANC among the azvudine, molnupiravir, and nirmatrelvir/ritonavir groups [median, 9 (95% CI 9–11) vs. 11 (95% CI 10–12) vs. 9 (95% CI 8–12) days, P = 0.15], time from administration to NANC [median, 9 (95% CI 8–10) vs. 10 (95% CI 9.48–11) vs. 8.708 (95% CI 7.51–11) days, P = 0.50], or hospital stay [median, 11 (95% CI 11–13) vs. 13 (95% CI 12–14) vs. 12 (95% CI 10–14) days, P = 0.14], even after adjustment for sex, age, COVID-19 type, comorbidities, Ct level, time from diagnosis to antiviral treatment, and number of symptoms. The cumulative NANC rates in the azvudine, molnupiravir, and nirmatrelvir/ritonavir groups were 15.2%/12.3%/16.0% at day 5 (P = 0.858), 34.8%/21.5%/32.0% at day 7 (P = 0.226), 66.7%/52.3%/60.0% at 10 days (P = 0.246), and 86.4%/86.2%/80.0% at day 14 (P = 0.721). No serious adverse events were reported. Azvudine may be comparable to nirmatrelvir/ritonavir and molnupiravir in adult patients with mild-to-moderate COVID-19 regarding time to NANC, hospital stay, and AEs.
Similar content being viewed by others
Introduction
COVID-19 is a pandemic infectious respiratory disease caused by the novel coronavirus SARS-CoV-2 that has caused a serious public health, social, and economic crisis worldwide1. COVID-19 infection has been confirmed in more than 767 million people worldwide by June 4, 2023, including more than 6.9 million deaths2, imposing a huge burden on the global socioeconomic and medical systems3,4. As many countries relaxed their lockdown policies in the past months, including China, the newly reported volatile increase in COVID-19 cases in China by the Chinese Center for Disease Control and Prevention (China CDC)5 might be due to the antibody escape and immunoneutralization of the Omicron variant from the constant mutation and evolution of COVID-196,7. The second wave of the pandemic caused by the SARS-CoV-2 Omicron variant tends to occur 5–7 months after the first wave8. The social and economic burden of mild and moderate COVID-19 infection cannot be ignored, though severe cases represent a small proportion of the second wave in most countries9.
Antiviral therapy is recommended by the World Health Organization for reducing mortality in hospitalized patients with COVID-19 infection10. Previous studies showed the efficacy and safety of nirmatrelvir/ritonavir (Paxlovid®)11,12,13 and molnupiravir14,15, although there is still some controversy16. However, nirmatrelvir/ritonavir and molnupiravir may not be widely available for developing countries due to the high costs. A new antiviral drug that would be safe, effective, and easily available is urgently needed.
Azvudine (FNC) is a nucleoside analog that can cure COVID-19 through its anti-SARS-CoV-2 activity concentrated in the thymus and strengthening patient immunity17. A pilot randomized controlled trial (RCT) with a small sample size (n = 20) in China showed that azvudine could shorten the treatment duration of patients with mild symptoms, and therefore saving a great deal of medical resources18. The same conclusion was drawn in a multi-center RCT in Brazil19. On the contrary, a retrospective Chinese study suggested that nirmatrelvir/ritonavir was superior to azvudine regarding the time to the first nucleic acid negative conversion (NANC) and antiviral activity20. Even so, the benefits of the three available anti-COVID-19 drugs for Chinese adult patients with mild or moderate symptoms remain uncertain.
Therefore, this study aimed to explore the effectiveness and safety of the azvudine, nirmatrelvir/ritonavir, and molnupiravir in adult patients with mild-to-moderate COVID-19. The results could help the management of patients with COVID-19.
Methods
Study design and patients
This retrospective cohort study included patients with confirmed COVID-19 at the First Hospital of Changsha (Hunan Province, China) between March and November 2022.
