Abstract
To evaluate the corrective effect of posterior hemivertebra resection and short-segment fusion surgery on pediatric patients and to assess the impact of short-segment fixation surgery on vertebral development during follow-up, a retrospective analysis was performed on 28 pediatric patients who underwent posterior hemivertebra resection surgery. The corrective effect was evaluated by comparing indicators such as segmental scoliosis Cobb angle, upper and lower compensatory curves and trunk balance at different time points. Meanwhile, the vertebral and spinal canal diameters of instrumented vertebrae and adjacent noninstrumented vertebrae were measured and compared to assess vertebral and spinal canal development. The correction rate of segmental scoliosis was 72.2%. The estimated mean vertebral volume of the instrumented vertebra was slightly lower than that of the unfused segment at the final follow-up, but the difference was not statistically significant. The growth rate of the spinal canal during follow-up was much smaller than that of the vertebral body. In summary, internal fixation at a young age shows no significant inhibitory effects on spinal development within the fusion segment. Posterior hemivertebra resection and short-segment fusion surgery are safe and effective.
Similar content being viewed by others
Introduction
Hemivertebra is a common cause of congenital scoliosis, which is a developmental defect formed during embryonic development1,2. Most hemivertebrae have growth potential and can lead to scoliosis during growth, the degree of which depends on the type, location, and size of the hemivertebra. The resulting asymmetric spinal growth causes not only physical deformities but also psychological distress3.
Non-surgical interventions exhibit restricted efficacy for hemivertebrae, with most cases necessitating surgical treatment4. Hemivertebrae retain the potential for ongoing progression during growth, potentially leading to alterations in adjacent vertebral structures. Consequently, early-stage surgical intervention becomes imperative to prevent local progression and occurrence of secondary deformities5. Among the available surgical modalities, posterior hemivertebra resection combined with short-segment fusion fixation surgery not only provides satisfactory corrective results but also ensures fusion stability while effectively reducing surgical trauma and complications.
The resection of the hemivertebra is a crucial intervention, significantly mitigating the ongoing progression of deformity. A posterior pedicle screw fixation system not only achieves satisfactory corrective outcomes but also ensures robust fixation6. However, there is little literature on the impact of the internal fixation system on the development of the vertebral body and spinal canal in children during long-term follow-up.
This study is a retrospective study of patients who underwent hemivertebra resection and short-segment fusion surgery, with a follow-up duration exceeding 5 years. This study evaluates the long-term efficacy of this procedure by assessing parameters such as segmental scoliosis, compensatory curves, segmental kyphosis, and trunk balance. Additionally, the impact of short-segment internal fixation surgery on vertebral and spinal canal development is examined through measurements of vertebral diameters and spinal canal diameters.
Results
General data
In this study, a total of 28 patients who had undergone hemivertebra resection and short segment fusion surgery in our hospital between January 2012 and June 2017 were enrolled, including 13 males and 15 females, aged 3–7 years, with an average age of 5.07 ± 1.25 years. Among them, there were 19 cases of fully segmented hemivertebrae and 9 cases of incompletely segmented hemivertebrae. The hemivertebrae were located in the thoracic spine in 16 cases and in the lumbar spine in 12 cases (Table 1).
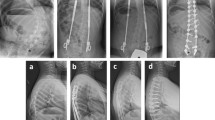
The surgical duration was 120–240 min, with an average of 160.71 min, and the blood loss was 150–400 ml, with an average of 219.64 ml. Due to the small amount of blood loss, no transfusion was recorded (Fig. 1).
The imaging data of a 4-year-old L2 hemivertebra patient who underwent L2 hemivertebra resection and short-segment fusion surgery with a 6-year follow-up. (a) and (b) Preoperative X-ray showed that the segmental scoliosis angle of the L2 hemivertebra was 35°, CBD was 0.3 cm, and VSA was 0.5 cm. (c-e) Preoperative CT scan showed complete segmentation of the hemivertebra. (f) Postoperative CT showed complete hemivertebra resection. (g) and (h) Postoperative X-ray showed that the segmental scoliosis angle was corrected to 4.4°, CBD was 1.45 cm, and SVA was 4.2 cm, which was increased compared to before surgery. (i) and (j) X-ray at the 6-year follow-up showed that the segmental scoliosis angle was 7.9°, CBD was 0.2 cm, and SVA was 0.4 cm, which was significantly improved compared to before. (k) and (l) The diameters of vertebral body and spinal canal in different vertebrae before surgery. (m) and (n) T diameters of vertebral body and spinal canal in different vertebrae before surgery at final follow-up.
