Abstract
The waiting time to deceased-donor kidney transplantation (DDKT) is long in Asian countries. We investigated the impact of sensitization and ABO blood type (ABO) on DDKT opportunity using two Korean cohorts: a hospital cohort from two centers and a national database. The impact of panel reactive antibody (PRA) based on the maximal PRA% and ABO on DDKT accessibility was analyzed using a competing risks regression model. In the hospital cohort (n = 4722), 88.2%, 8.7%, and 3.1% of patients belonged to < 80%, 80–99%, and ≥ 99% PRA groups, respectively, and 61.1%, 11.6%, and 27.3% belonged to A or B, AB, and O blood types, respectively. When PRA and ABO were combined, PRA < 80%/A or B and 80 ≤ PRA < 99%/AB had fewer DDKT opportunities (median, 12 years; subdistribution hazard ratio [sHR], 0.71) compared with PRA < 80%/AB (median, 11 years). Also, PRA < 80%/O, 80 ≤ PRA < 99%/A or B, and PRA ≥ 99%/AB had a much lower DDKT opportunity (median, 13 years; sHR, 0.49). Furthermore, 80 ≤ PRA < 99%/O and PRA ≥ 99%/non-AB had the lowest DDKT opportunity (sHR, 0.28). We found similar results in the national cohort (n = 18,974). In conclusion, an integrated priority system for PRA and ABO is needed to reduce the inequity in DDKT opportunities, particularly in areas with prolonged waiting times.
Similar content being viewed by others
Introduction
Kidney transplantation is the best treatment option for patients with end stage renal disease (ESRD)1,2,3. Deceased donation rates have been much lower in Asian countries than in Western countries4, whereas the recent ESRD incidence is higher in Asian countries than in Western countries5. Therefore, donor organ shortages are more severe and the waiting time for deceased-donor kidney transplantation (DDKT) is much longer in Asian countries6.
In patients on the waiting list for DDKT, sensitization to human leukocyte antigen (HLA) is a major barrier to DDKT allocation7,8. By assessing the reactivity of a waitlist patients’ serum with HLA antigens on beads, the panel reactive antibodies (PRA) are reported as a percentage based on the frequency of positive HLA antigens in the estimated donor pool, and the overall probability of recipient mismatching for donor pools is approximated. PRAs indicate the sensitization status of waitlisted patients9. Prioritization of DDKT candidates with higher PRA has been adopted in many kidney allocation systems, including the Unites States (US), United Kingdom (UK), Eurotransplant, Australia and New Zealand, to provide a fair DDKT opportunity and maintain an equity principle10,11,12.
The ABO blood type also induce inequity in DDKT opportunity13 due to the biological ABO blood type compatibility between the donors and recipients. O-type candidates are only biologically compatible with O-type donors, which limits their potential donor pool. In contrast, AB-type candidates are biologically compatible with A, B, and O donors, expanding their potential donor pool.
In the Korean kidney allocation system, adult waitlisted patients are prioritized based on HLA full match. Among waitlisted patients with zero HLA mismatch, deceased donor kidneys are allocated to patients with identical ABO blood types. When there is no candidate with the identical blood types, kidneys are allocated to waitlisted patients with compatible blood types. In cases of HLA mismatches, allocation is determined through a point system that consists of the degree of HLA matching (0–2 points), duration on the waiting (1 point for each year of wait), history of kidney transplantation or repeated, positive cross-match test results (2 points), and personal or familial history of organ donation (2–4 points). There is no additional point according to ABO blood types or PRA levels.
Sensitization might have decreased DDKT accessibility more seriously in Asian countries, including Korea, which have a longer waiting time than Western countries. Yet, the impact of sensitization on DDKT waiting period in Asian countries has not been studied in a nationwide cohort. Therefore, we aimed to investigate the impact of sensitization and ABO blood types on DDKT opportunities in a Korean nationwide database as well as a hospital-based database.
