Abstract
Preoperative serum lactate dehydrogenase (LDH) has been reported to be associated with adverse outcomes following thoracic surgery. However, its association with outcomes in noncardiac surgery as a whole has not been investigated. We conducted a retrospective cohort study at West China Hospital, Sichuan University, from 2018 to 2020, including patients undergoing noncardiac surgery. Multivariable logistic regression and propensity score weighting were employed to assess the link between LDH levels and postoperative outcomes. Preoperative LDH was incorporated into four commonly used clinical models, and its discriminative ability, reclassification, and calibration were evaluated in comparison to models without LDH. Among 130,879 patients, higher preoperative LDH levels (cut-off: 220 U/L) were linked to increased in-hospital mortality (4.382% vs. 0.702%; OR 1.856, 95% CI 1.620–2.127, P < 0.001), myocardial injury after noncardiac surgery (MINS) (3.012% vs. 0.537%; OR 1.911, 95% CI 1.643–2.223, P < 0.001), and ICU admission (15.010% vs. 6.414%; OR 1.765, 95% CI 1.642–1.896, P < 0.001). The inverse probability of treatment-weighted estimation supported these results. Additionally, LDH contributed significantly to four surgical prognostic models, enhancing their predictive capability. Our study revealed a significant association between preoperative LDH and in-hospital mortality, MINS, and ICU admission following noncardiac surgery. Moreover, LDH provided supplementary predictive information, extending the utility of commonly used surgical prognostic scores.
Similar content being viewed by others
Introduction
Previously, some studies have focused on exploring risk factors for noncardiac postoperative outcomes using routine laboratory tests, including hydroxybutyrate dehydrogenase (HBDH), neutrophil-to-lymphocyte ratio (NLR), hemoglobin (HB), albumin (ALB), and others1,2,3,4,5,6. The research on these indicators aims to investigate their roles in the pathophysiological status and prognosis of postoperative patients, providing a more comprehensive risk assessment. However, despite some achievements in past studies, considering their limitations and the limited understanding of comprehensive pathophysiology, we believe it is necessary to expand the focus to the application of lactate dehydrogenase (LDH).
Compared to other indicators, LDH, as an enzyme marker, covers multiple biological processes, including cell damage, inflammation, metabolism, and immune regulation. These factors may trigger inflammatory reactions and worsen oxygenation after surgery, increasing the risk of death. This makes LDH provide more extensive and in-depth biological information, potentially more comprehensively reflecting the preoperative physiological status of patients. This study continues this research approach by delving into the application of LDH, aiming to provide a more comprehensive and accurate preoperative risk assessment for noncardiac surgical patients, as well as meaningful biomarkers for monitoring during and after surgery. This not only offers more decision support for clinical physicians but also has the potential to provide new directions and insights for future related research, advancing a deeper understanding of postoperative outcomes.
Nowadays, serum LDH examination has become part of the routine preoperative biochemical test. Preoperative high LDH is common, with the incidence ranging from 10 to 35%7,8,9. A study of 626 patients has shown that preoperative serum LDH level is an independent predictor of cardiopulmonary complications following thoracoscopic lobectomy or segmental resection9. However, in the context of noncardiac surgery, the relationship between LDH and morbidity and mortality following surgery has not been thoroughly investigated.
Therefore, we aimed to evaluate the relationship between preoperative serum LDH levels and prognosis after noncardiac surgery and to explore whether the relationship persisted after the propensity score weighting methods and subgroup analysis.
Methods
Study design and data collection
The Strengthening the Reporting of Observational Studies in Epidemiology10 declaration is followed by this retrospective cohort study. In-hospital deaths, ICU admission, and myocardial injury after noncardiac surgery (MINS) were documented with death certificates and medical record reviews. Due to the sensitive nature of the data used in this study, hospital information center staff members without knowledge collected the data. Independent researchers who were blind to the outcomes compiled the baseline features into a standardized form after obtaining the raw data from the preoperative evaluation sheets. Qualified researchers with experience in human subject confidentiality agreements carried out the data analysis. All data were anonymized and de-identified for confidentiality reasons. This study was approved by Ethics committee in September 2021 (Project No.1082 in 2021), and the need for informed consent was waived by Ethics committee (the Ethics Committee on Biomedical Research, West China Hospital of Sichuan University). The study was performed in accordance with the Declaration of Helsinki and registered at chictr.org (ChiCTR2300068425).
