Abstract
Hypertension is a public health problem. Failure to control blood pressure figures is responsible for morbidity and premature mortality. This study aims to describe the characteristics of hypertensive patients followed at primary health care centers in Marrakech. Between May 2021 and December 2022, a cross-sectional study of 922 hypertension patients attending primary health care centers in Marrakech was done. To gather socio-demographic, behavioral, and clinical data, as well as hypertension treatment features and the care-patient-physician triad, a face-to-face questionnaire was employed. To identify risk factors associated with uncontrolled blood pressure, multivariate logistic regression was used. Uncontrolled blood pressure was found in 73.5% of people. The patients' average age was 63.4 ± 9.4 years (mean ± standard deviation), and 524 (77.3%) were women. Tobacco consumption (Adjusted Odd Ratio of 4.34; 95% CI [1.58–11.9]); lack of self-monitoring of hypertension (AOR of 1.69; 95% CI [1.14–2.52]); a family history of hypertension (AOR of 1.58; 95% CI [1.12–2.22]); overweight or obesity (AOR of 1.73; 95% CI [1.15–2.58]); and nonadherence to antihypertensive medication (AOR of 1.58; 95% CI [1.05–2.38]) were identified as risk factors for uncontrolled blood pressure. In hypertensive individuals, the percentage of uncontrolled blood pressure is considerable. It is essential to provide therapeutic education classes for hypertension patients in order to strengthen their power and autonomy in managing their hypertension.
Similar content being viewed by others
Introduction
Noncommunicable diseases are responsible for 41 million deaths each year worldwide1. In Morocco, 80% of deaths from all causes are due to noncommunicable diseases, and 38% are related to cardiovascular diseases2. Hypertension, defined as systolic blood pressure (SBP) greater than or equal to 140 mmHg and/or diastolic blood pressure (DBP) greater than or equal to 90 mmHg, is the primary risk factor for cardiovascular disease3. According to the World Health Organization (WHO), in 2021, 1.28 billion adults between the ages of 30 and 79 suffered from hypertension4.
In Morocco, in 2018, the prevalence of hypertension was 29.6%2,5. We know that the lack of control of hypertension is responsible for cardiovascular complications such as strokes, chronic renal failure, disabilities, and early mortality. It affects the quality of life of hypertensive people. Each rise in SBP from 20 mmHg to more than 115 mmHg, or each rise in DBP from 10 mmHg to more than 75 mmHg, doubles the risk of developing cardiovascular events and major strokes6. The management of hypertension aims to ensure the control of blood pressure and the reduction of cardiovascular risks, morbidity, and mortality. Clinical trials have indicated that antihypertensive medications lower the risk of stroke by 35–40%, myocardial infarction by 15–25%, and heart failure by 64%7,8,9. In 2017, 73% of hypertensive people in Meknes, Morocco, had uncontrolled blood pressure (UBP)10. The lack of control over hypertension is an obstacle to achieving sustainable development goals in terms of health. The objective of our study was this study aims to describe the characteristics of hypertensive patients followed at primary health care centers in Marrakech and identify the associated risk factors of UBP.
Methods
Marrakech is a city located in the center of Morocco. It covers an area of approximately 230 km2 and has a population of 1,330,468 people11, including 23,213 hypertensives treated by the 79 primary health care centers in Marrakech12. A cross-sectional study was conducted between May 2021 and December 2022 among hypertensive patients followed at primary health care centers in Marrakech. We stratified by area of residence since statistics from the Marrakech prefecture's health delegation show that 70% of hypertension patients live in urban areas and 30% live in rural areas. An exhaustive list of primary health care centers was provided by the delegation of the Ministry of Health of Marrakech. Data collection was made by convenience sampling. A first draw was carried out to select 15 health centers among the 79 health care centers present in Marrakech. A second draw was made to determine the hypertensive patients aged 18 years or older who were present at primary health care centers on the day of the survey and agreed to participate in the study. To determine hypertensive patients in each selected center, hypertensive patients were assigned a queue number upon arrival, and these numbers were randomly drawn to select patients until the required sample size was reached.
