Abstract
In cancer patients, psychological distress, which encompasses anxiety, depression, and somatization, arises from the complex interplay of emotional and behavioral reactions to the diagnosis and treatment, significantly influencing their functionality and quality of life. The aim was to investigate factors associated with psychological distress in cancer patients. This prospective and multicenter study, conducted by the Spanish Society of Medical Oncology (SEOM), included two cohorts of patients with cancer (localized resected or advanced unresectable). They completed surveys assessing psychological distress (BSI-18) before and after cancer treatment and coping (MINI-MAC) and spirituality (FACIT-sp) prior to therapy. A multivariable logistic regression analysis and a Structural Equation Modeling (SEM) were conducted. Between 2019 and 2022, 1807 patients were evaluated, mostly women (54%), average age 64 years. The most frequent cancers were colorectal (30%), breast (25%) and lung (18%). Men had lower levels of anxiety and depression (OR 0.66, 95% CI 0.52–0.84; OR 0.72, 95% CI 0.56–0.93). Colorectal cancer patients experienced less anxiety (OR 0.63, 95% CI 0.43–0.92), depression (OR 0.55, 95% CI 0.37–0.81), and somatization (OR 0.59, 95% CI 0.42–0.83). Patients with localized cancer and spiritual beliefs had reduced psychological distress, whereas those with anxious preoccupation had higher level. SEM revealed a relationship between psychological distress and coping strategies, emphasizing how baseline anxious preoccupation exacerbates post-treatment distress. This study suggests that age, sex, extension and location of cancer, coping and spirituality influence psychological distress in cancer patients.
Similar content being viewed by others
Introduction
Cancer is a growing concern worldwide, with the International Agency for Research on Cancer (IARC) estimating 18.1 million cases in 2020, rising to 28 million in 2040. According to the Spanish Society of Medical Oncology (SEOM), there will be an estimated 279,260 cases in 2023, potentially reaching 341,000 in 20401. Its impact on physical and mental health is significant, and its prognosis is often poor. As such, despite advances in diagnosis and treatment, it remains one of the leading causes of death, with 9.89 million fatalities in 2020, and an estimated 113,000 in Spain. This number is expected to grow to 16 million worldwide and 159,000 in Spain by 20401.
It is widely known that cancer patients are more likely to experience psychological distress, such as anxiety, depressive disorders, and somatization, due to the severity of the disease and its unfavorable prognosis2. Recent research, including Wang Y-H et al.'s 2020 meta-analysis, has further emphasized the connection between psychological distress and increased mortality risk and poorer survival outcomes3.
Psychological distress in cancer patients is conceptualized as psychological harm that affects an individual's functionality. This condition encompasses various emotional and behavioral aspects, emerging as a result of the diagnosis and treatment of the disease4 Haga clic o pulse aquí para escribir texto. Previous research has highlighted the significance of depressive disorders and intense emotional response patterns as key factors in reducing the quality of life of these patients4. In this context, it is crucial to recognize how anxiety, depression, and somatization, although distinct in their nature, intertwine in the cancer experience5. Anxiety may stem from the uncertainty and fear of the future, while depression could be a reaction to the challenges and changes imposed by the illness. Somatization, on the other hand, reflects how emotional stress can manifest in physical symptoms. This comprehensive understanding is essential to appropriately address the psychological needs of cancer patients, thereby improving their quality of life and their ability to cope with the disease4,6
Anxiety is the most widely reported psychological disorder found in up to 38% of cancer patients2.Age, gender, and cancer location are believed to be mediators, with higher anxiety levels generally seen in younger patients7. An Iranian meta-analysis in 2022 and another meta-analysis conducted in Iran revealed a higher prevalence of both anxiety and depression, as well as depression alone in breast cancer patients, respectively8,9. Moreover, depression is a common issue among cancer patients, affecting up to 16%10. Its prevalence is likely to vary throughout the course of the disease, as various elements, such as the patient's response to their diagnosis, fear of the appearance of symptoms related to the disease, and the adverse effects of treatments, can contribute to it. Additionally, living with the uncertainty of a recurrence or progression of the cancer, as well as the fear of death, can have a significant impact10. Relative to somatic symptoms, it has been observed that cancer patients may experience a plethora of symptoms, both from their cancer treatments and the tumor disease. Common examples include pain, fatigue, anorexia, tiredness, lack of energy, trembling and lethargy. A meta-analysis published in 2020 found an association between female gender and a higher level of fatigue in cancer patients11. It is important to note that it can be difficult to distinguish between physical symptoms caused by cancer and those caused by psychological issues, which might lead to misdiagnosis and a delay in providing psychological interventions12,13.
Coping is an essential psychological factor for cancer patients, as it can provide a sense of protection and adjustment from the negative effects associated with diagnosis, treatment adverse events, the risk of recurrence, and potential socio-economic and familial repercussions. Adaptive coping strategies, such as displaying a fighting spirit or maintaining a positive attitude, have been shown to facilitate positive psychosocial adaptation to the cancer experience. In contrast, those using a non-adaptive coping style, such as fatalism or anxious preoccupation-based approaches, are more likely to experience anxiety, depression, social isolation, and reduced quality of life14,15. In addition, research has demonstrated that those with a greater sense of psychospiritual well-being are better able to handle the terminal illness process16.