The inclusion criteria were (1) 18–60 years of age, (2) tested positive [cycle threshold (Ct) value ≤ 40] for SARS-CoV-2 nucleic acids by reverse transcriptase polymerase chain reaction (RT-PCR), (3) diagnosed as asymptomatic, mild, or common type of COVID-19 in accordance with the “Diagnosis and Treatment Protocol for Novel Coronavirus Pneumonia (Trial Version 9)”, and (4) received azvudine, molnupiravir, or nirmatrelvir/ritonavir as antiviral treatment. The exclusion criteria were (1) the time from diagnosis to treatment was > 5 days, (2) other antiviral therapies were given, or (3) incomplete key clinical information, such as the NANC time.
Ethical statement
The study was approved by the ethics committee of the First Hospital of Changsha (Approval #KL-2020005). The requirement for individual informed consent was waived by the ethics committee of the First Hospital of Changsha because of the retrospective nature of the study. This study was conducted in accordance with the principles of the Declaration of Helsinki.
Grouping and treatment
All eligible patients were grouped into the azvudine, nirmatrelvir/ritonavir, and molnupiravir groups according to their treatments. Azvudine was given at 5 mg/dose once daily for 7 days. Nirmatrelvir/ritonavir was given at 300 mg of nirmatrelvir and 100 mg of ritonavir twice a day for 5 days. Molnupiravir was given at 800 mg twice a day for 5 days. Other supportive treatments included ibuprofen and cough suppressant (Feilike Mixture).
Data collection and outcomes
The baseline data collected included age, sex, COVID-19 type, comorbidities, number of COVID-19 symptoms, Ct value of the COVID-19 nucleic acid test, and the time from diagnosis to administration of the antiviral agents. The comorbidities included cardiovascular diseases, chronic lung diseases, diabetes, chronic liver and kidney diseases, tumors, acquired immunodeficiency syndrome (AIDS), and immune diseases with long-term glucocorticoids or immunosuppressive drugs. COVID-19 symptoms included fever, fatigue, cough, nasal congestion/runny nose, intolerance of cold/chills, shortness of breath, abdominal pain, diarrhea, headache, dizziness, palpitations, chest tightness, chest pain, dry/sore/itchy throat, muscle soreness, nausea/vomiting, dyspnea, gastric distension, stomach pain, loss of taste/poor appetite, and hyposmia.
The outcomes were the times to negative conversion in a COVID-19 nucleic acid test, including (1) the time from diagnosis to NANC, defined as the time from the first positive result in a nucleic acid test to the first NANC, (2) the time from the start of treatment to NANC, defined as the time from the first use of antiviral therapy to the first NANC, and (3) the NANC rates within 5, 7, 10 and 14 days after starting antiviral therapy. The length of hospital stay and adverse events (AEs) during hospitalization were recorded as well.
The Ct value of the SARS-CoV-2 nucleic acid test was detected through a nasopharyngeal swab. Per Chinese policy guidelines, patients underwent nucleic acid testing every other day until their Ct reached 30 or higher, after which testing became daily. A Ct value > 40 was considered negative. Laboratory test results were checked at admission and before discharge to monitor patients’ liver function. Discharge was granted only after two consecutive Ct readings exceeded 35, taken 24 h apart.
Statistical analysis
R version 4.2.1 (The R Project for Statistical Computing, www.r-project.org) was used for statistical analysis. Age was expressed as mean ± standard deviation. The Ct value of the nucleic acid test was expressed as median (range). The comparison among the three groups was performed through one-way ANOVA or the Kruskal–Wallis H test. The categorical data were expressed as n (%), and the chi-square test was used to compare the three groups. The Kaplan–Meier method was used to analyze the time from diagnosis to the first NANC, the time from the start of antiviral therapy to NANC, and the length of hospital stay, calculating the median time and the corresponding 95% confidence interval (CI). The log-rank test was performed to analyze the differences among groups. Univariable and multivariable Cox regression analyses were performed to determine the association of the selection of azvudine, molnupiravir or nirmatrelvir/ritonavir with the NANC times and hospital stay. The multivariable analyses were adjusted for sex, age, COVID-19 type, comorbidities, Ct level, time from diagnosis to antiviral treatment, and number of symptoms. Variables with P < 0.05 in the univariable analyses were included in the multivariable analysis. Two-sided P-values < 0.05 were considered statistically significant.
