Abstract
While low winter temperatures are associated with increased mortality, this phenomenon has been suggested to be most severe in regions with seemingly mild winters. The study aimed to establish a temperature-based formula that could elucidate the previously ambiguous regional differences in vulnerability to low temperature. European weekly mortality data (2000–2019) were matched with meteorological data to determine for each region vulnerability to temperature decrease and the optimal temperature with lowest mortality. Regression models were developed to generalize and explain these findings considering regional temperature characteristics. Optimal temperature could be predicted based on local average summer temperature (R2 = 85.6%). Regional vulnerability to temperature decrease could be explained by combination of winter and summer temperatures (R2 = 86.1%). Regions with warm winters and cold summers showed the highest vulnerability to decrease of temperature during winter. Contrary to theories about economic disparities Eastern Europe exhibited resistance comparable to Scandinavia. The southern edges of Europe demonstrated serious low temperature vulnerability to decreased temperatures, even if temperature was relatively high around 20 °C. This suggests that the observed connection primarily reflects the modulation of the length of respiratory virus infection seasons by climate conditions, counterbalanced by varying levels of acquired immunity and the presence of heatwaves eliminating the most frail individuals. Thus, relatively low vulnerability and a flat mortality cycle in countries with harsh climates paradoxically imply the presence of threats throughout the whole year.
Similar content being viewed by others
Introduction
Observed differences in vulnerability to temperature are often attributed to local cultural or infrastructural adaptations to the prevailing conditions1. This interpretation finds some support in prior studies, which have noted regional variations in the optimal temperature for humans, with warmer regions generally exhibiting slightly higher optimal temperatures2,3. However, attempts to identify the actual factors that contribute to significant disparities have proven challenging. The Eurowinter Group conducted a comparative study involving European populations and found very faint differences. For instance, at a temperature of 7 °C, Finnish houses maintained a slightly higher average temperature than Greek (21.7 °C vs. 19.2 °C), and although the clothing surface area was similar, Finns were more likely to wear hats or gloves4. While this explanation implies acclimatization to a usual temperature range, it is noteworthy that the primary contributor to temperature related mortality is not extreme cold or heat, but rather moderate cold temperatures3. Furthermore, the theory that local populations are optimally adapted to their climate struggles to account for cases when the annual cycle is interrupted, as years with exceptionally mild winters correspond to lower mortality rates5,6. Conversely, in the aftermath of lifting COVID-19 restrictions, those same countries experienced out-of-season epidemics that were no longer suppressed7. Additionally, local adaptations alone cannot explain the clear pattern of late summer and early autumn having the lowest mortality, while the same conditions are not as favorable a few months earlier, which is especially noticeable in warmer countries with higher annual mortality amplitudes8,9.
While the increasing number of infections during winter is uncontroversial, the interpretation of their relationship with cold-related mortality remains contentious within the literature. Certain studies openly acknowledged influenza epidemics, but consider it as confounding factor when analyzing impact of cold weather on mortality4,10. Conversely, other findings highlighted influenza or other infections as a significant contributing factor to cold-related mortality3,11. Moreover, some research either openly suggest that additional mortality in winter is primarily caused by infections12 or implicitly, by successfully estimating the death toll associated with common viruses13. The mortality estimates attributed to nine well-monitored viruses are significant enough to account for a substantial portion of the excess mortality observed during winter. Furthermore, the superposition of these viruses' impact exhibits a resemblance to the overall observed mortality cycle13.
There are multiple studies suggesting a potential relationship between winter mortality and social deprivation, which is clearly correlated on regional level. While such a regional relationship was observed in Portugal, it lacked age control14. Considering the economic migration of young people, it is expected that the remaining population of retirees would exhibit a higher unadjusted mortality rate due to the age composition. Moreover, when crudely controlling for climate and age structure in a US dataset, the relationship does not appear to be robust, as various causes of death are predicted by distinct socio-economic markers15. Additionally, initial theories proposing fuel subsidies as a factor in reducing winter mortality in Britain16 have been challenged, with subsequent research suggesting that the observed difference is primarily attributable to variations in influenza strains12. There is a study indicating a correlation with a mix of climatic, socio-economic, and infrastructure factors, which, on the surface, seems methodologically sound. However, this study leaves unanswered questions, particularly regarding its model's suggestion that winter mortality falls with double glazing but rises with floor isolation17. Furthermore, in the case of analyzing the north–south divide, there are intertwined observations of climate factors, climate-adapted infrastructure and economic disparities.
