Abstract
Resistance training is an exercise against resistance designed to train the endurance and strength of muscle. To observe the effect of intervention of periodic resistance training on obese patients with type 2 diabetic nephropathy. A total of 60 obese patients with type 2 diabetic nephropathy were randomized into resistance training group and aerobic exercise group (30 patients each group) for observing the changes of blood glucose, body weight, blood lipid, insulin resistance, serum creatinine (Scr), urinary microalbumin, urinary albumin excretion rate (UAER) calculated by urinary creatinine, and glomerular filtration rate (GFR) after 12 weeks of intervention, and relevant significance as well. The number of patients with hypoglycemia during the intervention was also recorded. After 12 weeks of intervention, the weight, Body mass index (BMI), Waist, Triglyceride (TG), Cholesterol (TC), Low-density lipoprotein cholesterol (LDL), Fasting glucose (FBG), Fasting insulin (FINS), Glycosylated hemoglobin (HbA1c) and urine Albumin–Creatinine Ratio (uACR) were decreased and GFR was increased in both groups (P < 0.05), but the effect was more significant in the resistance training group. GFR was increased from 92.21 ± 10.67 mL/(min·1.73 m2) to 100.13 ± 12.99 mL/(min·1.73 m2) in resistance training group (P < 0.05). In the aerobic exercise group, GFR was increased from 89.98 ± 9.48 mL/(min·1.73 m2) to 92.51 ± 11.35 mL/(min·1.73 m2) (P > 0.05). Periodic resistance training can not only control the weight, blood sugar and blood lipid of obese patients with type 2 diabetic nephropathy, but also improve the urinary albumin excretion rate and glomerular filtration rate of early obese patients with type 2 diabetic nephropathy, and delay the progression of diabetic nephropathy. It is an effective non-drug intervention.
Similar content being viewed by others
Introduction
As a global disease, diabetes has affected about 463 million people aged 20–79 worldwide with a prevalence rate of about 9.3%. According to an estimation, in 2025, there will be about 700 million patients with diabetes, and the prevalence rate will be increase by 10.9%1. The incidence rate of diabetic nephropathy in patients with type 2 diabetes (T2DM) is about 40% at present, and is expected to increase to 50% by 20252,3,4. The number of obesity cases is also on the rise. The higher the body mass index, the higher the risk of type 2 diabetes. For the resistance training, an exercise against resistance designed to train the endurance and strength of muscle, this study adopted a resistance band. The band is cheap and portable, the requirements for training site are relatively low, and the compliance of subjects is high.
Globally, scholars have found that the exercise against resistance is beneficial to weight loss and blood glucose control in recent years. However, the application of resistance training has not been popularized among obese patients with diabetic nephropathy, and so, relevant data are to be provided. This study was to observe the therapeutic effect of periodic resistance training on obese patients with type 2 diabetic nephropathy.
Methods
Study design
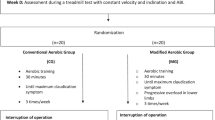
The subjects were randomized into two groups, namely resistance training group and aerobic exercise group. Before test, all of the subjects were provided with relevant education, and given diet instructions. Regular diabetic diet control was given with 30–35 kcal of energy per kilogram of ideal body weight per day. Ideal weight (kg) = height (cm) − 105. Their original medication regimens were maintained during test. For the control group, the patients performed aerobic exercise. Specifically, they warmed up for 5 min before exercise, ran slowly for 30 min, and rested for 5 min after exercise, that is, the exercise lasted about 40 min each time, and 5 times a week. For the observation group, a portable resistance band was used for movements as follows after 5 min of warm-up by walking slowly: squat with resistance band, and perform back neck flexion and extension with resistance band, 15–20 times each movement for females and 20–25 times each movement for males. Complete 3 sets of movements with a 2–3 min interval between sets. The exercise lasted about 40 min each time, with target heart rate (60–80% of the maximum heart rate) maintained for 20–40 min, and 5 times if exercise were performed every week. All of the subjects were followed up by telephone every month for recording their exercise, blood glucose test and drug use. For the included subjects, baseline data at inclusion as well as data 12 weeks after intervention were evaluated. The patients’ height, waist circumference and body weight were monitored for body mass index (BMI) calculation, and the FBG and FINS were monitored for calculating Homeostasis Model Assessment-Insulin Resistance (HOMA-IR) as follows: HOMA-IR = FBG·FINS/22.5. At the same time, HbA1c, TC, LDL-C, HDL-C, TG, Scr, uACR and GFR were tested. GFR = (186 × Scr) − (1.154 × age) − 0.203 × (0.742 if female). Scr is serum creatinine (mg/dL), and the unit conversion of blood creatinine is 1 mg/dL = 88.41 μmol/L. For all of the subjects, the person-times of hypoglycemia during the 12-week intervention were recorded. Symptoms of hypoglycemia are as follows: hunger, cold sweat, palpitation, hand shaking, fatigue, and etc. A hypoglycemic event occurs if blood glucose < 3.9 mmol/L.