We screened all patients over 14 years old who underwent surgery in West China Hospital of Sichuan University from February 2018 to November 2020. The following patients were excluded: (1) People having ophthalmic, cardiac, obstetric, and diagnostic surgery. (2) patients who didn't have a preoperative LDH measurement available.
Outcome
The primary outcome was in-hospital mortality, defined as all-cause mortality that occurred during postoperative hospitalization. The secondary outcomes included ICU admission and MINS. ICU admission was defined as patients who stayed in the ICU for more than 24 h and excluded patients who were in the ICU preoperatively. Patients who were in the ICU before surgery were excluded from ICU-related analyses. MINSis defined as high-sensitive postoperative troponin T (hs-cTnT) > 30 mmol/l, that occurs during or within 30 days after surgery.11,12 Clinicians screened high-risk groups for detection of myocardial injury, according to clinical guidelines and experience. Patients without a postoperative cardiac enzyme determination were assumed not to have an acute myocardial injury.
LDH measurements and management
Serum LDH examination was a routine preoperative biochemical test for all surgical patients in our hospital. All serum LDH was measured by Lactate Dehydrogenase acc. to IFCC ver.2 (LDHI2) using the International Federation of Clinical Chemistry and laboratory medicine (IFCC) reference method in a Cobas 8000 Modular Autoanalyzer (Roche Diagnostics, Basel, Switzerland). Samples with hemolysis index > 15 were discarded. Preoperative LDH level was defined as the last measured serum LDH concentration within 3 days before surgery. The patient’s serum LDH ranged from 10 to 1,000 U/L. The high LDH group was defined as serum LDH > 220 U/L, according to the minimum positive value set by our laboratory.
Statistical analysis
We examined the patient characteristics between normal and high LDH groups. The Mann–Whitney test or the t-test were used to compare differences in continuous data, which were provided as median with interquartile range. The χ2 or Fisher exact test was used to compare categorical data that were given as numbers (percentages).
The sample size is calculated according to the guidelines for a sample size of the clinical prediction model13. The highest R2 value at 1.09% mortality was 0.11. According to our conservative assumption, the new model will account for 15% of the variability; hence, the expected R2 value is 0.11 × 0.15 = 0.0165. The expected shrinkage required was set as a conservative 2.5%, to minimize the potential overfitting. The output shows that at least 82,026 samples are needed, which is numerically equal to 903 events and 26 events per covariate.
We constructed a multivariable logistic regression model to prove the association between the preoperative serum LDH level and outcomes after surgery. In addition to the well-established predictors14, we added as covariates factors that showed significant associations with mortality and morbidity in our preliminary experiments. Variables of skewness distribution were included in the model after logarithmic transformation. Then, least absolute shrinkage and selection operator regression (LASSO) was used to filter variables and adjust the complexity of the logistic regression model to reduce overfitting. Collinearity was evaluated by the variance inflation factor (VIF), and only variables with VIF ≤ 10 were input into the model. The variable selection process consisted of a preliminary variable selection using LASSO, which was then submitted to the clinicians for final confirmation to ensure that the final set of variables was statistically significant and clinically interpretable. The variables ultimately included in constructing the multivariable logistic regression model, after the selection process, encompass general patient conditions (hypertension, ischemic heart disease, diabetes, chronic obstructive pulmonary disease [COPD], liver disease, renal failure, malignancy), demographic factors (gender, age, Body Mass Index, preoperative heart rate, American Society of Anesthesiologists Physical Status [ASA-PS]), surgical characteristics (emergency, anesthesia method, surgery sites, anesthesia duration), and blood biomarkers (hemoglobin, white blood cell count, neutrophil-to-lymphocyte ratio, blood urea nitrogen, serum creatinine, serum albumin, alkaline phosphatase, serum globulin).