Previous works measured regional differences in annual mortality cycles but were less successful in generalizing the underlying mechanism. They notably detected a relationship between Excess Winter Mortality (EWM) and climate18, with the highest mortality amplitude observed around latitude 35, gradually decreasing towards the equator and poles12,19. Additionally, while analyzing the roles of climate and economic factors, prior works did not leverage the natural experiment provided by Eastern Europe, which combines the harsh climate of Northern Europe with the economic development of Southern Europe. The purpose of this article is to investigate whether the observed regional differences in optimal temperature and vulnerability to low temperatures could be attributed to simple climatic patterns. The detection of such patterns could provide valuable insights into the underlying mechanisms driving these variations.
Methods
Data source
For this study, mortality data in ISO-weeks for NUTS1 regions from Eurostat for the period 2000-W01 to 2019-W52, covering 72.9 million deaths, were selected20. These data were combined with information from the European Climate Assessment and Dataset21, which contains data from 7050 meteorological stations. The regional climate data were based on the period from 1995-W01 to 2019-W52.
Calculation
Weather stations located above 1250 m were excluded due to their lack of representativeness for major population centers. To account for potential projection and rounding errors encountered with stations located on the edges of regions (such as sea shores or minor mountain peaks), a tolerance level of 10 km was applied during the matching process. This allowed them to be linked with more than one region if applicable, resulting in the creation of a dataset comprising 7130 region/station pairs. Subsequently, the regional time series underwent a deduplication process. For each region, the daily median temperature across stations was calculated to mitigate the impact of extreme observations, and from these medians, a weekly average temperature was derived.
While previous studies often focused on average annual14 or winter temperatures4,15,16, we took inspiration from the Köppen–Geiger climate classification system22. This system typically employs two proxy variables related to the average temperatures of colder and warmer seasons. For modeling consistency, we had to standardize these seasons length owing to their diverse durations in the original classification. To ensure robustness and accommodate minor regional variations in the timing of warmer and colder seasons, we calculated average temperatures by considering observations above or below the regional median, further referred to as summer and winter temperatures.
Previous studies have indicated that the specific temperature measure used does not appear to be relevant, but properly considering the lag is highly relevant23. However, the lagged impact of high and low temperature is different. Heatwaves cause death almost immediately; however, they are followed by around 2 weeks of below-trend mortality, as there is observed a very strong harvesting effect24,25. Especially during less intense heatwaves, the majority of casualties are expected to include individuals in the final days of their lives, and it would be desirable not to overestimate this impact. The impact of low temperatures is mediated through an indirect, delayed mechanism. The relationship between mortality and temperature displays a peak around a single-week lag1,11 before gradually diminishing, with noticeable impact diminishing after 3 weeks1,5. To further complicate the issue some works suggest that the best fit lag undergoes some subtle fluctuations over annual cycles26,27. The lag of 3 weeks, typically used in the literature1,2,3,5,28, seems to be the most suitable approach, though due to mortality data being available in weeks, this means comparing mortality in week n against temperature in weeks n to n-2.
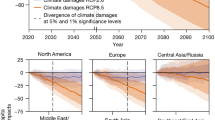
Logarithmic normalization was applied to regional weekly mortality data and they were decomposed using STL (Seasonal and Trend decomposition using Loess) to eliminate regional trend and magnitude. This allowed for the extraction of the relative seasonal component and relative residuals. The resulting data was then transformed into percentage deviation from the trend. These regional time series were plotted alongside the corresponding temperature data for each region, as depicted in Fig. 1 for selected regions. The selection of the presented areas was based on those that aligned with the study conducted by Gasparrini et al.3, with the inclusion of a few additional from eastern part of the European continent. Loess trend lines were employed to depict the relation between mortality. The optimal temperature for each region was identified as the temperature corresponding to the lowest mortality rate, after excluding observations falling within the first and last percentile. A subset of observations within the temperature range from 1 °C to the optimal temperature was selected for each region to calculate the slope using the Theil–Sen estimator. Subsequently regression models explaining optimal temperature and low temperature vulnerability based on climate variables were calculated, what is presented in Fig. 2.