Corrective outcome
The segmental scoliosis Cobb angle was corrected from 35.49° preoperatively to 9.87° postoperatively, with a correction rate of 72.2%. The cranial compensatory curve was corrected from 12.79° preoperatively to 3.49° postoperatively, with a correction rate of 67.28%. The caudal compensatory curve was corrected from 18.17° preoperatively to 4.51° postoperatively, with a correction rate of 74.17%. The segmental kyphosis angle was corrected from 15.28° preoperatively to 3.99° postoperatively, with a correction rate of 84.85%. No significant correction loss was found during follow-up (Table 2).
Growth of vetebral body
In the comparative analysis between preoperative and final follow-up assessments, varying degrees of growth were observed in the VBW, VBH and VBL across different vertebrae. Notably, among these dimensions, VBH exhibited the highest growth rate compared to the other two parameters (Table 3).
Pv represents an estimate of the change in vertebral body volume, determined by the ratio of the product of diameters (VBW, VBH, VBL) measured at the last follow-up to the product of preoperative diameters. ANOVA analysis indicates that there is no statistically significant difference in Pv among different vertebrae (a = 0.515) (Table 5).
Growth of spinal canal
In the measurements of spinal canal development, the results indicate an increase in both CLAT and CAP in different vertebrae at the last follow-up compared to preoperative values. However, the growth rate of the spinal canal is significantly lower than that of the vertebral bodies (Table 4).
Pa represents the ratio of the product of CLAT and CAP at the last follow-up to the preoperative values, providing an estimation of the change in the spinal canal area. ANOVA analysis indicates that there is no statistically significant difference in Pv among different vertebrae (a = 0.189) (Table 5).
Complications
Among the 28 patients, two individuals experienced postoperative superficial incisional infections. Both cases achieved full recovery after a comprehensive treatment involving intensified antibiotic therapy, wound dressing changes, and nutritional support. Throughout the follow-up period, only one case exhibited an “adding-on” phenomenon; however, given its minimal angular deviation and inconspicuous impact on appearance, a secondary surgical intervention was deemed unnecessary. None of the patients experienced trunk and lower limb sensory abnormalities or motor impairments after surgery. No neurological complication was observed in any of the patients during the postoperative period and follow-up.
Discussion
For progressive hemivertebra, nonsurgical treatment proves ineffective in preventing deformity progression. The literature widely supports the use of surgical treatment in progressive curves7. The surgical treatment aims to correct the deformity and balance the trunk. Early surgical intervention can help save the fusion range and preserve spinal mobility and growth potential of unaffected segments8. In this study, we focused on the corrective effect of hemivertebra resection and short segment fusion surgery and the influence of internal fixation on spinal growth.
Corrective effect
Compared to alternative approaches, posterior hemivertebra resection and short segment fusion surgery are currently the most widely used surgical methods8,9. In our study, this procedure was employed for all patients. Utilizing wedge osteotomy or complete hemivertebra removal allowed for a more substantial correction angle within a single segment7. Benefiting from the favorable flexibility and relatively small scoliosis angles, the correction rate of the segmental scoliosis was 72.2%. Throughout the follow-up period, although some patients experienced slight correction loss, it did not significantly impact the overall outcome. The correction rates for cranial and caudal compensatory curves were 67.28% and 74.17%, respectively. Due to the inherent flexibility of the pediatric spine, substantial correction of compensatory curves could be attained following adequate correction of the structural curve (Table 2).
The orthopedic results indicate that the correction rate of segmental kyphosis is lower than that of segmental scoliosis. In cases enrolled in our study, deformities primarily manifest as lateral curvature in the coronal plane. In some patients, the kyphosis deformity is not as pronounced, resulting in a relatively lower correction rate. Meanwhile, in another subset of patients with a larger kyphotic angle, satisfactory kyphosis correction can be achieved by removing the posterior elements of the hemivertebra and compressing the fixation rods. Throughout the follow-up period, both CBD and SVA showed further reduction, likely attributed to the spontaneous postural correction during growth10. Only one case of the Adding-On phenomenon occurred during follow-up among all patients, which may be related to incomplete hemivertebra resection and a larger angle of UIV tilt11,12.
Spinal growth after surgery
Having undergone spinal internal fixation surgery at a young age, the spine retains significant growth potential13. We measured relevant parameters of the vertebral body and spinal canal, utilizing adjacent vertebrae outside the fixed segment as a reference. The results indicated a slightly lower growth rate in the vertebral body’s width, length, and height within the fusion segment compared to the upper and lower adjacent vertebrae outside the fusion segment.