Inclusion criteria
We included in the study participants who were previously known to be hypertensive due to a medical diagnosis, were on antihypertensive treatment for at least six months, were monitored at primary health care centers in Marrakech, and consented to participate in the study.
Exclusion criteria
We excluded pregnant women and patients with mental disorders from the study.
Data collection tool and procedure
Data collection was carried out through a questionnaire administered face-to-face after an interview with patients. This questionnaire contained sociodemographic and economic characteristics, behavioral characteristics, knowledge of hypertension, clinical characteristics, characteristics of antihypertensive treatment, and the relationship between the care system, patient, and physician.
Operational definitions
Uncontrolled blood pressure
Blood pressure was taken on both arms at the end of the interview using an electronic tensiometer (Microlife). Blood pressure was taken in a seated position, back leaning against the chair, feet flat on the floor, and arm at heart level. Two other measurements spaced two minutes apart were taken in the arm where the blood pressure was the highest. The blood pressure taken was the average of the last three measurements. The classification of blood pressure was made according to the recommendations of the European Society of Hypertension and the European Society of Cardiology (ESH/ESC)13. Hypertension was considered uncontrolled when SBP was greater than or equal to 140 mmHg and/or DBP was greater than or equal to 90 mmHg in the general population. In people with diabetes, we spoke of UBP when the SBP was greater than or equal to 140 mmHg and/or the DBP was greater than or equal to 85 mmHg. For people with renal insufficiency, we spoke of UBP when the SBP was greater than or equal to 130 mmHg and/or the DBP was greater than or equal to 90 mmHg13.
General knowledge about high blood pressure
General knowledge of high blood pressure has included symptoms (headaches, whistling, visual disturbances, dizziness, palpitations, difficulty breathing, epistaxis, hematuria), complications (heart attack, kidney damage, eye damage, and cerebrovascular accident), and preventive measures (hygiene-dietary, treatment adherence, self-measurement, and regular medical monitoring). General knowledge of high blood pressure was deemed satisfactory if the patient recognized at least half of the factors related to symptoms, complications, and prevention; otherwise, it was deemed unsatisfactory.
Drug non-adherence
Drug non-adherence was assessed using the Girerd test5,14. This test contains six questions to which the participant must answer "yes" or "no." “Yes” has a value of 1 point, and “no” has a value of 0 points. Adding the points for each question gives a score between 0 and 6. When the score is greater than or equal to one, we are talking about non-adherence to antihypertensive medication. Otherwise, we talk about good adherence. These questions are: did you forget to take your medication this morning? Since the last consultation, have you run out of medication? Have you ever taken your treatment later than usual? Have you ever not taken your medication because some days your memory fails you? Have you ever not taken your medication because some days you feel like your medication is doing more harm than good? Do you think you have too many tablets to take?.
Other variables
Anthropometric measurements included weight (in kilograms) and height (in meters). The body mass index (BMI) defined as the ratio between weight per kilogram and height per square meter, was classified into two categories: absence of overweight or obesity when the BMI was less than 25 kg per square meter and presence of overweight or obesity when the BMI was greater than or equal to 25 kg per square meter15,16.
-
A tobacco user was defined as anyone who has used tobacco in the last three months.
-
An alcohol user was defined as anyone who consumed alcohol in the past three months.
-
The presence of comorbidity was defined as anyone with diabetes, dyslipidemia, or renal failure.
-
The presence of a cardiovascular complication was defined as the presence of a self-reported history of myocardial infarction, stroke, stenting, angioplasty, or coronary artery bypass grafting.
Ethical consideration
The study complied with the Declaration of Helsinki. Informed consent from all participants was obtained after informing them about the aims of the research and respecting their privacy and confidentiality. The Ethics Committee of the Faculty of Medicine and Pharmacy of Rabat in Morocco read, reviewed, and approved the study protocol.