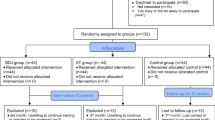
Participants
A total of 60 obese patients with type 2 diabetic nephropathy treated at the Endocrinology Clinic of our hospital between June 2021 and December 2022 were included. The patients were randomized into resistance training group and aerobic exercise group (30 cases each group) for observing the changes of relevant indicators after 12 weeks of intervention, and relevant significance as well. Inclusion criteria: Patients aged 20–50 years old with BMI ≥ 28 kg/m2, HbAlc 7–9%, and diagnosed as T2DM with symptoms consistent with the 1999 WHO diagnostic criteria for diabetes with disease course ≥ 1 year. Diagnosis criteria for early-stage diabetic nephropathy: increased urinary albumin excretion rate. In this study, urinary albumin/urinary creatinine ratio was used to express urinary albumin excretion rate, 30 μg/mg < urine albumin–creatinine ratio (uACR) < 299 μg/mg, and the results of both tests were abnormal. Glomerular filtration rate (eGFR) was > 60 mL/(min·1.73 m2). Other possible causes of urinary microalbumin increase were excluded. Exclusion criteria: (1) Patients with serious infections, and serious hyperglycemia for diabetics (e.g., ketoacidosis, lactic acidosis, hypertonic state, and etc.); (2) Patients with autoimmune diseases; and (3) Patients with serious dysfunctions or insufficiencies of vital organs like the heart, liver, kidney and brain. 5 people in the resistance training group and 1 in the aerobic exercise group quit the experiment. In the resistance training group, there were 11 males and 14 females. In the aerobic exercise group, there were 13 males and 16 females. Neither group received ACEI or ARB or SGLT2, drugs that may affect urinary protein excretion, during the study period.
Statistical analysis
SPSS 22.0 software was used for a statistical analysis. The results were expressed as x ± s, and the non-normal distribution was expressed as median and inter-quartile range. The inter-group and intra-group comparisons of relevant data were carried out by t test or rank sum test, and if P < 0.05, there was statistical significance.
Ethics approval and consent to participate
Ethical clearance and approval were obtained from Ethics Committee of the First Hospital of Putian, Fujian , China. All study participants were informed about the purpose of the study and additional information was given as they need. Written informed consent was obtained from all participants. We had complied with the Declaration of Helsinki Ethical Principles for medical research involving human subjects.
Results
Baseline characteristics
There was no statistical significance in gender, age, disease course, weight, BMI, waist, TG, TC, LDL, HDL, FBG, FINS, HbA1c, Scr, UAER or GFR before intervention (P > 0.05), as shown in Table 1.
After 12 weeks, the weight, BMI, waist, TC, TG, HDL,LDL, FBG, FINS and HbA1c were all decreased for both groups (P < 0.05). HDL was increased in the two groups, but the difference was not statistically significant (P > 0.05). The body mass, blood lipid and blood glucose in the resistance training group were significantly improved as compared with those in the aerobic exercise group (P < 0.05). See Table 2.
Comparison of renal function indicators for the two groups after treatment
The serum creatinine level was decreased after treatment for both groups, but there was no statistical significance (P > 0.05). The UARE level was reduced after exercise with statistical significance (P < 0.05) for both groups, but the reduction rate in the resistance exercise group higher than in the aerobic exercise group (P < 0.05). GFR was increased after resistance training with statistical significance (P < 0.05), while there was no significant change after treatment in the Table 2.
