Abstract
Severe trauma could induce sepsis due to the loss of control of the infection, which may eventually lead to death. Accurate and timely diagnosis of sepsis with severe trauma remains challenging both for clinician and laboratory. Combinations of markers, as opposed to single ones, may improve diagnosis. We compared the diagnostic characteristics of routinely used biomarkers of sepsis alone and in combination, trying to define a biomarker panel to predict sepsis in severe patients. This prospective observational study included patients with severe trauma (Injury severity score, ISS = 16 or more) in the emergency intensive care unit (EICU) at a university hospital. Blood samples were collected and plasma levels of procalcitonin (PCT), C-reactive protein (CRP), interleukin-6 (IL-6) and serum amyloid A (SAA) were measured using commercial enzyme linked immunosorbent assay (ELISA) kits. A total of 100 patients were eligible for analysis. Of these, 52 were diagnosed with sepsis. CRP yielded the highest discriminative value followed by PCT. In multiple logistic regression, SAA, CRP, and PCT were found to be independent predictors of sepsis. Bioscore which was composed of SAA, CRP, and PCT was shown to be far superior to that of each individual biomarker taken individually. Therefore, compared with single markers, the biomarker panel of PCT, CRP, and SAA was more predictive of sepsis in severe polytrauma patients.
Similar content being viewed by others
Introduction
Polytrauma means an anatomical injury of abbreviated injury scale (AIS) ≥ 3 in at least two body regions with the presence of systemic inflammatory response syndrome (SIRS) on at least one day during the first 72 h1. These patients are at risk of higher morbidity and mortality than the summation of expected morbidity and mortality of their individual injuries. Severe traumas induce a systemic inflammatory response that may be followed by an anti-inflammatory response2, which contributes to a state of transient immunosuppression3,4,5. A number of factors like poor blood perfusion, wound infection and stress response will lead to a series of pathophysiological processes such as ischemia and hypoxia, infection and sepsis, septic shock or multiple organ dysfunction syndrome, which eventually lead to death. Sepsis may induce fatal organ failures due to the loss of control of the infection, thereby leading to septic shock. There are 31,500,000 cases of sepsis every year worldwide, with 5,300,000 death and 17% mortality rate6, and it costs 170 billions dollars annually to treat the sepsis patients7. Therefore, it has become one of the most vital issues to lower the occurrence and mortality of sepsis in the field of critical medicine.
Despite the progress in the management of primary injury and supportive care in polytrauma patients, the incidence and mortality rate of post-traumatic sepsis have not been reduced to an acceptable level. If the incidence and outcome of post-traumatic sepsis can be predicted early, and the intervention measures can be implemented early for the high-risk injured patients, the incidence and mortality rate can be effectively decreased. Therefore, early intervention to prevent subsequent or worsening clinical deterioration is a key to the successful treatment of patients with potentially severe sepsis8,9. However, it is often difficult to determine which of the post-traumatic patients with signs of infection on initial evaluation have, or will develop, more severe illness. Therefore, the development of new biomarkers is desirable. However, to our knowledge, to date there is no single accepted biomarker or combination of biomarkers for use in patients with suspected sepsis. Many potential biomarkers have been investigated, but only C-reactive protein (CRP) and procalcitonin (PCT) are currently used on a routine basis10,11,12. Concentration of interleukin-6 (IL-6) is in relation with the severity of injury13, and serum amyloid A (SAA) and IL-6 are also of potential interest. Because sepsis is comprised of an array of signaling proteins from various cascades, we hypothesized that use of a multiple marker approach would improve clinical utility compared with the use of a single marker. That means, the search for a single magic bullet marker might ultimately be fruitless, but a combination of markers could improve diagnosis, prognosis and treatment efficacy, and thus survival10. Here, we performed a prospective study aimed at evaluating the diagnostic accuracy of PCT, CRP, IL-6 and SAA alone or in combination for differential diagnosis of post-traumatic sepsis, to possibly define a panel of biomarkers that would assess risk of sepsis in critically ill post-traumatic patients at emergency intensive care unit (EICU) admission.