Similar to our another study1, we further analyzed the robustness of the association between different LDH levels and postoperative death using the treatment weighted inverse probability (IPTW)15,16 method. A standardized mean difference (SMD) of less than 10% was considered to be balanced between IPTW-matched groups. A restricted spline fitting curve was constructed to simulate the potential non-linear relationship between outcome and LDH.
‘Extended model’ was calculated by adding the preoperative LDH variable to the score of the four commonly used clinical models including American Society of Anesthesiologists (ASA), Charlson Comorbidity Index (CCI), Revised Cardiac Risk Index (RCRI), and Combined Assessment of Risk Encountered in Surgery (CARES)17. We explored the performance differences between extended models with or without preoperative LDH variables. The discrimination of the prediction models was assessed by the area under the receiver operating characteristic curve (AUROC)18. The reclassification power was assessed by the net reclassification improvement (NRI), and the Integrated Discrimination Increment (IDI). The calibration of the models was assessed using the Hosmere-Lemeshow goodness-of-fit test. We also use the Brier score to indicate overall model performance.
It was determined whether the association continued during subgroup analyses. We analyzed data separately for different sexes, age groups, ASA-PS scores, emergency case, anaesthesia methods and surgical sites, and with versus without comorbidities including hypertension, ischemic heart disease, diabetes, COPD, liver disease, renal failure, and malignancy tumor. In assessing the odds ratios (OR) for the association between serum LDH levels and post-surgery mortality, each subgroup was treated as independent data. The associated subgroup analysis excluded pertinent variables, while the logistic regression analysis proceeded with the inclusion of the remaining variables.
We conducted a sensitivity analysis by excluding individuals under 18 years of age. The primary analysis focused on ages over 14 years, but as a sensitivity check, we restricted the age criteria to individuals over 18 years.
R 4.0.2 (Vienna, Austria; http://www.R-project.org/) was used to conduct the statistical analyses.
Ethics approval and consent to participate
This study was approved by Ethics committee in September 2021 (Project No.1082 in 2021), and the need for informed consent was waived by Ethics committee (the Ethics Committee on Biomedical Research, West China Hospital of Sichuan University).
Results
Baseline characteristics
Figure 1 depicts the patient flowchart. Our analysis included 130,879 patients, whose death, MINS, and ICU admission rates were, respectively, 1.109%, 0.801%, and 7.33%. Preoperative LDH values were taken in 96.16% of the total patients. Patients without LDH readings had rates of death, MINS, and ICU admission of 1.05%, 1.24%, and 6.49%, respectively. The rate between those who had LDH measurement and who did not was comparable. The median of LDH measurements was 164.0 (143.0–190.0) U/L.
There were 6193 patients who had hs-cTnT test postoperatively, of which 1048 patients had hs-cTnT higher than 30 mmol/l. Patients had a median age of 52.0 [40.0–63.0] years with females 64,311 (40.1%). Dividing the patients according to high and normal LDH, 13,944 patients (10.65%) had high preoperative LDH, and 116,935 (89.35%) had normal ones. Table 1 contrasts patients with normal LDH and those with high LDH in terms of demographics, preoperative factors, and perioperative characteristics. The prevalence of ischemic heart disease, COPD, and central nervous system (CNS) surgery was all higher in patients with high LDH.
LDH and postoperative outcomes
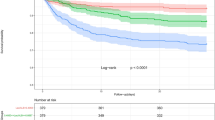
As shown in Fig. 2, restricted spline fitting curves illustrates an escalating risk of postoperative mortality, ICU admission, and MINS with increasing preoperative LDH values In contrast to patients with normal preoperative LDH levels, those with high LDH (> 220 U/L) demonstrated high mortality rates (611 [4.382%] compared to 821 [0.702%]), an increased ICU admission rate (2093 [15.01%] versus 7500 [6.414%]), and a higher incidence of MINS (420 [3.012%] versus 648 [0.537%]). High LDH levels, when compared to the normal LDH group, maintained an independent and statistically significant association with heightened in-hospital mortality (OR 1.856, 95% CI 1.620–2.127; P < 0.001), ICU admission rate (OR 1.765, 95% CI 1.642–1.896; P < 0.001), and MINS (OR 1.911, 95% CI 1.643–2.223; P < 0.001), even after adjusting for confounding factors. Mortality, ICU admission, and MINS prediction outcomes with the IPTW method remained stable (OR 1.814, 95% CI 1.676–1.962; P < 0.001; OR 1.596, 95% CI 1.542–1.651; P < 0.001; OR 1.815, 95% CI 1.664–1.980; P < 0.001). Refer to Supplementary Table 1 for the matching details.
