Abstract
With the development of assisted reproductive technology, the number of twin pregnancies is increasing year by year. Given the increased risk of pregnancy complications associated with twin pregnancies, and the fact that these babies are rare and difficult to obtain through assisted reproductive technology, clinicians urgently require finding effective and safe drugs to improve pregnancy outcomes. Low-dose aspirin can not only promote placental blood supply, but also effectively anti-inflammatory. Whether Low-dose aspirin can effectively reduce the risk of pregnancy complications in this special group needs to be clarified. We therefore retrospectively analyzed 665 twin pregnancies from assisted reproduction technology, grouped according to aspirin use, and followed pregnancy outcomes to assess bleeding risk. Low-dose aspirin was found to be effective in preventing preeclampsia without a significant risk of bleeding. However, aspirin does not prevent specific complication in twin pregnancies and seems to have a better preventive effect only when the mother is under 30, which should alarm clinicians should not blindly using aspirin in this particular group.
Similar content being viewed by others
Introduction
Assisted reproductive technology (ART) has become an integral part of modern medicine since 19781. However, pregnancies from ART might not have a better perinatal outcome than non-assisted pregnancies2. On the other hand, growing utilization of assisted reproductive technology (ART) and advanced maternal age births have resulted in an overall increase in the incidence of twin pregnancies3. However, comparing singletons, the complication of twin pregnancies with their increased morbidity and mortality has created significant problems. Including preterm labor (PTL), hypertensive disorders of pregnancy, intrauterine growth restriction and scarred uterus4. The rate of preterm labor in twins is > 50%, approximately two to three times greater as compared to singleton pregnancies5. The relative risk of preeclampsia also has dramatically increase among twins compared to singletons, 3.50 for dichorionic twins and 2.61 for monochorionic twins, respectively6. Rates of caesarean section were significantly higher in twin pregnancies than that in singletons7. Moreover, clinicians should also be aware of the likelihood of psychological problems in mothers of multiples and women undergoing assisted reproductive treatment because of the higher expectation of their pregnancy outcomes8.
Among singletons, preeclampsia and fetal growth restriction often coexist, with related placental pathologie9. Strong evidence suggests that initiation of low-dose aspirin (LDA) prophylaxis prior to 16 weeks gestation reduces the relative risk of developing preeclampsia (PE) or delivering a small for gestational age (SGA) neonate10. Thus, aspirin has been suggested preventing preeclampsia, fetal growth restriction or birth of a small-for-gestational-age (SGA) neonate11. There was a randomised, double-blind, placebo-controlled trial rolled 11,976 women suggested that the incidence of preterm labor in women took aspirin was 11.6%, lower than that in women took aspirin (13.1, RR 0·89 [95% CI 0.81 to 0.98], p = 0.012)12. In addition to these potential benefits, clinicians also need to weigh risks, that is using aspirin during pregnancy might increase the risk of postpartum bleeding13. However, few studies have reported the effectiveness of LDA in twin pregnancies, especially in twin pregnancies from ART14. Accordingly, it was our aim to assess whether there is a beneficial improvement of pregnancy outcomes after LDA use in twin pregnancies from ART.
Results
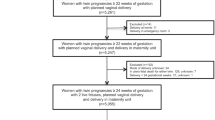
In total, 665 twin pregnancies from ART were recruited in this study. Among them, 155 lost to follow-up were excluded for final analysis. Finally, we obtained complete information from 510 pregnancies (253 in the LDA group and 257 in the control group). The study population included 476 DC and 34 MC according to the type of twins, 500 IVF-ET and 10 IUI according to the mode of conception. The baseline characteristics of the twin pregnancies included in the study are shown in Table 1.
Comparison of prevalence of aspirin use in
In this nearly 6-year study, we found that twin pregnancies from ART are increasing. Aspirin use is also increasingly prevalent in this particular group of pregnant women (χ2 = 75.513, p < 0.05) (Table 2). However, the benefits and risks of aspirin are not clear.
