Abstract
Rehabilitation improves symptoms, quality of life, and survival in patients with chronic respiratory or cardiovascular disease. We evaluated smartphone application-based rehabilitation programs for patients with chronic respiratory or cardiovascular diseases. This was a single-center prospective single arm study. Participants underwent smartphone application-based pulmonary or cardiac rehabilitation for 12 weeks. A total of 93 participants were recruited, and 75 visited after rehabilitation. Their median age was 67.0 (interquartile range, 60.0–70.8) years, and 60 (80.0%) were men. For patients with chronic respiratory disease (n = 41), VO2peak (median 13.7 to 15.4 ml/kg/min, P = 0.049), chronic obstructive pulmonary disease assessment test (median 14 to 6, P < 0.001), Euro-QoL 5-Dimension 5-Level (EQ-5D-5L) index (median 0.795 to 0.862, P = 0.001), and Health-related Quality of Life Instrument with 8 Items (HINT-8) index (median 0.784 to 0.855, P < 0.001) were significantly improved. For patients with chronic cardiovascular disease (n = 34), VO2peak (median 21.8 to 23.3, P = 0.007), EQ-5D-5L index (median 0.871 to 1.000, P = 0.037), and HINT-8 index (median 0.890 to 0.903, P < 0.001) were significantly improved. The smartphone application-based rehabilitation program improved exercise capacity and quality of life in patients with chronic respiratory or cardiovascular disease.
Trial registration: https://clinicaltrials.gov/ct2/show/NCT05383950 (20/05/2022).
Similar content being viewed by others
Introduction
Globally, chronic respiratory and cardiovascular diseases remain important causes of mortality and morbidity1,2,3. In 2019, lung cancer, chronic obstructive lung disease (COPD), lower respiratory infections and ischemic heart disease are among the top-ten causes of disability-adjusted life-years among people over 50 years of age1. Individuals with chronic respiratory and cardiovascular diseases also experience various problems, including reduced exercise capacity and poor quality of life4,5,6,7,8.
Pulmonary rehabilitation is an intervention that can improve physical and psychological conditions of individuals with chronic respiratory disease via exercise training, behavior modification, and education5. Pulmonary rehabilitation has been shown to efficaciously improve the exercise capacity, dyspnea, and quality of life in patients with chronic respiratory disease4,5,9. Furthermore, muscle wasting and muscle dysfunction are common in chronic respiratory diseases, and result in decreased respiratory function and exercise capacity10,11. For the population affected by these conditions, pulmonary rehabilitation with exercise training and nutritional support can be the most effective alternative intervention11.
Cardiac rehabilitation is a component of a comprehensive treatment program that includes exercise training, medical treatment, and education to improve mortality and quality of life as well as reduce recurrence of individuals with chronic cardiovascular disease6,7,8. Increased exercise capacity has been found to be correlated with reduced mortality risk12, and increased physical activity was associated with reduced mortality risk in individuals with cardiovascular disease13.
However, participating in center-based rehabilitation has remained challenging for patients with chronic respiratory and cardiovascular diseases due to transportation barriers, lack of facilities and motivation, and low social support14,15,16. Recently, evidence supporting the effectiveness and feasibility of home-based pulmonary and cardiac rehabilitation compared with center-based rehabilitation has increased17,18. Furthermore, obstacles to practicing face-to-face rehabilitation programs during the COVID-19 pandemic have prompted the development of telerehabilitation alternatives to center-based rehabilitation for chronic respiratory and cardiovascular disease treatment19,20. Therefore, we developed a smartphone application and aimed to evaluate the efficacy of smartphone application-based rehabilitation programs to improve exercise capacity and quality of life of patients with chronic respiratory or cardiovascular disease.
Methods
Study design
This was a single-center prospective single arm study designed to evaluate the clinical efficacy of smartphone application-based rehabilitation in patients with chronic respiratory or cardiovascular disease. In 2022, 90 participants from Asan Medical Center, comprising 50 and 40 patients with chronic respiratory and cardiovascular disease, respectively, were recruited. Participants were screened at outpatient clinics of the pulmonology and cardiology departments. Subsequently, they were assigned to the pulmonary and cardiac rehabilitation program, respectively.
Participants were provided with the smartphone application and performed an application-based self-directed rehabilitation program for the entire intervention duration of 12 weeks. They were evaluated at the baseline and at the end of the rehabilitation.