The restricted cubic spline of postoperative in-hospital mortality, ICU admission, and MINS after noncardiac surgery, according to preoperative LDH. Note: This figure presents the results of the restricted cubic spline analysis, depicting the relationship between preoperative LDH (Lactate Dehydrogenase) levels and three crucial postoperative outcomes: in-hospital mortality, ICU admission, and MINS (Myocardial Injury after Noncardiac Surgery). The x-axis represents the spectrum of preoperative LDH levels, capturing the linear patterns. The y-axis represents the odds ratios (OR) of outcomes. The curves showcase how the odds of each outcome change with varying LDH levels. The use of restricted cubic splines allows for a flexible representation of the relationship, capturing potential non-linear associations between LDH and postoperative outcomes.
Optimizing models with LDH extension
Additionally, we assessed the model performance for a number of conventional models, including the ASA, CCI, CARES, RCRI, and our multivariable logistic regression model, with and without the LDH element. Table 2 demonstrates that once LDH was included as a new marker, the AUROC values significantly improved. The Chi-square Statistics of the four models increased, with the exception of our multivariable logistic regression model. An improvement in classifying in models with LDH is shown by an increase in IDI or NRI. In all models using LDH, the Brier score dropped, indicating an improvement in the model's overall performance.
Sub-group analysis
After adjustment for all potential confounders listed in Table 1, preoperative LDH remained independent and significantly associated with increased mortality and morbidity. High LDH significantly influences the in-hospital mortality across different age groups, genders, ASA-PS classifications, surgical urgency levels, anesthesia methods, pre-existing comorbidities, and surgical sites. Preoperative high LDH led to increased mortality in patients with comorbidity. Although patients with high LDH had numerically higher mortality than patients with normal LDH in the group of patients with ischemic heart disease, the difference did not show statistical significance (see Table 3).
Sensitivity analysis
In the sensitivity analysis excluding patients under 18 years, we reassessed the relationship between preoperative LDH levels and prognosis. The age criteria for this analysis included individuals aged 18 and above (n = 128,033). The results indicated a significant association between higher preoperative LDH levels and in-hospital mortality (4.401% vs. 0.707%; 1.852, 95% CI 1.614–2.125, P < 0.001), myocardial injury after noncardiac surgery (MINS) (3.027% vs. 0.537%; OR 1.896, 95% CI 1.627–2.208, P < 0.001), and ICU admission (15.061% vs. 6.468%; OR 1.749, 95% CI 1.627–1.881, P < 0.001), consistent with the main analysis. This supports the robustness and generalizability of our research findings across different age groups.
Discussion
Our multivariable logistic regression study revealed a significant relationship between preoperative LDH levels and postoperative mortality and morbidity following noncardiac surgery. In addition, propensity score weighting method returned unchanged results, which again validated the robustness of the findings.
In subgroup analysis, increased LDH was not significantly associated with increased mortality in the ischemic heart disease subgroup (OR 1.444, 95% CI 0.773–2.700; P = 0.249), which may be related to the general increase of LDH level caused by myocardial injury before surgery. The low AUROC of LDH for predicting ICU admission may be due to the fact that ICU retention is often affected by many factors such as social environment and patient condition. This complexity of the results makes the predictive performance of LDH in this scenario challenging. The identification, correction, reclassification, and overall model performance of both the traditional model and our model could be improved to varying degrees by adding LDH. Thus, we can conservatively conclude that high preoperative LDH levels are associated with increased in-hospital mortality, MINS, and ICU admission risk after noncardiac surgery.