Statistical analysis
All the data was entered in Excel and analyzed on Epi-Info version 7. A descriptive analysis of the entire study population was carried out. Continuous variables were expressed as the mean and standard deviation, if appropriate. Categorical variables were expressed as numbers and percentages, where appropriate. Continuous variables were compared using the Analysis Variances test, if appropriate. Categorical variables were compared using the Pearson chi-square test when appropriate. During the bivariate analysis, all variables with a p-value up to 0.20 were included in the multiple logistic regression. The association between the risk factor and the presence of UBP was determined by the adjusted odds ratio (AOR) and its 95% confidence interval.
Results
Socio-demographic and economic characteristics
During the study period, a total of 922 participants were collected, with a percentage of UBP of 73.5%. The average age of the participants was 63.1 ± 9.8 years, with extremes ranging from 33 to 102 years. 727 (78.8%) were women, and 649 (70.4%) had a monthly income per household of less than $200 (Table 1).
Data on knowledge of hypertension and behavioral characteristics
Table 2 summarizes the data in relation to knowledge about hypertension and the behavioral characteristics of the participants. Thus, out of 922 participants, 905 (98.2%) had unsatisfactory general knowledge about hypertension, and 912 (98.9%) had unsatisfactory knowledge about its preventive measures. A total of 86 (09.3%) were tobacco users, and 739 (80.1%) did not self-monitor their blood pressure at home.
Clinical characteristics
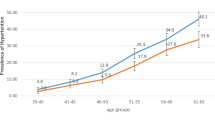
The data in Table 3 shows that 464 (50.3%) of participants had comorbidities, 418 (45.3%) had diabetes, 542 (58.8%) had a family history of hypertension, 742 (80.5%) were overweight or obese, 551 (59.8%) reported symptoms of depression, and 319 (34.6%) reported symptoms of anxiety. The mean systolic blood pressure (SBP) was 151.4 ± 18.1 mmHg, while the diastolic blood pressure was 81.9 ± 11.0 mmHg in the hypertensive patients. Isolated arterial hypertension was present in 455 (49.3%) of the cases (Fig. 1).
Characteristics related to treatment and the patient-physician-Healthcare system triad
A total of 776 (84.2%) participants reported an unsatisfactory relationship with the healthcare system, 778 (84.4%) had an unsatisfactory relationship with their physician, and 760 (82.4%) had drug nonadherence (Table 4).
Uncontrolled blood pressure
A total of 678 participants had UBP, which means a percentage of 73.5%. Their average age was 63.4 ± 9.4 years, 524 (77.3%) were women, and 487 (71.8%) had a monthly income per household of less than 200 dollars (Table 1). 78 (11.5%) participants used tobacco, and 559 (82.5%) declared not self-monitoring their blood pressure at home (Table 2). 560 (82.6%) were overweight or obese, and 411 (60.6%) had a family history of hypertension (Table 3). The mean systolic blood pressure (SBP) was 158.4 ± 15.6 mmHg, while the diastolic blood pressure was 84.9 ± 10.7 mmHg. The unsatisfactory relationship with the healthcare system was observed in 583 (86.0%) participants, and non-adherence to antihypertensive drugs in 576 (85.0%) (Table 4).
As mentioned in Table 5, after bivariate analysis, the following variables were associated with the presence of poor hypertension control: 1. female sex; 2. age; 3. low monthly income per household; 4. unsatisfactory knowledge about hypertension; 5. unsatisfactory knowledge about preventive measures against hypertension; 6. tobacco consumption; 7. alcohol consumption; 8. low- to moderate-intensity physical activity; 9. non-consumption of five fruits and vegetables per day; 10. lack of self-monitoring; 11. lack of family support; 12. presence of comorbidity; 13. presence of diabetes; 14. duration of hypertension of more than three years; 15. presence of a family history of hypertension; 16. presence of self-reported symptoms of depression; 17. presence of self-reported anxiety symptoms; 18. presence of overweight or obesity; 19. unsatisfactory relationship between patient and healthcare system; 20. unsatisfactory patient-physician relationship; and 21. non-adherence to antihypertensive medication.