Comparison of complications in twin pregnancies from ART with different aspirin use or not
Complications were compared between the two groups. The incidence of women overall hypertensive disorders of pregnancy was higher in women taking aspirin than in women taking nothing (χ2 = 4.593, p < 0.05). However, the incidence of preeclampsia was lower in women taking aspirin than in women taking nothing (χ2 = 4.283, p < 0.05). Out of we expected, aspirin use did not contribute much to gestational age at delivery. In addition, the incidence of gestational diabetes (χ2 = 0.001, p = 0.978), placenta accrete (χ2 = 0.098, p = 0.754) and placental abruption (χ2 = 1.866, p = 0.172) were not different between women who received aspirin or not. However, the rate of cesarean section neonatal was lower in aspirin use group than that of the no use group, and the difference was statistically significant (χ2 = 4.001, p = 0.045). Other maternal outcomes were similar between the two groups (Table 3). The protective role of LDA on specific complication in twins, however, was uncertain (χ2 = 1.623, p = 0.203) (Table 4).
Comparison of bleeding risk in twin pregnancies from ART with different aspirin use or not
Notably, Aspirin use did not increase the risk of bleeding during delivery or postpartum. No difference in Postpartum hemorrhage (χ2 = 0.063, p = 0.801) and Postpartum bleeding volume (24 h after birth) (p = 0.0754) between the two groups (Supplementary Fig. 1). Also, there was no observed increase in the transfer to Intensive Care Unit (ICU) (χ2 = 0.32, p = 0.572), postpartum blood transfusion (χ2 = 0.186, p = 0.666) and uterine embolism (χ2 = 0.221, p = 0.638) (Table 5).
Comparison of neonatal outcomes in twin pregnancies from ART with different aspirin use or not
There was no statistical significance of the outcome of neonates between the two groups except neonatal gender (p = 0.006). Aspirin may affect uterine artery blood flow, however, neither affect neonatal weight gain (p = 0.491) nor cause their weight differences (p = 0.966). Unfortunately, aspirin use did not reduce their admission to the NICU (p = 0.768) (Table 6).
Comparison of adverse outcomes associated with age in twin pregnancies from ART with different aspirin use or not
To more fully assess the overall effect of LDA during pregnancy. We further revealed a protective effect of aspirin across age stratification. We chose hypertensive disorder complicating pregnancy, preterm birth, SIUGR, TTTS, TRAP, postpartum hemorrhage, maternal ICU transfer, and intrauterine death as maternal adverse outcomes somewhat arbitrarily. And we found that LDA seemed to be more effective in preventing adverse pregnancy outcomes when the mother was younger than 30 years (Fig. 1).
A protective effect of LDA across age stratification: (A) the numerator is the number of mothers who experienced at least one of the 8 outcomes, and the denominator is the total number of mothers at the corresponding age. (B) Cumulative outcomes, meaning that the numerator is the total frequency of all 8 outcomes, while the denominator is 8 times the number of mothers.
Discussion
Twin pregnancies are occurring more frequently with the development of ART, and these women are more likely to develop complications such as gestational hypertension, gestational diabetes, and premature birth15,16,17. There is general consensus on the potential effect of aspirin in early pregnancy for singleton pregnancies to prevent preeclampsia18,19,20, selective fetal restriction21, or preterm labor12. However, the effect and safety of LDA prophylaxis during pregnancy for twin pregnancies from ART has not been discussed. LDA also seems to have a good preventive effect in Twin pregnancies22. Coincidentally, a large proportion of ART pregnant women will take aspirin in the first trimester because they need to increase uterine artery blood flow23,24, which leads us to believe empirically that aspirin will bring good prevention effect in this special group of twin pregnancies from ART. As it turns out, the tepid performance of LDA surprised us. Our study found that aspirin does reduce the risk of PE. However, there was no significant protective effect on other outcomes such as preterm labor and fetal weight. In addition, LDA use in the first trimester did not appear to carry a significant risk of prenatal and postnatal bleeding. At the same time, we further found that the overall preventive effect of LDA was affected by age, with the protective effect of aspirin on adverse pregnancy outcomes disappearing at age 30. These findings indicate that LDA can effectively prevent the occurrence of PE, but also has an maternal age limit.