Results
Characteristics of the patients
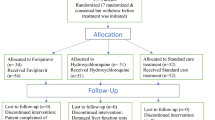
This study included 157 patients with COVID-19 treated with azvudine (n = 66), molnupiravir (n = 66), or nirmatrelvir/ritonavir (n = 25). The mean age of patients in the azvudine, molnupiravir, and nirmatrelvir/ritonavir groups were 41.1 ± 10.0, 38.0 ± 10.8, and 44.3 ± 13.4 years, respectively. A higher proportion of patients in the nirmatrelvir/ritonavir group had comorbidities (azvudine: 21.2%; molnupiravir: 48.5%; nirmatrelvir/ritonavir: 84.0%; P < 0.001). More asymptomatic patients were in the azvudine and molnupiravir groups (azvudine: 33.3%; molnupiravir: 37.9%; nirmatrelvir/ritonavir: 12.0%; P = 0.004). More patients started antiviral treatment on the day of diagnosis in the azvudine group than the molnupiravir or nirmatrelvir/ ritonavir groups (57.6% vs. 33.3% vs. 44.0%, P = 0.029). There were no statistically significant differences among groups regarding sex, Ct values, and number of symptoms (all P > 0.05) (Table 1).
Clinical outcomes
There were no statistically significant differences in the time from diagnosis to NANC among the azvudine, molnupiravir, and nirmatrelvir/ritonavir groups [median, 9 (95% CI 9–11) vs. 11 (95% CI 10–12) vs. 9 (95% CI 8–12) days, P = 0.15] (Fig. 1A). No statistically significant differences were observed among the three groups in terms of the time from antiviral treatment to NANC [median, 9 (95% CI 8–10) vs. 10 (95% CI 9.48–11) vs. 8.708 (95% CI 7.51–11) days, P = 0.50] (Fig. 1B). The length of hospital stay were similar among the three groups as well [median, 11 (95% CI 11–13) vs. 13 (95% CI 12–14) vs. 12 (95% CI 10–14) days, P = 0.14] (Fig. 1C).
The cumulative NANC rates in the azvudine, molnupiravir, and nirmatrelvir/ritonavir groups were 15.2%, 12.3%, and 16.0% at day 5 (P = 0.858), 34.8%, 21.5%, and 32.0% at day 7 (P = 0.226), 66.7%, 52.3%, and 60.0% at 10 days (P = 0.246), and 86.4%, 86.2%, and 80.0% at day 14 (P = 0.721) (Table 2).
Univariable and multivariable analyses
The univariable and multivariable Cox regression analyses showed that the selection of azvudine, molnupiravir or nirmatrelvir/ritonavir was not associated with the time from diagnosis to NANC, the time from treatment start to NANC, or the length of hospital stay after adjustment for sex, age, COVID-19 type, comorbidities, Ct level, time from diagnosis to antiviral treatment, and number of symptoms (all P > 0.05) (Table 3).
Subgroup analysis of the NANC rates
Patients who received azvudine had higher NANC rates at day 5, 7, 10, and 14 when they started the antiviral drug on the day of diagnosing COVID-19 compared to those who started it later. Similarly, patients who received molnupiravir had higher NANC rates at days 5, 7, and 10 when starting the drug on the day of diagnosis, but not at day 14. On the other hand, patients who received nirmatrelvir/ritonavir showed an opposite trend: those who started the drug at least one day after diagnosis had higher NANC rates at days 5, 7, and 10 compared to those who started it on the day of diagnosis, while the rates were similar at day 14 (Table 4).
Changes in blood biochemical parameters and adverse events
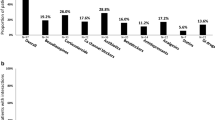
The changes in biochemical parameters at discharge from admission were compared among the three groups (Fig. 2). The decreases in alanine aminotransferase (ALT) and aspartate aminotransferase (AST) levels were significantly greater with azvudine than with molnupiravir or nirmatrelvir/ritonavir (all P < 0.05), while there were no significant differences between molnupiravir and nirmatrelvir/ritonavir (both P > 0.05). The increase in creatinine in the nirmatrelvir/ritonavir group was significantly smaller than in the molnupiravir (P = 0.021) and azvudine (P = 0.017) groups; there were no significant differences between the molnupiravir and azvudine groups (P = 0.71). The increase in the albumin-to-globulin ratio of the azvudine group was significantly higher than in the molnupiravir group (P < 0.001), without difference with the nirmatrelvir/ritonavir group (P = 0.46); there were no significant differences between the nirmatrelvir/ritonavir and molnupiravir groups (P = 0.073). There were no significant differences among the three groups regarding the changes in IgG, IgM, globulin, and blood urea nitrogen (all P > 0.05).