Results
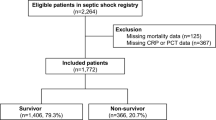
Characteristics of the inception cohort patients
Among the 100 patients enrolled in this study, 52 (52%) were diagnosed with sepsis. Clinical and demographic characteristics, comorbidity and prognosis are summarized in Table 1. At admission, the proportion of male, age, Injury Severity Score (ISS), sepsis-related organ failure assessment (SOFA) score and acute physiology and chronic health evaluation (APACHE) II score were higher in sepsis group than in control group, and the total score of Glasgow coma score (GCS) was lower in sepsis group than in control group (P < 0.05). Also, the length of ICU stay and mortality rate were significantly higher in sepsis group than in control group (P < 0.05).
At admission and during the first seven days in the hospital, blood cultures, urine cultures, sputum cultures, swabs cultures and cerebrospinal fluid cultures were conducted in all enrolled patients. All 52 patients in sepsis group were classified as having infection, and a clinically relevant pathogen was isolated from the sepsis patients. All the infections were caused by bacteria according to the culture results. The primary sites of infection and microorganisms isolated are summarized in Table 2.
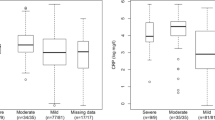
Patients’ blood samples were collected at 8 a.m. every day after admission to the EICU, and finally five samples of each patient were chosen for analysis. For the sepsis group, the five time points of the samples were the day of sepsis, 24 h before or after sepsis, 48 h before and after sepsis; for the no-sepsis group, blood samples of 5 days from the day of admission to the EICU were analyzed. The levels of the four biomarkers are shown in Table 3. SAA (on sepsis, and at 24 h and 48 h after sepsis), CRP (at 48 h and 24 h before sepsis, on sepsis, and at 24 h and 48 h after sepsis), PCT (at 48 h and 24 h before sepsis, on sepsis, and at 24 h and 48 h after sepsis), IL-6 (on sepsis, and at 24 h after sepsis) were significantly higher in patients with sepsis compared with no-sepsis (P < 0.05).
As shown in Fig. 1, CRP yielded the highest discriminative value with an area under the ROC curve (AUC) of 0.82 (82% confidence interval [CI] 0.73–0.91; P < 0.001), followed by PCT (AUC 0.77 [0.68–0.86]; P < 0.001). Table 4 summarizes the performances of each of these biomarkers in diagnosing sepsis. CRP proved to be the optimal individual marker in terms of specificity (90%) and sensitivity (71%).
In multiple logistic regression, SAA, CRP, and PCT were found to be independent predictors of sepsis (Table 5).
Areas under the receiver operating characteristic curves for SAA (0.75 [95% CI 0.65–0.84]); CRP (0.82 [95% CI 0.73–0.91]); PCT (0.77 [95% CI 0.68–0.86]); and IL-6 (0.75 [95% CI 0.65–0.85]). CI = confidence interval; SAA = serum amyloid A; CRP = C-reactive protein; PCT = procalcitonin; IL-6 = Interleukin-6.
Combination of PCT, CRP, and SAA Index in a bioscore
Since SAA, CRP, and PCT were found to be independent predictors of sepsis from the result of multiple logistic regression, we need to determine whether the combination of these three biomarkers into a single bioscore could improve the diagnostic performance. We used a sepsis bioscore14 to report the multimarker assessment. This score was calculated using standard methods by utilizing the derived equation from the multivariate regression model:
For the multimarker assessment for sepsis, bioscore = − 4.760 + 0.007 SAA + 0.004 CRP + 0.102 PCT was used to calculate that bioscore for each patient. When the bioscore was entered into the multiple logistic regression model (Fig. 2), its performance with AUC = 0.89 (95% CI 0.82–0.95), cut-off = 0.28, sensitivity = 0.77, specificity = 0.9, P < 0.001, was shown to be far superior to that of each individual biomarker taken individually.
CI = confidence interval; SAA = serum amyloid A; CRP = C-reactive protein; PCT = procalcitonin.
Identification of independent risk factors for sepsis
We used logistic regression models to identify independent risk factors for sepsis by analyzing patients' clinical variables and biosore. Clinical variables included sex, age, ISS, SOFA score, APACHE II score, history of smoking, history of drinking alcohol, GCS, vital signs of body temperature, pulse, respiratory rate, blood pressure, oxygen saturation of pulse, and usage of vasopressors. Bioscore was composed of the three biomarkers, SAA, CRP, and PCT, as mentioned in Fig. 2.