The predictive significance of preoperative blood LDH concentration for postoperative adverse events has only been examined in a small number of trials, and it is uncertain whether this correlation could extend to other surgical procedures.7,8,9. It was discovered that pulmonary problems following thoracic surgery were predicted by the preoperative high LDH level (> 230 U/l)8. Mitsudomi et al.19 found that preoperative LDH levels greater than 178U/L were significantly associated with mortality after pneumonectomy (n = 62). Ruoyu Zhang9 in 2019 analyzed LDH as a continuous indicator for the first time and demonstrated its linear relationship with a predictor of pulmonary complications. A review in 201920 summarizes the recent advances in the design and development of inhibitors, pointing out their specificity and therapeutic potential. This study indicates that high preoperative LDH is a significant predictor of postoperative mortality, ICU stay, and MINS. In future related predictive models, it may be beneficial to incorporate LDH as a predictor for simultaneous modeling. As LDH is a readily available preoperative laboratory indicator and a modifiable factor, prospective research in the future is warranted to explore its causal relationship with postoperative outcomes, aiming to gain a better understanding of its role in the disease process. This exploration will contribute to determining whether LDH can be a target for intervention to improve patient postoperative outcomes.
This study investigated the relationships among different surgical subgroups, excluding thoracic surgery, and concurrently expanded the utility of LDH in predicting surgical outcomes. To mitigate the impact of data imbalance, we employed propensity score weighting combined with a multifactor logistic regression model. Furthermore, leveraging the advantage of sample size, we depicted a restricted cubic spline function curve to elaborate on the nonlinear relationship between LDH and postoperative mortality. Beyond that, we demonstrated the additional contribution of LDH to various commonly used surgical prognostic models by incorporating LDH as an extended variable.
We have several limitations that should be noted. First, there is selection bias as a result of the use of retrospective data from a single center. Second, some unadjusted variables, including ECG, myocardial enzyme, the effects of surgery and perioperative treatment, may still result in residual confounding factor even when we employ multi-factor logistic regression and the propensity score weighting technique. Third, it is essential to acknowledge that this study is purely observational in nature. As such, while it identifies associations between variables, it does not establish causality. The findings should be interpreted with caution, recognizing that inherent limitations in observational research preclude the attribution of causal relationships. Future prospective studies or randomized controlled trials are warranted to further explore the causative aspects of the observed associations. Finally, in this study, the definition of MINS did not include measuring hs-cTnT in all patients. This may result in some cases of MINS being missed. However, it is important to note that this study aims to unfold within the context of real-world practice, where universally measuring hs-cTnT may not always be feasible or practical in the clinical environment. While this is one of the limitations of the study, we emphasize that our goal is to provide valuable information in actual clinical settings and to support physicians in making decisions in resource-constrained environments.
Conclusion
After noncardiac surgery, greater preoperative LDH levels were linked to an increased risk of in-hospital mortality, MINS, and ICU admission. LDH could provide extra predictive information in addition to the commonly used surgical prognostic scores, including the ASA, CCI, CARES and RCRI models.
Data availability
The datasets presented in this article are not readily available because this dataset was not publicly available due to ethics committee requirements. Requests to access the datasets should be directed to 739501155@qq.com.
References
Zhu, Y., Bi, Y., Zhang, Y., Ma, J. & Liu, B. Preoperative serum alpha-hydroxybutyrate dehydrogenase level as a predictor of postoperative mortality and morbidity after noncardiac surgery: A propensity-adjusted analysis. Surgery 171(4), 1027–1035 (2022).
Zhu, Y., Bi, Y., Liu, B. & Zhu, T. Assessment of prognostic value of preoperative neutrophil-to-lymphocyte ratio for postoperative mortality and morbidity. Front Med (Lausanne) 10, 1102733 (2023).
Zhu, Y., Bi, Y., Yu, Q. & Liu, B. Assessment of the prognostic value of preoperative high-sensitive troponin T for myocardial injury and long-term mortality for groups at high risk for cardiovascular events following noncardiac surgery: A retrospective cohort study. Front Med (Lausanne) 10, 1135786 (2023).
Will, N. D. et al. Initial postoperative hemoglobin values and clinical outcomes in transfused patients undergoing noncardiac surgery. Anesth. Analg. 129(3), 819–829 (2019).
Garg, T. et al. Preoperative serum albumin is associated with mortality and complications after radical cystectomy. BJU Int. 113(6), 918–923 (2014).
