Abstract
Although increase in physical activity is important to improve prognosis of cardiac patients in addition to hospital-based exercise cardiac rehabilitation, their physical activity levels are not properly understood. This study aimed to examine domain- and intensity-specific physical activity in individuals with coronary heart disease (CHD) and compare them with non-CHD individuals. Data from the Korean National Health and Nutrition Examination Survey (KNHANES) from 2014 to 2019 were analyzed, including 1083 CHD patients and 38,532 non-CHD individuals. The inclusion criteria were age 19 years or older and data not missing for CHD information. Before and after propensity score matching (PSM) for age, sex, body mass index, education, household income, alcohol intake, and smoking status, domain (leisure, work, transportation)—and intensity (moderate, vigorous) -specific physical activity participation levels were compared between individuals with and without CHD. Before PSM, CHD individuals were older, less educated, more sedentary, and participated less in PAs compared to non-CHD individuals. After PSM, CHD individuals had similar levels of domain-specific PAs. However, they had higher work-related PA levels (29.7 ± 209.6 vs. 42.1 ± 291.3 min/week p = 0.022) and more sedentary time (487.2 ± 224.2 vs. 514.1 ± 228.7. p = 0.003) than those without CHD. Subgroup analysis revealed lower leisure-related PA in men with CHD (63.5 ± 165.5 vs. 47.3 ± 140.2, p < 0.05) and higher work-related PA in women with CHD (18.9 ± 159.7 vs. 57.1 ± 397.5, p < 0.01). Among those < 65 years of age, individuals with CHD spent more time sedentary than individuals without CHD. CHD individuals are not physically inactive compared with non-CHD individuals who are similar in sociodemographic status and lifestyle. CHD patients’ PA levels may have been underestimated.
Similar content being viewed by others
Introduction
Coronary heart diseases (CHD) are a leading cause of global mortality and a significant contributor to disability1. In the Republic of Korea, the number of people hospitalized for heart disease in 2018 increased four-fold from 2002 and was the second leading cause of death in 20192. The most prevalent heart disease is CHD which includes angina and myocardial infarction (MI). Preventing recurrent CHD is important considering the increasing number of risk factors given the aging population in Korea2.
Exercise-based cardiac rehabilitation (CR) is a class 1 recommendation for preventing recurrent CHD events3. Exercise improves physical health and reduces the risk of MI, all-cause hospitalization, all-cause mortality, and cardiovascular mortality in individuals with CHD4. In developing effective physical activity program for patients with CHD, it is important to understand physical activity participation levels. While studies have reported physical activity behaviors of individuals with various CVDs, they were either baseline physical activity levels from intervention studies or prospective cohort studies. It is challenging to compare the physical activity levels of individuals with CHD to individuals without CHD. In addition, studies have suggested different domains of physical activity may have unique health effects7. Leisure activities (e.g., sports and exercise) are performed at the discretion of an individual and are not essential for daily living. Work activities (e.g., construction, manufacturing) include all activities within occupational settings, and transportation activities (e.g., walking, cycling) include activities done as a mode of transportation. There is limited research on domain-specific physical activity among individuals with CHD8,9,10. Any potential differences between individuals (with and without CHD) matched on sociodemographic and lifestyle factors are unknown. The CR team should consider any unique physical activity patterns or characteristics of individuals with CHD when planning and implementing CR programming.
In South Korea, the Korean National Health and Nutrition Examination Survey (KNHNES) is an annually conducted nationwide survey (including domain-specific physical activity). This survey aims to recruit a representative population-based sample and includes individuals with CHD and other chronic diseases. The objective of our study was to determine domain-specific physical activity behaviors, intensities, and sedentary time among individuals with CHD. The secondary objective of our study was to explore differences in these activity-related variables by comparing individuals with CHD to a sample of individuals without CHD matched for socioeconomic status and lifestyle factors. We hypothesized that individuals with CHD would report doing less physical activity in all domains than individuals without CHD.
Methods
Participants and data source
We used the 2014–2019 KNHANES data. The KNHANES is conducted annually by the Korea Centers for Disease Control and Prevention (KCDC). This nationwide cross-sectional survey recruits approximately 10,000 non-institutionalized civilians each year through a stratified multistage probability sampling method. KNHANES data allows for monitoring of public health and health trends and policy planning and development. KNHANES includes health interviews, health examinations, and nutrition surveys. The KNHANES data resource profiles11 provides further details on the KNHANES study procedures.