Patients and methods
Patients
Data from two cohorts were analyzed in this study. First, the hospital cohort comprised 5322 waitlisted patients from Severance Hospital and Seoul National University Hospital between February 15, 2000 and July 31, 2021. Of those, 4722 patients were included in the final analysis after excluding 133 patients ≤ 18 years who received additional points in the current Korean kidney allocation scheme and 477 patients without PRA data (Supplementary Fig. S1). Second, the national cohort was retrieved from the Korean Organ Network for Organ Sharing (KONOS) database between January 1, 2000 and December 31, 2018. A total of 18,974 patients were included in the study from a total of 35,859 patients; 106 patients ≤ 18 years and 16,779 without PRA data were excluded (Supplementary Fig. S1).
This study was performed in accordance with the 2000 Declaration of Helsinki14 and the Declaration of Istanbul 200815, and was approved by the Institutional Review Board of Severance Hospital (4-2023-0244) and Seoul National University Hospital (H-2304-061-1421). Informed consent was waived by the Institutional Review Board of Severance Hospital (4-2023-0244) and Seoul National University Hospital (H-2304-061-1421) owing to the retrospective nature of the study, which involved medical records without identifiable patient information.
Data collection
Data from the hospital cohort were obtained from the electronic medical records of Severance Hospital and Seoul National University Hospital. National cohort data were obtained from the KONOS database. Clinical information, such as age, sex, ABO blood type, and diabetes mellitus status were extracted. The primary outcome was the number of waitlisted patients’ who underwent DDKT.
PRA information
In the hospital cohort, PRA was assessed using LABScreen single-antigen assays, identification assays (One Lambda Inc., Canoga Park, CA, USA), LIFECODES single-antigen assay, or identification assays (Immunocor Inc., Norcross, GA, USA). Maximum PRA values in percentages (max PRA%) among class I and II PRA values in PRA identification assays were used before single-antigen bead assays were introduced, and we then used higher values (%) among class I and II calculated PRA (cPRA) in the single-antigen assays were used after single-antigen bead assays were introduced. In the national cohort, most PRA data were collected as positive or negative instead of as a specific percentage of PRA; therefore, these qualitative PRA results were used in the analysis. We defined a negative PRA as having a value of 0% for both PRA class I and class II. Conversely, we defined a positive PRA as a case where either class I or class II showed a PRA value greater than 0%. Waitlisted patients were categorized into three PRA groups according to the max PRA% as follows: low (PRA < 80%), intermediate (80 ≤ PRA < 99%), and high (PRA ≥ 99%) in hospital cohort. They were also categorized into positive and negative PRA groups in both hospital and national cohort.
Statistical analyses
Comparisons of clinical characteristics between the PRA groups were performed using the Mann–Whitney U test or Kruskal–Wallis test for continuous variables. For categorical variables, the chi-squared test or Fisher’s exact test was used, as appropriate. Continuous variables were presented as medians (interquartile range [IQR]), and categorical variables were presented as absolute numbers (percentages). Kaplan–Meier survival analysis was used to assess the cumulative DDKT rates, and the log–rank test was used to compare DDKT rates between the PRA groups. The independent association of PRA groups or ABO bloody types with accessibility to DDKT was analyzed using Fine and Gray competing risks regression models to estimate the subdistribution hazard ratio (sHR) of DDKT, accounting for death while on the waiting list as a competing risk16. We reported the sHR with a 95% confidence interval (CI). The multivariate model for PRA was adjusted for age, sex, baseline diabetes mellitus status, and ABO blood type. P < 0.05 was considered statistically significant. All analyses were conducted using the R software (R Foundation for Statistical Computing, www.r-project.org, ver.4.2.2).
Results
Characteristics of the hospital cohort
A total of 4722 patients were included in the hospital cohort. The median age was 53 (IQR 44–60) years and 1858 (39.3%) were women. At the median follow-up time of 5 years, 819 (17.3%) had underwent DDKT. Regarding PRA, 4163 (88.2%), 412 (8.7%), and 147 (3.1%) patients belonged to the low, intermediate, and high PRA groups, respectively. Patients in the high PRA group were younger, and more likely to be women (Table 1). The high PRA group had longer waiting times and was less likely to undergo DDKT (Table 1).