Multivariate analysis
After controlling for the other variables, we identified the following factors as associated with poor hypertension control: 1. tobacco consumption (Adjusted Odd Ratio of 4.34; 95% CI [1.58–11.9]); 2. lack of self-monitoring (AOR of 1.69; 95% CI [1.14–2.52]); 3. presence of a family history of hypertension (AOR of 1.58; 95% CI [1.12–2.22]); 4. presence of overweight or obesity (AOR of 1.73; 95% CI [1.15–2.58]); and 5. non-adherence to antihypertensive drugs (AOR of 1.58; 95% CI [1.05–2.38]) (Table 5).
Discussion
Our study estimated the percentage of UBP at 73.5% among hypertensives followed at primary health care centers in Marrakech. This result is similar to the 73.0% observed in Meknes in 2017 in 922 hypertensive patients10. In developing countries, the percentage of poor hypertension control varies between 69 and 77%17,18. Indeed, in 12 sub-Saharan countries, among 2198 hypertensive patients, the percentage of poor hypertension control was 77.4%17. In Turkey, in 2017, out of 556 hypertensive patients, the percentage of poor hypertension control was 69.8%18. In Ghana, in 2018, out of 2870 hypertensive patients, the percentage of poor hypertension control was 57.7%19. In developed countries, this percentage is between 50 and 61%. Thus, in the United Kingdom, out of 100,000 hypertensive patients, 61.9% had UBP20, and in the United States, between 2011 and 2014, in 9623 hypertensives, the percentage of UBP was 53.4%21.
In our study, tobacco consumption was associated with UBP. Several studies have reported tobacco as a risk factor associated with the UBP22,23,24. Tobacco includes nicotine, which causes vasoconstriction of blood vessels25. It also activates the sympathetic nervous system, producing an increase in heart rate and blood pressure26. People who smoke can have damaged blood vessels, causing the formation of plaques in the arteries27. This narrowing creates a significant resistance to blood flow, thus causing an increase in blood pressure.
Self-monitoring of blood pressure with accurate electronic blood pressure monitors is becoming increasingly important in the treatment of hypertension28. It allows better control of blood pressure and a reduction in cardiovascular complications29. It also reduces the white coat effect and ensures the availability of blood pressure data in different places and at different times. Blood pressure self-monitoring is a form of self-management that involves and empowers individuals in the treatment of their condition. It represents a source of motivation for therapeutic adherence and a way of evaluating the effectiveness of antihypertensive treatment. In our study, the absence of self-monitoring was associated with UBP.
As in our survey, several other studies have demonstrated that there is an important relationship between the presence of a family history of hypertension and UBP10. His relationship can be explained by genetics and heritability30, adoption of an unhealthy lifestyle, smoking and physical inactivity31.
In our study, overweight and obesity were associated with UBP. The literature reports an increase in the activity of the sympathetic nervous system in obese subjects32. This activity causes arterial vasoconstriction and decreased renal perfusion. As a result, the renin-angiotensin system is activated, which also produces sodium and water retention, thus promoting an increase in blood pressure33. In 2003, a meta-analysis of 4874 hypertensive patients showed that reducing body weight leads to a decrease in blood pressure. For every kilogram of weight lost, systolic and diastolic blood pressure decrease by approximately 1 mmHg34.
In our study, non-adherence to antihypertensive drugs was associated with UBP. This same result was observed in other studies5,10,35. This could be explained by a lack of knowledge about the adverse effects of antihypertensive drugs, repeated stock-outs of antihypertensive drugs at primary health care centers, high cost, low monthly household income, and a lack of social support.