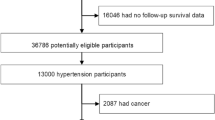
From the 2014–2019 KNHANES data, we included all participants over 18 years old (N = 55,419). We excluded participants with missing values for CHD-related questions and physical activity (N = 15,804). After the exclusion, we identified 38,532 individuals without CHD and 1083 individuals with CHD (Fig. 1). Individuals without CHD were those who reported that they had never been diagnosed with any CHD. Individuals with CHD were those who reported that they had been previously diagnosed with angina or MI. Individuals with both angina and MI were categorized in the MI group, as MI is a more severe condition that can occur if angina worsens. Individuals were asked if they had a) a history of being diagnosed by a doctor, b) currently suffering from the disease, or c) currently receiving treatment for the disease. We counted those who answered yes to at least one of the items as individuals with angina or MI.
Measures
In KNHANES, demographic, socioeconomic, and physical activity information were collected via self-reported questionnaires and face-to-face interviews using standardized questionnaires. Data were collected in a mobile inspection vehicle. All participants provided written informed consent. Angina and MI were the only types of CHD included in the KNHANES data.
Sociodemographic and descriptive variables included age, sex, body mass index (BMI) (kg/m2), educational attainment, marital status, employment status, household income, smoking status, alcohol intake, and age at CHD diagnosis. BMI was taken from the measured weight and height to the nearest 0.1 kg and 0.1 cm and was calculated as the ratio of weight in kilograms to height in squared meters. Household income was calculated by dividing the monthly household income by the square root of the household size and grouped into quartiles (i.e., low, moderate-low, moderate-high, and high), education attainment (i.e., ≤ elementary, middle school, high school, ≥ college), smoking status (i.e., current smoker, past smoker, never smoker), and alcohol intake (i.e., < 1/month, 2–4/month, ≥ 2/week). We calculated the time from CHD diagnosis by subtracting the age at the first CHD diagnosis from the age at the time of completing the survey.
Physical activity was measured using the Global Physical Activity Questionnaire (GPAQ)12. The GPAQ captures physical activity domain (i.e., work, leisure, transport) and intensity (i.e., vigorous, moderate), frequency, and duration. Vigorous intensity activity was defined as any activity that required a considerable amount of physical effort and caused heavy breathing and a high heart rate. Moderate intensity activity was defined as any activity that required less physical effort and slightly increased breathing and heart rate. Work and leisure physical activity included information on intensity, but not physical activity for transport. Total physical activity was calculated by summing the time/duration spent in each activity domain. The validity and reliability of the GPAQ in Korean population have been previously described13.
Statistical analysis
“SPSS version 25 (IBM Corp., Armonk, NY, USA) was used for all analyses. For propensity score matching (PSM), we used SAS 15.1 (SAS Institute Inc., Cary, North Carolina, USA). Propensity score, which indicates the probability that an individual being assigned to a particular condition (CHD in the current study), was calculated using logistic regression based on predefined factors including age, sex, BMI, education, household income, smoking status, and alcohol intake that are recognized as major risk factors for both physical activity and CHD. Using these calculated propensity scores, individuals with CHD (cases) and without CHD (controls) were matched in a 1:5 ratio using the 1:N case-control matching macro with greedy algorithms provided the SAS group14. The number of matches per subject was selected as 1:5 to increase the precision of estimates and statistical power.”
For descriptive analysis, continuous variables including physical activity were expressed as means (standard deviation), and categorical variables were presented as percentages. To test the normality of the data, the Kolmogorov–Smirnov test was used. To compared the differences between individuals with and without CHD, Chi-squared and t-tests were used for normally distributed variables. When the data were not normally distributed, Kruskal Wallis and the Mann–Whitney U tests were used to compare variables between the groups. Statistical significance was set at p < 0.05.
Ethics approval
The Institutional Review Board of the Korea Centers for Disease Control and Prevention approved KNHANES study protocols (2013-12EXP-03-5C, 2018–01-03-P-A, 2018–01-03-C-A). All parts of the study were carried out in agreement with the Declaration of Helsinki.
Results
We identified 38,532 non-CHD individuals and 1083 CHD patients in the KNHANES data from 2014 to 2019. Before matching, the mean age of individuals without CHD was 51 ± 16.8 years and 68.9 ± 8.9 years for individuals with CHD. BMI among individuals without CHD was 23.9 ± 3.6 and 24.8 ± 3.2 kg/m2 for individuals with CHD. After matching, the mean age for both samples was 69 years and the mean BMI was 24.7 kg/m2. Table 1 shows significant differences across all variables when comparing individuals with and without CHD before PSM. After PSM, a total of 5415 non-CHD individuals were matched and differences for only employment status (p < 0.05) and smoking status (p < 0.05) remained. Among individuals with CHD, 61.5% (n = 666) reported angina and 38.5% (n = 417) reported MI. There were no missing data for variables in Table 1.