The calculations were performed in Python 3.10 with its inbuilt library math and using libraries such as pandas 1.4.3 and numpy 1.21.1. The map was processed using geopandas 0.13.2, and the coordinates were converted using pyproj 3.5.0. The weather stations were matched with regions using shapely.geometry 1.7.1. Trends were calculated using statsmodels 1.13.5 and numpy, and the results were visualized using matplotlib 3.7.1 and geopandas. 95% confidence intervals (CI) were employed.
Results
The association between the average temperature of the preceding three weeks and mortality changes compared to the baseline was depicted in Fig. 1. Employing Loess instead of splines maintained the characteristic U-shaped trend, albeit with a less pronounced slope due to reduced sensitivity to extreme values. Notably, at both the lower and upper ends of the temperature range, mortality exhibited not only an overall increase but also a growing upward dispersion, leading to the selection of the central band for further analysis. At low temperatures, increased dispersion was attributable to the modulation of winter infections without affecting the severity of circulating strains. Conversely, high temperatures exhibited a harvesting effect, predominantly impacting individuals who were already frail, resulting in somewhat lower mortality in subsequent weeks in spite of continuously elevated temperature. Contrary to economic-based theories, cities like Warsaw or Budapest exhibited robust resistance to low temperatures, similar to Stockholm or Berlin. Within the typical temperature range, there was a nearly linear trend between decreasing temperature and increasing mortality. Remarkably, the deadly impact of low temperatures was evident in the southern edges of Europe even around 20 °C.
Figure 2 illustrates the climate conditions of European regions and their correlation with vulnerability to low temperatures and the temperature at which mortality is the lowest. The temperature gradient in Europe is influenced not only by the north–south difference in solar irradiance but also by a discernible east–west divide due to the Gulf Stream. This warm oceanic current stream provides the western part of the continent with a milder climate, characterized by unusually warm winters relative to their latitude. This geographical pattern aligns well with the vulnerability to low temperatures, explaining why the mortality pattern observed in London resembles that of Madrid more than Stockholm. The vulnerability to low temperature followed an exponential relationship with climate factors. High winter temperature was the main predictor (coefficient: 0.137; CI 0.124–0.148), while high summer temperature was observed to reduce vulnerability (coefficient: − 0.076; CI − 0.092 to − 0.061). Additionally, there was a constant component (coefficient: − 3.756; CI − 3.967 to − 3.545). Given the exponential nature of the relationship, regions with warm winters and relatively cold summers experience heightened vulnerability to cold. Furthermore, the optimal temperature is 79.6% (CI 73.0% to 86.2%) of the average summer temperature in Celsius plus 4.56 °C (CI 3.44 to 5.68).
Discussion
The observed phenomena can be aptly explained by considering basic climate variables. While the traditional focus of inquiry regarding winter mortality revolves around the puzzling question of why seemingly almost favorable conditions can turn staggeringly deadly in certain regions, a shift in perspective reveals a more suitable question. It becomes important to understand the conditions that allow individuals to live long enough to become vulnerable. The model provides an answer by suggesting that people fortunate enough to reside in climates where they neither face harsh winters nor heatwaves are particularly likely to have a higher chance of surviving until they become frail and succumb in less than optimal conditions. Conversely, in harsher climates, the lower annual amplitude of mortality also becomes easily explainable, as the conditions are unfavorable for most of the year. Similarly, at temperatures decreasing below zero the linear relationship starts to break as if the factor has already exhausted its impact.
The majority of our findings are in line with previous studies. Results for Eastern Europe were highly consistent with those of Germany or Scandinavia, indicating that the observed patterns in these countries followed climate rather than economic development level. However, the use of Loess instead of splines in our analysis inadvertently leads to somewhat different conclusions regarding the impact of high temperatures. In previous studies, a very steep increase in mortality was observed due to high temperatures. In our study, we find that the impact of temperatures deviating above the optimum was comparable to the impact of temperatures deviating below the optimum. In case of more robust fitting, provided a more balanced representation of the data as prolonged periods of warm spell tended to have mortality below the baseline. We consider the previous fitting predominantly as a visualization of the outlier bias, as prior models effectively predict an impending and deadly natural disaster if such weather conditions persist. However, in countries where these conditions do persist, they instead result in an increase in the optimal temperature. Even with temperatures reaching levels considered high by local standards, there is only moderately higher number of fatalities observed.