Limits of the study
Our study has certain limitations, such as the social desirability bias seen while gathering data on alcohol and tobacco intake, as well as the willful lying bias experienced when gathering data on monthly income.
Conclusion
The percentage of people with hypertension who have UBP is significant. Smoking, being overweight or obese, having a family history of hypertension, a lack of self-monitoring of blood pressure, and nonadherence to antihypertensive medication were all risk factors for UBP. Therapeutic education and patient empowerment in disease management are important.
Data availability
All data generated or analyzed during this study are included in this published article.
References
Principaux repères sur les maladies non transmissibles. https://www.who.int/fr/news-room/fact-sheets/detail/noncommunicable-diseases.
Ministère de la santé Maroc. Enquête nationale sur les facteurs de risque des maladies non transmissibles, 2019. https://www.sante.gov.ma/Publications/Etudes_enquete/Pages/default.aspx.
Haute Autorité de Santé—Hypertension artérielle—Des outils pour une prise en charge optimale. https://www.has-sante.fr/jcms/pprd_2974311/en/hypertension-arterielle-des-outils-pour-une-prise-en-charge-optimale.
Hypertension. https://www.who.int/fr/news-room/fact-sheets/detail/hypertension.
Essayagh, T., Essayagh, M. & Essayagh, S. Drug non-adherence in hypertensive patients in Morocco, and its associated risk factors. Eur. J. Cardiovasc. Nurs. 20, 1 (2021).
Weber, M. A. et al. Clinical practice guidelines for the management of hypertension in the community. J. Clin. Hypertension 16, (2014).
Psaty, B. M. et al. Health outcomes associated with antihypertensive therapies used as first-line agents: A systematic review and meta-analysis. JAMA 277. https://doi.org/10.1001/jama.277.9.739 (1997).
Neal, B. et al. Effects of ACE inhibitors, calcium antagonists, and other blood-pressure-lowering drugs: Results of prospectively designed overviews of randomised trials. Lancet 356, (2000).
Bibbins-Domingo, K. et al. Reductions in cardiovascular disease projected from modest reductions in dietary salt. NEJM 362, 590–599 (2010).
Essayagh, T. et al. Prevalence of uncontrolled blood pressure in Meknes, Morocco, and its associated risk factors in 2017. PLoS ONE 14, e0220710 (2019).
Haut-Commissariat-au Plan. Monographie générale de la région de Marrakech-Safi | Portail national des collectivités territoriales. (2020).
Ministère de la Santé, M. Santé en chiffres. https://www.sante.gov.ma/Documents/2023/03/Sante%20en%20chiffre%202021%20VF%20(1).pdf (2021).
Mancia, G. et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J. Hypertens. 31, 1281–1357 (2013).
Girerd, X., Hanon, O., Pannier, B., Mourad, J. J. & Vaïsse, B. Déterminants de l’hypertension artérielle contrôlée chez les sujets traités par antihypertenseurs en France: Enquête FLAHS 2015. Ann. Cardiol. Angeiol. (Paris) 65, 219–222 (2016).
Principaux repères sur l’obésité et le surpoids. https://www.who.int/fr/news-room/fact-sheets/detail/obesity-and-overweight.
Essayagh, F. et al. Disease burden among migrants in Morocco in 2021: A cross-sectional study. PLoS One 18, e0281129 (2023).
Macquart de Terline, D. et al. Poor adherence to medication and salt restriction as a barrier to reaching blood pressure control in patients with hypertension: Cross-sectional study from 12 sub-Saharan countries. Arch. Cardiovasc. Dis. 113, 1 (2020).
Selçuk, K. T., Mercan, Y. & Aydın, T. Uncontrolled blood pressure in patients with hypertension and associated factors: The role of low health literacy. Erciyes Med. J. 40 (2018).
Sarfo, F. S. et al. Factors associated with uncontrolled blood pressure among Ghanaians: Evidence from a multicenter hospital-based study. PLoS One 13, e0193494 (2018).