Comparison of the differences in the outcomes of each intervention (ΔHbA1c, ΔuACR and ΔGFR): ΔHbA1c decreased by 0.64% and 0.33% in resistance training and aerobic exercise groups, respectively (P < 0.05). ΔuACR decreased by 19.67 μg/mg and 7.65 μg/mg in resistance training group and aerobic exercise group, respectively. ΔGFR increased by 7.90 mL/(min·1.73 m2) and 2.56 mL/(min·1.73 m2) in resistance training group and aerobic exercise group, respectively. See Figs. 1, 2 and 3.
Hypoglycemia in weeks 3–4 of intervention
A total of 8 person-times of hypoglycemia occurred in the resistance training group, that is, 2 person-times of peripheral blood glucose < 3.9 mmol/L. In the aerobic exercise group, and 2 person-times of hypoglycemia occurred in the aerobic exercise group, that is, 0 person-time of peripheral blood glucose < 3.9 mmol/L. Hypoglycemic drugs were appropriately adjusted after hypoglycemia occurred, and no hypoglycemic event occurred again in weeks 5–12 of intervention for both groups.
Follow up for willingness to adhere
After the study, a questionnaire survey was conducted on the willingness to continue resistance training mode. The results showed that the resistance training group had lower long-term adherence than the aerobic exercise group. Most patients think that the exercise load of resistance training is strong, and the short-term phase can adhere to it, but the long-term persistence worries that with the growth of age, the body can not tolerate. The results are shown in Table 3.
Discussion
In this study, obese patients with type 2 diabetic nephropathy were given 12 weeks of resistance training or aerobic exercise in addition to drugs for blood glucose control. After intervention, the weight, BMI, Waist, TG, TC, LDL, FBG, FINS, HbA1c and uACR were decreased and GFR was increased in both groups (P < 0.05), but the effect was more significant in the resistance training group. GFR was increased from 92.21 ± 10.67 mL/(min·1.73 m2) to 100.13 ± 12.99 mL/(min·1.73 m2) in resistance training group (P < 0.05). In the aerobic exercise group, GFR was increased from 89.98 ± 9.48 mL/(min·1.73 m2) to 92.51 ± 11.35 mL/(min·1.73 m2) (P > 0.05).
The incidence of type 2 diabetes is increasing year by year. The main environmental factors of type 2 diabetes include excessive intake of high-calorie diet, low consumption due to insufficient physical activity, obesity and so on. Worldwide, the prevalence of obesity has increased the morbidity and mortality of cardiovascular and cerebrovascular diseases, diabetes, nephropathy, tumors and etc.5. A relevant study has shown that increased daily exercise and dietary intervention can reduce the incidence of type 2 diabetes, and lower the occurrence and development of diabetes microvascular-related organ complications as realizing a weight loss effectively6. As a common microvascular complication of diabetes, diabetic kidney damage may affect the patients’ quality of life seriously during its occurrence and development. Albuminuria monitoring and GFR estimation should be carried out among diabetic patients every year7. Chronic kidney disease (CKD) is defined as kidney damage resulting from reduced GFR or increased albumin excretion. However, exercise training is an important non-pharmacological intervention to improve and prevent diabetes and CKD8.
This study found that the reduction in HbA1C and uACR was greater in the resistance training group than in the aerobic exercise group, and the increase in GFR was also greater than in the control group. It shows that the increase of GFR and the decrease of UAER after resistance training intervention may be due to the direct benefit of resistance training on the one hand, but may be due to the increase of GFR and the decrease of UAER caused by better control of blood glucose and weight after resistance training on the other hand. Deus et al. also pointed out that, Resistance training can effectively control glucose and blood lipid in kidney disease. Resistance training-induced glucose regulation prevents the progression of CKD9. Under long-term aerobic exercise training, the body can obtain more mitochondria and higher capillary density, increase the maximum oxygen consumption and improve the secretion and sensitivity of insulin gradually, thus lowering the blood glucose10,11,12. Mostly, the staged resistance training promotes muscle synthesis as well as glucose uptake through enhancing the oxidative capacity of mitochondria. After the enhanced exercise, the synthesis of muscle glycogen can enhance the synthesis of insulin related positive regulators to further reduce the insulin resistance of skeletal muscle, regulate the body's glucose metabolism, promote its glucose uptake, and increase the glucose clearance rate, thus reducing HbA1c13,14. There has been a definite consensus on the effect of aerobic exercise on improvement of diabetes, but there is still no sufficient data supporting the effect of resistance training in obese patients with type 2 diabetic nephropathy. For this, this study was conducted.