Characteristics of the national cohort
Among the 18,974 patients in the national cohort, the median follow-up time was 3 years. The median age was 55 (IQR 47–62), and 39.0% were women (Supplementary Table S1). PRA was positive in 7910 (41.7%) of the patients in this cohort. Patients in the positive-PRA group were more likely to be female and less likely to undergo DDKT with longer waiting times (Supplementary Table S1).
Impact of PRA sensitization on DDKT
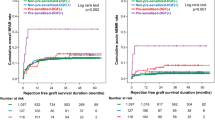
In the hospital cohort, Kaplan–Meier analyses showed that both the intermediate PRA group (80 ≤ PRA < 99%, median 18 years; 95% CI 13– not applicable) and the high PRA group (PRA ≥ 99%, median not applicable) waited longer for DDKT than the low PRA group (PRA < 80%, median 12 years; 95% CI 11–12 years) (P < 0.001, Fig. 1A). We found that the positive-PRA group (median 13 years; 95% CI 12–not applicable) had a longer waiting time for DDKT than the negative-PRA group (median 12 years; 95% CI 11–13 years) when PRA was categorized into negative and positive groups (P = 0.047).
Cumulative DDKT rates according to PRA. (A) Cumulative DDKT rates according to PRA groups (low [< 80%], intermediate [80 ≪ 99%], high [≥ 99%]) in the hospital cohort. (B) Cumulative DDKT rates according to PRA groups (positive versus negative PRA) in the national cohort. DDKT deceased donor kidney transplantation, max maximum, PRA panel reactive antibody.
Competing risks regression analysis revealed that the higher PRA group had a lower opportunity for DDKT after adjusting for other covariates (Table 2). Compared to the low PRA group (PRA < 80%), the intermediate PRA group (80 ≤ PRA < 99%) had a lower chance to receive DDKT by 36% (sHR, 0.64; 95% CI 0.49–0.83; P < 0.001) and DDKT probability was reduced by 58% (sHR, 0.42; 95% CI 0.26–0.68; P < 0.001) in the high PRA group (PRA ≥ 99%). When we categorized PRA into two groups, sensitized patients (positive PRA group) had fewer opportunities for DDKT (sHR, 0.85; 95% CI 0.74–0.99; P = 0.032) compared with the non-sensitized patients (negative PRA group). Maximal PRA% as a continuous variable was also significantly associated with a decreased likelihood of DDKT (sHR 0.99, 95% CI 0.99–1.00; P < 0.001).
Similar results were observed in a national cohort study. Kaplan–Meier analyses demonstrated that the sensitized group with positive PRA waited longer for DDKT (median not applicable years; 95% CI 16– not applicable) than the non-sensitized group with negative PRA (median 11 years; 95% CI 10–13 years) (P < 0.001, Fig. 1B). Competing risks regression results also showed that sensitized patients had a lower opportunity of DDKT (sHR, 0.72; 95% CI 0.67–0.77; P < 0.001) compared to the non-sensitized patients after adjusting for other covariates (Table 2).
Impact of ABO blood type on DDKT
In both national and hospital cohorts, only 88.6–88.7% of type O donors were allocated to type O recipients, whereas 100.0% of type AB donors were allocated to type AB recipients and 94.5–97.4% of type A or B donors were allocated to recipients with the same blood types (Supplementary Table S2).
In the hospital cohort, Kaplan–Meier analyses showed that the AB blood type (P < 0.001) waited for a shorter period and the O blood type (P < 0.001) waited longer for DDKT compared with the A or B blood type (Fig. 2A). Competing risks regression analysis demonstrated that blood type AB increased the probability of DDKT (sHR, 1.37; 95% CI 1.13–1.67; P = 0.002) and blood type O reduced DDKT probability (sHR, 0.69; 95% CI 0.59–0.82; P < 0.001) compared with blood types A or B (Table 3).
In the national cohort, Kaplan–Meier analyses also showed that patients with the AB blood type waited for a shorter time (P < 0.001) and those with the O blood type waited for a longer period (P < 0.001) for DDKT than those with the A or B blood type (Fig. 2B). Multivariate competing risks regression analysis demonstrated that blood type AB patients had a higher DDKT probability (sHR, 1.45; 95% CI 1.31–1.59; P < 0.001) and blood type O patients had a lower DDKT probability (sHR, 0.73; 95% CI 0.67–0.79; P < 0.001) compared with patients with blood types A or B (Table 3). Blood types A and B had similar patterns in both the hospital cohort and the national cohort and they were combined for this analysis.