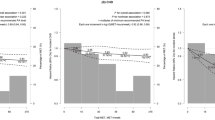
Table 2 shows physical activity intensity and minutes per week for different domains between individuals with and without CHD. Before PSM, individuals with CHD reported significantly fewer minutes of vigorous physical activity, leisure physical activity, physical activity for transport, and total physical activity compared to individuals without CHD. Individuals with CHD reported significantly more sedentary time than those without CHD. After PSM, we found no significant differences in leisure time and transport-related physical activity between groups. Individuals with CHD spent significantly more time in work-related physical activity and significantly more time sedentary compared to those without CHD.
Table 3 shows subgroup analyses of domain-specific physical activity according to sex (men vs. women) and age (< 65 years vs. ≥ 65 years). Leisure-time physical activity was significantly lower in men with CHD, and work-related physical activity was higher in women with CHD. Both men and women with CHD reported significantly more sedentary time then those without CHD. Among those < 65 years of age, individuals with CHD spent significantly more time sedentary than individuals without CHD.
There were no significant associations between any physical activity variables (i.e., intensity and domain) and time since angina or MI diagnosis (see Supplementary Table s1). Individuals who reported work-related physical activity had significantly fewer sedentary time min/day and higher vigorous, moderate, leisure, and total physical activity than those who did not report work-related physical activity (see Supplementary Table s2). Physical activity guideline (more than 150 min per week of moderate intensity physical activity) satisfaction rates of participants with and without CHD were 11.3%, 6.4% and 15.7%, 5.4%, for male and female respectively (see Supplementary Table s3).
Discussion
We hypothesized individuals with CHD would be less physically active than the general population who do not have CHD. Before PSM, we observed a significantly lower amount of time spent in vigorous, leisure, transport, and total physical activity participation and significantly more sedentary time among individuals with CHD than those without CHD. Considering the differences in sociodemographic and lifestyle variables between the two groups, we used PSM to compare the groups. After matching, individuals with CHD had equivalent physical activity levels to individuals without CHD other than work-related physical activity. Leisure physical activity time was significantly lower in men with CHD, while women reported higher work-related physical activity. Among those < 65 years of age, individuals with CHD spent significantly more time sedentary than those without CHD.
We observed similar physical activity levels in individuals with and without CHD when matched for sociodemographic and lifestyle variables. One study in the United States reported the age-standardized percentage of adults with and without CHD who participated in physical activity at recommended levels. Their data suggested individuals with CHD participated in significantly less total (40% meeting recommendations vs. 49% meeting recommendations), moderate (32% vs. 37%), and vigorous (22% vs. 29%) physical activity compared with individuals without CHD15. Another study reported physical activity participation rates of coronary patients from European countries (moderate or vigorous physical activity for at least 20 min once or more times a week: 38%) but not in comparison to those without CHD16. Furthermore, discrepancies exist between the findings of the current study and those of Baker et al.17, which reported a significant reduction in objectively measured physical activity compared to the health control group. One of the primary distinctions between our study and Baker et al.'s study is the average age of participants. Notably, participants in Baker et al. (2019) are significantly older (no disease: male 61.0 ± 8.0 and female 60.7 ± 7.7 years old; chronic disease: male 65.5 ± 7.1, female 63.5 ± 7.5). Considering that vigorous physical activity tends to decrease with age, the observed lower physical activity participation in individuals with CVD compared to those without CVD could be partially attributed to the higher age among individuals with CVD. In our study, we employed propensity score matching. Consequently, we were able to compare physical activity participation levels between participants who were matched for age, BMI, education, household income, alcohol intake, and smoking status. This approach enhances the robustness of our comparisons, minimizing potential confounding effects and providing a more accurate assessment of the impact of chronic disease on physical activity participation.
When interpreting our data, one should note that physical activity levels are generally low among Korean adults in comparison to other countries. A recent study on physical activity prevalence among Korean adults between the ages of 60 and 69 years reported that 10.2% were engaging in high levels of physical activity18, which is lower than older Czech adults (24.9–28.3%)19 and Iranians between the ages of 55 and 64 years (23.7%)20. In addition, some people with CHD may have recognized the importance of PA and tried to be more physically active. Stewart and colleagues reported that 34% of individuals with CHD increased their physical activity after their CHD diagnosis21 and similar results have been reported in European samples16. The extent to which people are motivated to increase the amount of activity after diagnosis and the effect over time is unclear and may vary by country and/or ethnicity.