In this study, both waist circumference and body mass decreased, the blood glucose was controlled, and the insulin resistance was alleviated. Overall, relevant lipid metabolism indicators were improved for the subjects. Skeletal muscle is critical for body function and metabolic health. As one of the most effective non-pharmacological external variables, resistance training can stimulate factors associated with muscle hypertrophy, and thus reduce muscle loss15. However, some other studies have suggested that resistance training has more important effects on body composition, muscle strength, and metabolic risk factors16. Marques EA et al. reported changes of metabolic parameters in 60 obese women after 20 weeks of resistance training without diet control, and as a result, the resistance training reduced the Tc and TG levels in the obese women significantly17. In a study of Amouzad18, after 8 weeks of resistance training in patients with type 2 diabetes, their blood glucose, insulin, and insulin resistance index were significantly lowered as compared with the control group. A meta-analysis has shown that resistance training may improve the blood glucose as well as the strength and endurance of muscle in elderly patients with T2DM19.
Similar to other studies, this study showed that the blood glucose, blood lipid and body weight of patients in the resistance training group decreased significantly as compared with those in the aerobic exercise group. Resistance training is an effective strategy for lowering HbA1c for type 2 diabetes20. Ranasinghe proposed that the high baseline HbAlc (> 7.5%) group had a more significant effect (resistance training > aerobic exercise)21. In terms of hypoglycemia, the frequency of hypoglycemia was higher in the resistance training group at the initial stage of the study, but did not occur any more after adjusting the glucose-lowering regimen. Therefore, it was considered relevant to the effect in lowering blood glucose more significantly.
This study showed that in patients at an early stage of T2DM nephropathy, 12 weeks of resistance training significantly reduced UAER, an renal function index, and increased GFR, and the effect was more obvious than that in the control group, suggesting that resistance training may improve the renal function in patients with T2DM. A 1% reduction in HbAlc was associated with a 37% reduction in microangiopathy risk in patients with type 2 diabetes22. In patients with diabetic nephropathy, proper physical exercise may reduce the albuminuria and alleviate the progression of nephropathy23,24. Some animal experiments have shown that resistance training can enhance insulin-induced vasodilation function in rats25. The function of vascular endothelium was improved by increasing the release of nitric oxide and the level of nitric oxide synthetase, and different intensity and frequency of resistance training improved the vascular endothelium to different degrees26. Resistance training may further affect the microvascular function in T2DM patients through improving their micro-vasodilation and insulin signaling27. Zaki et al. found that the exercise training mode of aerobic exercise and resistance exercise at the same time can effectively improve the metabolic markers, blood lipids and body composition of T2DM patients28. In this study, the improvement of renal function in T2DM patients may be related to resistance training.
This study has several limitations. The number of cases in this study is limited, and the follow-up time is only 12 weeks, so longer follow-up observation and more cases are needed for the later improvement data of diabetic nephropathy. Subsequently, we are also observing the effects of resistance training combined with drugs (ACEI, ARB, SGLT2, etc.) or combined aerobic exercise in early diabetic nephropathy patients.
Conclusions
Periodic resistance training can not only control the weight, blood sugar and blood lipid of obese patients with type 2 diabetic nephropathy, but also improve the urinary albumin excretion rate and glomerular filtration rate of early obese patients with type 2 diabetic nephropathy, and delay the progression of diabetic nephropathy. It is an effective non-drug intervention.
Data availability
The datasets used in the analyses described in this study are available from the corresponding author on reasonable request.