As the lag for low temperature and deaths necessitates an intermediate factor, respiratory viral infections exhibit many parallels. For instance, the lag between a decrease in temperature and an upswing in respiratory visits is strikingly similar29,30. While these viruses typically peak during winter, this seasonal pattern is most pronounced in intermediate climate zones but not in northern latitudes31 or equatorial32. The onset of the recent COVID-19 pandemic served as a natural experiment to elucidate the modulation mechanism by providing interruption of a non-climatic nature, followed by an ultimate significant rebound in infections. During the initial phase of the pandemic, due to restrictions and voluntary behavior changes, respiratory infection visits33,34 and mortality reduced7,35. This was accompanied by a decreasing detectable antibody level for common viruses36. Nevertheless, in the aftermath of the lifting of pandemic restrictions, there was an extraordinary and out-of-season rebound of those infections37,38, with the increase in mortality being the strongest in countries that were the most successful in containing the pandemic7.
While only a minority of EWM deaths are officially certified as caused by respiratory infection, there is a well-known issue of underdetection, even with the best-monitored viruses, which becomes pronounced during pandemic waves. While the COVID-19 pandemic highlighted underdetection39,40,41, in influenza pandemics, only a mere one fourth of influenza-associated deaths were even officially associated with respiratory illness42,43. Additionally, the same causes of death that were highly likely to be selected for influenza-associated deaths are the ones that show annual fluctuation, peaking throughout winter4,18,44.
Analysing the observed vulnerability to low temperature as epidemiological phenomenon starts to explain observed paradoxes. Within this framework prior works trying to establish whether the key to containing numerous concurrent respiratory outbreaks number lies in improving housing conditions14, fuel subsidies16, installing double glazing17 or donning slightly warmer clothing4 might seem a bit unconventional. Instead, the primary determinant for any endemic virus would be the underlying level of acquired immunity modulated by weather conditions29,45. This mechanism would be able to explain staggering differences in vulnerability between regions with shorter or longer infection season.
The model highlights an additional mechanism unrelated to infection spread, revealing that warm winters reduce vulnerability to cold, challenging the concept of adapting to a specific temperature range. A similar pattern of the most frail people finding some stressors partially interchangeable is well-documented: seasons with more deadly influenza correlate with subsequent reductions in heatwave deaths25,46,47,48, or notably deadly heatwaves lead to detectable lower mortality the following winter49. Despite earlier studies recognizing a broad connection between climate, particularly winter temperature, and EWM, the significance of summer temperature through the harvesting effect of heatwaves seems to have been neglected.
While prior studies have suggested a broad optimal temperature around the 75th percentile1, indicating some general trends, regional studies have revealed a more nuanced climate relationship50. This variation spans from the 60th percentile in tropical areas to approximately the 80–90th percentile in temperate regions3. This is consistent with the estimation for our sample at the 81st percentile, with a standard deviation of 5.9 percentiles. To the best of our knowledge, our contribution lies in being the first to formulate a predictive model for this nuanced climate relationship, shedding new light on the understanding of optimal temperature patterns.
Our findings significantly impact the interpretation of the impact of global warming, especially in light of Gasparrini et al.'s predictions, which suggest a significant increase in heat-related deaths due to global warming, combined with a modest reduction in winter deaths2. While they acknowledge assuming no adaptation, in light of our findings, they effectively assume that over the span of a century, the local climate-based relationship would remain constant despite the changing climate. Moreover, for the observed local relationships to hold under changing climate conditions, requires additionally existence of an unobserved mechanism in regions that currently experience infrequent heatwaves, ensuring the replenishment of a pool of highly vulnerable individuals every week. However, studies on the impact of heatwaves have found a completely opposite phenomenon. Heatwaves tend to lead to a harvesting effect, where mortality falls below the trend line in subsequent weeks, as those who were the most vulnerable have already succumbed24,25.
The assumption of a lack of adaptation is also hard to reconcile with literature as demonstrable cases of population suffering elevated mortality due to lack of adaptation, required to analyze migrants who moved to countries 10 °C colder than their country of origin51. Lifting the assumption that the local climate-based relationship would remain constant over the long run would paint a somewhat different picture of our future. After a challenging-to-quantify adjustment period, the new local relationship would be simply based on the new climate as derived from the formula. A warmer summer should lead to higher locally optimal temperatures, resulting in only a slight rise in the number of high-temperature deaths. Conversely, a warmer winter should shorten the infection season but make it more intense, paradoxically leading to an elevated number of deaths in winter in relation to the annual minimum. While this suggestion may seem paradoxical, that's exactly what we observe right now in the Mediterranean climate8,19.