Changes in biochemistry indicators between admission and discharge. (A) Alanine aminotransferase. (B) Aspartate aminotransferase. (C) IgG. (D) IgM. (E) Globulin. (F) Blood urea nitrogen. (G) Creatinine. (H) Albumin to globulin ratio. ns indicates P > 0.05; * denotes P ≤ 0.05; ** indicates P ≤ 0.01; *** represents P ≤ 0.001; **** signifies P ≤ 0.0001.
No serious AEs (SAEs) were reported in any of the three groups. No AEs leading to suspension, dose reduction, or permanent discontinuation of the antiviral agents were observed.
Discussion
This retrospective study explored the effectiveness and safety of azvudine, nirmatrelvir/ritonavir, and molnupiravir in adult patients with mild-to-moderate COVID-19. The results suggest no statistically significant differences among the three groups regarding the time from diagnosis to NANC, the time from starting antiviral treatment to NANC, or hospital stay. No SAEs were recorded in any group. Nevertheless, some numerical differences were observed among the three groups regarding the time to and the response patterns in time, suggesting that large-scale multicenter trials should be conducted to investigate these differences.
Previous studies indicated that nirmatrelvir/ritonavir can shorten the NANC time and hospital stay in patients with COVID-1911,13,21. It was also reported that molnupiravir could reduce the risks of hospitalization and death and shorten the time of viral clearance in adult patients with mild or moderate COVID-1914,15,16,22. Consequently, nirmatrelvir/ritonavir and molnupiravir are recommended in the World Health Organization guidelines for managing COVID-1910. Azvudine is an antiviral agent developed in China and has been shown to reduce the NANC time18. Regarding mild COVID-19, another study indicated that azvudine reduced the viral load and shortened the NANC time19. Still, most studies compared the antiviral drugs with a placebo or historical controls.
A recent retrospective study by Gao et al. revealed that nirmatrelvir/ritonavir in patients older than 65 years could better reduce the NANC time than azvudine20. In the present study, there were no differences between nirmatrelvir/ritonavir and azvudine in terms of NANC times, but the patients included here were mostly younger than in the previous study and had fewer comorbidities (and possibly fewer concomitant medications), as supported by a comparison between younger and older patients with COVID-1923. Furthermore, the groups were different in size, which could influence the comparisons. Some patients in Gao et al.20 were not prescribed antivirals at the initial phase, while in the present study, all patients started the antiviral drugs within 2 days of diagnosis, increasing the reliability of the present results. The present study suggests that azvudine in patients with mild-to-moderate COVID-19 was not weaker than nirmatrelvir/ritonavir. Still, the quality of evidence from retrospective studies is low, and confirmation is required.
Interestingly, the subgroup analysis suggested that the NANC rates with azvudine (at days 5, 7, 10, and 14) or molnupiravir (at days 5, 7, and 10) were higher if azvudine or molnupiravir were started on the same day as diagnosis, while an inverse pattern (at days 5, 7, and 10) was observed with nirmatrelvir/ritonavir, i.e., the NANC rate was higher if started 1–2 days after diagnosis. Still, the subgroups were too small to be able to perform reliable statistical analyses. Furthermore, such differences in NANC patterns were not reported before in the literature. Although there is a possibility that these results are coincidental, they could be explored in future large-scale multicenter studies.
In the present study, the Cox analyses showed that compared with azvudine, the HRs of molnupiravir or nirmatrelvir/ritonavir were all smaller than 1, suggesting a possible numerical benefit trend of azvudine, even after adjustment for sex, age, COVID-19 type, comorbidities, Ct level, time from diagnosis to antiviral treatment, and the number of symptoms. Still, all HRs were not statistically significant, and no conclusion can be reached at present, pending additional large-scale prospective studies.