Univariate logistic regression analysis revealed that age (OR = 1.045, 95% CI 1.018–1.074, P = 0.001), ISS (OR = 1.248, 95% CI 1.146–1.360, P < 0.001), SOFA score (OR = 1.047, 95% CI 1.015–1.080, P = 0.004), APACHE2 score (OR = 1.077, 95% CI 1.035–1.121, P < 0.001), GCS (OR = 0.636, 95% CI 0.524–0.772, P < 0.001), and bioscore (OR = 3.194, 95% CI 1.940–5.258, P < 0.001) were associated with sepsis, as shown in Table 6.
Then, all the significant univariates were taken into multiple logistic analysis, and proved that only ISS (OR = 1.265, 95% CI 1.077–1.487, P = 0.004), SOFA score (OR = 1.184, 95% CI 1.005–1.394, P = 0.043), and bioscore (OR = 3.067, 95% CI 1.187–7.925, P = 0.021) were the independent risk factors, as shown in Table 7.
Discussion
In this study, we assembled a cohort of patients with severe trauma and studied several common biomarkers, including PCT, CRP, IL-6 and SAA, with the overall goal of creating a panel that would allow discrimination of ICU patients who are at increased risk of sepsis. Of all the clinical data, ISS and SOFA score were found to be independent risk factors for post-traumatic sepsis. Of the biomarkers, we showed here that PCT, CRP and SAA were useful in the diagnosis of sepsis. Subsequently, we combined these markers into a simple score, called “bioscore”, which turned out to be associated with an impressive diagnostic value for having or not having sepsis. The results of this study have several potential implications.
First, this study helps to support the independent associations of ISS with the risk of post-traumatic sepsis. As reported in previous studies, the incidence of post-traumatic sepsis ranged from 1.4 to 14.4%15,16. The occurrence of sepsis during post-traumatic events was found to be 2% in a study by Osborn et al.17, while Wafaisade et al.18 indicated that 10% of trauma patients developed sepsis. One reason for such differences in the occurrence rate of post-traumatic sepsis is thought to be the differences in the injury severity in the patients in each study. A prospective study including 183 trauma patients reported that ISS was relevant as the risk factor for sepsis19. Another retrospective study reviewed 422 trauma patients with ISS ≥ 15 and found that ISS was an associated factor for sepsis-320.
Second, this study showed SOFA score, instead of APACHE II score, was the independent risk factor for post-traumatic sepsis. We may possibly find answers from the evolution history of the concept of sepsis. In 201621, the European Society of Intensive Care Medicine and the Society of Critical Care Medicine (SCCM) created a task force that proposed Sepsis-3, a new definition for sepsis. The new definition excluded the establishment of systemic inflammatory response syndrome (SIRS) criteria to define sepsis and made it more nonspecific as any life-threatening organ dysfunction caused by the dysregulated host response to infection. The task force claimed that sequential organ failure assessment (SOFA) had a better predictive validity for sepsis than SIRS criteria. It had better prognostic accuracy and the ability to predict in-hospital mortality.