Even with this enhanced extrapolation, it is most likely to not include the most important caveat. While the overall pattern of annual mortality cycles seems to have largely stabilized in the last half-century, suggesting a period of relative consistency, earlier dynamics clearly hinted that moderately high temperatures used to be a major environmental hazard before the widespread adoption of modern sanitary standards9,52,53. Nevertheless, even in recent decades, our resilience to environmental hazards is steadily increasing, as there has been both an observed decrease in EWM35,54 and a reduction in vulnerability to heatwaves54,55,56. Thus, the future relationship is likely in flux and depends not only on our climate but also on the relative success in mitigating specific threats.
Conclusion
The observed regional differences in optimal temperature and vulnerability to low temperature are clearly shaped by the local climate and are unlikely to remain constant under climate change. The linear relationship between summer temperature and optimal temperature implies that spline-based extrapolation is highly likely to overestimate mortality from temperature increase. As the relationship is typically climate-based, it was disrupted by COVID-19 restrictions. This strongly suggests that the observed connection primarily reflects the modulation of respiratory virus infection cycles by climate conditions. Differences in the length of the infection season, varying levels of acquired immunity, and the existence of other stressors eliminating the most frail individuals would well explain the underlying process. This would suggest that the situation is not most severe in countries with high EWM but paradoxically in those countries with harsher climates, as a flatter cycle and low vulnerability imply the steady presence of threats over the whole year.
Limitations
The model exclusively focused on calculating the impact of temperature, while characterizing climate under the Köppen–Geiger classification system includes three variables, with the omitted one being precipitation22. Although precipitation is likely to play a role, it is more challenging to model, given the unique preferences of particular viral strains. For example, influenza A is known to favor low humidity, while influenza B exhibits a preference for high humidity57. While we consider the most plausible interpretation of the role of warm summers as heatwave deaths, our model effectively detected climate continentality. Thus, it would be possible that there were some other coexisting, less conspicuous climate-related risks that, for model purposes, were indistinguishable, like higher daily temperature amplitudes. Attempting to incorporate these relationships would introduce additional layers of complexity with limited prospects for significantly enhancing predictive accuracy. For some countries, time series were relatively short (e.g., 5 years for the UK). Although it did not affect the fitting, as bootstrapping did not cause any noticeable differences due to the extreme robustness of Theil–Sen estimator, there is an underlying issue of representativeness.
Data availability
The datasets analyzed during the current study are available in the Eurostat repository (mortality) https://ec.europa.eu/eurostat/databrowser/product/view/demo_r_mwk2_ts and ECAD (mean temperature) https://knmi-ecad-assets-prd.s3.amazonaws.com/download/ECA_blend_tg.zip
References
Guo, Y. et al. Global variation in the effects of ambient temperature on mortality: A systematic evaluation. Epidemiology 25, 781–789. https://doi.org/10.1097/EDE.0000000000000165 (2014).
Gasparrini, A. et al. Projections of temperature-related excess mortality under climate change scenarios. Lancet Planet Health 1, e360–e367. https://doi.org/10.1016/S2542-5196(17)30156-0 (2017).
Gasparrini, A. et al. Mortality risk attributable to high and low ambient temperature: A multicountry observational study. The Lancet 386, 369–375. https://doi.org/10.1016/S0140-6736(14)62114-0 (2015).
The Eurowinter Group. Cold exposure and winter mortality from ischaemic heart disease, cerebrovascular disease, respiratory disease, and all causes in warm and cold regions of Europe. The Lancet 349, 1341–1346. https://doi.org/10.1016/S0140-6736(96)12338-2 (1997).
Madaniyazi, L. et al. Seasonality of mortality under a changing climate: A time-series analysis of mortality in Japan between 1972 and 2015. Environ. Health Prev. Med. 26, 69. https://doi.org/10.1186/s12199-021-00992-8 (2021).
Hajat, S. Health effects of milder winters: A review of evidence from the United Kingdom. Environ. Health 16, 109. https://doi.org/10.1186/s12940-017-0323-4 (2017).