Spirituality is commonly understood as an individual's search for significance and purpose in life, as well as a connection with intangible aspects of existence and transcendence. Patients may draw from their spiritual beliefs to find strength, hope and meaning in the face of a cancer diagnosis and its associated phases. Factors such as prognostic knowledge, family and social support, autonomy, hope and meaning in life have been identified to contribute to psychospiritual well-being, while emotional distress, anxiety, helplessness, hopelessness, and fear of death are known to detract from it process16. Patients facing a chronic, incurable, or terminal illness may begin to question the meaning of life. Studies have suggested a positive relationship between religion/spirituality and mental health in cancer patients17. Furthermore, meaning-focused interventions may be beneficial for improving quality of life in those with advanced cancer18. In addition, spiritual interventions have been found to reduce anxiety, depression, and hopelessness in cancer patients, leading to physical and psychological benefit17,18. As such, it is important for the medical team to consider the patient's spirituality, and to provide interventions if necessary or requested19.
With all the above in mind, the aim of this study was to evaluate the sociodemographic, clinical, and psychological factors predictive of anxiety, depression, and somatization in cancer patients. Additionally, the correlation between psychological distress and coping, spirituality and age was also explored. Furthermore, Structural Equation Modeling (SEM) was utilized to investigate the relationship between psychological distress before and after treatment and coping strategies.
Materials and methods
Patients and study design
This study, sponsored by the Spanish Society of Medical Oncology (SEOM) Bioethics Section, was prospective, observational, and consecutive in nature. It was approved by the Ethics Committee of each institution, as well as the Spanish Agency of Medicines and Health Products, and all participants signed an informed consent form prior to inclusion.
The participants were those who had a histologically confirmed cancer and were candidates for systemic therapy. Individuals under the age of 18 and those with any serious mental illness that would hinder their understanding of the study, as well as any underlying personal, family, sociological, geographic, and/ or medical condition that might impede their participation, were excluded. Moreover, individuals who had already received any systemic cancer treatment or patients with resected metastatic cancer were also excluded.
The study was based on a series of questionnaires that the medical oncologist provided to the patient during the same visit in which they discussed the potential benefits of adjuvant (for resected localized cancer) or palliative (for unresectable advanced cancer) systemic cancer treatment. These forms were completed by the patient at home prior to the start of treatment and then handed in to the study assistants at the next visit. Each form contained clear instructions and specified that its completion was voluntary and anonymous. Patients with resected localized cancer completed the psychological distress questionnaire at the end of their adjuvant treatment, which was 6 months after starting treatment. Subjects with unresectable advanced cancer completed the questionnaire after their first radiological response evaluation study, which was 2–3 months after their antineoplastic treatment began. This was closer to baseline, as this population has a poorer prognosis and increased risk of premature death.
Measures and variables
The information was collected and updated by medical oncologists specially trained to meet the requirements of the study. Demographic and clinical data (age, sex, marital status, educational level, employment status, cancer location, and stage, and treatment received) were obtained directly from the patients and their medical records. Cancer location was classified into breast, bronchopulmonary, colon, non-colorectal digestive (encompassing esophagus, stomach, pancreas, biliary tract, liver, and anal canal) and all other cases were categorized as 'other'. Stage I-III cancers that had been resected were categorized as resected localized whereas stage III-IV cancers that were deemed unresectable were classified as unresectable advanced.
The participants finished the questionnaires BSI-18 (psychological distress), MINI-MAC (coping), and FACIT-sp (spirituality). The Brief Symptom Inventory (BSI-18) was employed, consisting of 18 items which measure the respondent's overall emotional adjustment or psychological distress over the preceding 7 days20, each rated on a five-point Likert scale, from zero (not at all) to four (extremely). Raw scores are converted to T-scores based on gender-specific normative data. Following the clinical case-rule criteria20 and using the cut-off values recommended by Derogatis20, patients with T-scores of 63 or higher were identified as likely experiencing significant anxiety, depression, or somatization20.
Cronbach's alpha for the scale has been reported to range from 0.81 to 0.90 20, and its validity has been established among Spanish-speaking populations21. In the current study, it was evaluated both at the start and conclusion of adjuvant treatment (in those with resected localized cancer) or following the first response assessment imaging study (in those with unresectable advanced disease).
The Mini-Mental Adjustment to Cancer (Mini-MAC) is a 29-item scale that evaluates the cancer-specific coping strategies of individuals22. It classifies four coping strategies: anxious preoccupation, helplessness, positive attitude, and cognitive avoidance. The version adapted for Spanish cancer patients was used in this study23. It is important to note that the four-factor structure of the Mini-MAC was initially identified in a prior study by our research group, using a different sample of cancer patients. Each item is rated on a four-point Likert scale from one (definitely does not apply to me) to four (definitely applies to me). The higher the score on a given subscale, the more frequently that coping strategy is employed. The omega coefficients for the Spanish version of the score range from 0.76 to 0.9023. In this study, the internal consistency of the scale scores ranges from 0.82 to 0.90.