Unlike common anticoagulants such as heparin, LDA the most widely used antipyretic analgesic and anti-inflammatory drug in the world. After hydrolysis in vivo, aspirin is distributed throughout the body as salicylate and can pass through the placenta25. As a popular and affordable drug in obstetrics and gynecology, LDA can effectively prevent preeclampsia and fetal growth restriction in singleton pregnancy due to its effect on improving placentation26. Aspirin’s role in preventing preterm labor requires further investigation, with some studies showing that LDA can prevent iatrogenic preterm labor caused by preeclampsia27 and others showing that aspirin can reduce the risk of recurrent preterm births28. But there is little strong evidence that LDA as an anti-inflammatory prolongs gestational weeks and prevents spontaneous preterm labor. Onset of preterm labor remains multifactorial with inflammation and immunological disorders. LDA could downregulate many inflammatory factors29, could theoretically lower the incidence of PTL as an immunomodulatory agent. We were fortunate to find that LDA was still effective in preventing PE in twin pregnancies from ART, however LDA was not found to prevent selective fetal restriction or other specific complication in twin pregnancies. Nor did it prolong pregnancy and prevent spontaneous preterm labor. Pregnancy complications in twin pregnancies have more complex mechanisms than in singleton pregnancies, so LDA may not solve all of these problems. Selective fetal restriction does have a similar pathogenesis to hypertensive disorders of pregnancy14,30, LDA may prevent preeclampsia by altering placental blood supply, however, in twin idiopathic disorders, such as TRAP and TTTS, most are caused by abnormal placental angiogenesis during early embryogenesis or abnormal development of the heart in one of the fetuses31,32. LDA alone may not be able to reverse this problem. Even if ART does not increase major obstetric complications and perinatal risk in twin pregnancies33, women who need ART may have underlying problems themselves that increase the risk of adverse pregnancy outcomes. This may also be why LDA does not have the desired overall effect.
Besides, a number of studies have also questioned LDA, which may connect to increased bleeding such as placental abruption and postpartum hemorrhage, leading to concerns that this harmful side effect may outweigh its benefits34,35,36,37. However, low-dose aspirin in our study did not increase the risk of bleeding, which may be due to our dose selection of 100 mg/day and timely discontinuation in the third trimester. As is known to all, LDA’s potential mechanisms for preventing preeclampsia were to improve blood supply to uterine arteries and platelet aggregation38. While, in our study, LDA use still did not increase the incidence of uterine artery embolism, suggesting that the potential risk of LDA is smaller than we expected.
Some previous studies found a frequency of adverse pregnancy outcomes and maternal age39. As an independent risk factor, the risk of pregnancy outcome associated with age cannot be reduced by LDA alone. The current definition of advanced maternal age is delivery at age 35 or older40. However, in our study, LDA appeared to be more protective against complications of pregnancy under 30. There have also been many studies in recent years devoted to finding age cut-offs at risk for singleton pregnancies. Due to ethnic and regional differences, age cutoffs vary, but 30 years old was associated with the absolute risk of pregnancy41. Our results may provide more precise age criteria for LDA use in this particular population of twin pregnancies from ART.
Highlights
To our knowledge, this is a novel study in the obstetrics field, which revealed the effectiveness and risk of LDA in twin pregnancies from ART. To enable clinical workers to correctly face the advantages and disadvantages of drug use, and effectively improve the pregnancy outcome of specific pregnant women on the premise of ensuring the safety of drug use.
Conclusion
As LDA became more widely available, we found that LDA did not have the totally same therapeutic effect in twin pregnancies from ART. LDA (100 mg/days) initiated at early gestational age in twin pregnancies from ART could significantly reduce the risk of PE without increasing the risk of serious bleeding-related complications. This study focuses on the advantages and disadvantages of LDA application and provides a multi-dimensional reference for clinical work.