Walkowiak, M. P., Domaradzki, J. & Walkowiak, D. Unmasking the COVID-19 pandemic prevention gains: Excess mortality reversal in 2022. Public Health 223, 193–201. https://doi.org/10.1016/j.puhe.2023.08.004 (2023).
Falagas, M. E. et al. Seasonality of mortality: The September phenomenon in Mediterranean countries. CMAJ 181, 484–486. https://doi.org/10.1503/cmaj.090694 (2009).
Alcoforado, M. J. et al. Weather and climate versus mortality in Lisbon (Portugal) since the 19th century. Appl. Geogr. 57, 133–141. https://doi.org/10.1016/j.apgeog.2014.12.017 (2015).
Liddell, C., Morris, C., Thomson, H. & Guiney, C. Excess winter deaths in 30 European countries 1980–2013: A critical review of methods. J. Public Health 38, 806–814. https://doi.org/10.1093/pubmed/fdv184 (2016).
Linares, C., Diaz, J., Tobías, A., Carmona, R. & Mirón, I. J. Impact of heat and cold waves on circulatory-cause and respiratory-cause mortality in Spain: 1975–2008. Stoch. Environ. Res Risk Assess. 29, 2037–2046. https://doi.org/10.1007/s00477-014-0976-2 (2015).
Jones, R. P. Excess winter mortality (EWM) as a dynamic forensic tool: Where, when, which conditions, gender, ethnicity and age. Int. J. Environ. Res. Public Health 18, 2161. https://doi.org/10.3390/ijerph18042161 (2021).
van Asten, L. et al. Mortality attributable to 9 common infections: Significant effect of influenza A, respiratory syncytial virus, influenza B, norovirus, and parainfluenza in elderly persons. J. Infect. Dis. 206, 628–639. https://doi.org/10.1093/infdis/jis415 (2012).
Almendra, R., Santana, P. & Vasconcelos, J. Evidence of social deprivation on the spatial patterns of excess winter mortality. Int. J. Public Health 62, 849–856. https://doi.org/10.1007/s00038-017-0964-7 (2017).
Gonseth, S., Nusslé, S., Bovet, P., Panese, F. & Wiemels, J. L. Excess winter deaths caused by cardiovascular diseases are associated with both mild winter temperature and socio-economic inequalities in the U.S. Int. J. Cardiol. 187, 642–644. https://doi.org/10.1016/j.ijcard.2015.03.412 (2015).
Iparraguirre, J. Have winter fuel payments reduced excess winter mortality in England and Wales?. J. Public Health (Oxf) 37, 26–33. https://doi.org/10.1093/pubmed/fdu063 (2015).
Healy, J. D. Excess winter mortality in Europe: A cross country analysis identifying key risk factors. J. Epidemiol. Community Health 57, 784–789. https://doi.org/10.1136/jech.57.10.784 (2003).
Madaniyazi, L. et al. Seasonal variation in mortality and the role of temperature: A multi-country multi-city study. Int. J. Epidemiol. 51, 122–133. https://doi.org/10.1093/ije/dyab143 (2022).
Douglas, S. & Rawles, J. Latitude-related changes in the amplitude of annual mortality rhythm. The biological equator in man. Chronobiol. Int. 16, 199–212. https://doi.org/10.3109/07420529909019086 (1999).
Eurostat. Eurostat Databse. https://ec.europa.eu/eurostat/data/database (2023).
Home European Climate Assessment & Dataset. https://www.ecad.eu/ (2023).
Beck, H. E. et al. Present and future Köppen-Geiger climate classification maps at 1-km resolution. Sci. Data 5, 180214. https://doi.org/10.1038/sdata.2018.214 (2018).
Barnett, A. G., Tong, S. & Clements, A. C. A. What measure of temperature is the best predictor of mortality?. Environ. Res. 110, 604–611. https://doi.org/10.1016/j.envres.2010.05.006 (2010).
Saha, M. V., Davis, R. E. & Hondula, D. M. Mortality displacement as a function of heat event strength in 7 US cities. Am. J. Epidemiol. 179, 467–474. https://doi.org/10.1093/aje/kwt264 (2014).
Qiao, Z., Guo, Y., Yu, W. & Tong, S. Assessment of short- and long-term mortality displacement in heat-related deaths in Brisbane, Australia, 1996–2004. Environ. Health Perspect. 123, 766–772. https://doi.org/10.1289/ehp.1307606 (2015).