The Functional Assessment of Chronic Illness-Spiritual Well-Being Scale (FACIT-Sp) is a 12-item questionnaire which uses a five-point Likert-type scale, with responses ranging from not at all (0) to very much (4). The scale is divided into three subdomains which assess spiritual well-being (meaning, peace and faith)24. The FACIT-sp scores vary from 0 to 48, with higher values indicating a higher spiritual well-being. Internal consistency reliability to the full-scale in the Spanish version was 0.87 25.
Statistical analysis
Descriptive statistics were employed to analyze demographic data and questionnaire responses. Categorial variables were expressed as percentages, while quantitative variables were reported in terms of mean and standard deviation (SD). Pearson’s correlation was used to determine the level of association between psychological variables and age. Analysis of variance (ANOVAs) were conducted to examine variances in psychological distress (anxiety, depression, and somatization) at the onset of the treatment related to demographic and clinical variables. Multivariate logistic regression analysis was performed to examine the influence of sociodemographic, clinical, and psychological predictors on psychological distress (anxiety, depression, and somatization) before and after treatment, as assessed using the BSI-18 scale. Covariables included sociodemographic variables (such as sex, and age), clinical variables (performance status measured with the Eastern Cooperative Oncology Group scale (ECOG), cancer location and stage), and psychological variables (coping and spiritual well-being). Cancer localization was re-categorized into k-1 dummy variables, where bronchopulmonary was the reference groups. SEM was used to identify the relationship between pre- and post-treatment psychological distress and the various coping strategies26. For all analyses, a significance level of α < 0.05 was adopted. Statistical analysis was performed using IBM SPSS Statistics for Windows, version 23.0 (IBM Corp., Armonk, N.Y., USA).
Ethics approval and consent to participate
This study was approved by the Research Ethics Committee of the Principality of Asturias (May 17, 2019) and by the AEMPS (May 8, 2019). The studies have been performed in accordance with the ethical standards of the 1964 Declaration of Helsinki and its later amendments. This study is a prospective, observational, non-interventionist trial. Signed informed consent was obtained from all patients.
Results
Sociodemographic and clinical features
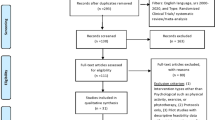
Between 2019 and 2022, 1977 patients were recruited, of which 1807 were eligible and 170 were excluded. Of those excluded, 40 did not meet any inclusion criteria, 42 met any exclusion criteria, and 88 had incomplete data at the time of analysis. Table 1 provides the baseline socio-demographic and clinical characteristics. A roughly equal proportion of men (46%) and women (54%) were included, with an average age of 64 years and 57% of participants being ≤ 65 years. Many participants were married or living with a partner (72%), had basic education levels (51%), and were either unemployed or retired (59%). The most common primary cancers were colorectal (30%), breast (25%), bronchopulmonary (18%), and non-colorectal digestive neoplasms (15%). Of the 944 participants with resected localized cancer, 19% were stage I, 36% were stage II, and 45% were stage III. Of the 863 participants with unresectable advanced cancer, 20% were stage III and 80% were stage IV.
Table 1 summarizes the adjuvant treatments administered to patients with resected cancer, and the first-line treatments given to those with unresectable advanced cancer. Chemotherapy was the systemic treatment given to patients with resected cancer (100%), and radiotherapy was also included in 33% of cases. For those with unresectable advanced cancer, the most common therapy was chemotherapy (55%), and 34% received immunotherapy or 11% were treated with targeted therapy either alone or in combination with chemotherapy. Prior to the completion of adjuvant treatment (6 months) in patients with resected cancer, and prior to the first response evaluation study (2–3 months) in those with advanced cancer, 5% (n = 86) had passed away, with a greater proportion of deaths seen in patients with advanced cancer (17.8%) than those with localized cancer (3.3%).
Based on the BSI score, it was observed that 57% had scores indicating of anxiety, 44% indicating depression and 48% indicating somatization. As illustrated in Table 1, women were found to have higher levels of anxiety (p = 0.001) and depression (p = 0.003) than men, and those ≤ 65 years had higher levels of anxiety (p = 0.002) and somatization (p = 0.044) than the elderly. Additionally, patients without a partner displayed more depression than those with a partner (p = 0.006), and those in employment showed higher levels of anxiety, depression, and somatization than non-working patients (p = 0.002, p = 0.001, and p = 0.001, respectively). Patients with colorectal cancer were found to have the lowest levels of anxiety, depression and somatization compared to all other neoplasms (all p = 0.001). Furthermore, patients with advanced unresectable cancer had higher levels of anxiety, depression, and somatization than those with resected stage I–III cancer (all p = 0.001). Lastly, patients who only received chemotherapy (n = 1087) had significantly lower levels of anxiety, depression and somatization when compared to other groups (p = 0.001, p = 0.005, p = 0.001, respectively).