Kim, H. J. et al. Association of C-reactive protein to albumin ratio with postoperative delirium and mortality in elderly patients undergoing hip fracture surgery: A retrospective cohort study in a single large center. Exp. Gerontol. 172, 112068 (2023).
Uramoto, H. et al. Prediction of pulmonary complications after a lobectomy in patients with non-small cell lung cancer. Thorax 56(1), 59–61 (2001).
Turna, A. et al. Lactate dehydrodgenase levels predict pulmonary morbidity after lung resection for non-small cell lung cancer. Eur. J. Cardiothorac. Surg. 26(3), 483–487 (2004).
Zhang, R., Kyriss, T., Dippon, J., Boedeker, E. & Friedel, G. Preoperative serum lactate dehydrogenase level as a predictor of major complications following thoracoscopic lobectomy: a propensity-adjusted analysis. Eur. J. Cardiothorac. Surg. 56, 294–300 (2019).
von Elm, E. et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet (London, England) 370(9596), 1453–1457 (2007).
Khan, J., Alonso-Coello, P. & Devereaux, P. J. Myocardial injury after noncardiac surgery. Curr. Opin. Cardiol. 29(4), 307–311 (2014).
Botto, F. & Alonso-Coello, P. Myocardial injury after noncardiac surgery: a large, international, prospective cohort study establishing diagnostic criteria, characteristics, predictors, and 30-day outcomes. Anesthesiology 120(3), 564–578 (2014).
Riley, R. D. et al. Calculating the sample size required for developing a clinical prediction model. BMJ 368, m441 (2020).
Park, J. et al. Associations between preoperative glucose and hemoglobin A1c level and myocardial injury after noncardiac surgery. J. Am. Heart Assoc. 10(7), e019216 (2021).
Austin, P. C. & Stuart, E. A. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat. Med. 34(28), 3661–3679 (2015).
Kuss, O., Blettner, M. & Börgermann, J. Propensity score: An alternative method of analyzing treatment effects. Dtsch. Arztebl. Int. 113(35–36), 597–603 (2016).
Chan, D. X. H., Sim, Y. E., Chan, Y. H., Poopalalingam, R. & Abdullah, H. R. Development of the Combined Assessment of Risk Encountered in Surgery (CARES) surgical risk calculator for prediction of postsurgical mortality and need for intensive care unit admission risk: a single-center retrospective study. BMJ Open 8(3), e019427 (2018).
Steyerberg, E. W. et al. Assessing the performance of prediction models: A framework for traditional and novel measures. Epidemiology 21(1), 128–138 (2010).
Mitsudomi, T. et al. Postoperative complications after pneumonectomy for treatment of lung cancer: multivariate analysis. J. Surg. Oncol. 61(3), 218–222 (1996).
Laganá, G., Barreca, D., Calderaro, A. & Bellocco, E. Lactate dehydrogenase inhibition: Biochemical relevance and therapeutical potential. Curr. Med. Chem. 26(18), 3242–3252 (2019).
Funding
This work was supported by the department fund of Natural Science Foundation of Sichuan Province (No.2022NSFSC1297) and the Post-Doctor Research Project of West China Hospital of Sichuan University (No. 2021HXBH079). The funding sources had no role in the design of this study and the analysis and interpretation of the results.
Author information
Authors and Affiliations
Contributions
All authors had full access to the data in the study and took responsibility for the integrity of the data and the accuracy of the data analysis. Y.C.Z.: Data analysis and interpretation, writing the first draft, revising the first draft, reviewing and submitting the manuscript. J.X.: Data analysis and interpretation, revising and submitting the manuscript. Y.D.B.: Data collection, data mining, and some data cleaning, analysis, interpretation, and revision of the first draft. B.L.: study design, funding acquisition, revision of the first draft, and review of the manuscript. T.Z.: Study design and revision of the draft of the manuscript. To ensure that any concerns about the accuracy or integrity of any portion of the work are duly examined and addressed, all the authors agree to accept responsibility for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhu, Y., Xin, J., Bi, Y. et al. The impact of preoperative serum lactate dehydrogenase on mortality and morbidity after noncardiac surgery. Sci Rep 14, 7367 (2024). https://doi.org/10.1038/s41598-024-53372-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-53372-x
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.