Rodrigues, M., Santana, P. & Rocha, A. Effects of extreme temperatures on cerebrovascular mortality in Lisbon: A distributed lag non-linear model. Int. J. Biometeorol. 63, 549–559. https://doi.org/10.1007/s00484-019-01685-2 (2019).
Rodrigues, M., Santana, P. & Rocha, A. Bootstrap approach to validate the performance of models for predicting mortality risk temperature in Portuguese Metropolitan Areas. Environ. Health 18, 25. https://doi.org/10.1186/s12940-019-0462-x (2019).
Achebak, H., Devolder, D., Ingole, V. & Ballester, J. Reversal of the seasonality of temperature-attributable mortality from respiratory diseases in Spain. Nat. Commun. 11, 2457. https://doi.org/10.1038/s41467-020-16273-x (2020).
Imai, C., Armstrong, B., Chalabi, Z., Mangtani, P. & Hashizume, M. Time series regression model for infectious disease and weather. Environ. Res. 142, 319–327. https://doi.org/10.1016/j.envres.2015.06.040 (2015).
Meerhoff, T. J., Paget, J. W., Kimpen, J. L. & Schellevis, F. Variation of respiratory syncytial virus and the relation with meteorological factors in different winter seasons. Pediatr. Infect. Dis. J. 28, 860. https://doi.org/10.1097/INF.0b013e3181a3e949 (2009).
Hawkes, M. T. et al. Seasonality of respiratory viruses at northern latitudes. JAMA Netw. Open 4, e2124650. https://doi.org/10.1001/jamanetworkopen.2021.24650 (2021).
Bloom-Feshbach, K. et al. Latitudinal variations in seasonal activity of influenza and respiratory syncytial virus (RSV): A global comparative review. PLoS ONE 8, e54445. https://doi.org/10.1371/journal.pone.0054445 (2013).
Tang, J. W. et al. Where have all the viruses gone? Disappearance of seasonal respiratory viruses during the COVID-19 pandemic. J. Med. Virol. 93, 4099–4101. https://doi.org/10.1002/jmv.26964 (2021).
Rodgers, L. et al. Changes in seasonal respiratory illnesses in the United States during the coronavirus disease 2019 (COVID-19) pandemic. Clin. Infect. Dis. 73, S110–S117. https://doi.org/10.1093/cid/ciab311 (2021).
Telfar-Barnard, L., Baker, M. G., Wilson, N. & Howden-Chapman, P. The rise and fall of excess winter mortality in New Zealand from 1876 to 2020. Int. J. Biometeorol. https://doi.org/10.1007/s00484-023-02573-6 (2023).
Reicherz, F. et al. Waning immunity against respiratory syncytial virus during the coronavirus disease 2019 pandemic. J. Infect. Dis. 226, 2064–2068. https://doi.org/10.1093/infdis/jiac192 (2022).
Riepl, A. et al. The surge of RSV and other respiratory viruses among children during the second COVID-19 pandemic winter season. Front. Pediatr. 11, 1112150. https://doi.org/10.3389/fped.2023.1112150 (2023).
Pruccoli, G. et al. The importance of RSV epidemiological surveillance: A multicenter observational study of RSV infection during the COVID-19 pandemic. Viruses 15, 280. https://doi.org/10.3390/v15020280 (2023).
WHO. Global Excess Deaths Associated with COVID-19 (Modelled Estimates). https://www.who.int/data/sets/global-excess-deaths-associated-with-covid-19-modelled-estimates (2023).
Walkowiak, M. P. & Walkowiak, D. Underestimation in reporting excess COVID-19 death data in Poland during the first three pandemic waves. Int. J. Environ. Res. Public Health 19, 3692. https://doi.org/10.3390/ijerph19063692 (2022).
Alicandro, G., Remuzzi, G., Centanni, S., Gerli, A. & La Vecchia, C. Excess total mortality during the Covid-19 pandemic in Italy: Updated estimates indicate persistent excess in recent months. Med. Lav. 113, e2022021. https://doi.org/10.23749/mdl.v113i2.13108 (2022).
Schanzer, D. L., Tam, T. W. S., Langley, J. M. & Winchester, B. T. Influenza-attributable deaths, Canada 1990–1999. Epidemiol. Infect. 135, 1109–1116. https://doi.org/10.1017/S0950268807007923 (2007).