The study protocol was approved by the Institutional Review Board of Asan Medical Center (Approval number: 2022-0562). Written informed consent was obtained from all participants prior to inclusion. This study complied with the guidelines stipulated in the Declaration of Helsinki and all methods were performed in accordance with the relevant guidelines. Finally, this study was registered in the ClinicalTrials.gov database (NCT05383950, https://clinicaltrials.gov/ct2/show/NCT05383950, 20/05/2022).
Study participants
Patients with a clinically diagnosed chronic respiratory or cardiovascular disease were recruited at the outpatient clinic of Asan Medical Center. The inclusion criteria were as follows: (1) aged 20–80 years; (2) dyspnea score ≥ 1 in the modified Medical Research Council (mMRC) or scale ≥ I in the New York Heart Association Functional Classification (NYHA); and (3) had a chronic respiratory or cardiovascular disease and underwent regular medications. Chronic respiratory diseases included (1) obstructive lung disease, such as asthma and COPD (defined as exhibiting a forced expiratory volume in one second [FEV1] < 80% of the predicted value or a FEV1/forced vital capacity [FVC] < 0.7), (2) bronchiectasis (defined as bronchiectasis visualized in more than one lobe of the lungs via chest computed tomography), or (3) restrictive lung disease, such as tuberculous lung destruction and interstitial lung disease (defined as an FVC or diffusing capacity for carbon monoxide [DLCO] < 80% of the predicted value)21. Chronic cardiovascular diseases included (1) ischemic heart disease (defined as coronary artery reperfusion therapy for myocardial infarction or angina pectoris) and (2) heart failure (defined as a left ventricular ejection fraction < 50% as measured by echocardiography)22. The exclusion criteria were as follows: (1) an acute exacerbation of underlying disease within 4 weeks immediately before enrollment; (2) inability to perform the rehabilitation program due to disability; and (3) inability to run the smartphone application.
Smartphone application and rehabilitation program
The smartphone application (SENIORS) was developed by LifeSemantics Corp. (Seoul, Republic of Korea). Briefly, investigators reviewed existing smartphone applications, the relevant scientific literature, and rehabilitation guidelines to design an application and related rehabilitation programs4,5,6,23,24. The application was developed on the Android platform (requiring at least Android 8.0). The application provides exercise programs, records, and partners, and disease education (Fig. 1). Pulmonary rehabilitation comprises one level of the exercise program and cardiac rehabilitation comprises three levels of the exercise program and includes different anaerobic exercises. Each exercise program consisted of two 30-min periods of aerobic and anaerobic exercise, respectively. Participants practiced various core and limb muscle exercises, and the exercise level increased weekly (Supplementary Table 1). Finally, participants could earn rewards that depended on their exercise records.
Screenshots of the “SENIORS” application. Shown are: (A) Opening screen (B) Home menu, which displays daily and total exercise records of the user and an exercise partner. (C) Each exercise program could be selected in a daily exercise schedule menu. (D) Rating of perceived exertion (RPE) scale, which were evaluated after each exercise. (E) Instructions for walking exercises. (F) Step counter and timer for walking exercises.
Study outcome
The primary outcome was peak oxygen uptake (VO2peak) as measured by the cardiopulmonary exercise test after the end of rehabilitation25. A cardiopulmonary exercise test was performed based on incremental protocol25. For patients with chronic respiratory disease, cycle ergometer (VIAsprint 150P; Carefusion, San Diego, CA, USA) and metabolic cart (Vmax 29; SensorMedics, Yorba Linda, CA, USA) were used. For patients with chronic cardiovascular disease, treadmill (COSMED T150 DE; h/p/cosmos sports & medical, Nussdorf-Traunstein, Germany) and metabolic cart (Quark CPET; COSMED, Rome, Italy) were used. Secondary outcomes after the end of rehabilitation included dyspnea scores, responses to quality of life questionnaires, lung function (for chronic respiratory disease), exercise time, and metabolic equivalents (METs) during a cardiopulmonary exercise test (for chronic cardiovascular disease), and a limb muscle test. Dyspnea symptoms were assessed using the mMRC dyspnea scale (for chronic respiratory disease) and NYHA class (for chronic cardiovascular disease). Quality of life questionnaires included the Euro-QoL 5-Dimension 5-Level (EQ-5D-5L)26,27, Health-related Quality of Life Instrument with 8 Items (HINT-8) questionnaire28,29,30, and COPD assessment test (CAT, for chronic respiratory disease)31. EQ-5D-5L and HINT-8 index scores were calculated based on previous studies29,30,32. Lung function was quantified by FVC, FEV1, and DLCO21. The limb muscle tests included hand grip strength and limb muscle mass as measured by bioelectrical impedance analysis33,34.