Correlations across psychological variables and age
Table 2 presents the means, standard deviations, and Pearson correlation analyses of the psychological variables and age. The mean scores of anxiety, depression, and somatization were 63.2, 61.7, and 62.9, respectively. The two most employed coping strategies were positive attitude and cognitive avoidance, with respective mean scores of 77.3 and 59.3, whilst anxious preoccupation and hopelessness were the least utilized (33.4 and 33.8, respectively). Furthermore, the mean score of the FACIT-Sp spirituality scale was 34.7. The results demonstrated that there were significant correlations between all psychological variables apart from helplessness and positive attitude. It was found that positive attitude-based coping was associated with lower levels of anxiety (r = − 0.142, p < 0.001), depression (r = − 0.231, p < 0.001), somatization (r = − 0.087, p < 0.001) and anxious preoccupation (r = − 0.182, p < 0.001). Similarly, spirituality was linked to decreased anxiety (r = − 0.240, p < 0.001), depression (r = − 0.342, p < 0.001), somatization (r = − 0.148, p < 0.001) and anxious preoccupation (r = − 0.295, p < 0.001). Additionally, older age was associated with lower levels of anxiety (r = − 0.074, p < 0.001) and anxious preoccupation (r = − 0.103, p < 0.001), as well as higher levels of positive attitude (r = 0.046, p < 0.001), cognitive avoidance (r = 0.107, p < 0.001), and spirituality (r = 0.263, p < 0.001).
Changes in symptoms of anxiety, depression, and somatization before and after treatment
The Table 3 categorized the sample into four groups: patients who did not exhibit symptoms of anxiety, depression, or somatization either before or after treatment (never), those who did not show symptoms before treatment but did afterwards (post-treatment symptoms), those who initially showed symptoms but not afterwards (pre-treatment symptoms), and finally, those who exhibited symptoms both before and after treatment (persistent symptoms).
Regarding anxiety, 22% exhibited high levels prior to the initiation of treatment, 33% had baseline anxiety that persisted during treatment, and 13% developed anxiety after 6 months of treatment. As for depression, 18% had baseline depression, 24% exhibited persistent baseline depression throughout the treatment, and 13% developed depression post-treatment. In the case of somatization, 13% had symptoms before starting treatment, 32% continued to experience symptoms after treatment, and 25% developed somatization symptoms after 6 months.
Sociodemographic and clinical risk factors for anxiety, depression, and somatization
Multivariable logistic regression assessing the association between pre-treatment psychological distress and sociodemographic, clinical, and psychological variables is shown in Table 3. Higher levels of anxiety and depression were identified in individuals who reported using helplessness (OR 1.02, 95% CI 1.01–1.02 and OR 1.02, 95% CI 1.01–1.02, respectively) and anxious preoccupation-based coping (OR 1.04, 95% CI 1.03–1.04 and OR 1.04, 95% CI 1.03–1.05, respectively). Additionally, cognitive avoidance was associated with greater anxiety (OR 1.01, 95% CI 1.00–1.01). In contrast, lower levels of anxiety and depression were observed in older patients (OR 0.99, 95% CI 0.98–1.00 for both), men (OR 0.66, 95% CI 0.52–0.84 and OR 0.72, 95% CI 0.56–0. 93, respectively), those with a localized cancer (OR 0.39, 95% CI 0.27–0.55 and OR 0.28, 95% CI 0.19–0.41, respectively), and those with spiritual well-being (OR 0.97, 95% CI 0.95–0.98 y OR 0.93, 95% CI 0.91–0.94, respectively). In addition, those with a positive attitude demonstrated lower level of anxiety (OR 0.99, 95% CI 0.98–1.00). Those with colorectal cancer exhibited lower level of anxiety (OR 0.63, 95% CI 0.43–0.92) and depression (OR 0.55, 95% CI 0.37–0.81). Furthermore, somatization was observed to be higher in those with anxious preoccupation (OR 1.02, 95% CI 1.01–1.02), while older age (OR 0.99, 95% CI 0.98–1.00), colorectal cancer (OR 0.59, 95% CI 0.42–0.83), and localized (OR 0.40, 95% CI 0.29–0.56) had lower levels, as did those with spiritual well-being (OR 0.97, 95% CI 0.95–0.98) (Table 4).
In the post-treatment phase, it was observed that 46% of patients displayed scores indicative of anxiety, 38% showed scores suggestive of depression, and 57% had scores consistent with somatization. Multivariable logistic regression assessing the association between post-treatment psychological distress and sociodemographic, clinical, and psychological variables is shown in Table 5. Anxious preoccupation was associated with increased risk of post-treatment anxiety (OR 1.02, 95% CI 1.01–1.03), depression (OR 1.02, 95% CI 1.01–1.03) and somatization (OR 1.01, 95% CI 1.00–1.02). In addition, higher levels of baseline anxiety (OR 2.16, 95% CI 1.59–2.93), depression (OR 3.15, 95% CI 2.26–4.39) and somatization (OR 2.78, 95% CI 2.08–3.72) were found to be associated with higher post-treatment psychological distress. Moreover, patients with a localized cancer were observed to have lower levels of anxiety (OR 0.44, 95% CI 0.28–0.71) and somatization (OR 0.62, 95% CI 0.39–0.98). Helplessness was also linked to a greater risk of somatization (OR 0.99, 95% CI 0.98–1.00).