Impact of PRA sensitization and ABO blood types on DDKT in the hospital cohort
When we assessed DDKT accessibility according to a combination of three PRA groups (low PRA [< 80%], intermediate PRA [80 ≤ < 99%], high PRA [≥ 99%]) and three ABO blood groups (AB, A or B, O), Kaplan–Meier analyses showed that the low PRA with blood type AB had the highest DDKT opportunity (category H1, median 11 years) followed by the low PRA/A or B group and the intermediate PRA/AB group (category H2, median 12 years, P < 0.001, Fig. 3A). Next, the low PRA/O, intermediate PRA/A or B, and high PRA/AB groups (category H3, median 13 years) had fewer opportunities to access DDKT than category H2 (P < 0.001, Fig. 3A). The intermediate PRA/O and high PRA/A, B, or O groups had the lowest DDKT opportunity (category H4, median not applicable, P = 0.001 compared to category H3, Fig. 3A).
Cumulative DDKT rates according to a combination of PRA and ABO blood types. (A) Cumulative DDKT rates according to a combination of PRA and ABO blood types in the hospital cohort. (B) Cumulative DDKT rates according to a combination of PRA and ABO blood types in the national cohort. DDKT deceased donor kidney transplantation, PRA panel reactive antibody.
Next, we compared DDKT opportunity according to the combination of the three PRA and three ABO blood groups using competing risks regression analysis (Table 4). Compared with the low PRA/AB group (reference group), the low PRA/A or B groups (sHR, 0.72) had fewer opportunities. The low PRA/O group (sHR, 0.50), intermediate PRA/A or B group (sHR, 0.48), and the high PRA/AB group (sHR, 0.35) also had fewer opportunities than the low PRA/AB group. Furthermore, the intermediate PRA/O group (sHR, 0.29), high PRA/A or B group (sHR, 0.26), and high PRA/O group had the lowest opportunities (sHR, 0.31).
When groups with similar DDKT opportunities were divided into four categories, as shown in Fig. 3A, we observed a categorical hierarchy of DDKT opportunities as follows: 1 (reference), 2 (sHR 0.71), 3 (sHR 0.49), and 4 (sHR 0.28) in the multivariate analysis (Table 5).
Impact of PRA sensitization and ABO blood types on DDKT in the national cohort
In the national cohort, we compared DDKT accessibility according to the combination of the two PRA groups and three ABO blood types (Table 4, Fig. 3B). Kaplan–Meier analyses showed that the negative PRA/A or B group (median, 10 years) and positive PRA/AB group (median 12 years) waited longer for DDKT than the negative PRA/AB group (median 8 years, P < 0.001, Fig. 3B). The negative PRA/O group (median, 15 years) and the positive PRA/A or B groups (median, 17 years) waited for a much longer time for DDKT. Moreover, the positive PRA/O group waited for the longest (median, not applicable, Fig. 3B).
In parallel with the survival curves, multivariate competing risks regression analysis demonstrated a similar hierarchy in DDKT opportunity according to the combination of PRA and ABO blood types (Table 4). Compared to the negative PRA/AB group (reference group), the negative PRA/A or B group (sHR, 0.66) and positive PRA/AB group (sHR, 0.65) had fewer opportunities. The negative PRA/O group (sHR, 0.47) and the positive PRA/A or B groups (sHR, 0.48) had much fewer opportunities. Furthermore, the positive PRA/O group had the lowest number of opportunities (sHR, 0.36).
When groups with similar DDKT opportunities were divided into four categories, there was a categorical hierarchy of DDKT opportunities in the following order: 1 (median, 8 years), 2 (median, 11 years, sHR 0.66), 3 (median, 16 years, sHR 0.48), and 4 (median not applicable, sHR 0.36) in the multivariate analysis (Table 5).