Sample size calculation
The sample size was calculated to determine the significance of improvements in the primary outcome between baseline and after rehabilitation based on previous studies. For pulmonary rehabilitation, a previous study demonstrated that baseline and after rehabilitation VO2peak measurements had mean values of 13.2 ± 3.0 and 14.8 ± 4.1 ml/kg/min, respectively35. We assumed that the participants’ mean baseline VO2peak was 13.2 ± 3.0 ml/kg/min, and therefore resulted in a 10% increase after rehabilitation. To achieve an alpha of 0.05 and a power of 80%, at least 41 participants were required. Moreover, to allow a 20% drop-out, 50 participants were required. For cardiac rehabilitation, we noted that a previous study demonstrated that the mean baseline and after rehabilitation VO2peak values were 22.8 ± 4.2 and 26.0 ± 4.0 ml/kg/min, respectively36. Therefore, we assumed that the participant mean baseline VO2peak was 23.0 ± 4.0 ml/kg/min, resulting in a 10% increase after rehabilitation. To achieve an alpha of 0.05 and a power of 80%, at least 31 participants were required. To account for an anticipated drop-out rate of 20%, 40 participants were required.
Statistical analysis
Continuous variables were presented as medians [interquartile range (IQR)] and were compared using Wilcoxon signed rank tests. Categorical variables were presented as counts (percentages). All P-values were two-tailed, with the threshold of statistical significance set to P < 0.05. All statistical analyses were performed using SPSS version 26.0 (Statistical Package for the Social Sciences, IBM SPSS Corporation, Armonk, NY, USA).
Results
Participant baseline characteristics
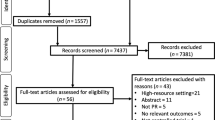
Figure 2 shows the flowchart of the study process. A total of 93 participants were recruited (48 and 45 from the pulmonary and cardiac departments, respectively), and 85 started rehabilitation (46 and 39 from the pulmonary and cardiac departments, respectively). Finally, 75 (41 and 34 from the pulmonary and cardiac departments, respectively) visited after rehabilitation, resulting in 20% withdrawal rate37,38. Table 1 shows the baseline characteristics of the study participants. Their median age was 67.0 (IQR, 60.0–70.8) years and 60 (80.0%) were men. Fifty-six (74.7%) participants had a history of smoking. Of the 41 participants with chronic respiratory disease, 33 had obstructive lung disease and eight had bronchiectasis. All 34 participants with chronic cardiovascular disease had ischemic heart disease.
Clinical parameters of participants
Among participants with chronic respiratory diseases, their VO2peak was significantly improved (P = 0.049). Moreover, we observed significant improvement in CAT score (P < 0.001), EQ-5D-5L index (P = 0.001), and HINT-8 index (P < 0.001; Table 2, Fig. 3). Among participants with chronic cardiovascular disease, we observed significant improvement in VO2peak (P = 0.007) and METs (P = 0.011). Significant improvement was also evident in the duration (exercise time) of the cardiopulmonary exercise test (P < 0.001), EQ-5D-5L index (P = 0.037), and HINT-8 index (P < 0.001; Table 3, Fig. 3). No participants experienced disease exacerbation or musculoskeletal injury related to rehabilitation activities during the study period.
Participant compliance during rehabilitation
Participants who performed both aerobic and anaerobic exercises ≥ 30% of the entire study period of 84 days, based on the log data of application, were considered to be compliant participants. Among participants with chronic respiratory disease, 17 (41.5%) were compliant (aerobic exercise, median 19.0 days [IQR, 1.0–47.3] and anaerobic exercise, median 36.0 days [IQR, 2.8–56.3]). We observed significant improvement in VO2peak only in these compliant participants (P = 0.012). Among participants with chronic cardiovascular disease, only 5 (14.7%) were compliant (aerobic exercise, median 4.0 days [IQR, 0.0–21.0] and anaerobic exercise, median 3.5 days [IQR, 1.0–21.0]), and significant improvement in VO2peak was observed regardless of compliance (Fig. 4).
HINT-8 distribution
To evaluate which dimensions of quality of life improved during rehabilitation, we subsequently analyzed the distribution of HINT-8 results by item and level. Participants with chronic respiratory disease reported significant improvements in all dimensions measured by HINT-8 except for climbing stairs. Participants with chronic cardiovascular disease reported significant improvement in terms of vitality, depression, and memory (Supplementary Table 2).