Physical activity domains (i.e., leisure, work, and transportation) may have varying associations with CHD. Leisure activity has an inverse linear association with CVD risk factors and mortality22,23. Associations of other physical activity domains with cardiovascular health remain less clear. Regarding work-related physical activity, research has suggested shift work may increase the risk of CVD events, and work-related physical activity may increase all-cause mortality in men24,25. As for transportation-related physical activity, adults living in walkable neighborhoods had lower 10-year CVD risk compared to those who do not live in walkable neighborhoods26. Referred to as the physical activity paradox, it is unclear why occupational or work-related physical activity does not confer similar health benefits as leisure or recreational physical activities7. It is noteworthy that there was no discernible difference in work-related physical activity before PSM; however, individuals with CHD exhibited higher levels of work-related physical activity. This observation may be attributed to significant disparities in age (51 ± 16.8 vs. 68.9 ± 8.9 years old), sex, BMI (23.9 ± 3.6 vs. 24.8 ± 3.2, kg/m2), marital status, and employment status before matching. Prior to PSM, individuals without CHD were notably younger, more likely to be single, leaner, and employed. Consequently, the comparison of work-related physical activity after PSM matching enhances the validity of the analysis by accounting for these baseline differences and ensuring a more balanced and unbiased assessment between the groups.
In our subgroup analyses, we observed a lower engagement in leisure physical activity among men with CHD, while women with CHD demonstrated higher levels of work-related physical activity. It is noteworthy that there was no significant difference in work-related physical activity before matching, but a notable disparity emerged after matching. Upon closer examination through subgroup analyses, we found that this divergence in work-related physical activity was specific to women. The reason for the heightened work-related physical activity in women with CHD remains unclear, especially considering a smaller proportion of participants with CHD were employed. It is essential to recognize that the GPAQ not only assesses occupational physical activity but also encompasses physical activity related to unpaid work, household chores, and harvesting food/crops. Additionally, it is pertinent to highlight that the types of employment were comparable between individuals with and without CHD. Therefore, the observed differences in work-related physical activity in our study may be attributed, at least in part, to variances in socioeconomic status. It is crucial to further investigate and understand the factors contributing to the observed patterns in physical activity among women with CHD in various domains. Among men and women who were < 65 years of age and had CHD, significantly more time was spent sedentary than those without CHD.
It is noteworthy that individuals with CHD showed significantly higher sedentary time in our study, in agreement with findings from previous studies27,28. Since replacing sedentary time with physical activity may reduce inflammation29, CVD mortality, and all-cause mortality30, individuals with CHD should be encouraged to limit the amount of time spent in sedentary pursuits. Replacing sedentary time with leisure physical activity should be strongly recommended. Sociodemographic characteristics of individuals with CHD who report high work-related physical activity levels should be further analyzed. Whether individuals with CHD who report high work-related physical activity levels need additional leisure activity should be a question for future research in this area.
Shorter sedentary time and higher levels of leisure physical activity are associated with beneficial effects on CVD22,30. Higher and prolonged sedentary time has adverse effects on CVD markers, such as blood pressure, high-density lipoprotein, low-density lipoprotein, and C-reactive protein31. Similar to previous research, individuals with CHD were spending significantly more time sedentary compared to those without CHD. Since all activities performed in a single day are interdependent, longer sedentary time could mean less time spent in physical activity. Recent studies point to the need to incorporate more sophisticated measures such as posture-discriminating accelerometry and distinguish between sedentary patterns. Future studies should also apply isotemporal substitution modeling approaches to determine the impact (on health outcomes) of reducing sedentary time and increasing time spent in other physical activity domains.