Abbreviations
- T2DM:
-
Type 2 diabetes
- FBG:
-
Fasting glucose
- FINS:
-
Fasting insulin
- BMI:
-
Body mass index
- HbA1c:
-
Glycosylated hemoglobin
- TC:
-
Cholesterol
- LDL-C:
-
Low-density lipoprotein cholesterol
- HDL-C:
-
High-density lipoprotein cholesterol
- TG:
-
Triglyceride
- Scr:
-
Serum creatinine
- UAER:
-
Urinary albumin excretion rate
- uACR:
-
Urine albumin–creatinine ratio
- GFR:
-
Glomerular filtration rate
- CKD:
-
Chronic kidney disease
References
International Diabetes Federation. IDF Diabetes Atlas 9th edn. (International Diabetes Federation, 2019).
Wheeler, D. C. et al. SGLT2 inhibitors: Slowing of chronic kidney disease progression in type 2 diabetes. Diabetes Ther. 11(12), 2757–2774. https://doi.org/10.1007/s13300-020-00930-x (2020).
Wu, B. et al. Understanding CKD among patients with T2DM: Prevalence, temporal trends, and treatment patterns-NHANES 2007–2012. BMJ Open Diabetes Res. Care 4(1), e000154. https://doi.org/10.1136/bmjdrc-2015-000154 (2016).
Kainz, A. et al. Prediction of prevalence of chronic kidney disease in diabetic patients in countries of the European Union up to 2025. Nephrol. Dial. Transplant. 30(Suppl 4), iv113–iv118. https://doi.org/10.1093/ndt/gfv073 (2015).
Cole, C. B. et al. Increased genetic risk for obesity in premature coronary artery disease. Eur. J. Hum. Genet. 24(4), 587–591. https://doi.org/10.1038/ejhg.2015.162 (2016).
Lindström, J. et al. Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: Follow-up of the Finnish Diabetes Prevention Study. Lancet 368(9548), 1673–1679. https://doi.org/10.1016/S0140-6736(06)69701-8 (2006).
Caramori, M. L. et al. Diabetic Kidney Disease (MDText.com Inc, 2022).
Saud, A. et al. Resistance exercise training ameliorates chronic kidney disease outcomes in a 5/6 nephrectomy model. Life Sci. 15(275), 119362. https://doi.org/10.1016/j.lfs.2021.119362 (2021).
Deus, L. A. et al. Metabolic and hormonal responses to chronic blood-flow restricted resistance training in chronic kidney disease: A randomized trial. Appl. Physiol. Nutr. Metab. 47(2), 183–194. https://doi.org/10.1139/apnm-2021-0409 (2022).
Newsom, S. A. et al. A single session of low-intensity exercise is sufficient to enhance insulin sensitivity into the next day in obese adults. Diabetes Care 36(9), 2516–2522. https://doi.org/10.2337/dc12-2606 (2013).
Yan, Z. et al. Regulation of exercise-induced fiber type transformation, mitochondrial biogenesis, and angiogenesis in skeletal muscle. J. Appl. Physiol. 110(1), 264–274. https://doi.org/10.1152/japplphysiol.00993.2010 (2011).
Strasser, B. & Pesta, D. Resistance training for diabetes prevention and therapy: Experimental findings and molecular mechanisms. Biomed Res. Int. 2013, 805217. https://doi.org/10.1155/2013/805217 (2013).
Zanuso, S. et al. Exercise for the management of type 2 diabetes: A review of the evidence. Acta Diabetol. 47(1), 15–22. https://doi.org/10.1007/s00592-009-0126-3 (2010).
Di Meo, S., Iossa, S. & Venditti, P. Improvement of obesity-linked skeletal muscle insulin resistance by strength and endurance training. J. Endocrinol. 234(3), R159–R181. https://doi.org/10.1530/JOE-17-0186 (2017).
Lim, C. et al. An evidence-based narrative review of mechanisms of resistance exercise-induced human skeletal muscle hypertrophy. Med. Sci. Sports Exerc. 54(9), 1546–1559. https://doi.org/10.1249/MSS.0000000000002929 (2022).