Walkowiak, M. P. & Walkowiak, D. From respiratory diseases to nervous system disorders: Unraveling the certified causes of influenza-associated deaths in Poland from 2000 to 2019. Influenza Other Respir. Viruses 17, e13214. https://doi.org/10.1111/irv.13214 (2023).
Nakaji, S. et al. Seasonal changes in mortality rates from main causes of death in Japan (1970–1999). Eur. J. Epidemiol. 19, 905–913. https://doi.org/10.1007/s10654-004-4695-8 (2004).
Shaman, J. & Galanti, M. Will SARS-CoV-2 become endemic?. Science 370, 527–529. https://doi.org/10.1126/science.abe5960 (2020).
Rocklöv, J., Forsberg, B. & Meister, K. Winter mortality modifies the heat-mortality association the following summer. Eur. Respir. J. 33, 245–251. https://doi.org/10.1183/09031936.00037808 (2009).
Ha, J., Kim, H. & Hajat, S. Effect of previous-winter mortality on the association between summer temperature and mortality in South Korea. Environ. Health Perspect. 119, 542–546. https://doi.org/10.1289/ehp.1002080 (2011).
Stafoggia, M., Forastiere, F., Michelozzi, P. & Perucci, C. A. Summer temperature-related mortality: Effect modification by previous winter mortality. Epidemiology 20, 575–583 (2009).
Toulemon, L. & Barbieri, M. The mortality impact of the August 2003 heat wave in France: Investigating the ‘harvesting’ effect and other long-term consequences. Popul. Stud. 62, 39–53. https://doi.org/10.1080/00324720701804249 (2008).
Yang, J. et al. Cardiovascular mortality risk attributable to ambient temperature in China. Heart 101, 1966–1972. https://doi.org/10.1136/heartjnl-2015-308062 (2015).
Shor, E. & Roelfs, D. Climate shock: Moving to colder climates and immigrant mortality. Soc. Sci. Med. 235, 112397. https://doi.org/10.1016/j.socscimed.2019.112397 (2019).
Momiyama, M. Biometeorological study of the seasonal variation of mortality in Japan and other countries on the seasonal disease calendar. Int. J. Biometeorol. 12, 377–393. https://doi.org/10.1007/BF01553284 (1968).
Ekamper, P., Van Poppel, F., Van Duin, C. & Garssen, J. 150 Years of temperature-related excess mortality in the Netherlands. DemRes 21, 385–426. https://doi.org/10.4054/DemRes.2009.21.14 (2009).
Carson, C., Hajat, S., Armstrong, B. & Wilkinson, P. Declining vulnerability to temperature-related mortality in London over the 20th century. Am. J. Epidemiol. 164, 77–84. https://doi.org/10.1093/aje/kwj147 (2006).
Sheridan, S. C. & Dixon, P. G. Spatiotemporal trends in human vulnerability and adaptation to heat across the United States. Anthropocene 20, 61–73. https://doi.org/10.1016/j.ancene.2016.10.001 (2017).
Coates, L., Haynes, K., O’Brien, J., McAneney, J. & de Oliveira, F. D. Exploring 167 years of vulnerability: An examination of extreme heat events in Australia 1844–2010. Environ. Sci. Policy 42, 33–44. https://doi.org/10.1016/j.envsci.2014.05.003 (2014).
Caini, S., Alonso, W. J., Séblain, C.E.-G., Schellevis, F. & Paget, J. The spatiotemporal characteristics of influenza A and B in the WHO European Region: Can one define influenza transmission zones in Europe?. Eurosurveillance 22, 30606. https://doi.org/10.2807/1560-7917.ES.2017.22.35.30606 (2017).
Author information
Authors and Affiliations
Contributions
M.P.W. designed the original study. M.P.W. conducted data collection, analysis, and preliminary interpretation. M.P.W., D.W. and J.W. drafted the original manuscript. All authors edited and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Walkowiak, M.P., Walkowiak, D. & Walkowiak, J. Exploring the paradoxical nature of cold temperature mortality in Europe. Sci Rep 14, 3181 (2024). https://doi.org/10.1038/s41598-024-53675-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-53675-z
This article is cited by
-
Beyond the sine wave: unveiling climate-driven baseline mortality cycles
International Journal of Biometeorology (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.