Ease-of-use of the application
Approximately 80% of participants indicated that they perceived the application as easy to use (i.e., “very easy,” 68.0% of participants; “easy,” 14.7% of the participants) and were accustomed to using the application within 3 days (i.e., 64.0% and 21.3% within 1 and 3 days, respectively). Moreover, approximately two-thirds (65.3%) of the participants indicated that they wanted to use the application if it were commercially available. The most attractive point of the application was that it was a physician-designed exercise program (as indicated by 37.3% of respondents, Supplementary Table 3).
Discussion
In this study, we evaluated a smartphone application-based rehabilitation program for patients with chronic respiratory and cardiovascular diseases. We found that the smartphone application-based rehabilitation program improved the clinical outcomes of participants, including exercise capacity and quality of life. Furthermore, older adult patients with chronic diseases can easily perform the rehabilitation program. Thus, smartphone application-based rehabilitation may be a useful treatment option for older adult patients with chronic diseases.
Exercise capacity and physical activity are important prognostic indicators for patients with chronic respiratory and cardiovascular disease. For example, exercise capacity has been found to be an important predictor of mortality in patients with COPD39. In addition, low levels of physical activity were found to be correlated with high risks for disease exacerbation and mortality in patients with COPD40. Similarly, higher exercise capacity was correlated with reduced mortality risk in patients with chronic cardiovascular diseases12, while high levels of physical activity resulted in reduced mortality risk in patients with cardiovascular disease13. This study demonstrated that exercise capacity can improve via an application-based rehabilitation program in older adult patients with chronic disease. Unfortunately, physical activity levels, such daily step counts, were not measured in this study. This would be simple to implement since it could be measured using a smartphone-mounted pedometer. Thus, further development of the application is required to obtain this data.
We found that the application-based rehabilitation program was associated with significantly improved quality of life for all groups of participants. In particular, patients with chronic respiratory disease reported significant improvements in CAT score, a predictor of the severity of airflow limitation and acute exacerbation in patients with COPD41,42. By improving exercise capacity and quality of life through rehabilitation programs, clinical outcomes such as disease exacerbation may be improved. We noted that no patient experienced acute disease exacerbation during the study period. Therefore, further studies are needed to evaluate the effect of rehabilitation on acute exacerbation or mortality using long-term follow-up assessments performed after the end of rehabilitation.
As previously described, compliance to rehabilitation program is an important issue in home-based rehabilitation43. A previous study reported an estimated − 0.22 (95% CI, − 0.74–0.31) decrease in the CAT score in every 7-day increase in application use for pulmonary rehabilitation44. However, another study reported that as time passed, the number of smartphone application users undergoing pulmonary rehabilitation decreased45. Therefore, to steadily use the application and perform rehabilitation program, initial professional assessment and goal setting are important46. Enabling self-monitoring and self-evaluation, such as feedback using wearable device and adjustable exercise program, is also important in real-world practice46. Moreover, patients’ preferences should be considered in designing eHealth platforms to enhance user engagement47.
In this study, participants showed low levels of compliance, which was only 14.7% among participants with chronic cardiovascular disease. However, in the subgroup analysis, significant improvement in VO2peak was noted in compliant participants with chronic pulmonary disease. In a previous study of home-based pulmonary rehabilitation without supervision, participants with good compliance showed significant improvement in clinical indices compared with non-compliant participants48. Because the lack of motivation was an important factor for poor compliance in home-based rehabilitation43, attending physicians should emphasize the need for patients to steadily use the application and perform rehabilitation program to achieve significant clinical improvement. The first step of pulmonary and cardiac rehabilitation involves fostering awareness among patients that engaging in appropriate exercise can contribute to the improvement of their symptom. In this regard, the application guided rehabilitation would be helpful. Moreover, some methods, such as regular text messages or telephone contacts from health care, can be applied to enhance motivation49. Repeated exposure to exercises that promote the use of the application may motivate individuals to exercise more.
In this study, the vitality dimension quantified by HINT-8 was reported as having improved significantly for all participant groups. The rehabilitation program required walking outdoors for 30 min daily, and this may have encouraged the participants to engage in outdoor activities. Previous studies have demonstrated that exercise is associated with improved vitality in patients with chronic diseases50,51. Older adult patients with chronic diseases may be sedentary and prefer to remain indoors, and therefore a significant improvement in vitality may be realized via daily walks outdoors. Taken together, our data suggest that increased physical and outdoor activity may be an important factor improving participant quality of life in this study.