We calculated the Pv for estimation to gain further insights into vertebral body development. Our findings revealed a 72% increase in volume for UIV and a 67% increase for the LIV. In contrast, the adjacent vertebrae outside the fixed segment exhibited more substantial changes (92% for UNV and 74% for LNV). However, one-way ANOVA demonstrated a p value of 0.515 in the comparing Pv among different vertebrae, indicating that, despite variations in mean values, these differences lacked statistical significance. This suggests that the inhibitory effect of internal fixation on vertebral development is relatively minimal. The vertebral bodies within the fixed segment also exhibited growth during the follow-up period, possibly attributed to intact vertebral periosteum and at least one intact growth plate on either side14.
Furthermore, in assessing of spinal canal development, we measured the transverse and sagittal diameters of the spinal canal. The results showed that after a long-term follow-up, the changes of spinal canal diameters were much lower than the changes in the vertebral body. One-way ANOVA analysis suggested no statistically significant difference in the Pa among different vertebrae, which indicated that the impact of the internal fixation system on spinal canal development is minimal. Pedicle screws pass through the neural central cartilage (NCC) that connects the pedicle and vertebral body. Previous studies13,15,16 have shown that the NCC of the thoracic and lumbar spine in children starts to close at 4–5 years old, and there is not much change in the size of the spinal canal from then until adulthood. In a study by Olgun et al.17, no negative effect of internal fixation on spinal canal development was observed during a 2-year follow-up of children who had pedicle screws implanted before the age of 5. In our study, all surgically treated patients were aged 3 years or older. The measurements indicated a slight enlargement of the spinal canal during follow-up. However, there was no case of iatrogenic stenosis of the spinal canal or spinal cord compression resulting from the restriction of internal fixation. No neurological dysfunctions were observed in any of the patients after surgery or during the follow-up period.
Limitations
This study has specific limitations. Some patients were too young before surgery to provide subjective assessments, such as satisfaction with appearance before the operation. Furthermore, the measurement of vertebral and spinal canal parameters for all patients relied on X-rays, introducing the potential for errors due to overlapping images, although these errors have been shown to be negligible in other studies18. More accurate CT scans are difficult to perform universally during long-term follow-up.
Conclusion
In summary, the posterior approach hemivertebra resection and short-segment fusion surgery prove to be effective in correcting deformities. Early surgery can save fusion range without significant loss of correction during follow-up. Internal fixation at a young age shows no significant inhibitory effects on spinal development within the fusion segment. Hence, posterior hemivertebra resection and short-segment fusion surgery emerge as a safe and effective procedure.
Methods
Inclusion and exclusion criteria
Inclusion criteria: (1) Congenital scoliosis caused by a single thoracic or lumbar hemivertebra (fully or incompletely segmented) in children under 10 years of age, with indications for surgical treatment: segmental scoliosis angle greater than 25°, rapid progression and ineffective conservative treatment; (2) Surgical resection of the hemivertebra through a posterior approach and short-segment fusion fixation, with a fixation range of one vertebra above and below the hemivertebra; (3) Follow-up for more than 5 years; (4) Complete imaging data.
Exclusion criteria: (1) Surgery through anterior or anteroposterior approaches; (2) Unilateral pedicle screw internal fixation; (3) Presence of multiple vertebral bodies deformities or history of previous spinal surgery.
Surgical methods
All surgical patients underwent surgery under neurologic monitoring. After endotracheal intubation under general anesthesia, the patient was placed in a prone position. The hemivertebra segment was exposed through a posterior midline incision, with full exposure of the posterior spinal structures, including the spinous process, lamina, and facet joints of the hemivertebra and the adjacent vertebrae above and below. Pedicle screws were placed in the adjacent vertebrae above and below the hemivertebra and temporarily fixed with a rod on the concave side. The lateral aspect of the hemivertebra was exposed along the base of the pedicle, and the hemivertebra and intervertebral disc were partially or completely excised based on the segmentation of the hemivertebra. Subsequently, a pre-contoured rod was placed on the convex side. Gradual compression was applied until the gap was successfully closed, addressing both the segmental scoliosis and kyphosis deformities for corrective purposes. C-arm radiography confirmed satisfactory correction, and spinal posterior column bone grafting was performed. The incision was closed layer by layer.