Third, four biomarkers of SAA, CRP, PCT, and IL-6 showed different results. All of them were significantly higher in patients with sepsis than in those without sepsis at several specific time points as described previously, but only SAA, CRP, and PCT were found to be independently predictive of sepsis except IL-6 as shown in this study. To date, CRP and PCT are quite widely used and studied biomarkers during sepsis in recent studies. Although PCT is considered superior to CRP in a number of studies22,23, it is not a definitive test for diagnosing sepsis because PCT levels can also be increased in other conditions24. And the combination of these two biomarkers may improve their ability to exclude sepsis25. SAA has been proposed as a potential biomarker for sepsis due to its rapid and robust induction in the early stages of the disease. Several studies have investigated the utility of SAA in predicting sepsis, either alone or in combination with other biomarkers. Many animal studies found that SAA concentration was higher in septic groups and can be used as a marker to rule out sepsis and nonsurvival26,27. Yuan et al. concluded that the level of SAA in sepsis is most useful in combination with other markers such as CRP and PCT as well as determining their correlation and SAA could be promising and meaningful in the diagnosis of neonatal sepsis28. Another study showed that SAA had overall better diagnostic accuracy in predicting neonatal late-onset sepsis compared to CRP and specificity29. IL-6 is considered as useful in septic patients but increase of its level is not specifically linked to infectious conditions30. Another study showed that IL-6 could be used as both diagnostic and prognostic biomarkers for sepsis and septic shock diagnosed in accordance with the Sepsis-3 definitions, and IL-6 was superior to PCT in both diagnostic and prognostic value for sepsis and septic shock31. Above all, numerous studies have produced a variety of results for these four biomarkers. However, to our knowledge, there is no study testing the diagnostic and prognostic values of the bioscore composed of the four biomarkers. The “bioscore” concept is considered biologically plausible as it incorporates biomarkers involved in key components of pathophysiology of sepsis. The multimarker bioscore offers a distinct mechanistic advantage over single-marker approaches14,32,33.In this study, the bioscore of these routinely available biomarkers was shown to be far superior to that of each individual biomarker taken individually in the prediction of sepsis, which was found to be associated with an impressive diagnostic accuracy and be useful in clinical practice in rapidly assigning the patients to having or not having sepsis.
This study has several limitations. First, the patients enrolled in the group were in post-traumatic period and the final results were post-traumatic sepsis or no-sepsis, which may restrict the pathophysiology of sepsis. Second, although we collected blood samples dynamically after admission, time-points in the final study were still five fixed cross-sectional points, and this did not precisely reflect the dynamic process of sepsis evolution. Third, although these four indicators of PCT, CRP, IL-6 and SAA are common and easy to measure in clinical practice, whether they are the optimal combination still needs further study. Finally, the study involves a relatively small sample size of 100 patients from a single center. This may limit the generalizability of the findings, as patient populations and healthcare practices can vary across different institutions and regions. We hope to further expand the sample size in the later stage to enhance the representativeness of the research results.
Conclusions
This prospective study illustrates the high value of bioscore combining PCT, CRP and SAA, which shows a significant predictive value for sepsis in severe post-traumatic patients. Further investigations are warranted to validate these findings and to assess whether the bioscore may be successfully used in ICUs and on which screening criteria. And if possible, we may measure these biomarkers using a poit-of-care-test (POCT) device to rapidly assay biomarkers and to produce the sepsis bioscore as its output to predict the possibility of sepsis. This approach offers a practical opportunity to improve bedside testing method of ICU patients with suspected sepsis in a clinically useful manner. This study, furthermore, provides robust thresholds for all readily obtained parameters as a strong basis for further multicenter studies.
Methods
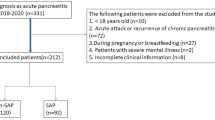
Study population
This prospective observational study was carried out over a 16-month period (August 2021–November 2022) in the EICU of the Third Hospital of Hebei Medical University (a 2000-bed hospital, and also a trauma emergency center at provincial level), China. Inclusion criteria were EICU patients aged 18 or older, and an Injury Severity Score (ISS)34,35 16 or more. Clinical exclusion criteria were age of less than 18 years, ISS of less than 16, pregnancy, chronic corticosteroid or Immunosuppressant therapy, do-not-resuscitate status and cardiac arrest.
Approval of the institutional review board and informed consent were obtained from our hospital before inclusion. Informed consent was obtained directly from each patient/legal representative before enrollment.
Data collection
All polytrauma patients admitted were followed up prospectively until the day they were transferred out of EICU or died. During admission, clinical and therapeutic data were collected. Clinical data collection comprised demographics (age, gender), ISS, the sepsis-related organ failure assessment (SOFA) score36, the acute physiology and chronic health evaluation (APACHE) II score37, comorbid conditions (e.g., hypertension, diabetes, vascular diseases, and other diseases including arrhythmia, cirrhosis, rheumatoid arthritis, diseases of the thyroid gland or end-stage renal diseases), social factors (history of smoking or alcohol use), vital signs (glasgow coma score [GCS], body temperature, pulse rate, respiratory rate, blood pressure, oxygen saturation), infection characteristics (sources and microorganisms identified). Therapeutic data were also collected on admission to the EICU, including the use of mechanical ventilation (MV), the use of vasopressors, the length of ICU stay and mortality rate were also recorded. The latest diagnostic criteria for sepsis 3.0 were infection + SOFA ≥ 238.