Relationship between pre- and post-treatment psychological distress and coping strategies, and path Analysis
The model exhibited good fit to the data, as indicated by the following statistics: χ2 = 27.255, p = 0.001; CFI = 0.978; TLI = 0.953; RMSEA = 0.067. As depicted in Fig. 1, pre-treatment psychological distress correlates positively with helplessness (β = 0.25) and anxious preoccupation (β = 0.53), and also influences post-treatment psychological distress (β = 0.46). Conversely, it shows a negative correlation with positive attitude (β = − 0.26). Furthermore, anxious preoccupation directly and positively impacts post-treatment psychological distress (β = 0.11).
Discussion
This study found a correlation between psychological distress (including anxiety, depression, and somatization), younger age, and anxious preoccupation-based coping in a large sample of cancer patients (n = 1807). Conversely, localized resected cancer and spirituality were found to be protective factors. Male patients and those with a positive attitude were less likely to present with anxiety (OR 0.66, 95% CI 0.52–0.84 and OR 0.99, 95% CI 0.98–0.99, respectively) and depression (OR 0.72, 95% CI 0.56–0.92 and OR 0.99, 95% CI 0.98–0.99, respectively). Those with colorectal cancer were less prone to suffer from anxiety (OR 0.63, 95% CI 0.43–0.92), depression (OR 0. 55, 95% CI 0.37–0.81) and somatization (OR 0.59, 95% CI 0.42–0.83). After systemic cancer treatment, it was observed that patients with pre-existing anxiety (OR 2.16, 95% CI 1.59–2.93), depression (OR 3.15, 95% CI 2.26–4.39), and somatization (OR 2.78, 95% CI 2.08–3.72) experienced an increase in psychological distress. Similarly, those with anxious preoccupation developed an increased in anxiety (OR 1.02, 95% CI 1.01–1.03), depression (OR 1.02, 95% CI 1.01–1.03) and somatization (OR 1.01, 95% CI 1.00–1.02). Moreover, the path analysis reaffirmed that anxious preoccupation is associated with post-treatment psychological distress. On the other hand, those with localized cancer showed reduced levels of anxiety (OR 0.44, 95% CI 0.28–0.71) and somatization (OR 0.62, 95% CI 0.39–0.98).
We have yet to uncover prospective studies assessing the impact of sociodemographic, clinical, coping and spirituality variables on psychological distress in cancer patients, though studies analyzing the influence of several of these variables have been identified. Concerning sociodemographic factors, the available data suggests that gender and age influence psychological distress in cancer patients. A Chinese study conducted in patients with thyroid cancer, for example, reported that gender could be a predictor of psychological distress27. Additionally, a Turkish study showed that female gender was associated with a higher level of anxiety and depression in outpatients with cancer28, while a Spanish study that focused on patients with resected localized cancer noted that females were more likely to suffer from depression10. In line with this, another study from Spain demonstrated that male patients develop greater stoicism, exhibiting a higher tolerance to psychological suffering29. This finding may explain the reduced access to psychosocial support systems observed in male oncology patients30.
In terms of age, several publications have demonstrated that younger age can be a predictor of psychological distress. For instance, a study of patients with localized prostate cancer reported that younger age was associated with poorer psychological functioning31, while a study of breast cancer patients showed that younger age predicted greater psychological distress32. Similarly, an American study looking at the role of younger age in psychological distress found that younger age also predicted greater psychological distress33. This greater psychological distress found in younger patients may be associated with having cancer at a time of personal, family, and professional development when the disease can interfere with and compromise responsibilities 34.
To the best of our knowledge, no studies have examined tumor location as a predictor of psychological distress. However, some studies have evaluated psychological distress in patients with different tumor sites. Our group previously investigated the biopsychosocial and clinical characteristics of patients with resected localized colon and breast cancer and observed that patients with breast cancer had higher levels of anxiety, depression, and somatization before the start of adjuvant treatment. These findings may be attributed to the psychological distress caused by the body image impact of surgical treatment35. Interestingly, the differences are lost after adjuvant treatment is completed, possibly due to the adverse effects of systemic cancer treatment toxicity36. In the present study, we found that colon cancer is associated with lower baseline anxiety (OR 0.63, 95% CI 0.43–0.92), depression (OR 0.55, 95% CI 0.37–0.81) and somatization (OR 0.59, 95% CI 0.42–0.83). However, this effect is again lost in the analyses performed at the end of treatment, probably due to the toxicity accumulated by cancer treatments, which is associated with an increase in psychological distress and affects all patients equally, regardless of tumor location. A study analyzing the spectrum of psychological disorders in cancer patients found that the greatest anxiety was suffered by patients receiving chemotherapy, a higher level of somatization was for those receiving both chemotherapy and associated radiotherapy, and depression affected more patients receiving only radiotherapy37. Our study also observed that patients receiving chemotherapy were the group with the lowest level of psychological distress compared to patients receiving other systemic cancer treatments (immunotherapy or targeted therapy). In future studies, it would be valuable to consider the primary tumor location, tumor extension, and expected response to systemic antineoplastic treatment. Understanding how these factors might influence prognosis and coping styles can provide a deeper insight into the psychological dynamics experienced by cancer patients.