Discussion
This study found that sensitization, represented by a positive or high PRA, increased the waiting period for DDKT and decreased DDKT opportunities in both hospital-based and national cohorts. Additionally, the waiting time or accessibility to DDKT differed according to the ABO blood type. Furthermore, by categorizing waitlisted patients according to a combination of PRA and ABO blood types, we identified a more precise hierarchy of DDKT opportunities.
Previous studies in the USA, Australia, and Mexico have shown that the probability of receiving DDKT decreases with higher PRA levels17,18,19. A German study reported a decreased likelihood of receiving DDKT for candidates with a virtual PRA (vPRA) > 85% who are younger than 65 years, and those with a vPRA > 50% who are older than 65 years. In both age groups, patients with a vPRA > 95% showed a further decrease in DDKT probability and longer waiting times9. According to the current Korean kidney allocation system, we also found that the probability of receiving DDKT decreases with higher PRA levels. Positive PRA significantly decreased the opportunity for DDKT in both hospital-based and national cohorts. Furthermore, both the high and the intermediate PRA groups had fewer DDKT opportunities than the low PRA group in the hospital cohort. Since the median DDKT waiting time is > 10 years in Korea, even for non-sensitized waitlisted patients, the delay due to sensitization probably has a more serious impact on DDKT opportunity for highly-sensitized patients, particularly in Korea compared with Western countries.
To resolve the sensitization-related inequity in DDKT opportunity, a new kidney allocation system was introduced in the US in 2014, which utilizes a sliding scale ranging from 0 to 200 points for candidates based on cPRA levels instead of the previous low scores (0–4)11,20. After the implementation of the new allocation system, particularly for highly-sensitized patients with a cPRA ≥ 90%, there have been improvements in the kidney access disparity related to HLA sensitization without any difference in graft survival outcomes21,22. In Israel, the adoption of the sliding scale points based on PRA improved equity in highly-sensitized patients. In the UK, Australia, and Eurotransplant, kidney allocation systems proved additional points for highly-sensitized candidates based on PRA to compensate for sensitization-related disparity12.
Our study revealed a significant difference in DDKT opportunities among different ABO blood types in both hospital-based and national cohorts. Patients with blood type O had the lowest DDKT opportunity, whereas those with blood types A or B had an intermediate DDKT opportunity, and those with blood type AB had the highest DDKT opportunity. Blood type O candidates received less than half of the opportunity for DDKT compared with blood type AB candidates and had more than 30% fewer chances for DDKT compared with non-O blood type candidates. This disparity occurred because candidates with O type are restricted to ABO-identical transplantation, whereas kidneys from blood group O donors can be given to non-O blood group recipients if no candidate with the same ABO blood type is available. Despite the disparity in DDKT opportunities due to ABO blood type, most of kidney allocation systems do not address this including those in the US, UK, Eurotransplant, France, and Korea10,11,12,23. Therefore, additional points should be considered for candidates with disadvantaged blood types and high PRA to correct the current inequity.
Efforts to reduce the inequity related to ABO blood type have been attempted for the A2 subtype of blood type A24,25,26. Since the antigen expression of A2 subtype is much lower than that of A1, A2 is functionally similar to blood type O and A2B is similar to blood type B in terms of ABO antigen expression27. In the US, access to transplantation for blood type B was increased to improve equity. Owing to the prolonged waiting time among other blood groups, the new 2014 KAS preferentially allocated A2 and A2B kidneys to B candidates28,29. Since the introduction of the new KAS, utilization of A2 kidneys for blood group B candidates has increased, while patient and graft outcomes remained consistent with those of conventional ABO-compatible DDKT, although there is a report of increased anti-A titer30,31,32,33. In a recent Canadian study, a new ABO-adjusted cPRA, which adjusts ABO sensitization on the same scale as HLA sensitization, was proposed to solve the disparity in kidney allocation for blood types B and O. Similarly, for the calculation of cPRA based on HLA sensitization, the ABO-adjusted cPRA is calculated based on the frequency of ABO blood groups in the donor pools. Candidates with blood types B and O, who have fewer opportunities for DDKT due to their blood type, can be assigned more bonus kidney allocation points through this system34,35.