Sample collection and biomarker assays
Ethylenediaminetetraacetic acid (EDTA)-anticoagulated blood samples were collected at 8 a.m. every day after admission to the EICU (that is, at day 0, 1, 2… until the day included patients were transferred out of EICU). Samples were acquired through central venous or arterial catheter, as the severity of the trauma required such equipment. Blood samples were stored immediately at 4 °C and then centrifuged (3000 g × 10 min) within 2 h after collection. Plasma levels of PCT, CRP, IL-6 and SAA were measured using commercial ELISA kits, according to the manufacturers’ recommendations (Dry fluorescence immunoassay analyzer QD-S300, Nanjing Vazyme MedTech Co., Ltd, Nanjing, China). Interassay and intraassay coefficients of variation were lower than 15%. The detection limits were 0.046 ng/ml, 3 mg/L, 7 pg/ml and 10 mg/L, respectively.
Statistical analysis
All statistical analysis were performed using R4.0 and GraphPad Prism 8.0 (GraphPad Software, La Jolla, CA). Normal distribution data were presented as mean ± standard deviation (mean ± SD), while skewed distribution data were presented as median (M) or interquartile range (IQR). Normal distribution data were analyzed by t-test, and skewed distribution data were analyzed by nonparametric test. The count data were described by frequency and analyzed by chi-square test. Receiver operating characteristic (ROC) curves were used to evaluate the ability of the biomarkers to identify the possibility of sepsis in the enrolled patients. Logistic regression models were used to identify independent risk factors for sepsis. P < 0.05 was considered statistically significant.
Ethical approval and informed consent
All methods were carried out in accordance with relevant guidelines and regulation under the ‘Ethics approval and consent to participate’ in the declaration section of the manuscript. This study was approved by the Institutional Review Board of the Third Hospital of Hebei Medical University [approval number: W2021-089-1; January 21, 2021]. Written informed consent was obtained directly from each patient/legal representative before enrollment.
Data availability
All data generated or analyzed during this study are included in this published article.
References
Butcher, N. & Balogh, Z. J. The definition of polytrauma: The need for international consensus. Injury 40(Suppl 4), S12-22. https://doi.org/10.1016/j.injury.2009.10.032 (2009).
Adib-Conquy, M. & Cavaillon, J. M. Compensatory anti-inflammatory response syndrome. Thromb. Haemost. 101, 36–47 (2009).
Khalid, N., Patel, P. D., Alghareeb, R., Hussain, A. & Maheshwari, M. V. The effect of sepsis on myocardial function: A review of pathophysiology, diagnostic criteria, and treatment. Cureus 14, e26178. https://doi.org/10.7759/cureus.26178 (2022).
Bone, R. C. Immunologic dissonance: A continuing evolution in our understanding of the systemic inflammatory response syndrome (SIRS) and the multiple organ dysfunction syndrome (MODS). Ann. Intern. Med. 125, 680–687. https://doi.org/10.7326/0003-4819-125-8-199610150-00009 (1996).
Ward, N. S., Casserly, B. & Ayala, A. The compensatory anti-inflammatory response syndrome (CARS) in critically ill patients. Clin. Chest Med. 29, 617–625. https://doi.org/10.1016/j.ccm.2008.06.010 (2008).
Liu, V. X. et al. Multicenter implementation of a treatment bundle for patients with sepsis and intermediate lactate values. Am. J. Respir. Crit. Care Med. 193, 1264–1270. https://doi.org/10.1164/rccm.201507-1489OC (2016).
Zilberman-Itskovich, S. et al. The epidemiology of multidrug-resistant sepsis among chronic hemodialysis patients. Antibiotics 11, 1255. https://doi.org/10.3390/antibiotics11091255 (2022).
Kumar, A. et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit. Care Med. 34, 1589–1596. https://doi.org/10.1097/01.CCM.0000217961.75225.E9 (2006).