Materials and methods
Study population
This study was a tertiary hospital-based retrospective cohort study that included women with twin pregnancies from ART between January 2016 and December 2021 were included in the study (n = 665), and their data from electronic standardized prenatal, delivery, and neonatal records. Informed consent was obtained from all participants. Inclusion criteria were: Twins conceived using ART diagnosed by ultrasound in the first visit (gestational age less than 16 weeks); 18–55 years old. Those who did not start their first antenatal care in our hospital were excluded because of their missing maternal prenatal health records. We also excluded women who had reported use of low-molecular-weight heparin or selective serotonin reuptake inhibitors, since we aim to explore the potential benefits of aspirin on twin pregnancies from ART. We finally followed up 510 women (253 in the LDA group and 257 in the control group). The ethics approval was obtained from the Ethics Committee of the First Affiliated Hospital of Chongqing Medical University. All experiments were performed in accordance with relevant guidelines and regulations. Research involving human research participants has been performed in accordance with the Declaration of Helsinki. Enrollment characteristics are presented in Table 1.
Exposure
Owing the fact that there were few evidences suggest the safety of aspirin given in twin pregnancy from ART, the obstetricians in this study carried out different policies on aspirin use for twin pregnancies from ART randomly and thus made this observational study feasible. 100 mg/days given in first prenatal visit (10–16 gestational weeks) was set as the LDA group. All data on aspirin use were obtained from prenatal care records.
Outcome measures
The primary outcomes were the incidence of pregnancy complications which was categorized into (1) common complications during pregnancy, such as gestational age at delivery, hypertensive disorders of pregnancy, preeclampsia (PE), gestational diabetes (GDM), premature rupture of membranes (PROM), placenta accreta placenta, previa placental abruption, intrahepatic cholestasis of pregnancy (ICP), abnormal amniotic fluid, abnormal thyroid function, mode of delivery. And secondary outcomes were specific complication in twins included small for gestational age (SGA), selective intrauterine growth restriction (SIUGR), twin reverse arterial perfusion sequence sign (TRAP), twin-to-twin transfusion syndrome (TTTS), stillbirth and abortion. Clinical safety of aspirin was evaluated by the occurrence of postpartum hemorrhage, transfusion. Uterine artery embolization and transfer to ICU. The assessment of birth and birth-related characteristics included sex ratio, birth weight and transfer to NICU.
Definition
Hypertensive disorders of pregnancy including pregnancy with chronic hypertension, gestational hypertension, Preeclampsia, Eclampsia or HELLP syndrome were defined by blood pressure ≥ 140/90 mmHg associated with proteinuria (> 300 mg/day or not) after 20 weeks of gestational age. Blood pressure was measured by a mercury sphygmomanometer and urine samples were collected and tested by the clinical laboratory in hospital. When calculating the amount of bleeding, intraoperative blood loss was recorded by the container of suction apparatus, while postoperative bleeding volume was counted by weighting. Cesarean postpartum hemorrhage was defined as postoperative bleeding volume > 1000 ml in 24 h, as for vaginal postpartum hemorrhage, was > 500 ml in 24 h. All other complications and adverse pregnancy outcomes were defined following international obstetrical practice.
Statistical analysis
SPSS version 22.0 software (SPSS Inc., Chicago, USA) was used for all statistical analyses. We described as mean ± standard deviation if continuous variables were in accordance with a normal distribution and examined them by the T test. The correlation coefficient is calculated by chi-square test and Fisher exact test to illustrate the correlation between classified variables those were presented by percentage. P < 0.05 was considered statistically significant.
Data availability
All data generated for this study are included in the article, and further inquiries can be directed to the corresponding author.
Abbreviations
- ART:
-
Assisted reproductive technology
- PE:
-
Preeclampsia
- PTL:
-
Preterm labor
- SGA:
-
Small for gestational age
- LDA:
-
Low-dose aspirin
- GDM:
-
Gestational diabetes
- PROM:
-
Premature rupture of membranes
- ICP:
-
Intrahepatic cholestasis of pregnancy
- SIUGR:
-
Selective intrauterine growth restriction
- TRAP:
-
Twin reverse arterial perfusion sequence sign
- TTTS:
-
Twin-to-twin transfusion syndrome
References
De Geyter, C. Assisted reproductive technology: Impact on society and need for surveillance. Best Pract. Res. Clin. Endocrinol. Metab. 33(1), 3–8 (2019).
Helmerhorst, F. M. Perinatal outcome of singletons and twins after assisted conception: A systematic review of controlled studies. BMJ 328(7434), 261 (2004).