Tapela, N. et al. Prevalence and determinants of hypertension control among almost 100,000 treated adults in the UK. Open Heart 8, e001461 (2021).
Muntner, P. et al. Potential US population impact of the 2017 ACC/AHA high blood pressure guideline. Circulation 137, 109–118 (2018).
Selçuk, K. T., Mercan, Y. & Aydın, T. Uncontrolled blood pressure in patients with hypertension and associated factors: The role of low health literacy. J. Clin. Pract. Res. 40, 222–227 (2018).
Mitra, M. & Wulandari, W. Factors affecting uncontrolled blood pressure among elderly hypertensive patients in Pekanbaru City, Indonesia. Open Access Maced. J. Med. Sci. 7, 1209–1213 (2019).
Wang, Y. et al. A12426 Association between smoking and blood pressure in elderly male patients with essential hypertension. J. Hypertens. 36, e321 (2018).
Hwang, K., Son, J. S. & Ryu, W. K. Smoking and flap survival. Plast. Surg. (Oakv) 26, 280–285 (2018).
Kaur, A., Kumar, A. & Singh, D. Effect of cigarette smoking on heart rate variability in health adult smokers in the age of 20–60 years. IOSR J. Dent. Med. Sci. (IOSR-JDMS) e-ISSN 16, 69–73 (2017).
Krishnamurthi, R. V. et al. Stroke incidence by major pathological type and ischemic subtypes in the Auckland regional community stroke studies: Changes between 2002 and 2011. Stroke 49, 3–10 (2018).
Citoni, B., Figliuzzi, I., Presta, V., Volpe, M. & Tocci, G. Home blood pressure and telemedicine: A modern approach for managing hypertension during and after COVID-19 pandemic. High Blood Pressure Cardiovasc. Prev. 29, 1 (2022).
Williams, B. et al. 2018 ESC/ESH Guidelines for the management of arterial hypertensionThe Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur. Heart J. 39, 3021–3104 (2018).
Kolifarhood, G. et al. Familial genetic and environmental risk profile and high blood pressure event: A prospective cohort of cardio-metabolic and genetic study. Blood Press 30, 196–204 (2021).
Steeger, C. M. et al. Time-varying effects of family smoking and family management on adolescent daily smoking: The moderating roles of behavioral disinhibition and anxiety. Drug Alcohol Depend 204, 107572 (2019).
Grassi, G. Leptin, sympathetic nervous system, and baroreflex function. Curr. Hypertens. Rep. 6, 236–240 (2004).
Burnier, M. & Taddei, S. Traitement de l’hypertension chez les patients obèses: Quelle approche thérapeutique choisir ?. Rev. Med. Suisse 2495, 1723–1732 (2004).
Neter, J. E., Stam, B. E., Kok, F. J., Grobbee, D. E. & Geleijnse, J. M. Influence of weight reduction on blood pressure: A meta-analysis of randomized controlled trials. Hypertension 42, 878–884 (2003).
Asgedom, S. W., Gudina, E. K. & Desse, T. A. Assessment of Blood Pressure Control among Hypertensive Patients in Southwest Ethiopia. PLoS One 11, 1 (2016).
Author information
Authors and Affiliations
Contributions
S.B., F.Z.B., F.E., O.T., M.E., T.E., and S.E.: conceptualization, methodology, investigation, analysis, project administration, validation, and writing original draft. I.M., A.L., A.Z.: writing original draft.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Belayachi, S., Boukhari, F.Z., Essayagh, F. et al. Uncontrolled blood pressure and its risk factors among hypertensive patients, Marrakech, Morocco. Sci Rep 14, 2953 (2024). https://doi.org/10.1038/s41598-024-53115-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-53115-y
This article is cited by
-
Determinants associated with low dietary diversity among migrants to Morocco: a cross sectional study
Scientific Reports (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.