Park, S. K. et al. The effect of early goal-directed therapy for treatment of severe sepsis or septic shock: A systemic review and meta-analysis. J. Crit. Care 38, 115–122. https://doi.org/10.1016/j.jcrc.2016.10.019 (2017).
Carrigan, S. D., Scott, G. & Tabrizian, M. Toward resolving the challenges of sepsis diagnosis. Clin. Chem. 50, 1301–1314. https://doi.org/10.1373/clinchem.2004.032144 (2004).
Meisner, M. Biomarkers of sepsis: Clinically useful?. Curr. Opin. Crit. Care 11, 473–480. https://doi.org/10.1097/01.ccx.0000176694.92883.ce (2005).
Marshall, J. C. et al. Measures, markers, and mediators: toward a staging system for clinical sepsis: A report of the Fifth Toronto Sepsis Roundtable, Toronto, Ontario, Canada, October 25–26, 2000. Crit. Care Med. 31, 1560–1567. https://doi.org/10.1097/01.CCM.0000065186.67848.3A (2003).
Jawa, R. S., Anillo, S., Huntoon, K., Baumann, H. & Kulaylat, M. Analytic review: Interleukin-6 in surgery, trauma, and critical care: Part I: Basic science. J. Intensive Care Med. 26, 3–12. https://doi.org/10.1177/0885066610395678 (2011).
Shapiro, N. I. et al. A prospective, multicenter derivation of a biomarker panel to assess risk of organ dysfunction, shock, and death in emergency department patients with suspected sepsis. Crit. Care Med. 37, 96–104. https://doi.org/10.1097/CCM.0b013e318192fd9d (2009).
Kisat, M. et al. Predictors of sepsis in moderately severely injured patients: An analysis of the National Trauma Data Bank. Surg. Infect. (Larchmt) 14, 62–68. https://doi.org/10.1089/sur.2012.009 (2013).
Muckart, D. J. & Bhagwanjee, S. American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference definitions of the systemic inflammatory response syndrome and allied disorders in relation to critically injured patients. Crit. Care Med. 25, 1789–1795. https://doi.org/10.1097/00003246-199711000-00014 (1997).
Osborn, T. M., Tracy, J. K., Dunne, J. R., Pasquale, M. & Napolitano, L. M. Epidemiology of sepsis in patients with traumatic injury. Crit. Care Med. 32, 2234–2240. https://doi.org/10.1097/01.ccm.0000145586.23276.0f (2004).
Wafaisade, A. et al. Epidemiology and risk factors of sepsis after multiple trauma: An analysis of 29,829 patients from the Trauma Registry of the German Society for Trauma Surgery. Crit. Care Med. 39, 621–628. https://doi.org/10.1097/CCM.0b013e318206d3df (2011).
Park, J. H. et al. Risk factors for sepsis in Korean trauma patients. Eur. J. Trauma Emerg. Surg. 42, 453–458. https://doi.org/10.1007/s00068-015-0552-6 (2016).
Chung, S. et al. Timing and associated factors for sepsis-3 in severe trauma patients: A 3-year single trauma center experience. Acute Crit. Care 33, 130–134. https://doi.org/10.4266/acc.2018.00122 (2018).
Chakraborty, R. K. & Burns, B. in StatPearls (2023).
Shilpakar, R. et al. Procalcitonin and C-reactive protein as markers of bacteremia in patients with febrile neutropenia who receive chemotherapy for acute Leukemia: A prospective study from Nepal. J. Glob. Oncol. 5, 1–6. https://doi.org/10.1200/JGO.19.00147 (2019).
Shokripour, M., Omidifar, N., Salami, K., Moghadami, M. & Samizadeh, B. Diagnostic accuracy of immunologic biomarkers for accurate diagnosis of bloodstream infection in patients with malignancy: Procalcitonin in comparison with C-reactive protein. Can. J. Infect. Dis. Med. Microbiol. 2020, 8362109. https://doi.org/10.1155/2020/8362109 (2020).
Park, J. H. et al. Clinical relevance of procalcitonin and C-reactive protein as infection markers in renal impairment: A cross-sectional study. Crit. Care 18, 640. https://doi.org/10.1186/s13054-014-0640-8 (2014).