Klepin, H. D. et al. Physical performance and subsequent disability and survival in older adults with malignancy: Results from the health, aging and body composition study. J. Am. Geriatr. Soc. 58(1), 76–82. https://doi.org/10.1111/j.1532-5415.2009.02620.x (2010).
Marques, E. A. et al. Effects of resistance and aerobic exercise on physical function, bone mineral density, OPG and RANKL in older women. Exp. Gerontol. 46(7), 524–532. https://doi.org/10.1016/j.exger.2011.02.005 (2011).
AmouzadMahdirejei, H. et al. Effects of an eight-week resistance training on plasma vaspin concentrations, metabolic parameters levels and physical fitness in patients with type 2 diabetes. Cell J. 16(3), 367–374 (2014).
Lee, J., Kim, D. & Kim, C. Resistance training for glycemic control, muscular strength, and lean body mass in old type 2 diabetic patients: A meta-analysis. Diabetes Ther. 8(3), 459–473. https://doi.org/10.1007/s13300-017-0258-3 (2017).
Jansson, A. K. et al. Effect of resistance training on HbA1c in adults with type 2 diabetes mellitus and the moderating effect of changes in muscular strength: A systematic review and meta-analysis. BMJ Open Diabetes Res. Care 10(2), e002595. https://doi.org/10.1136/bmjdrc-2021-002595 (2022).
Ranasinghe, C. et al. Glycemic and cardiometabolic effects of exercise in South Asian Sri Lankans with type 2 diabetes mellitus: A randomized controlled trial Sri Lanka diabetes aerobic and resistance training study (SL-DARTS). Diabetes Metab. Syndr. 15(1), 77–85. https://doi.org/10.1016/j.dsx.2020.12.011 (2021).
Selvin, E. et al. Meta-analysis: Glycosylated hemoglobin and cardiovascular disease in diabetes mellitus. Ann. Intern. Med. 141(6), 421–431. https://doi.org/10.7326/0003-4819-141-6-200409210-00007 (2004).
Formigari, G. P. et al. Renal protection induced by physical exercise may be mediated by the irisin/AMPK axis in diabetic nephropathy. Sci. Rep. 12(1), 9062. https://doi.org/10.1038/s41598-022-13054-y (2022).
Couto, S. M. F. et al. Physical training is a potential modifier of risk for contrast-induced acute kidney injury in diabetes mellitus. Biomed Res. Int. 2020, 1830934. https://doi.org/10.1155/2020/1830934 (2020).
Fontes, M. T. et al. Resistance exercise acutely enhances mesenteric artery insulin-induced relaxation in healthy rats. Life Sci. 94(1), 24–29. https://doi.org/10.1016/j.lfs.2013.11.017 (2014).
Mota, M. M. et al. Endothelium adjustments to acute resistance exercise are intensity-dependent in healthy animals. Life Sci. 142, 86–91. https://doi.org/10.1016/j.lfs.2015.10.007 (2015).
Olver, T. D. & Laughlin, M. H. Endurance, interval sprint, and resistance exercise training: Impact on microvascular dysfunction in type 2 diabetes. Am. J. Physiol. Heart Circ. Physiol. 310(3), H337–H350. https://doi.org/10.1152/ajpheart.00440.2015 (2016).
Zaki, S., Sharma, S. & Vats, H. Effectiveness of concurrent exercise training in people with type 2 diabetes: A systematic review and meta-analysis. Physiother. Theory Pract. 23, 1–22. https://doi.org/10.1080/09593985 (2023).
Funding
This work was supported by Putian Science and Technology Bureau, Fujian province, China. Item number: 2021SY005.
Author information
Authors and Affiliations
Contributions
S.L. conceived, designed and developed the project. S.L. studied the data and wrote the manuscript, G.X.L. reviewed/edited the manuscript and participated in the discussion, F.X. commented/edited the manuscript and participated in the discussion, F.X. and F.Z. collected data and made statistical analysis. J.Z. and S.Y. followed up the patients and contributed to the discussion. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, S., Yuan, S., Zhang, J. et al. The effect of periodic resistance training on obese patients with type 2 diabetic nephropathy. Sci Rep 14, 2761 (2024). https://doi.org/10.1038/s41598-024-53333-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-53333-4
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.