The relationship between different coping strategies and psychological distress has been studied in several contexts. A study of patients with esophageal cancer found that anxious preoccupation and fighting spirit were strongly associated with psychological distress before surgical treatment, while after treatment, helplessness was the most linked coping strategy38. In a European study of patients with nasopharyngeal cancer, those with higher levels of anxiety and depression were more likely to use dysfunctional coping strategies such as helplessness and anxious preoccupation39. Similarly, cancer patients with an optimistic outlook had the fewest symptoms of anxiety and depression in other study40. It should be noted that most of these studies analyze the impact of coping strategies on psychological distress using a linear regression model, unlike our study which uses a multivariate model controlling for confounding factors. We found that anxious preoccupation was associated with anxiety, depression and somatization, helplessness with anxiety and depression, and cognitive avoidance with anxiety, while a positive attitude had a protective effect against anxiety and depression. Although the Mini-MAC scale might lead one to believe that cognitive avoidance could be adaptive, our findings have revealed an unexpected correlation with increased anxiety, suggesting a more complex relationship. Cognitive avoidance, driven by a persistent perception of threat and continuous efforts to evade cancer-related thoughts, may contribute to heightened anxiety rather than adaptive coping. Its effectiveness in the short-term contrasts with long-term ineffectiveness in managing cancer-related stress. Furthermore, our use of SEM revealed a significant relationship between psychological distress and coping strategies in patients with advanced cancer, highlighting the intensification of post-treatment psychological distress by anxious preoccupation. These findings align with those of other researchers who have observed an increase in psychological distress in patients following various oncological treatments. For instance, a study focused on quality of life in cancer patients identified a significant rise in psychological distress following chemotherapy41. Similarly, another study in breast cancer patients documented an increase in anxiety and depression post-treatment42. Our study builds upon these observations, demonstrating that there is an escalation of psychological distress after treatment connected to baseline anxious preoccupation. Additionally, a Japanese study also found that patients who express negative emotions experience greater psychological distress following surgery43. An American study identified a correlation between emotional and financial distress, attributable to the costs associated with cancer treatments44. The financial burden of treatments and the loss of productivity, owing to reduced patient functionality post-treatment, may further contribute to this increased psychological distress. Consequently, we believe it is essential to implement psychological interventions to improve coping strategies and mitigate the impact of psychological distress, especially post-treatment, thereby enhancing overall patient outcomes.
Spirituality has been found to predict psychological distress in cancer patients during the Covid-19 pandemic, with higher spirituality associated with lower distress. Previous research has corroborated our findings that spiritual well-being is associated with mental well-being and less anxiety, depression, and somatization45,46. Similarly, it has been observed that addressing spirituality appropriately can significantly influence positive patient outcomes during the oncological process47. Thus, other studies have demonstrated that cancer patients utilize spirituality as a coping mechanism during their illness, helping them to contend with experiences that threaten their sense of lifey48.
The current study has several limitations that should be noted. Firstly, although the effect of different coping strategies was statistically significant, it was minimal in a large sample size with sufficient power. Secondly, the definition of psychological distress, anxiety, depression, and somatization was based on the BSI-18 scale rather than a clinical diagnosis. Thirdly, post-treatment analyses were conducted at different times for patients with localized or advanced cancer, at 6 months and 2–3 months, respectively. This was due to the prolonged treatment of patients with advanced disease until progression or unacceptable toxicity, with the risk of increased losses if the assessment was prolonged. Fourthly, although the study was controlled for clinical, socio-demographic, and psychological variables, there may have been other factors that influenced the psychological distress of the patients that were not considered. Finally, the questionnaires used were self-completed, which may lead to response bias due to errors in interpretation, inaccurate recall, or difficulty in understanding them. Although these questionnaires have proven useful in assessing psychological distress, coping and spiritual wellbeing, they should ideally be used in conjunction with a clinical assessment.
In conclusion, this study has identified several sociodemographic, clinical, and psychological variables that may predict psychological distress in cancer patients. These include young age and female sex, the presence of advanced unresectable cancer, and cancer location outside the colon, as well as anxious preoccupation and lack of spirituality. Further research is needed to confirm these findings and inform effective interventions to address psychological distress in cancer patients.
Data availability
Statistical analyses were performed with Statistical Package for Social Sciences (SPSS) software, 25.0 version (IBM SPSS Statistics for Windows, Armonk, NY: IBM Corp). The code is available upon request to the authors.
Code availability
Patients are identified by an encrypted code known only to the local researcher. The code of the analyses is available upon request to the authors.
References
Sociedad española de Oncología Médica. Cifras del cáncer en España. https://seom.org/prensa/el-cancer-en-cifras.