Interestingly, the memory and depression dimensions of HINT-8 improved in all participant groups. There is considerable scientific evidence that exercise can improve the performance of memory systems, even in older adults52,53. For example, one study showed that aerobic exercise increased the volume of gray and white matter in the prefrontal cortices of older adults54. Exercise has also been shown to increase blood volume, perfusion, and volume of the hippocampus in older adults55,56. In addition to structural changes in the brain, previous studies have also demonstrated that exercise can improve cognitive performance and functional connectivity in the brain57,58. Thus, physical activity is thought to improve cognitive function, improve memory, induce antidepressant effects, and confer a sense of wellbeing59. Further studies are required to ascertain the associations between physical exercise and mental health in patients with chronic respiratory and cardiovascular disease.
This study has notable strengths. Despite most participants being older adult, the application-guided rehabilitation treatment showed that they can achieve a significant improvement in exercise capacity and quality of life, particularly with respect to their mental health. Over 80% of participants perceived that the application was easy to use and became familiar with it within a remarkably short period of time. Furthermore, we did not observe disease exacerbation or musculoskeletal accidents during the study period. Previous studies also reported that adverse event rates were acceptable during home-based pulmonary and cardiac rehabilitation60,61. These results therefore highlight the fact that smartphone application-based rehabilitation can be successfully performed even in older adult patients with chronic diseases.
This study has some implications for further research. Although we observed significant improvement in some clinical parameters of the participants, further studies with additional participants and a randomized controlled study design are required to ascertain the efficacy of smartphone application-based rehabilitation programs. Although we noted that no patient experienced acute disease exacerbation during the study period (12 weeks), further studies are needed to evaluate the effect of rehabilitation on acute exacerbation or mortality using long-term follow-up assessments performed after the end of rehabilitation.
This study has some limitations. Physical activity levels, such daily step counts, were not measured in this study owing to the limitation of application. Thus, further development of the application is required to obtain this data through a smartphone-mounted pedometer. Moreover, this study failed to demonstrate improvement in hand grip strength and limb muscle mass. Although the rehabilitation program provided anaerobic exercise with incremental intensity, nutritional support—such as protein supplementation—was not provided. Nutritional support to maintain adequate body mass index and muscle mass is an important component of rehabilitation in chronic disease4,6. Further studies with proper nutritional support are expected to improve muscle mass and strength in patients with chronic diseases.
In conclusion, the smartphone application-based rehabilitation program described here improved clinical outcomes, including exercise capacity and quality of life, in patients with chronic respiratory or cardiovascular diseases. Furthermore, older adult patients with chronic diseases could easily and safely perform smartphone application-based rehabilitation. Thus, smartphone application-based rehabilitation programs may be a useful treatment option for older adult patients with chronic diseases when center-based rehabilitation is not feasible.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
References
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 396, 1204–1222. https://doi.org/10.1016/S0140-6736(20)30925-9 (2020).
Viegi, G., Maio, S., Fasola, S. & Baldacci, S. Global burden of chronic respiratory diseases. J. Aerosol Med. Pulm. Drug Deliv. 33, 171–177. https://doi.org/10.1089/jamp.2019.1576 (2020).
Roth, G. A. et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: Update from the GBD 2019 study. J. Am. Coll. Cardiol. 76, 2982–3021. https://doi.org/10.1016/j.jacc.2020.11.010 (2020).
Bolton, C. E. et al. British Thoracic Society guideline on pulmonary rehabilitation in adults. Thorax 68(Suppl 2), ii1-30. https://doi.org/10.1136/thoraxjnl-2013-203808 (2013).
Spruit, M. A. et al. An official American Thoracic Society/European Respiratory Society statement: Key concepts and advances in pulmonary rehabilitation. Am. J. Respir. Crit. Care Med. 188, e13-64. https://doi.org/10.1164/rccm.201309-1634ST (2013).
Kim, C. et al. Clinical practice guideline for cardiac rehabilitation in Korea. Ann. Rehabil. Med. 43, 355–443. https://doi.org/10.5535/arm.2019.43.3.355 (2019).
JCS Joint Working Group. Guidelines for rehabilitation in patients with cardiovascular disease (JCS 2012). Circ. J. 78, 2022–2093. https://doi.org/10.1253/circj.cj-66-0094 (2014).
Smith, S. C. Jr. et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: A guideline from the American Heart Association and American College of Cardiology Foundation. Circulation 124, 2458–2473. https://doi.org/10.1161/CIR.0b013e318235eb4d (2011).
McCarthy, B. et al. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD003793.pub3 (2015).
Wust, R. C. & Degens, H. Factors contributing to muscle wasting and dysfunction in COPD patients. Int. J. Chron. Obstruct. Pulmon. Dis. 2, 289–300 (2007).