One limitation of our study is that the diagnosis of CHD was based on a subjective questionnaire. This method may lead to instances where cases of angina, unrelated to CHD, are included, and some patients may not have experienced a MI. Another limitation stems from the broad definition of CHD, encompassing a spectrum of severity, ranging from well-controlled angina with minimal symptoms to those experiencing worsening conditions. Moreover, our study's measurement of physical activity relied on subjective, self-reported data. Individuals with CHD in our study might have provided socially desirable responses to the physical activity questionnaires, potentially leading to an overreporting of their physical activity levels. Although objective/device-based methods, such as accelerometers, cannot distinguish between different domains of physical activity, our findings remain credible. For future research, a more comprehensive approach would involve simultaneously implementing both objective and self-report methods for assessing physical activity. This would provide a more nuanced and accurate understanding of individuals' activity levels and contribute to a more robust interpretation of the relationship between CHD and physical activity. Moreover, although we adjusted for major demographic and lifestyle related factors, we cannot rule out unmeasured confounding by other diseases and factors that may influence physical activity level and CHD. Despite these limitations, our study stands as the first to compare physical activity levels between individuals with and without CHD after meticulous matching on sociodemographic and lifestyle variables on a national scale.
Conclusions
In conclusion, individuals with CHD) exhibit comparable levels of physical activity to their non-CHD counterparts with similar sociodemographic status and lifestyle, although in our study, both CHD and non-CHD are not very physically active. Interestingly, a notable difference emerges as CHD individuals demonstrate higher levels of work-related physical activity and spend more time in sedentary pursuits compared to those without CHD. It is established that reducing sedentary time and engaging in more leisure physical activity yield positive effects on recurrent CVD. Therefore, it is advisable to recommend the substitution of sedentary time with leisure physical activity for individuals with CHD, promoting cardiovascular health and overall well-being.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CHD:
-
Coronary heart disease
- KNHANES:
-
Korean National Health and Nutrition Examination Survey
- PSM:
-
Propensity score matching
- CR:
-
Cardiac rehabilitation
- MI:
-
Myocardial infarction
- BMI:
-
Body mass index
- GPAQ:
-
Global physical activity questionnaire
- CVD:
-
Cardiovascular disease
References
Roth, G. A. et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: Update from the GBD 2019 study. J. Am. Coll. Cardiol. 76(25), 2982–3021 (2020).
Lee, H. H. et al. Korea heart disease fact sheet 2020: Analysis of nationwide data. Korean Circ. J. 51(6), 495–503 (2021).
Taylor, R. S., Dalal, H. M. & McDonagh, S. T. J. The role of cardiac rehabilitation in improving cardiovascular outcomes. Nat. Rev. Cardiol. 19(3), 180–194 (2022).
Dibben, G. et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 11, CD001800 (2021).
Kim, S. H., Ro, J. S., Kim, Y., Leigh, J. H. & Kim, W. S. Underutilization of hospital-based cardiac rehabilitation after acute myocardial infarction in Korea. J. Korean Med. Sci. 35(30), e262 (2020).
Imran, H. M. et al. Home-based cardiac rehabilitation alone and hybrid with center-based cardiac rehabilitation in heart failure: A systematic review and meta-analysis. J Am Heart Assoc. 8(16), e012779 (2019).
Holtermann, A., Krause, N., van der Beek, A. J. & Straker, L. The physical activity paradox: Six reasons why occupational physical activity (OPA) does not confer the cardiovascular health benefits that leisure time physical activity does. Br. J. Sports Med. 52(3), 149–150 (2018).
De Smedt, D. et al. Physical activity status in patients with coronary heart disease: Results from the cross-sectional EUROASPIRE surveys. J. Phys. Act. Health. 13(12), 1378–1384 (2016).
Kambic, T., Sarabon, N., Hadzic, V. & Lainscak, M. Objectively measured physical activity in patients with coronary artery disease: A cross-validation study. Biosensors Basel. 11(9), 318 (2021).
Rastogi, T. et al. Physical activity and risk of coronary heart disease in India. Int. J. Epidemiol. 33(4), 759–767 (2004).
Kweon, S. et al. Data resource profile: The Korea national health and nutrition examination survey (KNHANES). Int. J. Epidemiol. 43(1), 69–77 (2014).
Timothy Armstrong, F. B. Development of the world health organization global physical activity questionnaire (GPAQ). J. Public Health. 14, 66–70 (2006).
Lee, J. et al. Development of the Korean global physical activity questionnaire: reliability and validity study. Glob. Health Promot. 27(3), 44–55 (2020).
LS, P., editor Reducing bias in a propensity score matched-pair sample using greedy matching techniques. In Proceedings of the twenty-sixth annual SAS Users group international conference; 2001: SAS Institute Inc.
Zhao, G., Ford, E. S., Li, C. & Mokdad, A. H. Are United States adults with coronary heart disease meeting physical activity recommendations?. Am. J. Cardiol. 101(5), 557–561 (2008).