Postoperative management
Strict bed rest is required for the first 2 weeks after surgery. The timing for the child to resume activities out of bed is determined based on the healing of the incision and postoperative imaging results. A plastic brace was provided for 3 months after the first ambulation, serving the purpose of protection and restriction of trunk movements to promote bone fusion. Imaging examinations are scheduled every 3 months during the first year postoperatively and every 6–12 months after the first year.
Imaging data
For the assessment of orthopedic outcomes, we measure indicators including segmental scoliosis Cobb angle, cranial and caudal compensatory curves, coronal balance distance (CBD), segmental kyphosis (SK), thoracic kyphosis (TK), lumbar lordosis (LL), Sagittal vertical axis (SVA), and tilt angles of upper instrumented vertebra (UIV) and lower instrumented vertebra (LIV). Comparisons between different time points, including preoperative, postoperative and follow-up, were conducted to evaluate the orthopedic effects. The specific definitions and measurement methods of these indicators are provided in Table 6.
Vertebral development was assessed by measuring the diameters of the upper instrumented vertebra (UIV), lower instrumented vertebra (LIV), upper adjacent noninstrumented vertebra (UNV), and lower adjacent noninstrumented vertebra (LNV). Comparison of vertebral size parameters before and at the last follow-up was conducted to evaluate the development in different vertebrae. The diameters include vertebral body height (VBH), vertebral body width (VBW), vertebral body length (VBL), spinal canal width (CLAT) and anterior–posterior diameter of the spinal canal (CAP)18. The definitions and measurement methods are detailed in Table 6 and Fig. 219,20,21.
Illustration of measurements. (a) and (b) Illustration of vertebral body and spinal canal diameters measurements: W1: the width of the upper endplate of the vertebral body in the coronal plane; W2: the width of the lower endplate of the vertebral body in the coronal plane; H1: the height of the anterior edge of the vertebral body in sagittal plane; H2: the height of the posterior edge of the vertebral body in sagittal plane; L1: the length of the upper endplate of the vertebral body in sagittal plane; L2: the length of the lower endplate of the vertebral body in sagittal plane; CLAT: interpedicular diameter of the spinal canal ; CAP : The distance from the posterior edge of the vertebral body to the lamina in sagittal plane.
In addition, the product of VBH, VBW and VBL was used to estimate the changes in vertebral volume before surgery and at the last follow-up, and the product of CLAT and CAP was used to estimate the changes in the vertebral canal area before and at the last follow-up20.
The ratio of vertebral body volume at the last follow-up to vertebral volume before surgery (Pv) was estimated as follows:
-
1.
\({\text{Pv}} = \frac{{{\text{VBW}}_{{{\text{pre-op}}}} \times {\text{VBH}}_{{{\text{pre-op}}}} \times {\text{VBL}}_{{{\text{pre-op}}}} }}{{{\text{VBW}}_{{{\text{LF}}}} \times {\text{VBH}}_{{{\text{LF}}}} \times {\text{VBL}}_{{{\text{LF}}}} }}\)
(Preop: preoperative; LF: last follow-up).
The ratio of the spinal canal area at the last follow-up to the preoperative spinal canal area (Pa) was estimated as follows:
-
2.
\({\text{Pa}} = \frac{{{\text{CAP}}_{{{\text{pre-op}}}} \times {\text{CLAT}}_{{{\text{pre-op}}}} }}{{{\text{CAP}}_{{{\text{LF}}}} \times {\text{CLAT}}_{{{\text{LF}}}} }}\)
(Preop: preoperative; LF: last follow-up).
Statistical analysis
Data analysis was performed using the SPSS 22.0 software package (IBM Corporation, USA). Paired sample t tests were used to compare preoperative, postoperative, and last follow-up data for corrective surgery-related information (segmental scoliosis angle, compensatory curve angle, CBD, VSA, LK, TL, LL, UIV tilt, LIV tilt). Paired sample t tests were also used to compare vertebral body development-related information (VBH, VBW, VBL, CLAT, CAP) between preoperative and last follow-up data. One-way ANOVA was used to compare differences in estimated Pv and Pa values between different vertebrae. Differences were considered statistically significant at a level of a < 0.05.
Ethical approval
We confirm that all methods were carried out in accordance with the Declaration of Helsinki and its later amendments, and all protocols were approved by the Ethics Committee of Xiangya Hospital of Central South University (ethics approval number: 201703359). We confirm that written informed consent was obtained from all subjects.
Data availability
Some or all data, or code that support the findings of this study are available from the corresponding author upon reasonable request.
References
Frank, S. et al. Hemivertebra resection in small children. A literature review. Glob. Spine J. https://doi.org/10.1177/21925682221130060 (2022).