We found that both the PRA and ABO blood types had significant effects on DDKT accessibility. Therefore, we assessed DDKT accessibility according to a combination of PRA status and ABO blood type. In the hospital-based cohort with more detailed PRA information, we categorized the groups into four categories with similar DDKT opportunities. First, the low PRA with blood type AB group (category H1) had the highest probability of receiving DDKT, followed by the low PRA/A or B and the intermediate PRA/AB groups (category H2). Next, the low PRA/O, intermediate PRA/A or B, and high PRA/AB groups (category H3) had much lower DDKT opportunities. The intermediate PRA/O and high PRA/non-AB groups (category H4) had the lowest probability of DDKT. In the national cohort with limited PRA information, we also categorized the groups into four categories with similar DDKT opportunities. Negative PRA with blood AB (category N1) had the highest DDKT opportunity, while positive PRA with blood group O (category N4) had the lowest DDKT opportunity. These data suggest that the combination of PRA and ABO blood type could provide more precise information regarding DDKT accessibility to waitlisted patients and medical staff than PRA information alone.
Since sensitization and ABO blood type significantly increased the waiting time for DDKT, priority scores should be given to sensitized candidates with blood type O to solve the inequity in DDKT opportunities. This issue is more critical in Asian countries, including Korea, which have long waiting times. For example, the recent mean waiting time was 6.5 years among Korean DDKT patients36. Moreover, the median waiting time until DDKT is > 10 years in Korea if all waitlisted patients are included in the calculation. However, the current Korean allocation system coordinated by KONOS, a governmental agency, only assigns two additional points to patients with prior cross-match positivity or a history of prior transplantation, and no additional points according to ABO blood type37. Given that the waiting time for highly sensitized patients has significantly decreased after the introduction of a new kidney allocation system in the US21,38, we need to revise the current system with higher compensatory points for waitlisted patients with a high PRA or blood type O to reduce the disadvantage of this population. Considering that the mean waiting time for DDKT patients ≤ 18 years who receive additional 3–4 points depending on age is 2.5 years, in contrast to adult DDKT patients with a median waiting time of 6.5 years, the appropriate advantage points could effectively improve the existing inequities related to blood types and PRA in the organ allocation process in Korea36.
To assign higher points based on PRA and ABO blood types for equitable kidney allocation, we also need to verify whether or not such allocation systems result in worse patient and graft survival on a national scale with respect to utility. For example, the allocation of more kidneys to sensitized patients without donor-specific antibodies would have a potential risk of increased rejection and worse graft outcomes. In addition to more benefits to highly-sensitized patients and patients with A2 blood type, the new US KAS has not led to worse graft and patient outcomes to date21,22,30,31,32,33. However, the outcomes for very highly sensitized patients with cPRA 100% is still controversial38. Therefore, a new kidney allocation scoring system that balances equity with utility should be developed. Even after the introduction of the new allocation system, a follow-up assessment is essential to determine whether assigning additional allocation points based on PRA and blood type would significantly enhance equity without compromising utility.
This study had several limitations. First, our cohorts did not implement cPRA, because cPRA had not been used in most Korean centers and it was recently introduced. We used the max PRA% for the analysis, which represented the highest PRA values between PRA Class I and II. This could have led to an overestimation of PRA values; therefore, a direct comparison with other kidney allocation systems that use cPRA may be difficult. Second, the impact of PRA% was analyzed only in the hospital cohort, and the results may not be representative of the entire Korean DDKT population because the national cohort provided only PRA positivity. Further studies using cPRA and ABO blood types are required to confirm these findings.
Nevertheless, this is the first nationwide study on the impact of sensitization on DDKT opportunity in Asian countries with prolonged waiting time and is expected to contribute to a better understanding of the current allocation system beyond Western countries. Furthermore, the analysis of the impact of PRA in combination with ABO blood type is a new approach solving inequity according to ABO blood type as well as PRA. We hope to develop a more integrated allocation scoring system based on this approach.
In summary, we found that both PRA and ABO blood types had significant impacts on DDKT opportunities. Highly-sensitized waitlisted patients with blood type O are unfairly disadvantaged, leading to serious inequity, especially in Asian countries with very long waiting times. Therefore, a new allocation system with higher additional points based on PRA and ABO blood types is required to improve the inequity in DDKT opportunities.