Nagano, A. et al. Respiratory sarcopenia and sarcopenic respiratory disability: Concepts, diagnosis, and treatment. J. Nutr. Health Aging 25, 507–515. https://doi.org/10.1007/s12603-021-1587-5 (2021).
Kokkinos, P. et al. Exercise capacity and mortality in black and white men. Circulation 117, 614–622. https://doi.org/10.1161/CIRCULATIONAHA.107.734764 (2008).
Jeong, S. W. et al. Mortality reduction with physical activity in patients with and without cardiovascular disease. Eur. Heart J. 40, 3547–3555. https://doi.org/10.1093/eurheartj/ehz564 (2019).
Johnston, K. N., Young, M., Grimmer, K. A., Antic, R. & Frith, P. A. Barriers to, and facilitators for, referral to pulmonary rehabilitation in COPD patients from the perspective of Australian general practitioners: A qualitative study. Prim. Care Respir. J. 22, 319–324. https://doi.org/10.4104/pcrj.2013.00062 (2013).
Augustine, A., Bhat, A., Vaishali, K. & Magazine, R. Barriers to pulmonary rehabilitation—A narrative review and perspectives from a few stakeholders. Lung India 38, 59–63. https://doi.org/10.4103/lungindia.lungindia_116_20 (2021).
Dunlay, S. M. et al. Barriers to participation in cardiac rehabilitation. Am. Heart J. 158, 852–859. https://doi.org/10.1016/j.ahj.2009.08.010 (2009).
Hartman, M. et al. Effects of home-based training with internet telehealth guidance in COPD patients entering pulmonary rehabilitation: A systematic review. Int. J. Chron. Obstruct. Pulmon. Dis. 18, 2305–2319. https://doi.org/10.2147/COPD.S425218 (2023).
Antoniou, V. et al. Effectiveness of home-based cardiac rehabilitation, using wearable sensors, as a multicomponent, cutting-edge intervention: A systematic review and meta-analysis. J. Clin. Med. https://doi.org/10.3390/jcm11133772 (2022).
Tsutsui, M., Gerayeli, F. & Sin, D. D. Pulmonary rehabilitation in a Post-COVID-19 world: Telerehabilitation as a new standard in patients with COPD. Int. J. Chron. Obstruct. Pulmon. Dis. 16, 379–391. https://doi.org/10.2147/COPD.S263031 (2021).
Sari, D. M. & Wijaya, L. C. G. Cardiac rehabilitation via telerehabilitation in COVID-19 pandemic situation. Egypt Heart J. 73, 31. https://doi.org/10.1186/s43044-021-00156-7 (2021).
Pellegrino, R. et al. Interpretative strategies for lung function tests. Eur. Respir. J. 26, 948–968. https://doi.org/10.1183/09031936.05.00035205 (2005).
Heidenreich, P. A. et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 145, e895–e1032. https://doi.org/10.1161/CIR.0000000000001063 (2022).
Consensus Document on Pulmonary Rehabilitation in Korea 2015, https://www.lungkorea.org/bbs/index.html?code=guide&category=&gubun=&page=2&number=3484&mode=view&keyfield=&key= (2015).
Holland, A. E. et al. Defining modern pulmonary rehabilitation. An official American Thoracic Society workshop report. Ann. Am. Thorac. Soc. 18, e12–e29. https://doi.org/10.1513/AnnalsATS.202102-146ST (2021).
American Thoracic Society & American College of Chest Physicians. ATS/ACCP statement on cardiopulmonary exercise testing. Am. J. Respir. Crit. Care Med. 167, 211–277. https://doi.org/10.1164/rccm.167.2.211 (2003).
Nolan, C. M. et al. The EQ-5D-5L health status questionnaire in COPD: Validity, responsiveness and minimum important difference. Thorax 71, 493–500. https://doi.org/10.1136/thoraxjnl-2015-207782 (2016).
Dyer, M. T., Goldsmith, K. A., Sharples, L. S. & Buxton, M. J. A review of health utilities using the EQ-5D in studies of cardiovascular disease. Health Qual. Life Outcomes 8, 13. https://doi.org/10.1186/1477-7525-8-13 (2010).
Kim, J. et al. Validity and reliability of the Health-Related Quality of Life Instrument with 8 Items (HINT-8) in Korean breast cancer patients. Osong Public Health Res. Perspect. 12, 254–263. https://doi.org/10.24171/j.phrp.2021.0005 (2021).
Kim, J., Lee, H. J. & Jo, M. W. Health-related quality of life instrument with 8 items for use in patients with type 2 diabetes mellitus: A validation study in Korea. J. Prev. Med. Public Health 55, 234–242. https://doi.org/10.3961/jpmph.22.020 (2022).