Marks, D. S. & Qaimkhani, S. A. The natural history of congenital scoliosis and kyphosis. Spine (Phila Pa 1976) 34, 1751–1755 (2009).
Pahys, J. M. & Guille, J. T. What’s new in congenital scoliosis?. J. Pediatr. Orthop. 38, e172–e179 (2018).
Kaspiris, A., Grivas, T. B., Weiss, H. R. & Turnbull, D. Surgical and conservative treatment of patients with congenital scoliosis: α search for long-term results. Scoliosis 6, 12 (2011).
Crostelli, M., Mazza, O. & Mariani, M. Posterior approach lumbar and thoracolumbar hemivertebra resection in congenital scoliosis in children under 10 years of age: Results with 3 years mean follow up. Eur. Spine J. 23, 209–215 (2014).
Shono, Y., Abumi, K. & Kaneda, K. One-stage posterior hemivertebra resection and correction using segmental posterior instrumentation. Spine (Phila Pa 1976) 26, 752–757 (2001).
Ruf, M., Jensen, R., Letko, L. & Harms, J. Hemivertebra resection and osteotomies in congenital spine deformity. Spine (Phila Pa 1976) 34, 1791–1799 (2009).
Zhang, Y. B. & Zhang, J. G. Treatment of early-onset scoliosis: Techniques, indications, and complications. Chin. Med. J. (Engl.) 133, 351–357 (2020).
Piantoni, L. et al. Hemivertebra resection with instrumented fusion by posterior approach in children. Spine Deform. 3, 541–548 (2015).
Wang, Y. et al. Proximal junctional kyphosis following posterior hemivertebra resection and short fusion in children younger than 10 years. Clin. Spine Surg. 30, E370–E376 (2017).
Chang, D. G. et al. Congenital scoliosis treated with posterior vertebral column resection in patients younger than 18 years: Longer than 10-year follow-up. J. Neurosurg. Spine 25, 225–233 (2016).
Roberts, S. B. & Tsirikos, A. I. Paediatric spinal deformity surgery: Complications and their management. Healthcare (Basel) 10, 2519 (2022).
Labrom, R. D. Growth and maturation of the spine from birth to adolescence. J. Bone Jt. Surg. Am. 89(Suppl 1), 3–7 (2007).
Lucas, P. et al. Long-term results of hemivertebra excision: How does the spine behave after the peak of puberty?. Spine Deform. 9, 161–167 (2021).
Kahraman, S. et al. Does pedicle screw fixation under age 5 cause spinal canal narrowing? A CT study with minimum 5 years follow-up. Eur. Spine J. 25, 1665–1673 (2016).
Rajwani, T. et al. MRI characteristics of the neurocentral synchondrosis. Pediatr. Radiol. 32, 811–816 (2002).
Olgun, Z. D., Demirkiran, G., Ayvaz, M., Karadeniz, E. & Yazici, M. The effect of pedicle screw insertion at a young age on pedicle and canal development. Spine (Phila Pa 1976) 37, 1778–1784 (2012).
Xue, X. et al. X-Ray assessment of the effect of pedicle screw on vertebra and spinal canal growth in children before the age of 7 years. Eur. Spine J. 23, 520–529 (2014).
Diab, K. M., Ollmar, S., Sevastik, J. A., Willers, U. & Svensson, A. Volumetric determination of normal and scoliotic vertebral bodies. Eur. Spine J. 7, 282–288 (1998).
Odaci, E. et al. Rapid estimation of the vertebral body volume: A combination of the Cavalieri principle and computed tomography images. Eur. J. Radiol. 48, 316–326 (2003).
Chang, D. G. et al. Posterior hemivertebra resection and short segment fusion with pedicle screw fixation for congenital scoliosis in children younger than 10 years: Greater than 7-year follow-up. Spine (Phila Pa 1976) 40, E484–E491 (2015).
Acknowledgements
The work was supported by the Hunan Province Natural Science Foundation of China (No. 2020JJ4913), Research project on postgraduate education and teaching reform of Central South University (No. 2021JGB082), Graduate course ideological and political construction project of Central South University (No. 2022YJSKS032) .
Author information
Authors and Affiliations
Contributions
H.Z. designed the study; Y.W. collected and analyzed the data; Y.D. collected and analyzed the data, and wrote the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Du, Y., Zhang, H. & Wang, Y. Clinical outcomes and spinal growth after posterior hemivertebra resection and short segment fusion in children. Sci Rep 14, 2755 (2024). https://doi.org/10.1038/s41598-024-53290-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-53290-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.