Data availability
Data supporting the findings of this study are available from the corresponding author upon reasonable request.
References
Abecassis, M. et al. Kidney transplantation as primary therapy for end-stage renal disease: A National Kidney Foundation/Kidney Disease Outcomes Quality Initiative (NKF/KDOQITM) conference. Clin. J. Am. Soc. Nephrol. 3, 471–480 (2008).
Tonelli, M. et al. Systematic review: Kidney transplantation compared with dialysis in clinically relevant outcomes. Am. J. Transplant. 11, 2093–2109 (2011).
Suthanthiran, M. & Strom, T. B. Renal transplantation. N. Engl. J. Med. 331, 365–376 (1994).
International Registry in Organ Donation and Transplantation. Worldwide Actual Deceased Organ Donors Rate 2021. Accessed April 25, 2023. https://www.irodat.org/img/database/grafics/2021_01_worldwide-actual-deceased-organ-donors.png.
United States Renal Data System. 2022 Annual Report, End Stage Renal Disease. Chapter11: International Comparisons. Accessed April 25, 2023. https://usrds-adr.niddk.nih.gov/2022/end-stage-renal-disease/11-international-comparisons.
Ryu, J. H. et al. Factors associated with waiting time to deceased donor kidney transplantation in transplant candidates. Transplant. Proc. 50, 1041–1044 (2018).
Clark, B. & Unsworth, D. J. HLA and kidney transplantation. J. Clin. Pathol. 63, 21–25 (2010).
Ogura, K. et al. The significance of a positive flow cytometry crossmatch test in primary kidney transplantation. Transplantation 56, 294–298 (1993).
Zecher, D. et al. Impact of sensitization on waiting time prior to kidney transplantation in Germany. Transplantation 106, 2448–2455 (2022).
Mayer, G. & Persijn, G. G. Eurotransplant kidney allocation system (ETKAS): Rationale and implementation. Nephrol. Dial. Transplant. 21, 2–3 (2006).
Friedewald, J. J. et al. The kidney allocation system. Surg. Clin. North Am. 93, 1395–1406 (2013).
Wu, D. A. et al. Global trends and challenges in deceased donor kidney allocation. Kidney Int. 91, 1287–1299 (2017).
Roodnat, J. I., van de Wetering, J., Claas, F. H., Ijzermans, J. & Weimar, W. Persistently low transplantation rate of ABO blood type O and highly sensitised patients despite alternative transplantation programs. Transpl. Int. 25, 987–993 (2012).
Hurst, S. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 310, 2191–2194 (2013).
Abboud, O. et al. The Declaration of Istanbul on organ trafficking and transplant tourism. Kidney Int. 74, 854–859 (2008).
Noordzij, M. et al. When do we need competing risks methods for survival analysis in nephrology?. Nephrol. Dial. Transplant. 28, 2670–2677 (2013).
Sypek, M. P. et al. The introduction of cPRA and its impact on access to deceased donor kidney transplantation for highly sensitized patients in Australia. Transplantation 105, 1317–1325 (2021).
Bostock, I. C. et al. Probability of deceased donor kidney transplantation based on % PRA. Transpl. Immunol. 28, 154–158 (2013).
Jackson, K. R. et al. The national landscape of deceased donor kidney transplantation for the highly sensitized: Transplant rates, waitlist mortality, and posttransplant survival under KAS. Am. J. Transplant. 19, 1129–1138 (2019).
Stegall, M. D., Stock, P. G., Andreoni, K., Friedewald, J. J. & Leichtman, A. B. Why do we have the kidney allocation system we have today? A history of the 2014 kidney allocation system. Hum. Immunol. 78, 4–8 (2017).
Jackson, K. R. et al. How do highly sensitized patients get kidney transplants in the United States? Trends over the last decade. Am. J. Transplant. 20, 2101–2112 (2020).
Stewart, D. E. et al. Changes in deceased donor kidney transplantation one year after KAS implementation. Am. J. Transplant. 16, 1834–1847 (2016).
Audry, B. et al. The new French kidney allocation system for donations after brain death: Rationale, implementation, and evaluation. Am. J. Transplant. 22, 2855–2868 (2022).