Jo, M.-W. Valuation of Korean Health-Related Quality of Life Instrument with 8 Items (HINT-8) (2017).
Jones, P. W. et al. Development and first validation of the COPD Assessment Test. Eur. Respir. J. 34, 648–654. https://doi.org/10.1183/09031936.00102509 (2009).
Kim, S. H. et al. The EQ-5D-5L valuation study in Korea. Qual. Life Res. 25, 1845–1852. https://doi.org/10.1007/s11136-015-1205-2 (2016).
Lee, S. H. & Gong, H. S. Measurement and interpretation of handgrip strength for research on sarcopenia and osteoporosis. J. Bone Metab. 27, 85–96. https://doi.org/10.11005/jbm.2020.27.2.85 (2020).
Kim, K. M., Jang, H. C. & Lim, S. Differences among skeletal muscle mass indices derived from height-, weight-, and body mass index-adjusted models in assessing sarcopenia. Korean J. Intern. Med. 31, 643–650. https://doi.org/10.3904/kjim.2016.015 (2016).
Ramponi, S. et al. Pulmonary rehabilitation improves cardiovascular response to exercise in COPD. Respiration 86, 17–24. https://doi.org/10.1159/000348726 (2013).
Kraal, J. J., Peek, N., Van den Akker-Van Marle, M. E. & Kemps, H. M. Effects of home-based training with telemonitoring guidance in low to moderate risk patients entering cardiac rehabilitation: Short-term results of the FIT@Home study. Eur. J. Prev. Cardiol. 21, 26–31. https://doi.org/10.1177/2047487314552606 (2014).
Piotrowicz, E. et al. Feasibility of home-based cardiac telerehabilitation: Results of TeleInterMed study. Cardiol. J. 21, 539–546. https://doi.org/10.5603/CJ.a2014.0005 (2014).
Lundgren, K. M. et al. Feasibility of telerehabilitation for heart failure patients inaccessible for outpatient rehabilitation. ESC Heart Fail. 10, 2406–2417. https://doi.org/10.1002/ehf2.14405 (2023).
Oga, T., Nishimura, K., Tsukino, M., Sato, S. & Hajiro, T. Analysis of the factors related to mortality in chronic obstructive pulmonary disease: Role of exercise capacity and health status. Am. J. Respir. Crit. Care Med. 167, 544–549. https://doi.org/10.1164/rccm.200206-583OC (2003).
Garcia-Rio, F. et al. Prognostic value of the objective measurement of daily physical activity in patients with COPD. Chest 142, 338–346. https://doi.org/10.1378/chest.11-2014 (2012).
Lee, S. D. et al. The COPD assessment test (CAT) assists prediction of COPD exacerbations in high-risk patients. Respir. Med. 108, 600–608. https://doi.org/10.1016/j.rmed.2013.12.014 (2014).
Ghobadi, H., Ahari, S. S., Kameli, A. & Lari, S. M. The relationship between COPD Assessment Test (CAT) scores and severity of airflow obstruction in stable COPD patients. Tanaffos 11, 22–26 (2012).
Li, Y., Qian, H., Yu, K. & Huang, Y. Nonadherence in home-based pulmonary rehabilitation program for COPD patients. Can. Respir. J. 2020, 5146765. https://doi.org/10.1155/2020/5146765 (2020).
Crooks, M. G. et al. Evidence generation for the clinical impact of myCOPD in patients with mild, moderate and newly diagnosed COPD: A randomised controlled trial. ERJ Open Res. https://doi.org/10.1183/23120541.00460-2020 (2020).
North, M. et al. A randomised controlled feasibility trial of E-health application supported care vs usual care after exacerbation of COPD: The RESCUE trial. NPJ Digit. Med. 3, 145. https://doi.org/10.1038/s41746-020-00347-7 (2020).
Kwon, H. et al. An mHealth management platform for patients with chronic obstructive pulmonary disease (efil breath): Randomized controlled trial. JMIR Mhealth Uhealth 6, e10502. https://doi.org/10.2196/10502 (2018).
Su, J. J., Paguio, J., Baratedi, W. M., Abu-Odah, H. & Batalik, L. Experience of coronary heart disease patients with a nurse-led eHealth cardiac rehabilitation: Qualitative process evaluation of a randomized controlled trial. Heart Lung 57, 214–221. https://doi.org/10.1016/j.hrtlng.2022.10.005 (2023).