Kotseva, K. et al. EUROASPIRE IV: A European society of cardiology survey on the lifestyle, risk factor and therapeutic management of coronary patients from 24 European countries. Eur. J. Prev. Cardiol. 23(6), 636–648 (2016).
Barker, J. et al. Physical activity of UK adults with chronic disease: Cross-sectional analysis of accelerometer-measured physical activity in 96 706 UK Biobank participants. Int. J. Epidemiol. 48(4), 1167–1174 (2019).
Min, K. et al. Physical activity patterns and their associated factors measured by global physical activity questionnaire survey among Korean. Korean J. Sports Med. 38(1), 1–11 (2020).
Hamrik, Z., Sigmundova, D., Kalman, M., Pavelka, J. & Sigmund, E. Physical activity and sedentary behaviour in Czech adults: Results from the GPAQ study. Eur. J. Sport Sci. 14(2), 193–198 (2014).
Sahebkar, M. et al. Prevalence and correlates of low physical activity in the Iranian population: National survey on non-communicable diseases in 2011. Scand. J. Med. Sci. Sports. 28(8), 1916–1924 (2018).
Stewart, R. et al. Physical activity in patients with stable coronary heart disease: An international perspective. Eur. Heart J. 34(42), 3286–3293 (2013).
Cheng, W. et al. Associations of leisure-time physical activity with cardiovascular mortality: A systematic review and meta-analysis of 44 prospective cohort studies. Eur. J. Prev. Cardiol. 25(17), 1864–1872 (2018).
Lee, E. B. et al. Association between domain-specific physical activity and diabetes in Korean adults. Sci. Rep. 11(1), 13066 (2021).
Coenen, P. et al. Do highly physically active workers die early? A systematic review with meta-analysis of data from 193 696 participants. Br. J. Sports Med. 52(20), 1320–1326 (2018).
Torquati, L., Mielke, G. I., Brown, W. J. & Kolbe-Alexander, T. Shift work and the risk of cardiovascular disease. A systematic review and meta-analysis including dose-response relationship. Scand. J. Work Environ. Health. 44(3), 229–38 (2018).
Howell, N. A., Tu, J. V., Moineddin, R., Chu, A. & Booth, G. L. Association between neighborhood walkability and predicted 10-Year cardiovascular disease risk: The CANHEART (cardiovascular health in ambulatory care research team) cohort. J. Am. Heart. Assoc. 8(21), e013146 (2019).
Bakker, E. A. et al. Sedentary behaviour in cardiovascular disease patients: Risk group identification and the impact of cardiac rehabilitation. Int. J. Cardiol. 326, 194–201 (2021).
Wu, Z. et al. Sedentary time, metabolic abnormalities, and all-cause mortality after myocardial infarction: A mediation analysis. Eur. J. Prev. Cardiol. 26(1), 96–104 (2019).
Phillips, C. M., Dillon, C. B. & Perry, I. J. Does replacing sedentary behaviour with light or moderate to vigorous physical activity modulate inflammatory status in adults?. Int. J. Behav. Nutr. Phys. Act. 14(1), 138 (2017).
Wilmot, E. G. et al. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: Systematic review and meta-analysis. Diabetologia. 55(11), 2895–2905 (2012).
Chastin, S. F., Palarea-Albaladejo, J., Dontje, M. L. & Skelton, D. A. Combined effects of time spent in physical activity, sedentary behaviors and sleep on obesity and cardio-metabolic health markers: A novel compositional data analysis approach. PLoS One. 10(10), e0139984 (2015).
Funding
This research was supported by the Patient-Centered Medical Technology Optimization Research Project (HC20C0120020021) through the National Evidence-Based Healthcare Collaborating Agency (NECA) funded by the Ministry of Health and Welfare, Korea. This research was also supported by the Yonsei Signature Research Cluster Project (2021-22-0009) and the Yonsei University Research Fund of 2023-22-0159. The funders had no role in the study design, data collection, analysis, decision to publish, or manuscript preparation.
Author information
Authors and Affiliations
Contributions
S.Y.G. and D.H.L. analyzed the data, S.Y.G. and J.Y.J. wrote the manuscript, M.K.L., D.H.P., T.H.L., J.Y.L., and C.J.L. reviewed and edited the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Goo, S.Y., Lee, M.K., Lee, D.H. et al. Comparing domain- and intensity-specific physical activity in coronary heart disease and non-CHD individuals. Sci Rep 14, 2622 (2024). https://doi.org/10.1038/s41598-024-52764-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-52764-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.