Pinborg, A. IVF/ICSI twin pregnancies: Risks and prevention. Hum. Reprod. Update 11(6), 575–593 (2005).
Evans, M. I. et al. Fetal reduction for everyone? Best Pract. Res. Clin. Obstetr. Gynaecol. 84, 76–87 (2022).
Chauhan, S. P. et al. Twins: Prevalence, problems, and preterm births. Am. J. Obstetr. Gynecol. 203(4), 305–315 (2010).
Francisco, C. et al. Hidden high rate of pre-eclampsia in twin compared with singleton pregnancy. Ultrasound Obstetr. Gynecol. 50(1), 88–92 (2017).
Hu, L. Clinical study on different delivery methods of twin pregnancy. Am. J. Perinatol. 40(12), 1306–1310 (2021).
van den Akker, O., Postavaru, G.-I. & Purewal, S. Maternal psychosocial consequences of twins and multiple births following assisted and natural conception: A meta-analysis. Reprod. BioMed. 33(1), 1–14 (2016).
Colson, A. et al. Adaptations of the human placenta to hypoxia: Opportunities for interventions in fetal growth restriction. Hum. Reprod. Update 27(3), 531–569 (2021).
Roberge, S. et al. The role of aspirin dose on the prevention of preeclampsia and fetal growth restriction: Systematic review and meta-analysis. Am. J. Obstetr. Gynecol. 216(2), 110–120 (2017).
Verdecchia, P., Reboldi, G. & Angeli, F. The 2020 International Society of Hypertension global hypertension practice guidelines—Key messages and clinical considerations. Eur. J. Intern. Med. 82, 1–6 (2020).
Hoffman, M. K. et al. Low-dose aspirin for the prevention of preterm delivery in nulliparous women with a singleton pregnancy (ASPIRIN): A randomised, double-blind, placebo-controlled trial. The Lancet 395(10220), 285–293 (2020).
Hastie, R. et al. Aspirin use during pregnancy and the risk of bleeding complications: A Swedish population-based cohort study. Am. J. Obstetr. Gynecol. 224(1), e1–e12 (2021).
Narang, K. & Szymanski, L. M. Multiple gestations and hypertensive disorders of pregnancy: What do we know? Curr. Hypertens. Rep. 23(1), 4 (2020).
Hollier, L. M., McIntire, D. D. & Leveno, K. J. Outcome of twin pregnancies according to intrapair birth weight differences. Obstetr. Gynecol. 94(6), 1006–1010 (1999).
Sebire, N. J. et al. Outcome of twin pregnancies with complete hydatidiform mole and healthy co-twin. The Lancet 359(9324), 2165–2166 (2002).
Gupta, S. et al. Outcomes in twin pregnancies reduced to singleton pregnancies compared with ongoing twin pregnancies. Am. J. Obstetr. Gynecol. 213(4), e1–e5 (2015).
Askie, L. M. et al. Antiplatelet agents for prevention of pre-eclampsia: A meta-analysis of individual patient data. The Lancet 369(9575), 1791–1798 (2007).
Coomarasamy, A. et al. Aspirin for prevention of preeclampsia in women with historical risk factors: A systematic review. Obstetr. Gynecol. 101(6), 1319–1332 (2003).
LeFevre, M. L. Low-dose aspirin use for the prevention of morbidity and mortality from preeclampsia: US preventive services task force recommendation statement. Ann. Intern. Med. 161, 11 (2014).
McCowan, L. M., Figueras, F. & Anderson, N. H. Evidence-based national guidelines for the management of suspected fetal growth restriction: Comparison, consensus, and controversy. Am. J. Obstetr. Gynecol. 218(2), S855–S868 (2018).
Ye, Y. et al. Low-dose aspirin for primary prevention of adverse pregnancy outcomes in twin pregnancies: An observational cohort study based on propensity score matching. BMC Pregn. Childbirth 21(1), 2 (2021).
Dirckx, K. et al. Does low-dose aspirin improve pregnancy rate in IVF/ICSI? A randomized double-blind placebo controlled trial. Hum. Reprod. 24(4), 856–860 (2008).