Liver function impairment can be observed in patients with COVID-19 and could contribute to poor outcomes in patients with severe COVID-19 or those with pre-existing liver conditions24,25,26. Liver function impairment, particularly increased ALT and AST, caused by nirmatrelvir/ritonavir, has been reported27,28,29. On the other hand, changes in liver function impairment from molnupiravir have been reported to be relatively small30. In the present study, azvudine was the only drug to show significant decreases in ALT and AST levels from baseline. Still, the present study could not determine causality. It remains unknown whether azvudine does not increase ALT and AST and/or controls COVID-19 well enough to alleviate the liver injury. Still, potential concerns about liver function impairment may discourage some physicians and patients from using antiviral therapies, especially in mild or moderate COVID-19 associated with a small risk of poor outcomes. According to the present study, azvudine may be a safer option for patients with pre-existing liver function impairment, but studies must examine that point specifically. On the other hand, nirmatrelvir/ritonavir showed the smallest increases in creatinine levels compared with azvudine and molnupiravir. These results are a little surprising since azvudine has been suggested to be the drug of choice for patients with chronic kidney diseases compared with other antiviral drugs for COVID-1931,32,33. The discrepancy could be due to several factors, including patient selection and the characteristics of the patients. Additional studies are necessary to examine that issue.
No SAEs were recorded in the present study. Although a documentation bias is possible for retrospective studies, especially for mild AEs difficult to distinguish from the signs and symptoms of COVID-19 and in the context of stretched human healthcare resources, SAEs would have been noted since all included patients were hospitalized and continuously monitored for their signs and symptoms and aggravation. Furthermore, the antiviral therapies for mild or moderate COVID-19 are short (generally 5–7 days10), decreasing the risk of AE development. Favorable safety profiles have been noted for nirmatrelvir/ritonavir11,13,21, molnupiravir14,15,16,22, and azvudine18,19. Again, the small sample size and the retrospective nature of the study probably led to an underestimation of the AEs.
Recent studies suggested viral load rebounds during nirmatrelvir/ritonavir and molnupiravir treatment for COVID-1934,35,36,37, but no rebound phenomenon has been reported so far for azvudine. A dynamic analysis of the viral loads suggested that azvudine could effectively reduce the patient viral loads without rebound19. The exact causes of viral load rebound are unknown but are probably related to a resistance mutation arising through selection pressure. The differences in the targets and mechanisms of action between azvudine and the other drugs could lead to a lower risk of resistance mutation, but it will have to be examined in future studies.
This study has limitations. First, since this was a retrospective study, it may suffer from several biases, and some essential data might be missing, leading to patient exclusion. Second, this study involved a single center, leading to a small sample size, especially in the subgroups, preventing reliable analyses. Third, only patients with asymptomatic, mild or common type of COVID-19 were included, and more severe and complex cases were not. The interaction of antiviral drugs with other therapies used for severe COVID-1938 should be investigated. Furthermore, the non-random selection of drugs, qualitative nature of nucleic acid testing, and potential variance in patient viral loads can impact results interpretation. For more definitive outcomes, prospective randomized controlled trials comparing the efficacy of these drugs are necessary.
In conclusion, azvudine may be comparable to nirmatrelvir/ritonavir and molnupiravir in adult mild-to-moderate COVID-19 patients regarding NANC times, hospital stay, and AEs. Formal randomized controlled trials should be performed to compare the three drugs directly and to identify subgroups of patients who might benefit more from a specific drug.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Wiersinga, W. J., Rhodes, A., Cheng, A. C., Peacock, S. J. & Prescott, H. C. Pathophysiology, transmission, diagnosis, and treatment of Coronavirus Disease 2019 (COVID-19): A review. JAMA 324, 782–793 (2020).
World Health Organization. COVID-19 Weekly Epidemiological Update. Edition 140 published 27 April 2023. https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---27-april-2023. Accessed May 2, 2023. (World health Organization, Geneva, 2023).