Han, J. H. et al. Use of a combination biomarker algorithm to identify medical intensive care unit patients with suspected sepsis at very low likelihood of bacterial infection. Antimicrob. Agents Chemother. 59, 6494–6500. https://doi.org/10.1128/AAC.00958-15 (2015).
Barr, B. & Nieman, N. M. Serum amyloid A as an aid in diagnosing sepsis in equine neonates. Equine Vet. J. 54, 922–926. https://doi.org/10.1111/evj.13540 (2022).
Hoeberg, E. et al. Serum amyloid A as a marker to detect sepsis and predict outcome in hospitalized neonatal foals. J. Vet. Intern. Med. 36, 2245–2253. https://doi.org/10.1111/jvim.16550 (2022).
Yuan, H. et al. Diagnosis value of the serum amyloid A test in neonatal sepsis: A meta-analysis. Biomed. Res. Int. 2013, 520294. https://doi.org/10.1155/2013/520294 (2013).
Ucar, B. et al. Serum amyloid A, procalcitonin, tumor necrosis factor-alpha, and interleukin-1beta levels in neonatal late-onset sepsis. Mediat. Inflamm. 2008, 737141. https://doi.org/10.1155/2008/737141 (2008).
Harbarth, S. et al. Diagnostic value of procalcitonin, interleukin-6, and interleukin-8 in critically ill patients admitted with suspected sepsis. Am. J. Respir. Crit. Care Med. 164, 396–402. https://doi.org/10.1164/ajrccm.164.3.2009052 (2001).
Song, J. et al. Diagnostic and prognostic value of interleukin-6, pentraxin 3, and procalcitonin levels among sepsis and septic shock patients: a prospective controlled study according to the Sepsis-3 definitions. BMC Infect. Dis. 19, 968. https://doi.org/10.1186/s12879-019-4618-7 (2019).
Andaluz-Ojeda, D. et al. A combined score of pro- and anti-inflammatory interleukins improves mortality prediction in severe sepsis. Cytokine 57, 332–336. https://doi.org/10.1016/j.cyto.2011.12.002 (2012).
Gibot, S. et al. Combination biomarkers to diagnose sepsis in the critically ill patient. Am. J. Respir. Crit. Care Med. 186, 65–71. https://doi.org/10.1164/rccm.201201-0037OC (2012).
Grandic, L., Olic, I., Pogorelic, Z., Mrklic, I. & Perko, Z. The value of injury severity score and abbreviated injury scale in the management of traumatic injuries of parenchymal abdominal organs. Acta Clin. Croat 56, 453–459. https://doi.org/10.20471/acc.2017.56.03.12 (2017).
MacKenzie, E. J., Shapiro, S. & Eastham, J. N. The abbreviated injury scale and injury severity score: Levels of inter- and intrarater reliability. Med. Care 23, 823–835. https://doi.org/10.1097/00005650-198506000-00008 (1985).
Vincent, J. L. et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure: On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 22, 707–710. https://doi.org/10.1007/BF01709751 (1996).
Knaus, W. A., Draper, E. A., Wagner, D. P. & Zimmerman, J. E. APACHE II: A severity of disease classification system. Crit. Care Med. 13, 818–829 (1985).
Singer, M. et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315, 801–810. https://doi.org/10.1001/jama.2016.0287 (2016).
Funding
This project was funded by the Scientific Research Fund Project of Hebei Provincial Department of Health (20211688).
Author information
Authors and Affiliations
Contributions
M.L. designed the study, planned the analysis and drafted the manuscript. Y.-J.Q., W.-C., and X.-L.Z. gave suggestions for the study design and analyzed data. C.-H.Z., R.-J.C. and D.-Z.H. helped collect samples and were involved in collection of data. S.-M.D. gave suggestions for the study design and revised the manuscript. All authors have reviewed and approved the submitted version and have agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, M., Qin, Yj., Zhang, Xl. et al. A biomarker panel of C-reactive protein, procalcitonin and serum amyloid A is a predictor of sepsis in severe trauma patients. Sci Rep 14, 628 (2024). https://doi.org/10.1038/s41598-024-51414-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-51414-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.