Zhu, Q. et al. A retrospective study on IVF/ICSI outcome in patients with anti-nuclear antibodies: The effects of prednisone plus low-dose aspirin adjuvant treatment. Reprod. Biol. Endocrinol. 11(1), 1–9 (2013).
Mueller, R. L. First-generation agents: Aspirin, heparin and coumarins. Best Pract. Res. Clin. Haematol. 17(1), 23–53 (2004).
Bujold, E., Roberge, S. & Nicolaides, K. H. Low-dose aspirin for prevention of adverse outcomes related to abnormal placentation. Prenatal Diagn. 34(7), 642–648 (2014).
van Vliet, E. O. G. et al. Antiplatelet agents and the prevention of spontaneous preterm birth. Obstetr. Gynecol. 129(2), 327–336 (2017).
Kupka, E. et al. Low-dose aspirin use in pregnancy and the risk of preterm birth: A Swedish register-based cohort study. Am. J. Obstetr. Gynecol. 228(3), e1–e9 (2023).
Esplin, M. S. Overview of spontaneous preterm birth: A complex and multifactorial phenotype. Clin. Obstetr. Gynecol. 57(3), 518–530 (2014).
Sinkey, R. G. et al. Prevention, diagnosis, and management of hypertensive disorders of pregnancy: A comparison of international guidelines. Curr. Hypertens. Rep. 22, 1–10 (2020).
Gembruch, U. et al. Twin reversed arterial perfusion sequence in twin-to-twin transfusion syndrome after the death of the donor co-twin in the second trimester. Ultrasound Obstetr. Gynecol. 17(2), 153–156 (2001).
De Paepe, M. E. Examination of the twin placenta. Semin. Perinatol. 39, 27 (2015).
Liu, T. et al. Hypertensive disorders of pregnancy and neonatal outcomes in twin vs singleton pregnancies after assisted reproductive technology. Front. Pediatr. 10, 839882 (2022).
Fiala, C. & Pasic, M. D. Aspirin: Bitter pill or miracle drug? Clin. Biochem. 85, 1–4 (2020).
Roberge, S., Bujold, E. & Nicolaides, K. H. Meta-analysis on the effect of aspirin use for prevention of preeclampsia on placental abruption and antepartum hemorrhage. Am. J. Obstetr. Gynecol. 218(5), 483–489 (2018).
Golding, J., Jamaica Low Dose Aspirin Study Group. A randomised trial of low dose aspirin for primiparae in pregnancy. BJOG Int. J. Obstetr. Gynaecol. 105(3), 293–299 (1998).
Sibai, B. M. et al. Prevention of preeclampsia with low-dose aspirin in healthy, nulliparous pregnant women. N. Engl. J. Med. 329(17), 1213–1218 (1993).
Rolnik, D. L., Nicolaides, K. H. & Poon, L. C. Prevention of preeclampsia with aspirin. Am. J. Obstet. Gynecol. 226(2S), S1108–S1119 (2022).
Sheen, J. et al. Maternal age and risk for adverse outcomes. Am. J. Obstetr. Gynecol. 219(4), 390.e1-390.e15 (2018).
Frick, A. Advanced maternal age and adverse pregnancy outcomes. Best Pract. Res. Clin. Obstetr. Gynaecol. 70, 92–100 (2021).
Waldenström, U. et al. Adverse pregnancy outcomes related to advanced maternal age compared with smoking and being overweight. Obstetr. Gynecol. 123(1), 104–112 (2014).
Acknowledgements
The authors thank participants in this retrospective cohort study and the study physicians and nurses for their contributions to this study.
Funding
The funding was provided by The National Natural Science Foundation of China (82171668) and also by National Key Research and Development Program of China (2022YFC2704700).
Author information
Authors and Affiliations
Contributions
Conception of the study: D.H., X.L. and H.Q. Data collection: Y.X., P.D., J.W. and J.X. Statistical analysis: D.H. All authors made substantial contributions to the paper and read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Huang, D., Xie, Y., Duan, P. et al. Potential impact on using aspirin as the primary prevention of adverse pregnancy outcomes in twins conceived using ART. Sci Rep 14, 2223 (2024). https://doi.org/10.1038/s41598-024-51543-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-51543-4
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.