Bryan, C. F. et al. Improving access to kidney transplantation without decreasing graft survival: Long-term outcomes of blood group A2/A2B deceased donor kidneys in B recipients. Transplantation 80, 75–80 (2005).
Hurst, F. P. et al. Transplantation of A2 kidneys into B and O recipients leads to reduction in waiting time: USRDS experience. Transplantation 89, 1396–1402 (2010).
Bryan, C. F., Cherikh, W. S. & Sesok-Pizzini, D. A. A2 /A2 B to B renal transplantation: Past, present, and future directions. Am. J. Transplant. 16, 11–20 (2016).
Garg, N. et al. Discrepant subtyping of blood type A2 living kidney donors: Missed opportunities in kidney transplantation. Clin. Transplant. 35, e14422 (2021).
Lentine, K. L. et al. OPTN/SRTR 2020 annual data report: Kidney. Am. J. Transplant. 22(Suppl 2), 21–136 (2022).
OPTN (Organ Procurement and Transplantation Network). OPTN Policies. Policy 8: Allocation of Kidneys. Accessed April 25, 2023.https://optn.transplant.hrsa.gov/media/eavh5bf3/optn_policies.pdf.
Martins, P. N. et al. Impact of the new kidney allocation system A2/A2B → B policy on access to transplantation among minority candidates. Am. J. Transplant. 18, 1947–1953 (2018).
Forbes, R. C., Feurer, I. D. & Shaffer, D. A2 incompatible kidney transplantation does not adversely affect graft or patient survival. Clin. Transplant. 30, 589–597 (2016).
Williams, W. W. et al. First report on the OPTN national variance: Allocation of A2 /A2 B deceased donor kidneys to blood group B increases minority transplantation. Am. J. Transplant. 15, 3134–3142 (2015).
Shaffer, D., Feurer, I. D., Rega, S. A. & Forbes, R. C. A2 to B kidney transplantation in the post-kidney allocation system era: A 3-year experience with anti-A titers, outcomes, and cost. J. Am. Coll. Surg. 228, 635–641 (2019).
Stewart, D. E. et al. Measuring and monitoring equity in access to deceased donor kidney transplantation. Am. J. Transplant. 18, 1924–1935 (2018).
Gragert, L. et al. ABO-adjusted calculated panel reactive antibody (cPRA): A unified metric for immunologic compatibility in kidney transplantation. Am. J. Transplant. 22, 3093–3100 (2022).
KONOS. Annual Report of the Transplant 2021 92–94 (Ministry of health and welfare (KR), 2022). Accessed April 25, 2023. https://www.konos.go.kr/board/boardListPage.do?page=sub4_2_1&boardId=30 (In kor).
KONOS. 8th Edition of Guidelines of Organ Transplantation Management. Ministry of health and welfare (KR). Accessed April 25, 2023. https://www.konos.go.kr/board/boardViewPage.do (In kor).
Jackson, K. R. et al. Outcomes of cPRA 100% deceased donor kidney transplant recipients under the new Kidney Allocation System: A single-center cohort study. Am. J. Transplant. 20, 2890–2898 (2020).
Acknowledgements
This study was supported by a grant from the National Institute of Organ, Tissue and Blood Management (20232400C1B-00), which was not involved in the design or analysis of the study.
Author information
Authors and Affiliations
Contributions
Research idea and study design: J.H.L., J.Y.; data acquisition: J.H.L., T.Y.K., J.E.L., K.H.O.; data analysis/interpretation: J.H.L., B.S.K., J.Y.; statistical analysis: J.H.L.; wrote the manuscript: J.H.L. and J.Y.; Each author contributed important intellectual content during manuscript drafting or revision and agrees to be pertaining to the accuracy or integrity of any portion of the work, even one in which the author was not directly involved, are appropriately investigated and resolved, including with documentation in the literature if appropriate.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, J.H., Koo, T.Y., Lee, J.E. et al. Impact of sensitization and ABO blood types on the opportunity of deceased-donor kidney transplantation with prolonged waiting time. Sci Rep 14, 2635 (2024). https://doi.org/10.1038/s41598-024-53157-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-53157-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.