Koelle, K., Martin, M. A., Antia, R., Lopman, B. & Dean, N. E. The changing epidemiology of SARS-CoV-2. Science 375, 1116–1121 (2022).
Rothan, H. A. & Byrareddy, S. N. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J. Autoimmun. 109, 102433 (2020).
China CDC. National Novel Coronavirus Infection Epidemic Situation. https://www.chinacdc.cn/jkzt/crb/zl/szkb_11803/jszl_13141/202304/t20230429_265709.html. Accessed June 14, 20232023.
Qu, P. et al. Enhanced neutralization resistance of SARS-CoV-2 Omicron subvariants BQ.1, BQ.1.1, BA.4.6, BF.7, and BA2752. Cell Host Microbe 31, 9–17 (2023).
Wang, Q. et al. Alarming antibody evasion properties of rising SARS-CoV-2 BQ and XBB subvariants. Cell 186, 279-286 e278 (2023).
Ren, S. Y., Wang, W. B., Gao, R. D. & Zhou, A. M. Omicron variant (B.1.1.529) of SARS-CoV-2: Mutation, infectivity, transmission, and vaccine resistance. World J. Clin. Cases 10, 1–11 (2022).
Niu, B., Ji, S., Zhao, S. & Lei, H. Timing and magnitude of the second wave of the COVID-19 Omicron variant—189 Countries and Territories, November 2021 to February 2023. China CDC Wkly. 5, 397–401 (2023).
Consortium, W. H. O. S. T. et al. (2021) Repurposed antiviral drugs for Covid-19—Interim WHO solidarity trial results. N. Engl. J. Med. 384, 497–511.
Dryden-Peterson, S. et al. Nirmatrelvir plus ritonavir for early COVID-19 in a large U.S. Health system: A population-based cohort study. Ann. Intern. Med. 176, 77–84 (2023).
Vassilopoulos, A. & Mylonakis, E. In patients with COVID-19 at risk for severe disease, nirmatrelvir + ritonavir reduced hospitalization or death. Ann. Intern. Med. 175, JC63 (2022).
Hammond, J. et al. Oral nirmatrelvir for high-risk, nonhospitalized adults with Covid-19. N. Engl. J. Med. 386, 1397–1408 (2022).
Jayk Bernal, A. et al. Molnupiravir for oral treatment of Covid-19 in nonhospitalized patients. N. Engl. J. Med. 386, 509–520 (2022).
Khoo, S. H. et al. Molnupiravir versus placebo in unvaccinated and vaccinated patients with early SARS-CoV-2 infection in the UK (AGILE CST-2): A randomised, placebo-controlled, double-blind, phase 2 trial. Lancet Infect. Dis. 23, 183–195 (2023).
Butler, C. C. et al. Molnupiravir plus usual care versus usual care alone as early treatment for adults with COVID-19 at increased risk of adverse outcomes (PANORAMIC): An open-label, platform-adaptive randomised controlled trial. Lancet 401, 281–293 (2023).
Zhang, J.-L. et al. Azvudine is a thymus-homing anti-SARS-CoV-2 drug effective in treating COVID-19 patients. Signal Transduct. Target. Ther. 6, 414 (2021).
Ren, Z. et al. A randomized, open-label, controlled clinical trial of azvudine tablets in the treatment of mild and common COVID-19, a pilot study. Adv. Sci. (Weinheim, Baden-Wurttemberg, Germany) 7, e2001435 (2020).
da Silva, R. M. et al. Serial viral load analysis by DDPCR to evaluate FNC efficacy and safety in the treatment of mild cases of COVID-19. Front. Med. 10, 1143485 (2023).
Gao, Y. et al. Antiviral effect of azvudine and nirmatrelvir-ritonavir among hospitalized patients with COVID-19. J. Infect. 86, e158–e160 (2023).
Petrakis, V., Rafailidis, P., Trypsianis, G., Papazoglou, D. & Panagopoulos, P. The antiviral effect of nirmatrelvir/ritonavir during COVID-19 pandemic real-world data. Viruses 15, 976 (2023).