Ayubi, E., Bashirian, S. & Khazaei, S. Depression and anxiety among patients with cancer during COVID-19 pandemic: A systematic review and meta-analysis. J. Gastrointest. Cancer 52, 499–507 (2021).
Wang, Y.-H. et al. Depression and anxiety in relation to cancer incidence and mortality: A systematic review and meta-analysis of cohort studies. Mol. Psychiatry 25, 1487–1499 (2020).
Rodriguez-Gonzalez, A. et al. Fatigue, emotional distress, and illness uncertainty in patients with metastatic cancer: Results from the prospective NEOETIC_SEOM study. Curr. Oncol. 29, 9722–9732 (2022).
Zhang, X. & Zhang, X. Somatization symptoms in lung cancer patients and correlative analysis between anxiety, depression and somatization symptoms. Zhongguo Fei Ai Za Zhi 20, 473–478 (2017).
Saxena, P. U. P. et al. Assessment of spectrum of mental disorders in cancer patients. J. Cancer Res. Ther. 14, 1312–1315 (2018).
Jimenez-Fonseca, P. et al. Factors associated with anxiety and depression in cancer patients prior to initiating adjuvant therapy. Clin. Transl. Oncol. 20, 1408–1415 (2018).
Darvishi, N. et al. The prevalence of depression and anxiety in patients with cancer in Iran: A systematic review and meta-analysis. Supp. Care Cancer 30, 10273–10284 (2022).
Aryankhesal, A. et al. Prevalence of depression in patients with cancer in Iran: A systematic review and meta-analysis. BMJ Supp. Palliat. Care 12, e518–e525 (2022).
Ghanem, I. et al. Coping strategies and depressive symptoms in cancer patients. Clin. Transl. Oncol. 22, 330–336 (2020).
Ma, Y. et al. Prevalence and risk factors of cancer-related fatigue: A systematic review and meta-analysis. Int. J. Nurs. Stud. 111, 103707 (2020).
Chaturvedi, S. K., PeterMaguire, G. & Somashekar, B. S. Somatization in cancer. Int. Rev. Psychiatry 18, 49–54 (2006).
Ha, S., Shim, I. & Bae, D. Differences in depressive and anxiety symptoms between cancer and noncancer patients with psychological distress. Indian J. Psychiatry 61, 395 (2019).
Grassi, L., Travado, L., Moncayo, F. L. G., Sabato, S. & Rossi, E. Psychosocial morbidity and its correlates in cancer patients of the Mediterranean area: Findings from the Southern European Psycho-Oncology Study. J. Affect. Disord. 83, 243–248 (2004).
Ferrero, J., Barreto, M. P. & Toledo, M. Mental adjustment to cancer and quality of life in breast cancer patients: An exploratory study. Psychooncology 3, 223–232 (1994).
Lin, H.-R. & Bauer-Wu, S. M. Psycho-spiritual well-being in patients with advanced cancer: An integrative review of the literature. J. Adv. Nurs. 44, 69–80 (2003).
Salsman, J. M. et al. A meta-analytic approach to examining the correlation between religion/spirituality and mental health in cancer. Cancer 121, 3769–3778 (2015).
Kang, K.-A., Han, S.-J., Lim, Y.-S. & Kim, S.-J. Meaning-centered interventions for patients with advanced or terminal cancer. Cancer Nurs. 42, 332–340 (2019).
D’Souza, K. & Astrow, A. B. Patient spirituality as a component of supportive care: Assessment and intervention. Curr. Treat Options Oncol. 21, 11 (2020).
Derogatis, L. R. & Melisaratos, N. The Brief Symptom Inventory: An introductory report. Psychol. Med. 13, 595–605 (1983).
Acosta, F. X., Nguyen, L. H. & Yamamoto, J. Using the brief symptom inventory to profile monolingual spanish-speaking psychiatric outpatients. J. Clin. Psychol. 50, 723–726 (1994).
Watson, M. et al. The mini-MAC. J Psychosoc. Oncol. 12, 33–46 (1994).
Calderon, C. et al. Psychometric properties of Spanish version of the Mini-Mental Adjustment to Cancer Scale. Int. J. Clin. Health Psychol. 21, 100185 (2021).
Peterman, A. H., Fitchett, G., Brady, M. J., Hernandez, L. & Cella, D. Measuring spiritual well-being in people with cancer: The functional assessment of chronic illness therapy—spiritual well-being scale (FACIT-Sp). Ann. Behav. Med. 24, 49–58 (2002).
Jimenez-Fonseca, P. et al. The mediating role of spirituality (meaning, peace, faith) between psychological distress and mental adjustment in cancer patients. Supp. Care Cancer https://doi.org/10.1007/s00520-017-3969-0 (2017).
Schermelleh‐Engel K, M. H. M. H. Evaluating the fit of structural equation models: Tests of significance and descriptive goodness‐of‐fit measures. in Methods of Psychological Research Online 2003, Vol.8, No.2, pp. 23–74 Department of Psychology Internet: http://www.mpr-online.de © 2003 University of Koblenz-Landau .