Lee, J. H. et al. Efficacy of unsupervised home-based pulmonary rehabilitation for patients with chronic obstructive pulmonary disease. Int. J. Chron. Obstruct. Pulmon. Dis. 15, 2297–2305. https://doi.org/10.2147/COPD.S268683 (2020).
Demeyer, H. et al. Physical activity is increased by a 12-week semiautomated telecoaching programme in patients with COPD: A multicentre randomised controlled trial. Thorax 72, 415–423. https://doi.org/10.1136/thoraxjnl-2016-209026 (2017).
Myers, V. H. et al. Exercise training and quality of life in individuals with type 2 diabetes: A randomized controlled trial. Diabetes Care 36, 1884–1890. https://doi.org/10.2337/dc12-1153 (2013).
Chin, A. P. M. J., van Poppel, M. N., Twisk, J. W. & van Mechelen, W. Effects of resistance and all-round, functional training on quality of life, vitality and depression of older adults living in long-term care facilities: A “randomized” controlled trial [ISRCTN87177281]. BMC Geriatr. 4, 5. https://doi.org/10.1186/1471-2318-4-5 (2004).
Loprinzi, P. D., Roig, M., Etnier, J. L., Tomporowski, P. D. & Voss, M. Acute and chronic exercise effects on human memory: What we know and where to go from here. J. Clin. Med. https://doi.org/10.3390/jcm10214812 (2021).
Zhidong, C., Wang, X., Yin, J., Song, D. & Chen, Z. Effects of physical exercise on working memory in older adults: A systematic and meta-analytic review. Eur. Rev. Aging Phys. Act 18, 18. https://doi.org/10.1186/s11556-021-00272-y (2021).
Colcombe, S. J. et al. Aerobic exercise training increases brain volume in aging humans. J. Gerontol. A Biol. Sci. Med. Sci. 61, 1166–1170. https://doi.org/10.1093/gerona/61.11.1166 (2006).
Burdette, J. H. et al. Using network science to evaluate exercise-associated brain changes in older adults. Front. Aging Neurosci. 2, 23. https://doi.org/10.3389/fnagi.2010.00023 (2010).
Erickson, K. I. et al. Exercise training increases size of hippocampus and improves memory. Proc. Natl. Acad. Sci. USA 108, 3017–3022. https://doi.org/10.1073/pnas.1015950108 (2011).
Colcombe, S. J. et al. Cardiovascular fitness, cortical plasticity, and aging. Proc. Natl. Acad. Sci. USA 101, 3316–3321. https://doi.org/10.1073/pnas.0400266101 (2004).
Voss, M. W. et al. Functional connectivity: A source of variance in the association between cardiorespiratory fitness and cognition?. Neuropsychologia 48, 1394–1406. https://doi.org/10.1016/j.neuropsychologia.2010.01.005 (2010).
Di Liegro, C. M., Schiera, G., Proia, P. & Di Liegro, I. Physical activity and brain health. Genes https://doi.org/10.3390/genes10090720 (2019).
Cox, N. S. et al. Telerehabilitation for chronic respiratory disease. Cochrane Database Syst. Rev. 1, CD013040. https://doi.org/10.1002/14651858.CD013040.pub2 (2021).
Stefanakis, M., Batalik, L., Antoniou, V. & Pepera, G. Safety of home-based cardiac rehabilitation: A systematic review. Heart Lung 55, 117–126. https://doi.org/10.1016/j.hrtlng.2022.04.016 (2022).
Funding
This research was supported by a grant from the Korea Health Promotion R&D Project, funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HS21C0096), the National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (2023R1A2C2006688 and RS-2023-00222687, SWL), and the Bio & Medical Technology Development Program of the National Research Foundation (NRF) funded by the Korean government (MSIT) (No. 2022M3A9G8017220). The funder did not have any role in the design of the study and will not have any role in the collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
C.C., A.R.K., I.Y.J., M.W.J., S.H.L., D.K., H.K., D.Y.K., and S.W.L. contributed to the planning of the study. S.W.L. procured the funding for the study. C.C., A.R.K., I.Y.J., M.W.J., S.H.L., D.Y.K., and S.W.L. conceived and designed the study. C.C. collected the data and conducted data analysis. C.C. and S.W.L. conducted data interpretation and drafted the manuscript. All authors revised and approved the final version of the manuscript, and all authors take responsibility for the accuracy of its content.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chung, C., Kim, AR., Kim, D. et al. Smartphone application-based rehabilitation in patients with chronic respiratory and cardiovascular diseases. Sci Rep 14, 3018 (2024). https://doi.org/10.1038/s41598-024-53583-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-53583-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.