Gao, Y., Liu, M., Li, Z., Xu, J., Zhang, J. & Tian, J. Molnupiravir for treatment of adults with mild or moderate COVID-19: A systematic review and meta-analysis of randomized controlled trials. Clin. Microbiol. Infect., (2023).
Zhou, Z. et al. Clinical characteristics of older and younger patients infected with SARS-CoV-2. Aging (Albany NY) 12, 11296–11305 (2020).
Vujcic, I. Outcomes of COVID-19 among patients with liver disease. World J. Gastroenterol. 29, 815–824 (2023).
Przekop, D., Gruszewska, E. & Chrostek, L. Liver function in COVID-19 infection. World J. Hepatol. 13, 1909–1918 (2021).
Yu, D. et al. Liver injury in COVID-19: Clinical features and treatment management. Virol. J. 18, 121 (2021).
Grandvuillemin, A., Rocher, F., Valnet-Rabier, M. B., Drici, M. D. & Dautriche, A. French Pharmacovigilance, N. Pharmacovigilance follow-up of patients in the context of the COVID-19 pandemic. Therapie, (2023).
Lory, P. et al. Safety profile of the lopinavir/ritonavir combination before and during the SARS-CoV-2 pandemic. Therapie 78, 419–425 (2022).
Casalini, G., Giacomelli, A. & Antinori, S. Liver tests abnormalities with licensed antiviral drugs for COVID-19: A narrative review. Expert Opin. Drug Saf. 21, 1483–1494 (2022).
Painter, W. P. et al. Human safety, tolerability, and pharmacokinetics of molnupiravir, a novel broad-spectrum oral antiviral agent with activity against SARS-CoV-2. Antimicrob. Agents Chemother. 65, 10–1128 (2021).
Kale, A., Shelke, V., Dagar, N., Anders, H. J. & Gaikwad, A. B. How to use COVID-19 antiviral drugs in patients with chronic kidney disease. Front. Pharmacol. 14, 1053814 (2023).
Izzedine, H., Jhaveri, K. D. & Perazella, M. A. COVID-19 therapeutic options for patients with kidney disease. Kidney Int. 97, 1297–1298 (2020).
Sun, Y. et al. Oral Azvudine for hospitalised patients with COVID-19 and pre-existing conditions: A retrospective cohort study. ClinicalMedicine 59, e101981 (2023).
Parums, D. V. Editorial: Rebound COVID-19 and cessation of antiviral treatment for SARS-CoV-2 with paxlovid and molnupiravir. Med. Sci. Monit. 28, e938532 (2022).
Anderson, A. S., Caubel, P., Rusnak, J. M. & Investigators, E.-H.T. Nirmatrelvir–ritonavir and viral load rebound in Covid-19. N. Engl. J. Med. 387, 1047–1049 (2022).
Charness, M. E. et al. Rebound of SARS-CoV-2 infection after nirmatrelvir-ritonavir treatment. N. Engl. J. Med. 387, 1045–1047 (2022).
Rubin, R. From positive to negative to positive again-the mystery of why COVID-19 rebounds in some patients who take paxlovid. JAMA 327, 2380–2382 (2022).
Zhou, Z. G. et al. Low-dose corticosteroid combined with immunoglobulin reverses deterioration in severe cases with COVID-19. Signal Transduct. Target. Ther. 5, 276 (2020).
Acknowledgements
This study was funded by the Key Research & Developmenta Program of Hunan Province (Numbers 2022SK2047 and 2020SK3014), and the Natural Science Foundation of Changsha city (Number kq2208448).
Author information
Authors and Affiliations
Contributions
Z.G.Z. and M.P.C. conceived and coordinated the study, designed, performed and analyzed the experiments, wrote the paper. D.X.J., J.X.R. and H.B.Z. carried out the data collection, data analysis, and revised the paper. All authors reviewed the results and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, MP., Jiang, DX., Rang, JX. et al. Comparison of azvudine, molnupiravir, and nirmatrelvir/ritonavir in adult patients with mild-to-moderate COVID-19: a retrospective cohort study. Sci Rep 14, 3318 (2024). https://doi.org/10.1038/s41598-024-53862-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-53862-y
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.