Gao, J. et al. Prevalence and predictors of psychological distress among patients with thyroid cancer during transitional period in China: A cross-sectional study. Supp. Care Cancer 30, 7903–7911 (2022).
Erdoğan Yüce, G., Döner, A. & Muz, G. Psychological distress and its association with unmet needs and symptom burden in outpatient cancer patients: A cross-sectional study. Semin. Oncol. Nurs. 37, 151214 (2021).
Gomez, D. et al. Stoic attitude in patients with cancer from the NEOcoping study: Cross-sectional study. PLoS One 17, e0269712 (2022).
Manii, D. & Ammerman, D. Men and cancer. J. Psychosoc. Oncol. 26, 87–102 (2008).
Bisson, J. I. et al. The prevalence and predictors of psychological distress in patients with early localized prostate cancer. BJU Int. 90, 56–61 (2002).
Syrowatka, A. et al. Predictors of distress in female breast cancer survivors: A systematic review. Breast Cancer Res. Treat 165, 229–245 (2017).
Acquati, C. & Kayser, K. Predictors of psychological distress among cancer patients receiving care at a safety-net institution: The role of younger age and psychosocial problems. Supp. Care Cancer 25, 2305–2312 (2017).
Fonseca, C. C. P. & Bayonas, J. Why young patients with cancer require different coping tools?. Abnormal Behav. Psychol. 3, 129–130 (2017).
Kagee, A., Roomaney, R. & Knoll, N. Psychosocial predictors of distress and depression among South African breast cancer patients. Psychooncology 27, 908–914 (2018).
García-García, T. et al. Biopsychosocial and clinical characteristics in patients with resected breast and colon cancer at the beginning and end of adjuvant treatment. BMC Cancer 19, 1143 (2019).
Prakash Saxena, P. et al. Assessment of spectrum of mental disorders in cancer patients. J. Cancer Res. Ther. (2018).
Ohkura, Y. et al. Association between psychological distress of each points of the treatment of esophageal cancer and stress coping strategy. BMC Psychol. 10, 214 (2022).
Ghiggia, A. et al. Psychological distress and coping in nasopharyngeal cancer: An explorative study in Western Europe. Psychol. Health Med. 22, 449–461 (2017).
Gustavsson-Lilius, M., Julkunen, J., Keskivaara, P., Lipsanen, J. & Hietanen, P. Predictors of distress in cancer patients and their partners: The role of optimism in the sense of coherence construct. Psychol. Health 27, 178–195 (2012).
Lewandowska, A. et al. Quality of life of cancer patients treated with chemotherapy. Int. J. Environ. Res. Public Health 17, 6938 (2020).
Grusdat, N. P. et al. Routine cancer treatments and their impact on physical function, symptoms of cancer-related fatigue, anxiety, and depression. Supp. Care Cancer 30, 3733–3744 (2022).
Nakatani, Y. et al. The relationship between emotional suppression and psychological distress in breast cancer patients after surgery. Jpn. J. Clin. Oncol. 44, 818–825 (2014).
Meeker, C. R. et al. Relationships among financial distress, emotional distress, and overall distress in insured patients with cancer. J. Oncol. Pract. 12, e755–e764 (2016).
Bovero, A. et al. The spirituality in end-of-life cancer patients, in relation to anxiety, depression, coping strategies and the daily spiritual experiences: A cross-sectional study. J. Relig. Health 58, 2144–2160 (2019).
Ciria-Suarez, L. et al. Correction to: Optimism and social support as contributing factors to spirituality in Cancer patients. Supp. Care Cancer 29, 3375–3376 (2021).
Richardson, P. Assessment and implementation of spirituality and religiosity in cancer care. Clin. J. Oncol. Nurs. 16, E150–E155 (2012).
Visser, A., Garssen, B. & Vingerhoets, A. Spirituality and well-being in cancer patients: A review. Psychooncology 19, 565–572 (2010).
Acknowledgements
The authors are grateful to the Bioethics Section of the SEOM for their contribution to this study. We would like to thank the IRICOM team for the support of the website registry and specially Natalia G Cateriano and Miguel Vaquero.
Funding
This work is funded by the FSEOM (Spanish Society of Medical Oncology Foundation) grant for Projects of the Collaborative Groups in 2018 and by an Astra Zeneca grant.
Author information
Authors and Affiliations
Contributions
V.V., C.C. and P.J.F. developed the project, analyzed the data, and drafted the manuscript. The other authors recruited patients and provided clinical information, data curation, comments, and improvements to the manuscript. All authors participated in the conceptualization, interpretation and discussion of data, supervision, visualization, and the critical review and edition of the manuscript.
Informed consent and approval by the national competent authorities includes permission for publication and diffusion of the data.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Velasco-Durantez, V., Cruz-Castellanos, P., Hernandez, R. et al. Prospective study of predictors for anxiety, depression, and somatization in a sample of 1807 cancer patients. Sci Rep 14, 3188 (2024). https://doi.org/10.1038/s41598-024-53212-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-53212-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.